Abstract
In April 2022, mandatory kilocalorie (kcal) labelling in the out-of-home food sector was introduced as a policy to reduce obesity in England. Here we examined whether the implementation of this policy was associated with a consumer behaviour change. Large out-of-home food sector outlets subject to kcal labelling legislation were visited pre- and post-implementation, and customer exit surveys were conducted with 6,578 customers from 330 outlets. Kcals purchased and consumed, knowledge of purchased kcals and reported noticing and use of kcal labelling were examined. The results suggested that the introduction of the mandatory kcal labelling policy in England was not associated with a significant decrease in self-reported kcals purchased (B = 11.31, P = 0.564, 95% confidence interval (CI) −27.15 to 49.77) or consumed (B = 18.51, P = 0.279, 95% CI −15.01 to 38 52.03). Post-implementation, participants underestimated the energy content of their purchased meal less (B = 61.21, P = 0.002, 95% CI 21.57 to 100.86) and were more likely to report noticing (odds ratio 2.25, P < 0.001, 95% CI 1.84 to 2.73) and using (odds ratio 2.15, P < 0.001, 95% CI 1.62 to 2.85) kcal labelling, which may have wider public health implications.
Similar content being viewed by others
Main
Food provided in the OHFS tends to be energy-dense and high in kilocalories (kcals)1,2. Frequently consuming food from the OHFS is associated with increased obesity risk3. This is problematic because, according to a 2015 study, 27% of UK adults eat foods in the OHFS once per week or more4. Obesity is a major global public health problem. In England, recent data suggest that 26% of people live with obesity5, with obesity linked to a range of diseases, including type 2 diabetes, several cancers and cardiovascular disease6,7,8,9,10. Obesity produces a substantial health care burden in the United Kingdom11,12. A likely contributing factor to obesity is the out-of-home food sector (OHFS). Obesity is also socio-demographically patterned13,14, and public health interventions are required to reduce obesity and its social inequalities.
Multiple countries, including the United States15 and parts of Canada16 have implemented mandatory kcal labelling legislation in response to the growing contribution of the OHFS on diet. In 2011, as part of the UK public health responsibility deal17, OHFS businesses were encouraged to make voluntary pledges to provide kcal labelling18. However, a 2018 study found that only 17% (18 out of 104) of OHFS outlets assessed in England were providing in-store kcal labelling, and when labelling was present, it did not adhere to government proposed best practice guidelines19. Motivated by a lack of voluntary compliance, the UK government announced the Calorie Labelling (Out of Home Sector) (England) Legislation 2021, with a policy enactment deadline of 6 April 2022 for eligible businesses20,21,22. The legislation applied to large (>250 employees) businesses (cafes, fast-food outlets, sit-down restaurants and pubs) in England selling food for immediate consumption. It requires businesses to provide kcal labelling on all unpackaged food and non-alcoholic drink items that are on the menu for more than 30 days per year, alongside contextual information on recommended kcal consumption23.
Systematic reviews examining the effect of kcal labelling on consumer behaviour have concluded that kcal labelling has a modest to null effect on kcals selected or purchased24,25,26,27,28,29. For example, a Cochrane review by Crockett et al.30 indicated that kcal labelling was associated with a reduction of ~47 kcals purchased30, but there was a high level of uncertainty in this estimate. Similar to England, the United States implemented mandatory labelling applying to food outlets with more than 20 locations in 2018. Petimar et al.31 examined whether kcal labelling changed purchasing behaviour for meals across 104 restaurants from a fast-food franchise pre- versus post-policy implementation. Using retail transactions, they demonstrated that kcal labelling implementation was associated with a reduction of 54 kcals per transaction31.
Kcal labelling in the OHFS could lead to a reduction in kcal consumption by influencing individuals’ food choices24,25,26,27,28,29 and through menu reformulation24. In addition, changes in consumer behaviour following the implementation of kcal labelling may be mediated by the level of existing knowledge of the kcal content of menu items in the general population, which may explain varying associations and impacts of kcal labelling in different populations and settings. For example, kcal labelling may have a greater impact on food choices if knowledge of kcal content of OHFS foods is poorer and could also have differing effects depending on whether menu items’ energy content tends to be under- or overestimated. Moreover, it may be the case that people somewhat randomly under- or overestimate the number of kcals in food items. For example, people may underestimate for the least healthy foods but overestimate for the healthiest foods or vice versa. If this is the case, the impact of kcal labelling could be influenced by the consumers’ original assumption of the number of kcals in the food item. Depending on this assumption, kcal labelling may lead to fewer or more kcals purchased by consumers.
So far, there has been no examination of whether the introduction of mandatory kcal labelling in England was associated with a reduction in the amount of energy purchased or consumed from the OHFS. Understanding whether the effects of the introduction of mandatory kcal labelling in the OHFS may differ by population socio-demographics will also be critical to understanding its potential to narrow or widen health inequalities.
This study examined energy purchased and consumed by customers in the OHFS pre- versus post-implementation of mandatory kcal labelling legislation in England. This study also examined whether customer estimation of energy content of their purchases, self-reported noticing and the use of kcal information differed pre- versus post-policy implementation.
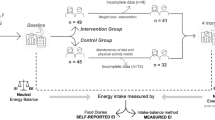
Characteristics of the sampled outlets are reported in Table 1. N = 6,578 participants were recruited, n = 3,308 pre-implementation and n = 3,270 post-implementation (Fig. 1). Across both timepoints, recruited participants were of a similar mean age and a comparable distribution of gender and ethnicity. It should be noted that there was a higher proportion of patients with lower socio-economic position (SEP) in the pre-implementation sample compared with post-implementation. Participant sample information is reported in Table 2. Approximately 28% of participants were recruited from pubs, 25% from restaurants, 24% from fast-food outlets, 20% from cafes and 3% from entertainment venues both pre- and post-implementation.
