Abstract
The response of breast cancer to neoadjuvant chemotherapy (NAC) varies substantially, even when tumours belong to the same molecular or histological subtype1. Here we identify the oestrous cycle as an important contributor to this heterogeneity. In three mouse models of breast cancer, we show reduced responses to NAC when treatment is initiated during the dioestrus stage, when compared with initiation during the oestrus stage. Similar findings were observed in retrospective premenopausal cohorts of human patients. Mechanistically, the dioestrus stage exhibits systemic and localized changes, including (1) an increased number of cells undergoing epithelial-to-mesenchymal transition linked to chemoresistance2,3,4 and (2) decreased tumour vessel diameter, suggesting potential constraints to drug sensitivity and delivery. In addition, an elevated presence of macrophages, previously associated with chemoresistance induction5, characterizes the dioestrus phase. Whereas NAC disrupts the oestrous cycle, this elevated macrophage prevalence persists and depletion of macrophages mitigates the reduced therapy response observed when initiating treatment during dioestrus. Our data collectively demonstrate the oestrous cycle as a crucial infradian rhythm determining chemosensitivity, warranting future clinical studies to exploit optimal treatment initiation timing for enhanced chemotherapy outcomes.
Similar content being viewed by others
Main
The body contains several internal timekeeping clocks to deal with oscillating environmental changes, such as variations in light and temperature. Over a 24 h period, physiological adaptations are orchestrated by the well-documented circadian rhythm6. For cycles exceeding 24 h, the body contains distinct infradian rhythms7. The menstrual cycle—and its murine equivalent, the oestrous cycle—are a typical example of such an infradian rhythm that regulates alternating periods of fertile and non-fertile phases in females. This oestrous/menstrual cycle is regulated by fluctuating hormone levels that are produced by the hypothalamic–pituitary–gonadal axis. These hormonal fluctuations are accompanied by local alterations, such as remodelling of the uterus and mammary tissue, and systemic alterations, such as changes in body temperature, dilation and constriction of blood vessels, and by differences in the immune landscape8,9,10. Internal rhythms that regulate large-scale cyclic alterations enable the body to adapt to internal and external changes, potentially including response to therapies11,12,13,14.
Neoadjuvant chemotherapy (NAC) is currently offered to patients with locally advanced breast cancer (BC) to eliminate potential micrometastases, and to those who would benefit from size reduction of the primary tumour before undergoing breast-conserving surgery1,15. However, the effectiveness of NAC is highly heterogeneous, even for tumours with the same molecular or pathological subtype. This variation led us to explore whether the oestrous/menstrual cycle might partly explain differences in the effectiveness of NAC. During different phases of the menstrual cycle, the epithelium in breast lobules undergoes major histological changes16,17. Analogous morphological changes have been observed in the murine mammary epithelium, including the formation and regression of alveolar buds during the oestrous cycle18,19. Nevertheless, it remains to be determined whether these distinct phases of cellular turnover observed in healthy ducts20,21,22 are maintained in tumours. Moreover, it is unknown whether these local or systemic changes during the oestrous/menstrual cycle can be a source for the observed heterogeneity in response to NAC, and whether they can be leveraged to improve NAC treatment outcomes23.
Oestrous cycle-driven tumour cell turnover
To prepare the healthy murine mammary epithelium for a possible pregnancy, proliferation drives the formation of alveolar buds during the oestrus stage. In the absence of pregnancy, however, these alveolar buds regress following coordinated cell death during the dioestrus stage18,22 (Extended Data Fig. 1a). Previous research showed that this cycle takes 4–6 days and that it can be blocked following ovariectomy24,25 (Extended Data Fig. 1a).
To explore whether mammary tumours exhibit similar cyclic patterns, we studied the behaviour of individual tumour cell clones in the MMTV-PyMT mouse model of invasive BC26 by intravital microscopy (IVM) (Fig. 1a). For visualization of individual clones, we crossed MMTV-PyMT mice with R26-CreERT2het;R26R-Confettihet mice. Following mammary tumour development, individual tumour cells were fluorescently labelled by administration of a low dose of tamoxifen (1.5 mg 25 g−1 body weight), resulting in stochastic Cre-mediated recombination of the confetti cassette in a minority of tumour cells throughout the tumour mass, and subsequent expression of one of the four confetti colours (yellow fluorescent protein, green fluorescent protein, red fluorescent protein and cyan fluorescent protein (CFP)) as an inheritable mark (Extended Data Fig. 1b). Next, a mammary imaging window was implanted over the mammary tumour between 7 and 14 days after confetti colour induction, as described in ref. 27. Using multiday IVM of the same tumour area through the mammary imaging window, we followed individual tumour cell clones over time (Fig. 1a,b). Interestingly, a subset of clones showed synchronized expansion and regression (Fig. 1c and Extended Data Fig. 1c). To test whether this synchronous expansion and regression mirrored the oestrous cycle-dependent growth and regression patterns occurring in the disease-free mammary gland, we impeded the oestrous cycle by ovariectomy. As anticipated, this procedure decreased the coordinated phases of expansion and regression of tumour cell clones (Fig. 1c,d and Extended Data Fig. 1c). These findings suggest that the specific oestrous cycle-dependent cellular turnover identified in disease-free ducts is, to a certain extent, conserved within mammary tumours.
a, Schematic representation of multiday IVM set-up (left), with representative overview images (single z-plane) (right) of five mice in the first imaging session (top) and the following imaging session (bottom). Rectangles indicate example clones represented over multiple imaging days shown in b (left). b, Total clone size (number of cells in a clone) (right, top) and clone growth rate (right, bottom) of example clones quantified over time. c, Representative examples of clone growth rate in genetic MMTV-PyMT tumours imaged over multiple days with IVM. Graphs depict all growth rates (graph I) or a selection of clones (graph II) measured in physiologically cycling mice (left) and ovariectomized mice (right). Each line represents a clone, and coloured lines highlight the behaviour of individual clones. d, Violin plots depicting percentage of clones showing synchronized alternating growth rates, as determined by multiday IVM for physiological cycling mice (Ctrl; n = 5 mice) and ovariectomized mice (OVX; n = 4 mice). e,f, Representative immune fluorescent images and quantification of EdU incorporation (e) and expression of PHH3 (f) in genetic MMTV-PyMT mammary tumours during different stages of the oestrous cycle (n = 3 mice per oestrous stage, 14 and 11 individual tumours for EdU and PHH3 staining, respectively). d–f, Thicker lines represent median, thinner lines indicate the 25th and 75th percentiles and dots represent individual tumours. Statistical analysis by two-sided Wilcoxon–Mann–Whitney test (d) or one-sided hypothesis testing using linear mixed-effects model (e,f). *P < 0.05, **P < 0.01. Further details on statistical analysis are provided in Supplementary File 1. Scale bars, 500 µm (a), 100 µm (b,e,f).
To validate these observations using an independent method, we labelled proliferative tumour cells using 4 h pulses of 5-ethynyl-2′-deoxyuridine (EdU), a marker for DNA replication, and phospho-histone H3 (PHH3), a marker for mitosis. We determined oestrus stage by vaginal cytology, as previously established28 (Extended Data Fig. 1d). The accuracy of our staging approach was confirmed by determination of serum progesterone levels in mice at different stages (Extended Data Fig. 1e). On the basis of staging results, we harvested tumours of comparable tumour size at either the oestrus or dioestrus stage. Next, we determined the ___location of proliferative cells within the tumour. In accordance with previous findings in intestinal tumours29, we found that the majority of proliferation occurred at the edges of mammary tumour lobes, and we did not observe spatial differences between different stages of the oestrous cycle (Extended Data Fig. 1f). On the basis of previous IVM experiments, we expect that proliferation in tumour tissues should be higher in the oestrus than in the dioestrus stage, and indeed we observed a significantly increased number of cells that went through S-phase during the oestrus stage when compared with dioestrus (Fig. 1e). We confirmed this result using an independent approach, scoring the mitotic index on the basis of PHH3 staining during the oestrus and dioestrus stages (Fig. 1f). Increased proliferation levels did not correlate with the expression level of the PyMT oncogene (Extended Data Fig. 1g), excluding the possibility that differences in proliferation are caused by heterogeneity in PyMT expression. To further validate these observations in a separate mouse model of BC, we performed similar experiments using the MMTV-Wnt1 mouse model, in which constitutive WNT1 overexpression leads to the formation of tumours resembling invasive BC30. In this model, we observed similar clonal growth and regression patterns by multiday IVM (Extended Data Fig. 2a,b). Furthermore, we found that proliferation levels in WNT1-driven mammary tumours were higher during the oestrus stage compared with dioestrus (Extended Data Fig. 2c).
