Abstract
The classification of steatotic liver disease (SLD) has evolved, incorporating all conditions characterized by hepatic lipid accumulation. SLD represents a continuum of disorders that are shaped by the dynamic factors of alcohol intake and cardiometabolic risk factors. This updated classification has profound implications for both the management and research of SLD, especially with the new distinct category of patients with both metabolic and alcohol-related liver disease. In this Perspective, we highlight the pivotal role of alcohol within the SLD framework. We introduce the ‘SLD burden paradox’: a concept illustrating the disparity in which metabolic dysfunction-associated steatotic liver disease is more prevalent, yet individuals with SLD and excessive alcohol intake (such as in metabolic and alcohol-related liver disease and in alcohol-related liver disease) account for greater global liver-related morbidity and mortality. We explore strategies to mitigate the effect of SLD on morbidity and mortality, emphasizing the importance of early detection and reducing stigma associated with alcohol intake. Our discussion extends to methods for assessing and monitoring alcohol intake together with the critical role of managing cardiometabolic risk factors in patients across the SLD spectrum. Conclusively, we advocate for a coordinated care framework that adopts a person-centric approach when managing SLD, aiming to improve outcomes and patient care.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
27,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
209,00 € per year
only 17,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Rinella, M. E. et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J. Hepatol. 79, 1542–1556 (2023).
Ludwig, J., Viggiano, T. R., Mcgill, D. B. & Oh, B. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin. Proc. 55, 434–438 (1980).
Israelsen, M., Torp, N., Johansen, S., Thiele, M. & Krag, A. MetALD: new opportunities to understand the role of alcohol in steatotic liver disease. Lancet Gastroenterol. Hepatol. 8, 866–868 (2023).
Åberg, F., Byrne, C. D., Pirola, C. J., Männistö, V. & Sookoian, S. Alcohol consumption and metabolic syndrome: clinical and epidemiological impact on liver disease. J. Hepatol. 78, 191–206 (2023).
Younossi, Z. M. et al. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology 77, 1335–1347 (2023).
Amonker, S., Houshmand, A., Hinkson, A., Rowe, I. & Parker, R. Prevalence of alcohol-associated liver disease: a systematic review and meta-analysis. Hepatol. Commun. 7, e0133 (2023).
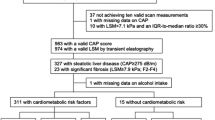
Schneider, C. V. et al. Prevalence of at‐risk MASH, MetALD and alcohol‐associated steatotic liver disease in the general population. Aliment. Pharmacol. Ther. 59, 1271–1281 (2024).
Lee, C.-m et al. Prevalence, distribution, and hepatic fibrosis burden of the different subtypes of steatotic liver disease in primary care settings. Hepatology 79, 1393–1400 (2024).
Kalligeros, M. et al. Prevalence of steatotic liver disease (MASLD, MetALD, and ALD) in the United States: NHANES 2017–2020. Clin. Gastroenterol. Hepatol. 22, 1330–1332.e1334 (2024).
Männistö, V. et al. ALT levels, alcohol use and metabolic risk factors have prognostic relevance for liver-related outcomes in the general population. JHEP Rep. 6, 101172 (2024).
Gu, W. et al. Trends and the course of liver cirrhosis and its complications in Germany: Nationwide population-based study (2005 to 2018). Lancet Reg. Health Eur. 12, 100240 (2022).
Kann, A. E., Jepsen, P., Madsen, L. G., West, J. & Askgaard, G. Cause-specific mortality in patients with alcohol-related liver disease in Denmark: a population-based study. Lancet Gastroenterol. Hepatol. 8, 1028–1034 (2023).
Ekstedt, M. et al. Fibrosis stage is the strongest predictor for disease‐specific mortality in NAFLD after up to 33 years of follow‐up. Hepatology 61, 1547–1554 (2015).
Israelsen, M. et al. Validation of the new nomenclature of steatotic liver disease in patients with a history of excessive alcohol intake: an analysis of data from a prospective cohort study. Lancet Gastroenterol. Hepatol. 9, 409–410 (2024).