Kcals purchased and consumed
At pre-implementation, a mean (M) of 1,007 kcals (standard deviation (s.d.) 630) and 909 kcal (s.d. 547) were purchased and consumed per customer, respectively. This was a smaller number of kcals compared with post-implementation (purchased M = 1,081 kcals, s.d. 650, consumed M = 983 kcals, s.d. 587). In adjusted models, there were no significant associations between time and kcals purchased (difference pre versus post, Beta (B) = 11.31, P = 0.564, 95% confidence interval (CI) −27.15 to 49.77)) or the number of kcals consumed (B = 18.51, P = 0.279, 95% CI −15.01 to 3,852.03) (Table 3). Bayes factors in unadjusted models demonstrated strong support for the null hypothesis for kcals purchased (BF01 of 546.51) and consumed (BF01 of 5,309.00). In supplementary models (Supplementary Information), there were no significant interactions between time and participant demographics ((1) SEP, (2) age, (3) gender and (4) ethnicity).
There were variations in the amount of kcal purchased and consumed based on participant demographics. Younger adults purchased more kcals than older adults (B = −1.18, P = 0.016, 95% CI −2.14 to −0.22), males purchased (B = 106.62, P < 0.001, 95% CI 76.76 to 136.48) and consumed (B = 133.47, P < 0.001, 95% CI 105.80 to 161.15) more than females and participants from a non-white ethnic background purchased (B = −58.31, P = 0.011, 95% CI −103.16 to −13.46) and consumed (B = −50.45, P = 0.010, 95% CI −88.16 to −12.30) less than those from a white ethnic background. Time of day (more kcals purchased for an evening meal) (B = 156.01, P < 0.001, 95% CI 222.99 to 89.04) and day of the week (more kcals purchased at weekends) (B = 99.59, P < 0.001, 95% CI 37.48 to 161.71) also was associated with the number of kcals purchased and consumed. Compared with cafes, people visiting pubs, restaurants and fast-food outlets purchased and consumed more kcals on average (Table 3).
Participant kcal estimates
Across both timepoints, customers underestimated the number of kcals in their purchases. The amount of kcal underestimation reduced from pre- (247 kcals) to post-implementation (217 kcals) by 30 kcals in unadjusted analyses, with Bayes factors indicating support for the null hypothesis (BF01 of 8.76). Consistent with this in the adjusted models, kcal underestimation reduced post- versus pre-implementation (B = 61.21, P = 0.002, 95% CI 21.57 to 100.86) (Table 3). Age (younger adults underestimated less) (B = −1.10, P = 0.028, 95% CI −2.09 to −0.12), ethnicity (white participants underestimated less) (B = −48.51, P = 0.018, 95% CI −88.67 to −8.35) and SEP (high SEP underestimated less) (B = −107.71, P < 0.001, 95% CI −146.75 to −68.67) were associated with accuracy of kcal estimates. Compared with cafes, participants showed greater underestimation of kcal amounts from purchasing from restaurants (B = 300.15, P < 0.001, 95% CI 233.57 to 366.73) and fast-food outlets (B = 211.18, P < 0.001, 95% CI 163.72 to 258.63) (Table 3).
Noticing and use of kcal labelling
In total, 16.5% (n = 402) of participants reported noticing kcal labelling pre-implementation whereas 31.8% (n = 959) reported noticing labelling post-implementation. Noticing kcal information was significantly higher post- versus pre-implementation (odds ratio 2.25, P < 0.001, 95% CI 1.84 to 2.73, BF01 <0.001, indicative of strong evidence against the null hypothesis) (Table 4). Of the people who reported noticing kcal labelling, 19% (n = 77) reported using kcal labelling to make their purchasing decision pre-implementation and 22% (n = 209) post-implementation. In the adjusted model, there was an association between time and reported use of kcal labelling (77/3,308 pre-implementation and 209/3,270 post-implementation) (odds ratio 2.15, P < 0.001, 95% CI 1.62 to 2.85) (Table 4). Of the people who reported using the kcal information, the majority of individuals, n = 249 (87%), reported using it to select lower-kcal options. For participant demographics, older adults noticed kcal labels more than younger adults but there was no significant difference in reported use. Gender and SEP influenced reported kcal noticing and use, with females reporting noticing and using kcal labels more than males and people from a high SEP reporting noticing and using labels more than those from a lower SEP. Participants were more likely to report noticing kcal labels when purchasing meals from a pub compared with a cafe, this may be due to variations in purchasing conditions such as displaying of kcal information and time spent viewing menus (for instance, in a cafe one often orders food and beverages together, whereas in a pub often one orders a drink first and then considers the food menu at a more leisurely pace). Participants were also more likely to report noticing kcal labels in outlets located in less affluent areas (IMD1) compared with more affluent areas (IMD5) (Table 4).
Discussion
Statement of principal findings
The current study did not observe an association between kcals purchased or consumed in OHFS pre-implementation (2021) versus post-implementation (2022) of mandatory kcal labelling legislation in England (adjusted models). Additional analyses indicated that the lack of observed change did not differ on the basis of participant age, gender, ethnicity or SEP (education level). Reported noticing of kcal labelling post-implementation significantly increased, and customers more accurately estimated the kcal content of their purchases at post- versus pre-implementation. Despite this, there was only a small change in reported use of kcal labelling pre- versus post-implementation (77/3,308 pre-implementation and 209/3,270 post-implementation).