NAC responses vary during the oestrous cycle
Neoadjuvant chemotherapy is the preferred treatment of choice for locally advanced BC, aimed at elimination of micrometastases and tumour debulking, thereby increasing the likelihood of breast- and axilla-conserving surgery. The established chemotherapeutics, such as anthracyclines (for instance, doxorubicin), cyclophosphamide and carboplatin, are aimed at targeting rapidly proliferating cells31. Therefore, we hypothesized that chemotherapy might be more effective in treating BC during the more proliferative oestrus stage than in dioestrus.
To test this hypothesis, we administered doxorubicin or cyclophosphamide to MMTV-PyMT;MMTV-Cre;R26-LSL-YFP;E-cad-CFP female mice bearing tumours with a cumulative volume of 500–750 mm3. We initiated treatment at either the oestrus or dioestrus stage. Tumours were dissected 2–4 days later, and the level of cell death in these tumours was determined using flow-cytometric analysis (Fig. 2a and Extended Data Fig. 3a). Notably, this analysis showed that treatment with doxorubicin or cyclophosphamide during oestrus resulted in a significantly higher level of cell death when compared with treatment during dioestrus (Fig. 2b), which was corroborated by a marginally significant reduction in tumour burden (Fig. 2c).
a, Experimental set-up; stages: oestrus (O) and dioestrus (D). b,c, Percentage of PI+ tumour cells (b) and change in tumour burden (c). n: ODoxo = 5 mice/30 tumours; DDoxo = 3 mice/22 tumours; OCyclo = 6 mice/47 tumours; DCyclo = 5 mice/40 tumours. d, Experimental set-up. e, Proportion of mice exhibiting physiological or disrupted oestrous cycle following doxorubicin treatment initiated at the indicated stage; n: O = 13, D = 10 mice. f,g, Number of preantral follicles per square millimetre in ovaries (f) and progesterone levels in serum (g) at pretreatment, 7 days following initial treatment and long term (LT) at the endpoint of experiment. Follicle count, n: O0 = 10; O7 = 7; OLT = 4; D0 = 10; D7 = 7; DLT = 8 mice. Hormone measurements, n: O0 = 9; O7 = 10; OLT = 8; D0 = 10; D7 = 7; DLT = 9 mice. h, Left, effect of oxorubicin treatment. Symbols represent mean relative tumour size per mouse; n = 8–9 mice per group, O = 69 and D = 84 tumours at first treatment. Lines represent mean of all tumours, shading represents s.e.m. Treatment effect is shown until the point at which over 40% of mice reached humane endpoint. Middle, fitted growth curves of mixed-effects model representing tumour volume. Right, Kaplan–Meier survival analysis; n: O = 8, D = 9 mice. i. Representative immunofluorescent lung section images, arrows indicate metastatic nodules. j–l, Quantification of macrometastatic nodules (j), tumour volume (k) and time elapsed between first treatment and analysis (l); n = 5 mice. b,c,f,g,j,k, Thicker solid lines represent median, and thinner solid lines the 25th and 75th percentiles. Individual dots represent either a tumour (b) or a mouse (c,f,g,h,j–l). Statistical analysis by either one-sided hypothesis testing using linear mixed-effects model (b), one-sided Wilcoxon–Mann–Whitney (c,j), Kruskal–Wallis (f,g), nonlinear modelling of tumour growth (h, left), a joint model (h, middle), a regression model (h, right) or two-sided Wilcoxon–Mann–Whitney test (k,l). #P < 0.1, *P < 0.05, **P < 0.01, ***P < 0.001. Further details on statistical analysis are provided in Supplementary Files 1 and 2. D0, day 0; NS, not significant; PI, propidium iodide. Scale bars, 2 mm.
We next questioned whether the increased NAC sensitivity observed during the oestrus stage would persist across successive treatments. To this end, we initiated NAC when mice had a cumulative tumour volume of 250–450 mm3 at either the oestrus or dioestrus stage. Mice underwent five consecutive chemotherapy treatments, until either their cumulative tumour volume exceeded 750 mm3 or a single tumour exceeded 350 mm3 (Fig. 2d). Given that chemotherapy often disrupts the oestrous/menstrual cycle32,33,34,35,36,37,38, we first questioned whether this holds true in our experiments. Postchemotherapy vaginal smears showed a disrupted oestrous cycle (presence of abnormal cells, absence of cells, stalling of changes in cycle-specific cells) in the majority of mice (Fig. 2e and Extended Data Fig. 3b). These findings were corroborated by a reduction in preantral follicle count in the ovaries (Fig. 2f and Extended Data Fig. 3c–e), in accordance with previous reports37,38. In addition, we observed a significant reduction in serum progesterone levels, affirming the profound impact of chemotherapy on the mouse reproductive cycle (Fig. 2g). Notably, regardless of the disrupted oestrous cycle, the difference in treatment response was maintained over the long term (Fig. 2h, left). To test for significance, we used a generalized-nested, mixed-effects model on fitted tumour volumes for both oestrus and dioestrus stages, which showed significant separation between phases (Fig. 2h, middle). Moreover, the superior response in mice that instigated NAC treatment during the oestrus phase was also reflected in extended overall survival (Fig. 2h, right). Indeed, in line with a higher response in the primary tumour, metastatic load in the lungs was significantly reduced in mice that began NAC during the oestrus stage compared with those that started treatment during the dioestrus stage (Fig. 2i,j). Important to note here is that primary tumour sizes at endpoint did not differ significantly between oestrous and dioestrous mice, and lungs from the oestrus-initiated treatment group were even analysed at a later time point owing to the extended survival of these mice (Fig. 2k–l). Collectively, these data demonstrate the impact of the oestrous cycle on both the immediate and prolonged NAC response in PyMT tumours.
Reduced NAC response in the dioestrus stage
To explore whether the loss of expression of hormone receptors (oestrogen receptor (ER) and progesterone receptor (PR)) negates the impact of oestrous cycle stage on NAC responses, we conducted parallel experiments in both hormone receptor-positive (MMTV-Wnt1) and hormone receptor-negative (Brca1−/−;Trp53−/−) BC models (Fig. 3a–d). Mirroring our findings in the PyMT tumour model, the hormone receptor-positive MMTV-Wnt1 model showed that mice receiving an initial NAC dose during the oestrus stage demonstrated a sustained enhanced response during successive treatments, when compared with those that began NAC treatment during the dioestrus stage (Fig. 3b). Unexpectedly, we also obtained similar data in the hormone receptor-negative Brca1−/−;Trp53−/− model. Despite minor differences in tumour reduction (Fig. 3d, left and middle), indicative of a good overall response, a significant difference in survival was observed (Fig. 3d, right). This implies that NAC sensitivity tied to the oestrous stage might be independent of hormone receptor expression by tumour cells.
a,c,e,f, Immunohistochemical staining for ER (left) and PR (right), representative of more than five treatment-naive tumours in more than five mice of the genetic MMTV-Wnt1 (a), transplanted Brca1−/−;Trp53−/− (c) and genetic (e) and transplanted MMTV-PyMT (f) models at oestrus (top) and dioestrus (bottom). b,d, Left, treatment effect in transplanted MMTV-Wnt1 (b) and Brca1−/−;Trp53−/− (d) models, represented as tumour size normalized to initial treatment size. Arrows indicate rounds of treatment, lines the tumour means and shading s.e.m. MMTV-Wnt1 model: n = 5–6 mice per group with O = 6 and D = 6 tumours at first treatment. Brca1−/−;Trp53−/− model: n = 6–8 mice per group, with O = 12 and D = 14 tumours at first treatment. Middle, fitted growth curves of mixed-effects model representing tumour volume for transplanted MMTV-Wnt1 (b) and Brca1−/−;Trp53−/− (d) models. Right, Kaplan–Meier curves for MMTV-Wnt1 (b) and Brca1−/−;Trp53−/− (d) mice treated with doxorubicin initiated during oestrus or dioestrus. MMTV-Wnt1: oestrus, n = 6 mice; dioestrus, n = 5 mice; Brca1−/−;Trp53−/−: oestrus, n = 6 mice; dioestrus n = 8 mice. g, Left, treatment effect in transplanted MMTV-PyMT model, represented as tumour size normalized to initial treatment size. Arrows indicate rounds of treatment, lines the tumour means and shading s.e.m.; n = 8–13 mice per group, with O = 25, D = 15 and OVX = 20 tumours at first treatment. Right, fitted growth curves of mixed-effects model representing tumour volume. b,d,g, Left, significance was determined using nonlinear modelling of tumour growth. Treatment effect is shown until over 40% (b,g) or over 20% (d) of mice reached humane endpoint. Response between groups was statistically evaluated using a joint model (b,d,g, middle); survival analysis was performed using a regression model (b,d,g, right). #P < 0.1, *P < 0.05; **P < 0.01. Scale bars, 150 µm.