Kwak, M. et al. MASLD/MetALD and mortality in individuals with any cardio-metabolic risk factor: a population based study with 26.7 years of follow-up. Hepatology 10, 1097 (2024).
Sripongpun, P., Kaewdech, A., Udompap, P. & Kim, W. R. Characteristics and long-term mortality of individuals with MASLD, MetALD, and ALD, and the utility of SAFE Score. JHEP Rep. 6, 101127 (2024).
Huang, D. Q. et al. Changing global epidemiology of liver cancer from 2010 to 2019: NASH is the fastest growing cause of liver cancer. Cell Metab. 34, 969–977.e962 (2022).
Huang, D. Q., Mathurin, P., Cortez-Pinto, H. & Loomba, R. Global epidemiology of alcohol-associated cirrhosis and HCC: trends, projections and risk factors. Nat. Rev. Gastroenterol. Hepatol. 20, 37–49 (2023).
Younossi, Z. M. et al. The changing epidemiology of adult liver transplantation in the United States in 2013-2022: the dominance of metabolic dysfunction–associated steatotic liver disease and alcohol-associated liver disease. Hepatol. Commun. 8, e0352 (2024).
Åberg, F., Jiang, Z. G., Cortez-Pinto, H. & Männistö, V. Alcohol-associated liver disease–global epidemiology. Hepatology 10, 1097 (2024).
Ochoa-Allemant, P. et al. Waitlisting and liver transplantation for MetALD in the United States: an analysis of the UNOS national registry. Hepatology 10, 1097 (2024).
Scholten, K. et al. You can’t handle the truth! Comparing serum phosphatidylethanol to self-reported alcohol intake in chronic liver disease patients. Dig. Liver Dis. 56, 1215–1219 (2024).
Nasr, P. et al. Misclassified alcohol-related liver disease is common in presumed metabolic dysfunction-associated steatotic liver disease and highly increases risk for future cirrhosis. Clin. Gastroenterol. Hepatol. 22, 1048–1057.e1042 (2024).
Staufer, K. et al. Ethyl glucuronide in hair detects a high rate of harmful alcohol consumption in presumed non-alcoholic fatty liver disease. J. Hepatol. 77, 918–930 (2022).
Hansen, E. D. et al. Quantification of alcohol intake in patients with steatotic liver disease and excessive alcohol intake. JHEP Rep. https://doi.org/10.1016/j.jhepr.2024.101200 (2024).
Louvet, A. et al. Low alcohol consumption influences outcomes in individuals with alcohol-related compensated cirrhosis in a French multicenter cohort. J. Hepatol. 78, 501–512 (2023).
Wong, R. J. et al. Impact of longitudinal alcohol use patterns on long-term risk of cirrhosis among US veterans with steatotic liver disease. Gastroenterology 166, 1156–1165.e4 (2024).
Hofer, B. S. et al. Alcohol abstinence improves prognosis across all stages of portal hypertension in alcohol-related cirrhosis. Clin. Gastroenterol. Hepatol. 21, 2308–2317.e2307 (2023).
Rasmussen, D. N. et al. Prognostic performance of 7 biomarkers compared to liver biopsy in early alcohol-related liver disease. J. Hepatol. 75, 1017–1025 (2021).
Angulo, P. et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology 149, 389–397.e310 (2015).
Mallet, V. et al. Burden of liver disease progression in hospitalized patients with type 2 diabetes mellitus. J. Hepatol. 76, 265–274 (2022).
Griswold, M. G. et al. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 392, 1015–1035 (2018).
Matteoni, C. A. et al. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology 116, 1413–1419 (1999).
Jarvis, H. et al. Does moderate alcohol consumption accelerate the progression of liver disease in NAFLD? A systematic review and narrative synthesis. BMJ Open 12, e049767 (2022).
Magherman, L. et al. Meta‐analysis: the impact of light‐to‐moderate alcohol consumption on progressive non‐alcoholic fatty liver disease. Aliment. Pharmacol. Ther. 57, 820–836 (2023).