Strengths and weaknesses of the study
This study examined purchasing, consumption and noticing and use of kcal labelling in the OHFS in England before versus after implementation of the national mandatory kcal labelling policy. This study recruited a large number of participants from a range of food outlets across multiple local authorities and area-level deprivation quintiles. Local authorities were purposively sampled to be generalizable across other areas of England and included outlets representing a large number of national chains.
A limitation of this study is the reliance on self-reporting of food purchased and consumed, which may introduce bias32. To mitigate inaccurate reporting, food purchases were recorded shortly after consumption and, where possible, customer receipts were used to verify purchases, although this was not always possible due to not being consistently issued by outlets. The calculation of kcals purchased was based on businesses’ reported kcal information for menu items. Previous research has indicated that this tends to be accurate but may be prone to underestimation of the energy content of some food items33,34; for example, one study found that kcal counts on menus were generally accurate, but restaurants underreported compared with fast food outlets34. We are not aware of any evidence suggesting that the accuracy of kcal information has changed over time, and so we presume this limitation is unlikely to introduce bias to the present results in relation to change estimates; however, kcal purchasing and consumption may be underestimated in this study. The use of objective verified measures of energy purchased and consumed would be preferable but was not feasible in this real-world policy evaluation. Further, it may be the case that people who were approached to take part in the study and declined may have purchased and consumed meals with a higher or lower energy content than participants sampled. Due to this, the data presented could be an underestimation or overestimation of the number of kcals purchased and consumed by people in the OHFS. However, there are no a priori reasons to expect this variance to be systematically different between pre- and post-policy implementation and, thus, not introducing substantial bias.
Although our study can conclude that the implementation of the policy was not associated with an immediate change in energy purchased and consumed, we cannot infer causality from a pre–post design owing to the inability to fully adjust for known and unknown confounders or compare data with any background trends (for example, pre-implementation data were collected shortly after coronavirus disease 2019 restrictions were removed in England).
Previous research has examined consumer behaviour changes following the implementation of kcal labelling in the OHFS; however, this has predominately been done in North America35. A small number of US studies have suggested that the introduction of kcal labelling was associated with small decreases in energy purchased in two fast food franchises and a supermarket chain selling prepared food31,36,37, but there has been no national evaluation of the US kcal labelling policy. In the United Kingdom, a limited number of trials in real-world settings have found no evidence that the introduction of kcal labelling reduced overall energy purchased38,39. Systematic reviews have produced similar findings, concluding that the quality of evidence is low and that kcal labelling has a small or no effect on the amount of energy selected, purchased and/or consumed25,26,27,28,29. The lack of an observed association between mandatory kcal labelling and energy purchased and consumed in the present study is not consistent with the three US studies described above31,36,37. However, these examined single fast food and supermarket chains (selling prepared food) in the United States, rather than the broad range of eligible OHFS businesses in the present study. In addition, contextual differences between the United States and England may also explain different findings, such as socio-demographic patterning, frequency of OHFS visits and/or food choice motives14.
Research has shown that a notable proportion of individuals do not notice kcal labels when eating out29,40. Larson et al.40 found that, out of 1,830 US adults, only 52.7% were aware of kcal labelling when eating at a restaurant in the past month, with 38.2%, among those who noticed labelling reporting that they did not use it when making their purchase decision. In our study, only around 30% of people post-implementation reported noticing kcal labelling. Of those people, only 22% (209/3,270 across all participants post-implementation) reported that they used this information when making their purchasing decisions. Despite a small increase (3%) in reported usage post-implementation, this may explain the lack of an association with consumer purchasing found in this study. Although there was an increase in participants who reported noticing kcal labelling following mandatory implementation (an increase from 17% to 32%), these figures are still relatively low compared with figures from the United States (for example, 60% noticed kcal labelling)41. Labelling guidance is similar between the United States42 and England. However, a US study examining compliance found that 94% of 197 chains had implemented kcal labelling post-regulations43, which is higher than compliance rates found in the England (80%)44. This greater level of compliance may have contributed to higher reported noticing and use of kcal labels in the United States and may have contributed to lower levels of reported noticing and use of kcal labels in this study. The lower compliance rates found in England44 has potentially limited the effectiveness and impact of the policy on customer noticing and use of kcal labels and, in turn, probably impacts on kcals purchased and consumed.
When making dietary choices, individuals of lower SEP are more likely to report being less motivated by weight management or the healthiness of food14. In our study, people from a lower SEP demonstrated greater underestimation of the energy content of meals purchased and lower reported noticing and use of kcal labelling in individuals from lower SEP. However, there was no evidence that the change in kcals purchased or consumed pre- versus post-implementation differed on the basis of any demographics, including SEP. This is consistent with previous systematic review evidence indicating that the effect of kcal labelling on consumer purchasing and consumption does not differ on the basis of SEP45. It should be noted that, in the current study, SEP was characterized only on the basis of highest education level, and although most appropriate for this study, education level does not consider factors such as generational differences in education opportunities or financial resources46,47.
The kcal content of OHFS meals purchased and consumed in this study was high compared with UK public health recommendations of 600 kcals per meal48. This finding is broadly consistent with previous research that food purchased in the OHFS is high in kcals1,49. Previous research has indicated socio-demographic differences in purchasing and consumption in the OHFS50, and this study observed some of these variations. Consistent with previous research, it was found that males purchased and consumed more than females51, younger adults purchased and consumed more than older age groups52,53, and there were ethnicity variations in purchasing and consumption, with participants from a white ethnic background purchasing and consuming more than those from a non-white ethnic background54.