To test this idea, we performed experiments in a hormone receptor-negative PyMT tumour model by transplanting late-stage PyMT tumour cells into the mammary fat pad of FVB mice. Although PyMT tumours, at their early stages of development, express hormone receptors39, these tumours progressively lose hormone receptor expression during tumour progression (Fig. 3e,f). In line with data from the hormone receptor-negative Brca1−/−;Trp53−/− model, a marked difference in tumour response was observed in transplanted PyMT tumours, depending on whether NAC treatment was started in the oestrus or dioestrus phase (Fig. 3g). This confirms that the influence of the oestrous cycle on NAC responses may be independent of hormone receptor expression. To further challenge this idea, we performed the same experiment in PyMT tumour-bearing ovariectomized mice. Interestingly, NAC outcomes in these ovariectomized mice closely mirrored the effect observed when NAC was initiated during the oestrus stage, and markedly surpassed the treatment response with NAC initiated at the dioestrus stage (Fig. 3g). This observation further reinforces the idea that hormone receptor-mediated proliferation status may not be the main determinant of chemosensitivity. Moreover, in contrast to the notion of increased sensitivity during the oestrus stage, these data suggest that mice in the dioestrus stage may experience reduced chemosensitivity.
Mechanisms of reduced NAC response
We next explored potential mechanisms that can contribute to the reduced sensitivity of NAC when initiated in the dioestrus stage. A rich body of literature describes many factors that can contribute to reduced chemosensitivity, including epithelial-to-mesenchymal transition (EMT)2,3,4 and changes in the tumour microenvironment, specifically the immune landscape5,40,41,42.
To explore whether the EMT state of tumour cells could explain the variation in sensitivity to NAC observed during oestrous cycle stages, we used our previously established EMT fluorescent reporter PyMT mouse model (MMTV-PyMT;MMTV-Cre;R26-LSL-YFP;E-cad-mCFP)43,44. In this model, all cancer cells are fluorescently labelled with yellow fluorescent protein, whereas endogenous E-cadherin (E-cad) is conjugated to monomeric CFP, facilitating the distinction between epithelial (E-cadHI) and mesenchymal (E-cadLO) cancer cell states43. As we have previously shown, E-cadLO cells have a mesenchymal phenotype and expression profile, including increased migratory behaviour and upregulation of mesenchymal markers such as vimentin43,44. Flow-cytometry analyses of treatment-naive tumours derived from this model showed a marked increase in mesenchymal cells (E-cadLO) during the dioestrus stage (Fig. 4a and Extended Data Fig. 3a). Because EMT is well known to lead to chemoresistance2,3,4, this increase might be a pivotal element behind the observed reduced NAC efficacy during the dioestrus stage.
a, Percentage of mesenchymal tumour cells determined in treatment-naive tumours of genetic MMTV-PyMT model at different oestrous cycle stages; n = 3 mice/24 tumours per group. b, Left, imunohistochemical staining for CD31; right, quantified diameter of intratumoural vasculature in treatment-naive genetic MMTV-PyMT tumours during stages of oestrous cycle. n = 3 mice/12 tumours per oestrous stage. c, Left, immunohistochemical staining for F4/80 (left). Quantification of percentage of F4/80+ cells in treatment-naive tumours (middle) or 7 days post treatment (right) in the genetic MMTV-PyMT model at oestrus and dioestrus. n: Opre = 5 mice/21 tumours; Dpre = 7 mice/27 tumours; Opost = 3 mice/12 tumours; Dpost = 3 mice/11 tumours. d, Schematic representation of experimental set-up. e, Immunohistochemical staining of chemotherapy treatment-naive tumours treated with either control antibody (anti-IgG2a) (top, representative of 15 tumours/3 mice) or macrophage depletion antibody (Ab) (anti-CSF1R) (bottom, representative of 21 tumours/5 mice). f,g, Percentage of PI+ tumour cells (f) and tumour volume change compared with baseline (g) for mice receiving control antibody (anti-IgG2a) or macrophage depletion antibody (anti-CSF1R) and treatment with doxorubicin. n: Oa-IgG2a = 6 mice/24 tumours; Da-IgG2a = 6 mice/28 tumours; Oa-CSF1R = 4 mice/17 tumours; Da-CSF1R = 5 mice/21 tumours. a,b,c,f,g, Thicker solid lines represent median, and thinner solid lines the 25th and 75th percentiles. Dots represent either individual tumours (a–c,f) or mice (g). Statistical analysis was performed using a linear mixed-effects model (a,c) or a two-sided (b) or one-sided (f,g) Wilcoxon–Mann–Whitney test. *P < 0.05, **P < 0.01, ***P < 0.001. Further details on statistical analysis are provided in Supplementary File 1. Scale bars, 500 µm (b (left)), 50 µm (b (right), c (right)), 200 µm (c (left), e).
Next, we examined the tumour microenvironment. First, we observed a reduction in blood vessel diameter during the dioestrus stage (Fig. 4b), suggesting potential constraints in drug delivery. Second, during the dioestrus stage, we noted an increased presence of macrophages, but not of T cells, within treatment-naive tumours (Fig. 4c and Extended Data Fig. 4a,b). This relative increase in macrophage presence persisted, even 7 days post treatment when the oestrous cycle was disrupted (Fig. 4c). Given that macrophages can promote tumour drug resistance (reviewed in ref. 5, for example), we explored their potential role in reduced chemotherapy sensitivity during the dioestrus stage by antibody-mediated depletion (Fig. 4d–g and Extended Data Fig. 5). Indeed, macrophage depletion, but not T cell depletion, enhanced therapy responses (that is, chemotherapy-induced cell death and tumour shrinkage) during the dioestrus stage to a level comparable to that during the oestrus stage (Fig. 4f,g and Extended Data Figs. 4c–f and 5).
Collectively, our mouse experiments show that the observed reduced chemosensitivity in the dioestrus stage may be caused by a multitude of systemic and localized oestrous cycle-induced changes. As contributing factors to the observed change in chemosensitivity, we identified a lower number of proliferative cells and reduced vasoconstriction (potentially leading to reduced drug delivery), an increased number of more chemoresistant mesenchymal tumour cells and an increase in macrophage abundance during the dioestrus phase. Importantly, depletion of macrophages led to similar treatment effects in mice treated in both oestrus and dioestrus, indicating that the increased chemoresistance is, at least in part, mediated by their presence. The sustained increase in macrophages following the first treatment in dioestrus explains why the therapy-suppressive phenotype persists even when the physiological oestrous cycle is lost.
Menstrual cycle impacts NAC response in BC
To investigate whether our findings in mouse models of BC translate to the human setting, we performed a retrospective study using patient data from the Antoni van Leeuwenhoek Hospital (Amsterdam) and the multicentre Dutch Breast Cancer Research Group DIRECT trial45. Whereas the oestrous cycle in rodents spans only 4–6 days46, in women it spans approximately 1 month and involves menstruation (that is, a menstrual cycle). During the menstrual cycle, serum levels of the steroid hormone progesterone mark distinct phases: progesterone levels are low during the follicular phase (below 2.2 nmol l−1), rise during the mid-cycle phase (2.2–6.4 nmol l−1) and peak during the luteal phase (above 6.4 nmol l−1)47. Therefore, to investigate potential differential responses at distinct phases of the menstrual cycle, we used progesterone concentrations in biobanked serum as a proxy for different phases of the cycle.