Moriya, A. et al. Alcohol consumption appears to protect against non‐alcoholic fatty liver disease. Aliment. Pharmacol. Ther. 33, 378–388 (2011).
Dunn, W. et al. Modest alcohol consumption is associated with decreased prevalence of steatohepatitis in patients with non-alcoholic fatty liver disease (NAFLD). J. Hepatol. 57, 384–391 (2012).
Romero-Gómez, M. et al. in Seminars in Liver Disease (Thieme Medical Publishers, Inc., 2024).
Yeo, Y. H. et al. Alcohol intake thresholds among individuals with steatotic liver disease. JAMA Netw. Open 6, e2347548–e2347548 (2023).
Marti-Aguado, D. et al. Low-to-moderate alcohol consumption is associated with increased fibrosis in individuals with metabolic dysfunction-associated steatotic liver disease. J. Hepatol. https://doi.org/10.1016/j.jhep.2024.06.036 (2024).
Ekstedt, M. et al. Alcohol consumption is associated with progression of hepatic fibrosis in non-alcoholic fatty liver disease. Scand. J. Gastroenterol. 44, 366–374 (2009).
Ajmera, V. et al. Among patients with nonalcoholic fatty liver disease, modest alcohol use is associated with less improvement in histologic steatosis and steatohepatitis. Clin. Gastroenterol. Hepatol. 16, 1511–1520.e1515 (2018).
Roerecke, M. et al. Alcohol consumption and risk of liver cirrhosis: a systematic review and meta-analysis. Am. J. Gastroenterol. 114, 1574–1586 (2019).
Tacke, F. et al. EASL–EASD–EASO Clinical Practice Guidelines on the management of metabolic dysfunction-associated steatotic liver disease (MASLD). J. Hepatol. 81, 492–542 (2024).
Shah, N. D. et al. Alcohol-related liver disease is rarely detected at early stages compared with liver diseases of other etiologies worldwide. Clin. Gastroenterol. Hepatol. 17, 2320–2329.e2312 (2019).
Karlsen, T. H. et al. The EASL–Lancet Liver Commission: protecting the next generation of Europeans against liver disease complications and premature mortality. Lancet 399, 61–116 (2022).
Israelsen, M., Rungratanawanich, W., Thiele, M. & Liangpunsakul, S. Non-invasive tests for alcohol-associated liver disease. Hepatology 10, 1097 (2024).
Thiele, M. et al. Accuracy of the enhanced liver fibrosis test vs FibroTest, elastography, and indirect markers in detection of advanced fibrosis in patients with alcoholic liver disease. Gastroenterology 154, 1369–1379 (2018).
Johnson, A. L. et al. Predicting liver‐related outcomes in people with nonalcoholic fatty liver disease: the prognostic value of noninvasive fibrosis tests. Hepatol. Commun. 6, 728–739 (2022).
Thorhauge, K. H. et al. Using liver stiffness to predict and monitor the risk of decompensation and mortality in patients with alcohol-related liver disease. J. Hepatol. 81, 23–32 (2024).
Avitabile, E. et al. Liver fibrosis screening increases alcohol abstinence. JHEP Rep. 6, 101165 (2024).
Subhani, M. et al. Does knowledge of liver fibrosis affect high-risk drinking behaviour (KLIFAD): an open-label pragmatic feasibility randomised controlled trial. EClinicalMedicine 61, 102069 (2023).
Kjaergaard, M. et al. Screening for fibrosis promotes lifestyle changes: a prospective cohort study in 4796 individuals. Clin. Gastroenterol. Hepatol. 22, 1037–1047.e1039 (2024).
Torp, N. et al. Binge drinking induces an acute burst of markers of hepatic fibrogenesis (PRO‐C3). Liver Int. 42, 92–101 (2022).
Stankevic, E. et al. Binge drinking episode causes acute, specific alterations in systemic and hepatic inflammation‐related markers. Liver Int. 43, 2680–2691 (2023).
Schomerus, G. et al. The stigma of alcohol-related liver disease and its impact on healthcare. J. Hepatol. 77, 516–524 (2022).