There were no observed changes in customer purchasing or consumption of energy in the OHFS following the implementation of mandatory kcal labelling in England in the current study. These findings indicate that the current implementation of mandatory kcal labelling legislation is unlikely alone to have substantial impacts on out-of-home eating. However, it may be the case that alongside other policies it may contribute to wider and more substantial impacts on diet and public health. The requirement to provide kcal labelling on OHFS menus in England was introduced alongside other public health policies, such as a tax on sugary soft drinks, restrictions on advertising unhealthy foods and increased funding for physical activity in schools55. The kcal labelling policy alone may not have large impacts on OHFS consumer purchasing, but instead contributes to improved wider public health alongside other policies, especially through the gradual shift of social norms. Future research would benefit from examining the impacts of multiple newly implemented policies and the combined impact of these policies on public health.
Mandatory kcal labelling in the OHFS could lead to a reduction in kcal consumption through two pathways: by influencing individuals’ food choices and through menu reformulation24. The current study did not find a reduction in kcals due to consumer behaviour change. However, the policy may have impacted overall kcal consumption via menu reformulation. A recent study56 examined changes in online menu information from large out-of-home food outlets in England between September 2021 and September 2022, finding a small reduction in mean kcals after the implementation of the kcal labelling policy. This reduction was driven by the removal of higher-kcal menu items and the introduction of lower-kcal menu items. The study found no changes pre- and post-implementation of the policy in kcal content for continuously available items. This indicates that if reductions in population level kcal consumption following the policy have occurred, they may have been more likely to have been driven by menu reformulation rather than consumer behaviour change.
Complementary research examining kcal labelling legislation compliance in OHFS outlets in England pre- versus post-implementation found that, while the provision of labelling increased pre–post, only 80% of sampled OHFS provided kcal labelling post-regulations44. When examining the quality of this labelling it was found that only 15% of outlets met all kcal labelling compliance criteria post-regulations, with a minority of outlets not presenting kcal labelling in a clear (33%) or legible (29%) manner44. A lack of compliance with labelling legislation in outlets may therefore have contributed to the lack of change in energy purchased and consumed observed in the present study. Enforcement of the policy is currently being conducted at a local authority level, with local authorities encouraged to attempt to improve compliance with the food business before issuing a £2,500 fine23. Greater and stricter enforcement of labelling legislation may be required to improve compliance and increase the likelihood that consumers notice and use kcal labelling in the OHFS, which in turn may lead to impacts on customer purchasing and consumption.
A potential barrier to the use of kcal labelling in the OHFS may be a lack of public understanding of the kcal information presented. Research conducted in the United States found that only 64–73% of the general public was able to accurately report daily kcal needs57. Increased awareness and availability of kcal labelling may have helped to improve the public’s knowledge of the kcal content of foods from the OHFS, and this was reflected by more accurate customer kcal estimates post-implementation found in this study. However, public education campaigns about kcal requirements may be required to further increase understanding and, in turn, may increase usage of kcal labelling in the OHFS. Alternatively, additional labelling formats that provide more context and/or define foods as ‘low’, ‘moderate’ or ‘high’ kcals may aid understanding58. These types of nutrition label have shown to be effective on the front of package labels aiming to improve people’s judgements of healthiness of food items59, with traffic light labels leading to the greatest accuracy at identifying healthier food items compared with other labelling types60. Labelling types that provide greater content and guidance may aid understanding and may increase the likelihood of customers selecting healthier food items in OHFS contexts. Future research is required to fully examine the extent of the UK public’s understanding of kcal labelling in the OHFS and if education campaigns and other labelling formats have the potential to promote greater use of kcal information.
As this study included only education as an indicator of SEP, future research would benefit from examining the effects of kcal labelling on consumer behaviour and whether this differs on the basis of multiple indicators of SEP, such as household income.
Conclusions
The current study did not observe a significant decrease in the number of kcals purchased or consumed in OHFS outlets following the introduction of mandatory kcal labelling policy in England. A lack of compliance with labelling legislation found in previous research44 may have contributed to the lack of change in energy purchased and consumed observed in the present study.
Methods
This research complies with all relevant ethical regulations, and ethical approval was granted by the University of Liverpool’s Ethics Committee (project ID 10137). All participants provided informed verbal consent, and participants were offered a £5 shopping voucher for taking part in the study. The study protocol and analysis strategy were pre-registered on Open Science Framework (https://osf.io/pfnm6/).
Study design
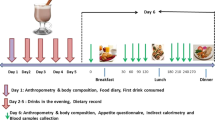
We used a pre-implementation (August to December 2021) versus post-implementation (August to December 2022) observational study design in which we visited OHFS outlets and surveyed customers in four areas of England before and after the introduction date of the mandatory kcal labelling legislation on 6 April 202223.
Outlet sampling procedure
Four local authorities in England were purposively selected for sampling to ensure representation across quintiles of deprivation (assessed using the Index of Multiple Deprivation (IMD)61 at the local authority level) and geographical coverage across the South, North, Midlands and London areas of England. The four local authorities sampled were Liverpool (IMD1 northern region), Dudley (IMD2 midlands), Milton Keynes (IMD3, IMD4 South) and Richmond upon Thames (IMD4, IMD5 London). IMD1 reflects the most deprived areas and IMD5 the least deprived areas defined at the lower layer super output area (LSOA) to better capture small area geographic variations in IMD. Businesses subject to the mandatory kcal labelling policy were identified using the Inter-Departmental Business Register62. This is a list of UK businesses and their core characteristics, including principal activities and the number of employees, used by the government for statistical purposes with the principal activities of businesses defined using Standard Industrial Classification codes. Codes likely to include businesses serving food were identified (see Supplementary Section 1 for the full list of Standard Industrial Classification codes used), and then those that were not large businesses with >250 employees globally were excluded. Within the four local authorities, individual outlets belonging to each identified large business (individual businesses could contribute to multiple outlets, for example, chain restaurants) were identified using Ordnance Survey Points of Interest data from September 202063. Following this, we used stratified random sampling by business type and IMD quintile within each local authority to select outlets for inclusion. Business types were categorized by Ordnance Survey as follows: restaurants; pubs and bars; retail; hotels; cafes; fast food; attractions; and entertainment. Outlets that were found to be closed, not selling food subject to the mandatory kcal labelling policy, or would not permit data collection on visiting at the pre-implementation assessment were replaced by resampling.