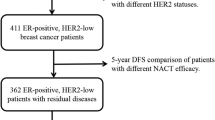
For the first cohort (cohort 1), we selected premenopausal patients (under 50 years of age) with hormone receptor (HR)+ and human epidermal growth factor receptor 2 (HER2)− (HR+HER2−) BC (Fig. 5a). To focus solely on patients with a physiological menstrual cycle, we excluded those using hormonal contraception, pregnant patients and those who had undergone oophorectomy (Fig. 5a). Finally, we selected from these patients only those who had a sufficient amount of serum in the biobank (Fig. 5a). To obtain a reliable estimation of the status of the menstrual cycle at the time of therapy initiation, we included only patients whose serum was biobanked within 5 days preceding NAC. Because individuals in the mid-cycle progress within 1–3 days to the luteal phase, patients in mid-cycle were categorized under the progesterone-high phase. Following these criteria, 17 and 13 patients were determined as having started NAC treatment when progesterone levels were low and high, respectively (Extended Data Fig. 6a). Crucially, known prognostic or predictive factors for NAC response1,15, including age, receptor status, tumour size and tumour grade, showed balanced distribution across both groups (Extended Data Fig. 6b–f). Moreover, lymph node status and type of chemotherapy were similar between groups (Extended Data Table 1).
a, Flowchart of case-selection processes for the HR+HER2− BC cohort (cohort 1) and TNBC cohort (cohort2 ), showing every selection step. b,e, Evaluation of BC treatment response to NAC initiated during the progesterone-low (top) and progesterone-high phase (bottom) in patients with HR+HER2− (b) and TNBC (e), based on Response Evaluation Criteria in Solid Tumours 1.1111 criteria. c,f, Change in size of target lesion post treatment compared with pretreatment, as a percentage, in patients with HR+HER2− BC (c) and TNBC (f). Blue and red represent progesterone-low and -high conditions, respectively. Solid bars indicate patients from the Antoni van Leeuwenhoek Hospital-Netherlands Cancer Institute (AvL-NKI), striped bars indicate patients from the Dutch Breast Cancer Research Group DIRECT study, with data collected at the Clinical Research centre of Leiden University Medical Center (LUMC). Tumour (T), lymph node (N), metastases (M) staging of individual patients is indicated below bars. Dashed lines indicate −30% and +20%, which represent the thresholds for response and progression in HR+HER2− tumours (c); −30% indicates minimal reduction in tumour size for a partial response classification in TNBC (f) based on Response Evaluation Criteria in Solid Tumours 1.1111 guidelines. d,g, Change in primary tumour size following NAC relative to tumour size before treatment, as a percentage in patients with HR+HER2− BC (d) and TNBC (g). HR+HER2−: n = 17 (progesterone-low) and n = 13 (progesterone-high) at first NAC treatment; TNBC: n = 17 (progesterone-low) and n = 8 (progesterone-high) at first NAC treatment. Data shown as violin plots; thicker solid lines represent median, thinner solid lines indicate the 25th and 75th percentiles and dots represent individual patients. Statistical analysis was performed using two-sided Wilcoxon–Mann–Whitney testing. *P < 0.05, **P < 0.01. Further details on statistical analysis are provided in Supplementary File 1.
Notably, similar to our findings of reduced sensitivity of NAC in the dioestrus stage in mouse models, our retrospective analysis showed that progressive and steady disease was more frequently observed among patients starting NAC in the progesterone-high phase compared with those in the progesterone-low phase (Fig. 5b). In addition, partial and complete pathological responses were more prevalent in the progesterone-low group (Fig. 5b). Moreover, we evaluated the reduction of tumour burden by comparing tumour size in pretreatment clinical images with that of residual disease as assessed by pathological evaluation. Similar to our findings in mice, patients in which NAC was initiated during the progesterone-high phase had significantly lower tumour reduction compared with those in which NAC was initiated during the progesterone-low phase (Fig. 5c,d).
Because these data are based on a relatively small patient cohort, we performed a second retrospective study in premenopausal women with a physiological menstrual cycle who were diagnosed with triple-negative breast cancer (TNBC). For this TNBC cohort, we maintained the inclusion and exclusion criteria from the HR+HER2− cohort (cohort 1), resulting in a cohort of 25 patients (cohort 2). Progesterone level assessments classified 17 patients in the progesterone-low phase and eight in the progesterone-high phase during NAC initiation (Extended Data Fig. 6g). Tumour size and grade of this TNBC cohort were similar between the two groups, with a marginally significant increase in age in the progesterone-high group (Extended Data Fig. 6h–l and Extended Data Table 2). In line with the results obtained from mice and the HR+HER2− BC group, the outcomes for patients with TNBC indicate that NAC initiated during the progesterone-high phase was less effective, as evidenced by fewer instances of achieving a pathological complete response and reduced tumour shrinkage, compared with treatment started in the progesterone-low phase (Fig. 5e–g). Together, these data are in line with our mouse data showing that cycle stage is a determinant of sensitivity to NAC.
Discussion
Globally, over 30% of women diagnosed with BC are premenopausal48. Even with a more personalized treatment strategy based on the histopathologic classification of BC, the response to NAC is still highly heterogeneous and challenging to predict49. Our investigation highlights the oestrous/menstrual cycle as an important factor influencing this variability in chemosensitivity among patients with DC. One limitation worth noting is the sample size for our human retrospective studies. Although this may appear modest, it is essential to understand that the studies in the two human cohorts were not designed to deliver clinical conclusions, but acted as a foundational proof of concept, grounded in our findings from three distinct genetic mouse models for BC.
Most chemotherapeutics target rapidly proliferating cells31 and, in line with this idea, we found the best responses when NAC was initiated at the most proliferative stage of the menstrual cycle. However, although most cells in mouse MMTV-PyMT and Brca1−/−;Trp53−/− tumours and human TNBC tumours do not express hormone receptors (Fig. 3)26,30,50, our data demonstrate that the chemosensitivity of these tumours still differs between cycle phases. Clinical studies performed in the 1980s hinted at this and showed increased therapy responses following boosting of BC proliferation by oestrogen administration before chemotherapy treatment; however, this observation could not be confirmed in a larger study cohort51,52. This suggests that hormone receptor-mediated proliferation may not be the only factor determining chemosensitivity. In line with this, the high sensitivity to NAC in ovariectomized mice suggests that mice do not have enhanced NAC sensitivity in the proliferative oestrus stage, but rather exhibit reduced chemosensitivity in the dioestrus stage. What other factors can contribute to this differential sensitivity to NAC? It is important to realize that, although oestrogen and progesterone may be the local executing molecules of the menstrual cycle, the oscillation of their levels is regulated by hormones produced by the hypothalamic–pituitary–gonadal axis. These hormones may have effects independent of, or parallel to, oestrogen and progesterone on chemosensitivity. For example, in addition to oestrogen and progesterone, hormones secreted by the hypothalamic–pituitary–gonadal axis have been suggested to induce systemic changes in the overall immune landscape53,54,55 that may severely affect therapy response. Indeed, our studies particularly pointed to increased macrophage, but not lymphocyte, abundance during the dioestrus stage. This finding is in line with previous studies demonstrating that both the number and spatial distribution of macrophages fluctuate within the disease-free mammary gland during the oestrous cycle, with the highest numbers observed during dioestrus56,57,58. Importantly, increased macrophage abundance persists even following chemotherapy-induced oestrous cycle disruption, contributing to the observed lasting decreased sensitivity to NAC when initial chemotherapy treatment was initiated during the dioestrus stage. This observation is in line with the established role of macrophages in promoting tumour drug resistance5.
In addition to the overall immune landscape, the hypothalamic–pituitary–gonadal axis may also impact therapy response by inducing changes in body temperature, vasodilation or vasoconstriction9,58,59. This adds an additional layer of factors within the tumour macroenvironment that can influence therapy response, because these changes may influence the pharmacokinetics and pharmodynamics of many therapeutics, including their absorption, distribution and metabolism60. In line with this, we observed a decrease in intratumoural blood vessel diameter within mouse tumour samples taken in the dioestrus stage compared with those taken in the oestrus stage, suggesting potential vasoconstriction during the former. Moreover, during dioestrus, our data point to an increase in cells undergoing the EMT process, which has been extensively linked to chemoresistance2,3,4. Our findings, although shedding light on specific mechanisms, also underscore the multifaceted nature of chemotherapy sensitivity, and suggest that the menstrual cycle phase may, in addition to proliferation differences, influence chemosensitivity through a multitude of systemic and localized changes.