Kilian, C. et al. Stigmatization of people with alcohol use disorders: an updated systematic review of population studies. Alcohol. Clin. Exp. Res. 45, 899–911 (2021).
Thursz, M. et al. EASL clinical practice guidelines: management of alcohol-related liver disease. J. Hepatol. 69, 154–181 (2018).
Luoma, J. B. et al. Self-stigma in substance abuse: development of a new measure. J. Psychopathol. Behav. Assess. 35, 223–234 (2013).
Østberg, N., Jacobsen, B. G., Lauridsen, M. M. & Ladegaard Grønkjær, L. Mental health, quality of life, and stigmatization in Danish patients with liver disease. Int. J. Environ. Res. Public Health 20, 5497 (2023).
Bush, K. et al. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch. Intern. Med. 158, 1789–1795 (1998).
Sobell, L. & Sobell, M. in Measuring Alcohol Consumption (eds Litten, R. Z. & Allen, J. P.) 41–72 (Humana Press Inc, 1992).
Stewart, S. H., Koch, D. G., Willner, I. R., Anton, R. F. & Reuben, A. Validation of blood phosphatidylethanol as an alcohol consumption biomarker in patients with chronic liver disease. Alcohol. Clin. Exp. Res. 38, 1706–1711 (2014).
Khanna, S., Shah, N. L. & Argo, C. K. Use of phosphatidylethanol testing in patients with liver disease. Am. J. Gastroenterol. 10, 14309 (2022).
Luginbuhl, M. et al. Consensus for the use of the alcohol biomarker phosphatidylethanol (PEth) for the assessment of abstinence and alcohol consumption in clinical and forensic practice (2022 Consensus of Basel). Drug Test. Anal. 14, 1800–1802 (2022).
Cabezas, J., Lucey, M. R. & Bataller, R. Biomarkers for monitoring alcohol use. Clin. Liver Dis. 8, 59–63 (2016).
Stewart, S. H., Koch, D. G., Willner, I. R., Randall, P. K. & Reuben, A. Hair ethyl glucuronide is highly sensitive and specific for detecting moderate-to-heavy drinking in patients with liver disease. Alcohol Alcohol. 48, 83–87 (2013).
Triolo, V. et al. EtG quantification in hair and different reference cut-offs in relation to various pathologies: a scoping review. Toxics 10, 682 (2022).
Shield, K. D., Parry, C. & Rehm, J. Chronic diseases and conditions related to alcohol use. Alcohol Res. Curr. Rev. 35, 155 (2014).
Kim, D. et al. Changing trends in etiology-based annual mortality from chronic liver disease, from 2007 through 2016. Gastroenterology 155, 1154–1163.e1153 (2018).
Singh, S. P., Panigrahi, S., Mishra, D. & Khatua, C. R. Alcohol-associated liver disease, not hepatitis B, is the major cause of cirrhosis in Asia. J. Hepatol. 70, 1031–1032 (2019).
Asrani, S. K., Devarbhavi, H., Eaton, J. & Kamath, P. S. Burden of liver diseases in the world. J. Hepatol. 70, 151–171 (2019).
Chong, B. et al. Trends and predictions of malnutrition and obesity in 204 countries and territories: an analysis of the Global Burden of Disease Study 2019. EClinicalMedicine 57, 101850 (2023).
Hart, C. L., Morrison, D. S., Batty, G. D., Mitchell, R. J. & Smith, G. D. Effect of body mass index and alcohol consumption on liver disease: analysis of data from two prospective cohort studies. BMJ 340, c1240 (2010).
Israelsen, M. et al. Metabolic and genetic risk factors are the strongest predictors of severity of alcohol-related liver fibrosis. Clin. Gastroenterol. Hepatol. 20, 1784–1794.e1789 (2022).
Åberg, F., Helenius‐Hietala, J., Puukka, P., Färkkilä, M. & Jula, A. Interaction between alcohol consumption and metabolic syndrome in predicting severe liver disease in the general population. Hepatology 67, 2141–2149 (2018).
Åberg, F. et al. Development and validation of a model to predict incident chronic liver disease in the general population: the CLivD score. J. Hepatol. 77, 302–311 (2022).