Customer exit survey sampling procedure
Exit surveys with customers from sampled outlets were conducted to measure the number of kcals purchased and consumed, kcal knowledge of meal purchases, and self-reported noticing and use of kcal labelling. To be eligible for inclusion, participants were required to have purchased at least one food item from the selected outlet and be aged 16 years or over.
Researchers stood outside the selected food outlets during peak operating times (typically 12:00–21:00, Wednesday to Sunday) and approached all customers as they entered or exited the outlet. Where possible, data collection timepoints (weekend or weekday and evening or midday) were kept consistent across the pre and post data collection periods. Participants completed a short exit survey lasting approximately 5–10 min per participant (survey questions in Supplementary Section 2). Participants were initially told that the study was investigating dining habits to minimize influencing participants’ purchasing behaviour and avoid increasing their focus on kcal labelling. Participants were later debriefed with a full explanation of the study’s aims. Basic demographic information was collected (age, gender, ethnicity and highest education level), with education level used to indicate participants’ SEP (lower SEP: school level qualifications or lower; higher SEP: post-school level qualifications). Participants were asked to estimate the total number of kcals in their purchases. Following this, participants were asked about whether they noticed kcal labelling provided by the outlet (yes/no), whether they used this when making their purchases (yes/no) and, if yes, why (to select lower-kcal options, to select higher-kcal options, other) and how (selected alternative meal option, selected a smaller or larger portion, made a meal substitution or customization). Participants were then asked to report the food and drink items that they purchased from the outlet for their own consumption and to estimate any food that was shared or was not consumed. Self-reporting of shared items and leftovers was used to calculate consumption values for each participant. Whenever possible, customers were asked to provide a receipt to verify purchases; however, many outlets were not issuing receipts during data collection owing to hygiene concerns and procedural changes related to the coronavirus disease 2019 pandemic. Data were collected on the availability and quality of kcal labelling in a subset of food outlets at both pre and post timepoints, with data reported in a recent publication44. The proportion of outlets providing kcal labelling at any point-of-choice increased from pre (21%) to post (80%) policy implementation.
Sample size
The sample size required for customer exit surveys was based on results from a Cochrane review that included 28 studies examining the effect of nutritional labelling on purchasing and consumption30. The sample size was calculated to detect a 47 kcal reduction from a baseline mean of 706 kcal (s.d. 326) purchased per individual (7% reduction) as reported in the Cochrane review. Assuming a modest intra-class correlation of kcals purchased within outlets of 0.39 (ref. 64) and 10 participants per outlet, we estimated required sample sizes of N = 3,440 at pre and post from 344 outlets to detect a 7% reduction in energy purchased or consumed per participant with 80% power at α = 0.05.
Permission from outlets was withheld for data collection in retail, attraction and hotel outlets, resulting in 21 outlets from these categories being excluded from data collection. The sample for pre-implementation consisted of 330 outlets (from 76 unique businesses) including cafes, fast food, pubs, restaurants and entertainment, resulting in a pre-implementation participant sample size of n = 3,308 (approximately 10 people per outlet, with some variations when participants were recruited in groups). At the post-implementation observation, we attempted to conduct surveys at the same outlets sampled pre-implementation. Due to the closure of some of the outlets, five outlets were excluded from the sample (Fig. 1), resulting in a post-implementation participant sample of n = 3270.
Estimation of meal kcal content
The kcal content of each participant’s food and drink purchases was estimated using information from MenuTracker65. MenuTracker is a database of web-scraped nutritional information on menu items in large UK OHFS businesses. Data are collected quarterly, and data from September 2021 were used to calculate kcal content for the pre-implementation data collection and September 2022 for the post-implementation data collection to minimize the effects of seasonal variation on menu items available. Nutritional content was sought from the business’s websites in instances where the kcal content was not available from MenuTracker. In instances where multiple menu item options were available in the database, or the item was not identifiable (for example, if it was unclear which menu item was purchased from the participant’s description), the closest matching item (or mean of items) was used or the item was coded as missing (Supplementary Section 3).
Data exclusions
If the total number of kcals the participant purchased was unavailable or incomplete, they were excluded from the kcal purchased, kcal consumed and kcal estimates primary analyses. However, these participants were retained for the analyses of noticing and use of kcal labelling. The number of exclusions is reported by reason of missing data in Supplementary Section 3.