Although the physiology of the female body changes substantially during the menstrual cycle, therapies have not been extensively adapted to or optimized for these oscillating physiological changes. Our data warrant investigation in future clinical studies into the menstrual cycle as a factor that influences BC outcome. This is especially relevant if one considers the ‘life years gained’ that can be obtained from treatment at premenopausal age. This insight into the interaction between oestrous/menstrual cycle stages and therapeutic efficacy raises broader questions beyond BC: could there be similar interactions in other diseases influenced by hormonal changes or other physiological rhythms? This exploration might redefine how we approach the treatment of numerous conditions, emphasizing the importance of understanding the body’s natural rhythms and their interplay with medical interventions. For optimization of therapy response, future research should delve deeper into the myriad of mechanisms contributing to NAC sensitivity during different oestrous/menstrual cycle stages. Moreover, prospective clinical trials will be essential to ascertain whether the timing of NAC in relation to the menstrual cycle stage can indeed increase chemotherapeutic efficacy in patients with BC, and potentially in other types of cancer.
Methods
Patient samples
All retrospective medical data/biospecimen studies at the Netherlands Cancer Institute have been executed pursuant to Dutch legislation and international standards. Before 25 May 2018, national legislation on data protection applied, as well as the International Guideline on Good Clinical Practice. From 25 May 2018 we also adhered to the General Data Protection Regulation of the European Union. Within this framework, patients are informed and have always had the opportunity to object or actively consent to the (continued) use of their personal data and biospecimens in research. Hence, the procedures comply both with (inter)national legislative and ethical standards. All retrospective medical data/biospecimens provided by LUMC were part of the DIRECT study (NCT02126449 (ref. 45)), were conducted in accordance with the Declaration of Helsinki (October 2013) and were approved by the Ethics Committee of LUMC in agreement with Dutch law for medical research involving human subjects.
Assessment of HER2 status in this study followed established guidelines, with scoring based on both immunohistochemistry (IHC) and in situ hybridization techniques. Immunohistochemistry results were categorized as 0/1+ (HER2-negative), 2+ (equivocal; considered positive if amplification was detected with in situ hybridization) or 3+ (HER2-positive). Assessment of oestrogen receptor was performed according to Dutch guidelines, with scores of 10% or above considered positive, and those below 10% negative. Pathological complete response (pCR) scoring adhered to local standard guidelines. For one patient, pCR was determined based on radiological images because surgery was not performed due to pCR having been achieved. For measurement of tumour reduction from baseline, we compared pretreatment radiological images with post-treatment residual disease as assessed by pathological evaluation.
Experimental model and subject data
All mice were adult females, housed under a 12/12 h light/dark cycle and under specific-pathogen-free laboratory conditions and received food and water ad libitum. All experiments were approved and performed according to the guidelines of the Animal Welfare Committees of the Royal Dutch Academy for Sciences (Hubrecht Institute), the Netherlands Cancer Institute or KU Leuven. Sample size was not determined a priori. Mice were randomly assigned to experimental groups. All experiments were performed in a blinded manner, except for tumour volume measurement, which was performed by the same investigator who administered chemotherapy treatment, making it impossible to work in a blinded manner.
MMTV-PyMT26 and MMTV-Cre61 mice were purchased from Jackson Laboratory. E-cad-mCFP mice62 were a gift from H. Clevers, R26-loxP-stop-loxP-YFP (R26R-YFP) mice a gift from J. Deschamps and MMTV-Wnt1 (ref. 30) mice a gift from J. Hilkens. MMTV-PyMT;R26R-Confetti;R26-CreERT2 mice62,63, of a mixed BL6/FVB genetic background, were used to label and trace single cells by IVM. Following tumour development, mice were intraperitoneally injected with tamoxifen (Sigma-Aldrich; 1.5 mg 25 g−1, diluted in sunflower oil) to activate Cre recombinase and induce colour randomization of the confetti cassette. MMTV-Wnt1;R26R-Confetti:R26-CreERT2 mice62,63, of a mixed BL6/FVB genetic background, were used to isolate tumour pieces, which were transplanted into NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) female mice (8–12 weeks of age) Following tumour development, mice were intraperitoneally injected with tamoxifen (Sigma-Aldrich; 1.5 mg 25 g−1, diluted in sunflower oil) to activate Cre recombinase and induce colour randomization of the confetti cassette. Staining and treatment experiments in transgenic mice were performed on MMTV-PyMT;MMTV-Cre;R26-LSL-YFP;E-cad-mCFP and MMTV-Wnt1;MMTV-Cre; R26-LSL-YFP;E-cad-mCFP mice of a pure FVB genetic background.
For staining and treatment experiments in transplanted models, tumours from three independent, treatment-naive MMTV-PyMT;MMTV-Cre;R26-LSL-YFP;E-cad-mCFP donors were harvested. Mammary tumours were minced and enzymatically digested by gentle shaking for 30 min at 37 C in digestion mix (0.2% trypsin from bovine pancreas; Sigma) and 0.2% collagenase A (Roche)). The digested tumours were spun down and cell fragments embedded in basal membrane extract (BME) (RGF BME type 2 PathClear). Mammary tumour organoid medium contained DMEM/F12 GlutaMAX (GIBCO), 2% B27 (Invitrogen) and 10 ng ml−1 fibroblast growth factor. Brca1−/−Trp53−/− organoids were a gift from J. Jonkers. Both MMTV-PyMT and Brca1−/−Trp53−/− organoids were orthotopically transplanted into both fourth mammary glands of 8–12-week-old FVB/NRj female mice (Janvier Labs).
For transplantation of MMTV-PyMT organoids, 250,000 single cells were plated 3 days before transplantation. On the day of transplantation, BME was dissolved by mechanical disruption and cells dissolved in 100 μl of BME type 2 (RGF BME type 2 PathClear)/PBS. For transplantation of Brca1−/−Trp53−/− organoids, 10.000 single cells were transplanted in both fourth mammary glands of FVB/NRj mice.
Staging of mice
For determination of the oestrous stage of mice, a vaginal smear was collected and analysed as described in refs. 24,46,64. In short, the vagina was flushed with 50 µl of PBS which was then transferred to a glass slide. Following air drying, the slide was stained with 0.01% crystal violet and oestrus stage determined by examination of cytological characteristics using a light microscope. Mice were categorized as regularly cycling when they showed cycles of length 4–6 days37.
Ovariectomy
In a subgroup of mice, ovariectomy was performed when mammary tumours of volume 50 mm3 could be palpated, after which mice were allowed to recover for at least 7 days before IVM or treatment.
Chemotherapeutic treatment of mice
When tumours had reached a cumulative volume of 500–750 mm3 following short-term treatment, or either 250–450 mm3 (transgenic MMTV-PyMT model) or 50–200 mm3 (transplanted models) for long-term treatment, mice were treated with either vehicle (PBS) or chemotherapeutic—either doxorubicin hydrochloride (5 mg kg−1; catalogue no. D1515, Sigma-Aldrich) or cyclophosphamide monohydrate (100 mg kg−1; catalogue no. C7397, Sigma-Aldrich)—once per week by intravenous injection. Treatment cycles were continued for a maximum of 5 weeks or until the humane endpoint was reached (cumulative tumour load over 750 mm3 or single tumour over 350 mm3). Tumour diameter was measured three times per week by calipers. Following the last treatment cycle, primary tumours and lungs were collected from these mice for further analyses.
Depletion experiments
When mice approached a cumulative tumour volume of 500–750 mm3, they began receiving depletion antibodies at least 1 week before chemotherapeutic treatment and this continued until the end of the experiment. Individual mice were treated every week with either 60 mg kg−1 of either InVivoMAb anti-mouse CSF1R (CD115) monoclonal antibody (BioXCell, clone AFS98, catalogue no. BE0213) or InVivoMAb rat IgG2a isotype control (BioXCell, clone 2A3, catalogue no. BE0089), or received InVivoMAb anti-mouse CD4 (BioXCell, clone GK1.5, catalogue no. BE003-1) and InVivoMAb anti-mouse CD8 (BioXCell, clone YTS 169.4, catalogue no. BP0117), three times per week, every other day, with a first dose of 400 µg followed by 200 µg per antibody.