Kim, H.-s et al. Synergistic associations of PNPLA3 I148M variant, alcohol intake, and obesity with risk of cirrhosis, hepatocellular carcinoma, and mortality. JAMA Netw. Open 5, e2234221–e2234221 (2022).
Romeo, S. et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat. Genet. 40, 1461–1465 (2008).
Ghouse, J. et al. Integrative common and rare variant analyses provide insights into the genetic architecture of liver cirrhosis. Nat. Genet. 56, 827–837 (2024).
Emdin, C. A. et al. Association of genetic variation with cirrhosis: a multi-trait genome-wide association and gene–environment interaction study. Gastroenterology 160, 1620–1633.e1613 (2021).
Ding, C. et al. Binge-pattern alcohol consumption and genetic risk as determinants of alcohol-related liver disease. Nat. Commun. 14, 8041 (2023).
Wyper, G. M. et al. Evaluating the impact of alcohol minimum unit pricing on deaths and hospitalisations in Scotland: a controlled interrupted time series study. Lancet 401, 1361–1370 (2023).
Retat, L. et al. Preventing liver disease with policy measures to tackle alcohol consumption and obesity: the HEPAHEALTH II study. J. Hepatol. 80, 543–552 (2024).
Chang, Y. et al. Alcoholic and non-alcoholic fatty liver disease and associations with coronary artery calcification: evidence from the Kangbuk Samsung Health Study. Gut 68, 1667–1675 (2019).
Chang, W. H., Mueller, S. H., Chung, S.-C., Foster, G. R. & Lai, A. G. Increased burden of cardiovascular disease in people with liver disease: unequal geographical variations, risk factors and excess years of life lost. J. Trans. Med. 20, 1–13 (2022).
Wild, S. H. et al. Cardiovascular disease, cancer, and mortality among people with type 2 diabetes and alcoholic or nonalcoholic fatty liver disease hospital admission. Diabetes Care 41, 341–347 (2018).
Chuong, V. et al. The glucagon-like peptide-1 (GLP-1) analogue semaglutide reduces alcohol drinking and modulates central GABA neurotransmission. JCI Insight 8, e170671 (2023).
Flippo, K. H. et al. FGF21 suppresses alcohol consumption through an amygdalo-striatal circuit. Cell Metab. 34, 317–328.e316 (2022).
Jensen, E. L., Israelsen, M. & Krag, A. Transforming steatotic liver disease management: the emerging role of GLP-1 receptor agonists. Hepatol. Commun. 8, e0561 (2024).
Wang, W. et al. Associations of semaglutide with incidence and recurrence of alcohol use disorder in real-world population. Nat. Commun. 15, 4548 (2024).
Wester, A., Shang, Y., Grip, E. T., Matthews, A. A. & Hagström, H. Glucagon-like peptide-1 receptor agonists and risk of major adverse liver outcomes in patients with chronic liver disease and type 2 diabetes. Gut 73, 835–843 (2024).
Quddos, F. et al. Semaglutide and Tirzepatide reduce alcohol consumption in individuals with obesity. Sci. Rep. 13, 20998 (2023).
Loomba, R. et al. Novel antisense inhibition of diacylglycerol O-acyltransferase 2 for treatment of non-alcoholic fatty liver disease: a multicentre, double-blind, randomised, placebo-controlled phase 2 trial. Lancet Gastroenterol. Hepatol. 5, 829–838 (2020).
Addison, T. Observations on fatty degeneration of the liver. Guys Hosp. Rep. 1, 485 (1836).
von Rokitansky, K. F. in A Manual of Pathological Anatomy (Sydenham Society, 1849).
Eslam, M. et al. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology 158, 1999–2014.e1991 (2020).
Lee, B. P., Dodge, J. L. & Terrault, N. A. National prevalence estimates for steatotic liver disease and subclassifications using consensus nomenclature. Hepatology 79, 666–673 (2024).
Thiele, M. et al. Noninvasive assessment of hepatic decompensation. Hepatology https://doi.org/10.1097/HEP.0000000000000618 (2023).