Data analysis
To examine whether outcome variables differed pre- versus post-implementation, linear and logistic regression were used with time (pre-implementation/post-implementation), age, gender, ethnicity and SEP as demographic adjustment variables and outlet type and outlet ___location IMD (at the LSOA level, calculated from outlet postcode) as outlet adjustment variables, and with robust standard errors to account for clustering by outlet. Time of day (lunch versus dinner) and day (weekday versus weekend) were included as covariates. Analyses were conducted using the ‘estimatr’66 and ‘clubSandwich’67 packages in R version 4.3.1. Outcome variables were number of kcals purchased; number of kcals consumed (adjusting for leftover and items shared estimates); accuracy of customer kcal estimates (customer estimate minus actual kcal amount determined via MenuTracker); and kcal noticing and use (both yes versus no). As meal kcal content could influence the accuracy of customer kcal estimates68, models examining the accuracy of kcal estimates additionally included total kcals purchased. We planned to use local authority as a further variable in models, but this was highly collinear with outlet IMD so it was removed. However, in supplementary analyses (Supplementary Section 5), we replaced IMD with local authority in the models and the results were consistent. When analysing the use of kcal labels, missing values (this question was not asked if participants did not report noticing kcal labels) were coded as ‘did not use’. An α value of 0.05 for statistical significance was used for the main analyses described above. Additional models for kcals purchased and consumed were examined if the effect of time (pre versus post) was moderated by participant demographics by adding interaction terms between time and (1) SEP, (2) age, (3) gender and (4) ethnicity. For these additional analyses including interactions, an α value of 0.01 (99% confidence intervals) was used to determine statistical significance to account for the relatively large number of additional analyses conducted. Bayes factors were computed for unadjusted and unclustered simple models (the association between time and outcomes of kcals purchased and consumed, kcal estimation accuracy and noticing of labels) using the ‘ttestBF’ and ‘contingencyTableBF’ functions from the ‘bayesfactor’ package in R. We tested one-sided hypotheses that kcals purchased and consumed would be lower at post-implementation. We report BF01, in which a value >1 is indicative of support for the null model (absence of evidence for change) over the alternative model (a reduction in kcal purchasing or consumption as post-implementation). The analysis protocol was registered on the Open Science Framework (https://osf.io/pfnm6/) with minor deviations made from the registered protocol reported in Supplementary Section 4. The lead author affirms that this manuscript is an honest, accurate and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data from this study are available on the Open Science Framework at https://osf.io/rva8g/.
Code availability
Analysis code from this study is available on the Open Science Framework at https://osf.io/rva8g/.
References
Robinson, E., Jones, A., Whitelock, V., Mead, B. R. & Haynes, A. (Over)eating out at major UK restaurant chains: observational study of energy content of main meals. BMJ 363, k4982 (2018).
Muc, M. et al. A bit or a lot on the side? Observational study of the energy content of starters, sides and desserts in major UK restaurant chains. BMJ Open 9, e029679 (2019).
Nago, E. S., Lachat, C. K., Dossa, R. A. & Kolsteren, P. W. Association of out-of-home eating with anthropometric changes: a systematic review of prospective studies. Crit. Rev. Food Sci. Nutr. 54, 1103–1116 (2014).
Adams, J. et al. Frequency and socio-demographic correlates of eating meals out and take-away meals at home: cross-sectional analysis of the UK national diet and nutrition survey, waves 1–4 (2008–12). Int. J. Behav. Nutr. Phys. Act. 12, 51 (2015).
Health Survey for England 2017 Adult and Child Overweight and Obesity (National Health Service, 2019).
Meigs, J. B. et al. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J. Clin. Endocrinol. Metab. 91, 2906–2912 (2006).
Bhaskaran, K. et al. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5·24 million UK adults. Lancet 384, 755–765 (2014).
Khan, S. S. et al. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. 3, 280–287 (2018).
Witkam, R. et al. Does body mass index mediate the relationship between socioeconomic position and incident osteoarthritis? Semin. Arthritis Rheum. 56, 152063 (2022).
Qin, B. et al. Body mass index and the risk of rheumatoid arthritis: a systematic review and dose–response meta-analysis. Arthritis Res. Ther. 17, 1–12 (2015).
Statistics on obesity, physical activity and diet, England 2021. National Health Service https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/england-2021 (2021).
Pranata, R. et al. Body mass index and outcome in patients with COVID-19: a dose–response meta-analysis. Diabetes Metab. 47, 101178 (2021).
Obesity profile: short statistical commentary July 2022. Office for Health Improvement & Disparities https://www.gov.uk/government/statistics/obesity-profile-update-july-2022/obesity-profile-short-statistical-commentary-july-2022 (2022).
Robinson, E., Jones, A. & Marty, L. The role of health-based food choice motives in explaining the relationship between lower socioeconomic position and higher BMI in UK and US adults. Int. J. Obes. 46, 1818–1824 (2022).
Cleveland, L. P., Simon, D. & Block, J. P. Compliance in 2017 with Federal Calorie Labeling in 90 chain restaurants and 10 retail food outlets prior to required implementation. Am. J. Public Health 108, 1099–1102 (2018).
Goodman, S., Vanderlee, L., White, C. M. & Hammond, D. A quasi-experimental study of a mandatory calorie-labelling policy in restaurants: Impact on use of nutrition information among youth and young adults in Canada. Prevent. Med. 116, 166–172 (2018).
Public Health Responsibility Deal (Department of Health & Social Care, 2011).
Jebb, S. A. Calorie labelling on the high street. BMJ 343, d4502 (2011).
Robinson, E., Burton, S., Gough, T., Jones, A. & Haynes, A. Point of choice kilocalorie labelling in the UK eating out of home sector: a descriptive study of major chains. BMC Public Health 19, 1–6 (2019).
Impact assessment: mandatory calorie labelling in the out-of-home sector. Department of Health & Social Care https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/992872/calorie-labelling-impact-assessment.pdf (2020).
Tackling Obesity: Empowering Adults and Children to Live Healthier Lives (Department of Health & Social Care, 2020).