Mammary imaging window implantation and IVM
To follow in vivo tumour clone dynamics, a mammary imaging window was inserted into tumour-bearing mice 2–3 days following induction of lineage tracing. Mice were anaesthetized using a mixture of 2% isoflurane and compressed air, with surgery performed under aseptic conditions. Before surgery, the skin overlying the tumour was shaved and the skin disinfected using 70% ethanol. An incision was made through the skin overlying the tumour and an imaging window inserted65,66. The imaging window was secured using a non-absorbable, non-woven, purse‐string suture (4‐0 prolene suture) in the skin. For imaging, mice were sedated using isoflurane inhalation anaesthesia (roughly 2.0% isoflurane/compressed air mixture) and received 200 µl of sterile PBS by subcutaneous injection to prevent dehydration. Mice were placed in a custom-designed imaging box on the microscope stage and maintained under constant anaesthesia under the microscope within a temperature-adjusted climate chamber (34.5 °C). Following each imaging session, mice were allowed to recover on a heat mat. Imaging was performed on either an inverted Leica TCS SP5 AOBS multiphoton microscope with a chameleon Ti:Sapphire pumped Optical Parametric Oscillator (Coherent Inc.; www.coherent.com) or a Leica SP8-DIVE confocal microscope equipped with an Insight X3 dual-beam pulsed layer (Spectra Physics; www.spectra-physics.com), equipped with non-descanned detectors. CFP was excited at a wavelength of 840 nm, and yellow fluorescent protein (YFP), green flourescent protein and red flourescent protein at a wavelength of 960 nm. All images were in 12-bit and acquired with a ×25 (HCX IRAPO, numerical aperture 0.95, working distance 2.5 mm) water objective with a free working distance of 2.40 mm. Three-dimensional tile scans of large tumour areas were taken at the indicated time points (at least 5.0 × 5.0 × 0.5 mm3 (x, y, z)) with z-steps of 5–10 µm. Tile scans were collected at regular intervals over time periods of up to 5 weeks following induction of lineage tracing. The same imaging fields were followed during subsequent imaging sessions, using the imaging coordinates of the first imaging session.
Postprocessing and analysis of IVM data
For analysis of three-dimensional tile scans, all intravital images were stitched and processed using Leica Application Suite X software (Leica Microsystems) and ImageJ software (https://imagej.net). Clones were manually annotated in the images, and clone size (number of cells) counted in three dimensions throughout the z-stacks. By following the same clones in our intravital images, we quantified individual clone sizes over time. The fraction of clones that behaved in a synchronized manner with phases of growth, when clones become larger, followed by a phase of regression during which the clones become smaller, was denoted as alternating. To distinguish synchronized clones from non-synchronized in quantitative terms, we identified as synchronized clones those that showed clear, regular alternating phases of growth and regression with the same periodicity, similar to a sinusoidal wave, over multiple consecutive cycles throughout the imaging sessions. By contrast, non-synchronized clones did not exhibit this regular pattern.
Histochemistry and immunohistopathology
Mouse tissues were formalin fixed and paraffin embedded. Haematoxylin and eosin staining was performed on 2 µm sections and IHC staining on 4 µm sections using routine procedures. For IHC staining, antigen retrieval was performed with Tris/EDTA (pH 9.0) (Tris: Sigma, catalogue no. 252859; EDTA: Sigma, catalogue no. EDS) for ER-α (Invitrogen, clone 6F11, catalogue no. MA1-27107, 1:100), CD4 (Invitrogen, clone 4SM95, catalogue no. 14-9766-82, 1:1,000), CD8 (Invitrogen, clone 4SM15, catalogue no. 14-0808-82, 1:2,000), CD31 (Cell Signaling, catalogue no. 77699S, 1:100), F4/80 (Cell Signaling, catalogue no. 70076S, 1:1,000) or citrate buffer (pH 6.0) for progesterone receptor (Fisher Scientific, clone SP2, catalogue no. RM-9102-S1, 1:300). Sections were incubated with primary antibodies overnight at 4 °C. For CD4 and CD8 staining, additional labelling was performed by incubation of goat anti-rat biotin (SouthernBiotech, catalogue no. 3052-08, 1:150) antibody for 30 min at room temperature. Following washing, binding of primary antibody was visualized dependent on species using either the EnVision+ HRP Labelled Polymer anti-rabbit/mouse system (Dako, catalogue nos. K400, K4003 and K4001) or Streptavidin/HRP (Dako, catalogue no. P0397) and the Liquid DAB+ Substrate Chromogen System (Dako, catalogue no. K3468); counterstaining with haaematoxylin was then performed. Slides were digitally processed using a PANNORAMIC 1000 whole-slide scanner (3DHISTECH) and images captured with SlideViewer 2.7 (3DHISTECH). For determination of positive cells, IHC staining was quantified using QuPath 0.4.4 (GitHub) with atomized classifiers.
Immunostaining
Tumour samples were fixed in periodate/lysine/4% paraformaldehyde buffer overnight at 4 °C, incubated in 30% sucrose overnight at 4 °C and embedded in Tissue Freezing medium (Leica Biosystems). Tumours were cryosectioned and immunostaining performed on 10 µm sections. For this, sections were hydrated in PBS for 10 min at room temperature and subsequently blocked and permeabilized for 1 h with 0.5% TritonX/5% normal goat serum (NGS) in PBS. The primary antibody used was anti-PHH3 (Millipore, catalogue no. 06-570, 1:500); the antibody was diluted in 0.1% TritonX/5% NGS in PBS, and tissues were sectioned and stained overnight at 4 °C. Following three washes in PBS, the secondary antibody (donkey anti-rabbit AF568; Invitrogen, catalogue no. A10042, 1:1,000) was incubated for 1 h at room temperature and nuclei stained with TO-PRO-3 (Invitrogen, catalogue no. T3605, 1:5,000). Following three 10 min washes in PBS, stained sections were mounted using VectaShield. All stainings were imaged with an inverted Leica TCS SP8 confocal microscope. Fluorophores were excited as follows: AF594 at 561 nm, YFP at 514 nm and TO-PRO-3 at 633 nm. YFP was collected at 519–555 nm, Alexa-568 at 575–630 nm and TO-PRO-3 at 644–694 nm. All images were collected in 12-bit with a ×25 water-immersion objective (HC FLUOTAR L, numerical aperture 0.95, working distance 2.4 mm). For determination of positive cells, staining was quantified using Fiji/ImageJ v.1.49k and Excel 2016.
EdU detection
EdU was injected intraperitoneally 4 h before mice were killed (1 mg per animal, 5 mg ml−1 stock in PBS; Sigma, catalogue no. 900584). EdU staining was performed on paraffin sections of thickness 10 µm; sections were deparaffinized, and hot target retrieval performed in citrate buffer pH 6.0. EdU was detected by incubation with 100 mM Tris pH 8.5, 1 mM CuSO4, 100 mM ascorbic acid and 10 μM AlexaFluor-488 azide (Invitrogen, catalogue no. A10266) for 30 min at room temperature. Subsequently, DNA counterstaining was performed with TO-PRO-3 (Invitrogen, catalogue no. T3605, 1:5,000) in 0.1% TritonX/5% NGS in PBS for 1 h at room temperature. Following three 10 min washes in PBS, stained sections were mounted using VectaShield. All staining was imaged with an inverted Leica TCS SP8 confocal microscopes. Fluorophores were excited as follows: AF488 at 488 nm and TO-PRO-3 at 633 nm; AF488 was collected at 492–530 nm and TO-PRO-3 at 650–700 nm. All images were collected in 12-bit with a ×25 water-immersion objective (HC FLUOTAR L numerical aperture 0.95 W, VISIR 0.17, FWD 2.4 mm). For determination of positive cells, staining was quantified using semiautomated macros in Fiji/ImageJ v.1.49k and Excel 2016.