Sanyal, A. J. et al. Prospective study of outcomes in adults with nonalcoholic fatty liver disease. N. Engl. J. Med. 385, 1559–1569 (2021).
Hansen, C. D. et al. Effect of calorie-unrestricted low-carbohydrate, high-fat diet versus high-carbohydrate, low-fat diet on type 2 diabetes and nonalcoholic fatty liver disease: a randomized controlled trial. Ann. Intern. Med. 176, 10–21 (2023).
Holmer, M. et al. Treatment of NAFLD with intermittent calorie restriction or low-carb high-fat diet–a randomised controlled trial. JHEP Rep. 3, 100256 (2021).
Singal, A. K. et al. Nutritional status of patients with alcoholic cirrhosis undergoing liver transplantation: time trends and impact on survival. Transpl. Int. 26, 788–794 (2013).
Petermann-Rocha, F. et al. Diet modifies the association between alcohol consumption and severe alcohol-related liver disease incidence. Nat. Commun. 15, 6880 (2024).
Chen, V. L. et al. Genetic risk accentuates dietary effects on hepatic steatosis, inflammation and fibrosis in a population-based cohort. J. Hepatol. 81, 379–388 (2024).
Stine, J. G. et al. NASHFit: a randomized controlled trial of an exercise training program to reduce clotting risk in patients with NASH. Hepatology 76, 172–185 (2022).
Houghton, D. et al. Effects of exercise on liver fat and metabolism in alcohol drinkers. Clin. Gastroenterol. Hepatol. 15, 1596–1603.e1593 (2017).
Marjot, T., Ray, D. W., Williams, F. R., Tomlinson, J. W. & Armstrong, M. J. Sleep and liver disease: a bidirectional relationship. Lancet Gastroenterol. Hepatol. 6, 850–863 (2021).
Britton, A., Fat, L. N. & Neligan, A. The association between alcohol consumption and sleep disorders among older people in the general population. Sci. Rep. 10, 5275 (2020).
Swanson, G. R. et al. Night workers with circadian misalignment are susceptible to alcohol-induced intestinal hyperpermeability with social drinking. Am. J. Physiol. Gastrointest. Liver Physiol. 311, G192–G201 (2016).
Jbessone, F., Dirchwolf, M. & Rodil, M. Review article: drug-induced liver injury in the context of nonalcoholic fatty liver diseasea physiopathological and clinical integrated view. Aliment. Pharmacol. Ther. 48, 892–913 (2018).
Krag, A. & Rinella, M. E. Steatotic liver disease: a new name to reflect the combined role of alcohol and metabolic dysfunction. Nat. Med. 30, 933–936 (2024).
Tacke, F., Puengel, T., Loomba, R. & Friedman, S. L. An integrated view of anti-inflammatory and antifibrotic targets for the treatment of NASH. J. Hepatol. 79, 552–566 (2023).
Ratziu, V. et al. Aramchol in patients with nonalcoholic steatohepatitis: a randomized, double-blind, placebo-controlled phase IIb trial. Nat. Med. 27, 1825–1835 (2021).
Harrison, S. A. et al. A phase 3, randomized, controlled trial of resmetirom in NASH with liver fibrosis. N. Engl. J. Med. 390, 497–509 (2024).
Newsome, P. N. et al. A placebo-controlled trial of subcutaneous semaglutide in nonalcoholic steatohepatitis. N. Engl. J. Med. 384, 1113–1124 (2021).
Sanyal, A. J. et al. A phase 2 randomized trial of survodutide in MASH and fibrosis. N. Engl. J. Med. 391, 311–319 (2024).
Simon, T. G., Roelstraete, B., Khalili, H., Hagström, H. & Ludvigsson, J. F. Mortality in biopsy-confirmed nonalcoholic fatty liver disease: results from a nationwide cohort. Gut 70, 1375–1382 (2021).
Israelsen, M. et al. Collagen proportionate area predicts clinical outcomes in patients with alcohol‐related liver disease. Aliment. Pharmacol. Ther. 52, 1728–1739 (2020).