New calorie labelling rules come into force to improve nation’s health 2022. Department of Health & Social Care https://www.gov.uk/government/news/new-calorie-labelling-rules-come-into-force-to-improve-nations-health#:~:text=New%20legislation%20applying%20to%20large,comes%20into%20force%20on%20today.&text=New%20rules%20requiring%20calorie%20information (2022).
The Calorie Labelling (Out of Home Sector) (England) Regulations 2021. Department of Health & Social Care https://www.legislation.gov.uk/uksi/2021/909/contents/made (2021).
Grummon, A. H. et al. Changes in calorie content of menu items at large chain restaurants after implementation of calorie labels. JAMA Netw. Open. 4, e2141353 (2021).
Kiszko, K. M., Martinez, O. D., Abrams, C. & Elbel, B. The influence of calorie labeling on food orders and consumption: a review of the literature. J. Commun. Health 39, 1248–1269 (2014).
Long, M. W., Tobias, D. K., Cradock, A. L., Batchelder, H. & Gortmaker, S. L. Systematic review and meta-analysis of the impact of restaurant menu calorie labeling. Am. J. Public Health 105, e11–e24 (2015).
VanEpps, E. M., Roberto, C. A., Park, S., Economos, C. D. & Bleich, S. N. Restaurant menu labeling policy: review of evidence and controversies. Curr. Obes. Rep. 5, 72–80 (2016).
Bleich, S. N. et al. A systematic review of calorie labeling and modified calorie labeling interventions: impact on consumer and restaurant behavior. Obesity 25, 2018–2044 (2017).
Cantu-Jungles, T. M., McCormack, L. A., Slaven, J. E., Slebodnik, M. & Eicher-Miller, H. A. A meta-analysis to determine the impact of restaurant menu labeling on calories and nutrients (ordered or consumed) in U.S. adults. Nutrients https://doi.org/10.3390/nu9101088 (2017).
Crockett, R. A. et al. Nutritional labelling for healthier food or non-alcoholic drink purchasing and consumption. Cochrane Database Syst. Rev. 2, Cd009315 (2018).
Petimar, J. et al. Changes in the calorie and nutrient content of purchased fast food meals after calorie menu labeling: a natural experiment. PLoS Med. 18, e1003714 (2021).
Cook, A., Pryer, J. & Shetty, P. The problem of accuracy in dietary surveys. Analysis of the over 65 UK National Diet and Nutrition Survey. J. Epidemiol. Commun. Health 54, 611–616 (2000).
Urban, L. E. et al. The accuracy of stated energy contents of reduced-energy, commercially prepared foods. J. Am. Diet. Assoc. 110, 116–123 (2010).
Urban, L. E., McCrory, M. A. & Dallal, G. E. Calorie counts posted by restaurants are generally accurate; sit-down restaurants underreport compared with fast food. JCOM 18, 392–395 (2011).
Vadiveloo, M. K., Dixon, L. B. & Elbel, B. Consumer purchasing patterns in response to calorie labeling legislation in New York City. Int. J. Behav. Nutr. Phys. Act. 8, 1–9 (2011).
Petimar, J. et al. Assessment of calories purchased after calorie labeling of prepared foods in a large supermarket chain. JAMA Intern. Med. 182, 965–973 (2022).
Rummo, P. E. et al. Menu labeling and calories purchased in restaurants in a US national fast food chain. JAMA Netw. Open 6, e2346851 (2023).
Vasiljevic, M. et al. Impact of calorie labelling in worksite cafeterias: a stepped wedge randomised controlled pilot trial. Int. J. Behav. Nutr. Phys. Act. 15, 1–2 (2018).
Vasiljevic, M. et al. What is the impact of increasing the prominence of calorie labelling? A stepped wedge randomised controlled pilot trial in worksite cafeterias. Appetite 141, 104304 (2019).
Larson, N., Haynos, A. F., Roberto, C. A., Loth, K. A. & Neumark-Sztainer, D. Calorie labels on the restaurant menu: is the use of weight-control behaviors related to ordering decisions? J. Acad. Nutr. Diet. 118, 399–408 (2018).
Green, J. E., Brown, A. G. & Ohri-Vachaspati, P. Sociodemographic disparities among fast-food restaurant customers who notice and use calorie menu labels. J. Acad. Nutr. Diet. 115, 1093–1101 (2015).
Food labeling; nutrition labeling of standard menu items in restaurants and similar retail food establishments. Federal Register https://www.federalregister.gov/documents/2014/12/01/2014-27833/food-labeling-nutrition-labeling-of-standard-menu-items-in-restaurants-and-similar-retail-food (2014).
Cleveland, L. P., Simon, D. & Block, J. P. Federal calorie labelling compliance at US chain restaurants. Obes. Sci. Pract. 6, 207–214 (2020).
Polden, M. et al. Point-of-choice kilocalorie labelling practices in large, out-of-home food businesses: a preobservational versus post observational study of labelling practices following implementation of The Calorie Labelling (Out of Home Sector) (England) Regulations 2021. BMJ Open 14, e080405 (2024).
Robinson, E. et al. Socioeconomic position and the effect of energy labelling on consumer behaviour: a systematic review and meta-analysis. Int J. Behav. Nutr. Phys. Act. 20, 10 (2023).
Galobardes, B., Shaw, M., Lawlor, D. A. & Lynch, J. W. Indicators of socioeconomic position (part 1). J. Epidemiol. Commun. Health 60, 7–12 (2006).
Galobardes, B., Shaw, M., Lawlor, D. A. & Lynch, J. W. Indicators of socioeconomic position (part 2). J. Epidemiol. Commun. Health 60, 95 (2006).
Calorie reduction: the scope and ambition. Public Health England https://www.gov.uk/government/publications/calorie-reduction-the-scope-and-ambition-for-action (2018).