Flow-cytometric analysis of dying cells
Mammary tumours were collected separately and minced on ice using sterile scalpels, followed by digestion for depletion experiments in 25 μg ml−1 DNase I (Roche) and 5 Wünsch units TH Liberase ml−1 (Roche) in PBS at 37 C for 35 min, or in 25 μg ml−1 DNase I (Roche) and 3 mg ml−1 collagenase A (Sigma) in PBS at 37 °C for 1 h. The digestion mix was filtered through a 70 µm filter (BD Falcon) while adding DMEM/F12 + GlutaMAX, followed by spinning down for 4 min at 500 relative centrifugal force at 4 °C and resuspension of pellets in 5 mM EDTA/PBS. Cells were washed once in 5 mM EDTA/PBS and centrifuged (4 min at 500 relative centrifugal force at room temperature) before proceeding with antibody labelling. Tumour cells were blocked in fluorescent activated cell-sorting buffer supplied with 20% normal goat serum (Gibco) for 10 min on ice, before labelling with one of the following antibody combinations for depletion experiments: (1) E-cad-eFluor660 (catalogue no. DECMA-1, eBioscience, 1:200), biotin-conjugated anti-mouse CD41 clone eBioMWReg30 (eBioscience, catalogue no. 13-0411-821, 1:200) and anti-mouse CD45 clone 30-F11 (eBioscience, catalogue no. 13-0451-85, 1:200); (2) E-cad-eFluor660 (catalogue no. DECMA-1, eBioscience, 1:200); and (3) anti-mouse CD45-BUV395 clone 30-F11 (BD Bioscience, catalogue no. 564279, 1:200). Secondary labelling was performed using streptavidin-conjugated PerCP (BioLegend, catalogue no. 405213, 1:200). Dead cells were stained using the Apoptosis detection kit PE (Invitrogen, catalogue no. 88-8102-74) according to the manufacturer’s protocol. For depletion experiments no secondary labelling was performed and, following washing, cells were immediately stained with PI and analysed on a Symphony A5 (BD Biosciences) then washed once in 5 nM EDTA/PBS and analysed on a Symphony A5 (BD Biosciences). A broad forward scatter/side scatter (FSC/SSC) gate was followed by gates excluding doublets. Immune cells and megakaryocytes were then excluded, based on staining for CD41 and CD45, in a dump channel. Tumour cells were selected according to YFP positivity and further stringently gated for the presence of the cell death marker annexin and PI, or for PI only for depletion experiments. Data were manually analysed with FlowJo v.10.6.2. Analysis of staining and fluorescent activated cell-sorted samples was pseudomized by number coding.
RNA isolation, complementary DNA preparation and qPCR
RNA was isolated using Trizol reagent (Invitrogen Life Technologies) according to the manufacturer’s protocol. Purity and amount of RNA isolated were analysed using a Nanodrop spectrophotometer. Complementary DNA was prepared using the High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems) according to the manufacturer’s protocol. Sequences of used primers can be found below. Quantitative PCR (qPCR) was performed using Power SYBR Green PCR Master Mix (Applied Biosystems). Thermal cycle conditions used for all qPCR reactions were as follows: 5 min at 95 °C, followed by 40 cycles of denaturation for 30 s at 95 °C, annealing for 30 s at 60 °C and extension for 1 min at 72 °C. PCR reactions were concluded with incubation for 10 min at 72 °C to complete the extension of all synthesized products.
Progesterone assay
To 250 µl serum or calibrator samples was added 10 µl of deuterated internal standard (progesterone-d9, CDN Isotopes). Subsequently, progesterone was extracted with 1 ml of methyl tert-butyl ether and dried using a SpeedVac concentrator. Dried samples were reconstituted in 100 µl of injection solution (methanol:water 2:3, v:v). Thereafter, samples were centrifuged for 5.0 min at 18,213g and 50 µl was injected into a Nexera SIL30ACMP (Shimadzu) autosampler. Chromatographic separation was achieved using a Kinetex EVO 1.7 µm C18 column (2.1 mm, internal diameter 50 mm) (Phenomenex). A gradient protocol of two mobile phases, containing water with 0.1% formic acid and 2 mM ammonium acetate, and methanol, was applied at a flow rate of 0.6 ml min−1. The gradient started at 50% methanol, which was gradually increased to 75% over 2.3 min. Next, the column was washed with 100% methanol for 0.5 min before returning to the starting condition of 50% methanol, for 0.7 min. The assay had a total run time of 3.5 min. Tandem mass spectrometry analysis was performed with a QTRAP6500+ instrument (Sciex) operated in positive electrospray ionization mode (600 °C) and multiple-reaction monitoring mode. For quantitation of progesterone, mass:charge ratio, 315.1 → 97.0 (progesterone) and 324.2 → 100.0 (progesterone-d9) were monitored. The assay is standardized against the NIST SRM 971 standard. In two serum pools containing 1.1 and 27.5 nmol l−1, total coefficient of variation was 9.5 and 7.5%, respectively. The lower limit of quantitation was determined at 0.96 nmol l−1 (coefficient of variation 8.3%) in a serum pool containing low progesterone levels. Analysis of patient samples (sera) was performed blinded, and linked to tumour volume measurements and other clinical parameters only at a later stage.
Statistics and reproducibility
Statistical analyses were performed using R v.4.4.2 (R Development Core Team and the R Foundation for Statistical Computing) by integration of software from open-source packages. For further details on statistics see Supplementary File 1. The level of statistical significance was set at #P < 0.1, *P < 0.05, **P < 0.01, ***P < 0.001. For all violin plots, thicker solid centre lines represent the median, thinner solid lines the 25th and 75th percentiles. Statistical analyses of longitudinal mouse data were performed using R v.4.4.2 (R Development Core Team and the R Foundation for Statistical Computing) by integrating software from open-source packages, including nlme67, JMbayes2 (ref. 68) and packages from tidyverse69, including dplyr, tidyr and ggplot2, and were analysed as follows. Both tumour volume over time and time to event (either end of study or death) were recorded for each individual animal. To test for survival, survival regression (Cox) models were used to test whether survival probability between groups was different. For longitudinal tumour measurements, the mixed-effects model70 was used. Regression splines (natural cubic splines with 2 or 3 degrees of freedom, depending on the case) were used to fit a nonlinear tumour growth function per animal along time, taking into account all separate tumours for each individual animal separately. This model takes the correlated structure of the data into consideration by inclusion of individual animals as a grouping factor, and tumour (within the animal) as a subgrouping factor. Furthermore, the effects of time and treatment were considered as random and fixed effects, respectively. A joint model was used to combine survival and tumour volume measurements, to determine whether the responses together were different between treatment groups. Splines were again used to represent the effect of time. For this model, multiple tumours per animal had their growth curves averaged. For further details on these statistics, see Supplementary File 2.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All statistical analyses are available in Supplementary Files 1 and 2. Source data are provided with this paper.
Code availability
The code generated is available in Supplementary File 1.
References
Haque, W. et al. Response rates and pathologic complete response by breast cancer molecular subtype following neoadjuvant chemotherapy. Breast Cancer Res. Treat. 170, 559–567 (2018).
Bornes, L., Belthier, G. & van Rheenen, J. Epithelial-to-mesenchymal transition in the light of plasticity and hybrid E/M states. J. Clin. Med. 10, 2403 (2021).
Shibue, T. & Weinberg, R. A. EMT, CSCs, and drug resistance: the mechanistic link and clinical implications. Nat. Rev. Clin. Oncol. 14, 611–629 (2017).
Williams, E. D., Gao, D., Redfern, A. & Thompson, E. W. Controversies around epithelial-mesenchymal plasticity in cancer metastasis. Nat. Rev. Cancer 19, 716–732 (2019).
Larionova, I. et al. Interaction of tumor-associated macrophages and cancer chemotherapy. Oncoimmunology 8, 1596004 (2019).
Brown, F. M. & Graeber, R. C. Rhythmic Aspects of Behavior (Lawrence Erlbaum Associates, 1982).
Williams, S. J., Meadows, R. & Coveney, C. M. Desynchronised times? Chronobiology, (bio)medicalisation and the rhythms of life itself. Sociol. Health Illn. 43, 1501–1517 (2021).
Arruvito, L., Sanz, M., Banham, A. H. & Fainboim, L. Expansion of CD4+CD25+ and FOXP3+ regulatory T cells during the follicular phase of the menstrual cycle: implications for human reproduction. J. Immunol. 178, 2572–2578 (2007).
Charkoudian, N. & Stachenfeld, N. Sex hormone effects on autonomic mechanisms of thermoregulation in humans. Auton. Neurosci. 196, 75–80 (2016).