Loomba, R. et al. Combination therapies including cilofexor and firsocostat for bridging fibrosis and cirrhosis attributable to NASH. Hepatology 73, 625–643 (2021).
Villanueva, C. et al. β blockers to prevent decompensation of cirrhosis in patients with clinically significant portal hypertension (PREDESCI): a randomised, double-blind, placebo-controlled, multicentre trial. Lancet 393, 1597–1608 (2019).
Visekruna, A. & Luu, M. The role of short-chain fatty acids and bile acids in intestinal and liver function, inflammation, and carcinogenesis. Front. Cell Dev. Biol. 9, 703218 (2021).
Bernstein, E. Y., Baggett, T. P., Trivedi, S., Herzig, S. J. & Anderson, T. S. Outcomes after initiation of medications for alcohol use disorder at hospital discharge. JAMA Netw. Open 7, e243387–e243387 (2024).
Bergheim, I. et al. Metformin prevents alcohol-induced liver injury in the mouse: critical role of plasminogen activator inhibitor-1. Gastroenterology 130, 2099–2112 (2006).
Kim, R. G., Loomba, R., Prokop, L. J. & Singh, S. Statin use and risk of cirrhosis and related complications in patients with chronic liver diseases: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 15, 1521–1530.e1528 (2017).
Israelsen, M. et al. Rifaximin-α for liver fibrosis in patients with alcohol-related liver disease (GALA-RIF): a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Gastroenterol. Hepatol. 8, 523–532 (2023).
Arab, J. P., Addolorato, G., Mathurin, P. & Thursz, M. R. Alcohol-associated liver disease: integrated management with alcohol use disorder. Clin. Gastroenterol. Hepatol. 21, 2124–2134 (2023).
Mellinger, J. L. et al. Feasibility and early experience of a novel multidisciplinary alcohol-associated liver disease clinic. J. Subst. Abus. Treat. 130, 108396 (2021).
Rumgay, H. et al. Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study. Lancet Oncol. 22, 1071–1080 (2021).
Bagnardi, V. et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose–response meta-analysis. Br. J. Cancer 112, 580–593 (2015).
Aboona, M. B. et al. Mortality outcomes in individuals with MASLD versus MASLD and increased alcohol intake. J. Gastroenterol. Hepatol. https://doi.org/10.1111/jgh.16726 (2024).
Hagström, H., Thiele, M., Roelstraete, B., Söderling, J. & Ludvigsson, J. F. Mortality in biopsy-proven alcohol-related liver disease: a population-based nationwide cohort study of 3453 patients. Gut 70, 170–179 (2021).
Blaney, H. L. et al. Hepatology consultation is associated with decreased early return to alcohol use after discharge from an inpatient alcohol use disorder treatment program. Hepatol. Commun. 8, e0414 (2024).
Acknowledgements
During the preparation of this work, the authors used ChatGTP to improve language and readability. After using this tool/service, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
A.K. has served as speaker for Novo Nordisk, Norgine, Siemens and Nordic Bioscience; participated in advisory boards for Siemens, Boehringer Ingelheim and Novo Nordisk, all outside the submitted work; has received research support from Norgine, Siemens, Nordic Bioscience, Astra and Echosense; and is a board member and co-founder of Evido. N.T. and M.I. declare no competing interests.
Peer review
Peer review information
Nature Reviews Gastroenterology & Hepatology thanks Carolin Schneider, Karn Wijarnpreecha and Fredrik Åberg for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
NCT06409130: https://clinicaltrials.gov/study/NCT06409130
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Torp, N., Israelsen, M. & Krag, A. The steatotic liver disease burden paradox: unravelling the key role of alcohol. Nat Rev Gastroenterol Hepatol 22, 281–292 (2025). https://doi.org/10.1038/s41575-024-01022-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41575-024-01022-y
This article is cited by
-
Impact of steatotic liver diseases on diabetes mellitus risk in patients with atrial fibrillation: a nationwide population study
Cardiovascular Diabetology (2025)
-
Immunopathogenic mechanisms and immunoregulatory therapies in MASLD
Cellular & Molecular Immunology (2025)