Roberts, K., Cade, J., Dawson, J. & Holdsworth, M. Empirically derived dietary patterns in UK adults are associated with sociodemographic characteristics, lifestyle, and diet quality. Nutrients 10, 177 (2018).
Polden, M. et al. Kilocalorie labelling in the out-of-home sector: an observational study of business practices and consumer behaviour prior to implementation of the mandatory calorie labelling policy in England, 2022. BMC Public Health 23, 1–2 (2023).
Orfanos, P. et al. Eating out of home and its correlates in 10 European countries. The European prospective investigation into Cancer and Nutrition (EPIC) study. Public Health Nutr. 10, 1515–1525 (2007).
Kearney, J. M., Hulshof, K. F. & Gibney, M. J. Eating patterns—temporal distribution, converging and diverging foods, meals eaten inside and outside of the home—implications for developing FBDG. Public Health Nutr. 4, 693–698 (2001).
O’Dwyer, N. A., Gibney, M. J., Burke, S. J. & McCarthy, S. N. The influence of eating ___location on nutrient intakes in Irish adults: implications for developing food-based dietary guidelines. Public Health Nutr. 8, 258–265 (2005).
Kant, A. K. & Graubard, B. I. Eating out in America, 1987–2000: trends and nutritional correlates. Prevent. Med. 38, 243–249 (2004).
Balogun, B., Powell, T., Barker, C. & Long, R. Obesity policy in England. House of Commons Library https://commonslibrary.parliament.uk/research-briefings/cbp-9049/ (2023).
Essman, M. et al. Changes in energy content of menu items at out-of-home food outlets in England after calorie labelling policy implementation: a pre-post analysis (2021-2022). Preprint at medRxiv https://doi.org/10.1101/2024.08.09.24311741 (2024).
Krukowski, R. A., Harvey-Berino, J., Kolodinsky, J., Narsana, R. T. & DeSisto, T. P. Consumers may not use or understand calorie labeling in restaurants. J. Am. Diet. Assoc. 106, 917–920 (2006).
VanEpps, E. M., Downs, J. S. & Loewenstein, G. Calorie label formats: using numeric and traffic light calorie labels to reduce lunch calories. J. Public Policy Mark. 35, 26–36 (2016).
Vanderlee, L. et al. The efficacy of ‘high in’ warning labels, health star and traffic light front-of-package labelling: an online randomised control trial. Public Health Nutr. 24, 62–74 (2021).
Findling, M. T. et al. Comparing five front-of-pack nutrition labels’ influence on consumers’ perceptions and purchase intentions. Prevent. Med. 106, 114–121 (2018).
English indices of deprivation. National Statistics https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (2019).
Evans, P. & Welpton, R. Business Structure Database: The Inter-Departmental Business Register (IDBR) for Research. Econ. Labour Mark. Rev. 3, 71–75 (2009).
Points of interest: technical information. Ordnance Survey. https://beta.ordnancesurvey.co.uk/products/points-of-interest (2020).
Vartanian, L. R., Spanos, S., Herman, C. P. & Polivy, J. Modeling of food intake: a meta-analytic review. Soc. Influence 10, 119–136 (2015).
Huang, Y. et al. Monitoring the nutrient composition of food prepared out-of-home in the United Kingdom: database development and case study. JMIR Public Health Surveill. 8, e39033 (2022).
Blair, G. estimatr: fast estimators for design-based inference. R package version 030 (R Foundation for Statistical Computing, 2021).
Pustejovsky, J. clubSandwich: cluster-robust (sandwich) variance estimators with small-sample corrections. R package version 0.5.10 (R Foundation for Statistical Computing, 2017).
Chandon, P. & Wansink, B. Is obesity caused by calorie underestimation? A psychophysical model of meal size estimation. J. Mark. Res. 44, 84–99 (2007).
Acknowledgements
This project is funded by the National Institute for Health and Care Research (Implementation and assessment of mandatory kcal labelling in the out-of-home sector, NIHR200689). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. J.A., T.B., T.R.P.B., M.E., S.J.S. and M.W. are supported by the MRC Epidemiology Unit, University of Cambridge (UKRI grant number MC/UU/00006/7). M.P. receives support from the NIHR Applied Research Collaboration ARC NWC and Alzheimer’s Society and is funded through a Post-Doctoral Fellowship. E.R. is funded by the National Institute for Health and Care Research (NIHR) Oxford Health Biomedical Research Centre (BRC), Economic and Social Research Council (ES/W007932/1) and European Research Council (grant reference PIDS, 803194). The views expressed are those of the authors and not necessarily those of the funders, NHS or Department of Health and Social Care. For the purpose of open access, we have applied a Creative Commons Attribution (CC BY) licence to any author accepted manuscript version arising.
Author information
Authors and Affiliations
Contributions
Funding was obtained by J.A., E.R., A.J., M.W., R.S., T.B., T.R.P.B. and S.J.S. Conceptualization and methodology design contributions and project administration contributions were made by J.A., E.R., A.J., M.W., R.S., T.B., T.R.P.B., S.J.S., M.E. and M.P. The formal analysis, data curation and original draft preparation contributions were made by M.P., E.R. and A.J. All authors contributed to revising the manuscript. All authors read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Human Behaviour thanks Amanda Daley, Eric Finkelstein and Jessica Packer for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Tables and Information.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Polden, M., Jones, A., Essman, M. et al. Evaluating the association between the introduction of mandatory calorie labelling and energy consumed using observational data from the out-of-home food sector in England. Nat Hum Behav 9, 277–286 (2025). https://doi.org/10.1038/s41562-024-02032-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41562-024-02032-1