Dasari, P. et al. Hormonal regulation of the cytokine microenvironment in the mammary gland. J. Reprod. Immunol. 106, 58–66 (2014).
Bellet, M. M. et al. The circadian protein PER1 modulates the cellular response to anticancer treatments. Int. J. Mol. Sci. 22, 2974 (2021).
Brolese, E. K. et al. The impact of delivery daytime and seasonality of radiotherapy for head and neck cancer on toxicity burden. Radiother. Oncol. 158, 162–166 (2021).
Redondo, J. A. et al. PER2 circadian oscillation sensitizes esophageal cancer cells to chemotherapy. Biology (Basel) 10, 266 (2021).
Ruan, W., Yuan, X. & Eltzschig, H. K. Circadian rhythm as a therapeutic target. Nat. Rev. Drug Discov. 20, 287–307 (2021).
Masood, S. Neoadjuvant chemotherapy in breast cancers. Womens Health (Lond.) 12, 480–491 (2016).
Atashgaran, V., Wrin, J., Barry, S. C., Dasari, P. & Ingman, W. V. Dissecting the biology of menstrual cycle-associated breast cancer risk. Front. Oncol. 6, 267 (2016).
Ramakrishnan, R., Khan, S. A. & Badve, S. Morphological changes in breast tissue with menstrual cycle. Mod. Pathol. 15, 1348–1356 (2002).
Giraddi, R. R. et al. Stem and progenitor cell division kinetics during postnatal mouse mammary gland development. Nat. Commun. 6, 8487 (2015).
Schedin, P., Mitrenga, T. & Kaeck, M. Estrous cycle regulation of mammary epithelial cell proliferation, differentiation, and death in the Sprague-Dawley rat: a model for investigating the role of estrous cycling in mammary carcinogenesis. J. Mammary Gland Biol. Neoplasia 5, 211–225 (2000).
Fata, J. E., Chaudhary, V. & Khokha, R. Cellular turnover in the mammary gland is correlated with systemic levels of progesterone and not 17beta-estradiol during the estrous cycle. Biol. Reprod. 65, 680–688 (2001).
Joshi, P. A. et al. Progesterone induces adult mammary stem cell expansion. Nature 465, 803–807 (2010).
Shehata, M. et al. Proliferative heterogeneity of murine epithelial cells in the adult mammary gland. Commun. Biol. 1, 111 (2018).
Bernhardt, S. M. et al. The menstrual cycle is an under-appreciated factor in premenopausal breast cancer diagnosis and treatment. Curr. Opin. Endocr. Metab. Res. 15, 37–42 (2020).
Ajayi, A. F. & Akhigbe, R. E. Staging of the estrous cycle and induction of estrus in experimental rodents: an update. Fertil. Res. Pract. 6, 5 (2020).
Ng, K. Y., Yong, J. & Chakraborty, T. R. Estrous cycle in ob/ob and ovariectomized female mice and its relation with estrogen and leptin. Physiol. Behav. 99, 125–130 (2010).
Guy, C. T., Cardiff, R. D. & Muller, W. J. Induction of mammary tumors by expression of polyomavirus middle T oncogene: a transgenic mouse model for metastatic disease. Mol. Cell. Biol. 12, 954–961 (1992).
Zomer, A. et al. Intravital imaging of cancer stem cell plasticity in mammary tumors. Stem Cells 31, 602–606 (2013).
Cora, M. C., Kooistra, L. & Travlos, G. Vaginal cytology of the laboratory rat and mouse: review and criteria for the staging of the estrous cycle using stained vaginal smears. Toxicol. Pathol. 43, 776–793 (2015).
Lenos, K. J. et al. Stem cell functionality is microenvironmentally defined during tumour expansion and therapy response in colon cancer. Nat. Cell Biol. 20, 1193–1202 (2018).
Tsukamoto, A. S., Grosschedl, R., Guzman, R. C., Parslow, T. & Varmus, H. E. Expression of the int-1 gene in transgenic mice is associated with mammary gland hyperplasia and adenocarcinomas in male and female mice. Cell 55, 619–625 (1988).
Amadori, D. et al. Cell proliferation as a predictor of response to chemotherapy in metastatic breast cancer: a prospective study. Breast Cancer Res. Treat. 43, 7–14 (1997).
Furlanetto, J. et al. Chemotherapy-induced ovarian failure in young women with early breast cancer: prospective analysis of four randomised neoadjuvant/adjuvant breast cancer trials. Eur. J. Cancer 152, 193–203 (2021).
Koga, C. et al. Chemotherapy-induced amenorrhea and the resumption of menstruation in premenopausal women with hormone receptor-positive early breast cancer. Breast Cancer 24, 714–719 (2017).
Liedtke, C. & Kiesel, L. Chemotherapy-induced amenorrhea – an update. Geburtshilfe Frauenheilkd 72, 809–818 (2012).
Pourali, L. et al. Incidence of chemotherapy-induced amenorrhea after adjuvant chemotherapy with taxane and anthracyclines in young patients with breast cancer. Iran. J. Cancer Prev. 6, 147–150 (2013).
Turnbull, A. K., Patel, S., Martinez-Perez, C., Rigg, A. & Oikonomidou, O. Risk of chemotherapy-related amenorrhoea (CRA) in premenopausal women undergoing chemotherapy for early stage breast cancer. Breast Cancer Res. Treat. 186, 237–245 (2021).
Gao, Y. et al. Increased cellular senescence in doxorubicin-induced murine ovarian injury: effect of senolytics. Geroscience 45, 1775–1790 (2023).
Wang, Y. et al. Doxorubicin obliterates mouse ovarian reserve through both primordial follicle atresia and overactivation. Toxicol. Appl. Pharmacol. 381, 114714 (2019).
Lin, E. Y. et al. Progression to malignancy in the polyoma middle T oncoprotein mouse breast cancer model provides a reliable model for human diseases. Am. J. Pathol. 163, 2113–2126 (2003).
Denkert, C. et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 19, 40–50 (2018).
Issa-Nummer, Y. et al. Prospective validation of immunological infiltrate for prediction of response to neoadjuvant chemotherapy in HER2-negative breast cancer–a substudy of the neoadjuvant GeparQuinto trial. PLoS ONE 8, e79775 (2013).
Loi, S. et al. Tumor-infiltrating lymphocytes and prognosis: a pooled individual patient analysis of early-stage triple-negative breast cancers. J. Clin. Oncol. 37, 559–569 (2019).
Beerling, E. et al. Plasticity between epithelial and mesenchymal states unlinks EMT from metastasis-enhancing stem cell capacity. Cell Rep. 14, 2281–2288 (2016).
Bornes, L. et al. Fsp1-mediated lineage tracing fails to detect the majority of disseminating cells undergoing EMT. Cell Rep. 29, 2565–2569 (2019).
de Groot, S. et al. Fasting mimicking diet as an adjunct to neoadjuvant chemotherapy for breast cancer in the multicentre randomized phase 2 DIRECT trial. Nat. Commun. 11, 3083 (2020).
Byers, S. L., Wiles, M. V., Dunn, S. L. & Taft, R. A. Mouse estrous cycle identification tool and images. PLoS ONE 7, e35538 (2012).
Burtis, C. A., Ashwood, E. R. & Bruns, D. E. Tietz Textbook of Clinical Chemistry and Molecular Diagnostics (Elsevier Health Sciences, 2012).
Heer, E. et al. Global burden and trends in premenopausal and postmenopausal breast cancer: a population-based study. Lancet Glob. Health 8, e1027–e1037 (2020).
Harbeck, N. et al. Breast cancer. Nat. Rev. Dis. Primers 5, 66 (2019).
Duarte, A. A. et al. BRCA-deficient mouse mammary tumor organoids to study cancer-drug resistance. Nat. Methods 15, 134–140 (2018).
Conte, P. F. et al. Chemotherapy with or without estrogenic recruitment in metastatic breast cancer. A randomized trial of the Gruppo Oncologico Nord Ovest (GONO). Ann. Oncol. 7, 487–490 (1996).
Conte, P. F. et al. Chemotherapy following estrogen-induced expansion of the growth fraction of human breast cancer. Cancer Res. 45, 5926–5930 (1985).
Ben-Eliyahu, S., Shakhar, G., Shakhar, K. & Melamed, R. Timing within the oestrous cycle modulates adrenergic suppression of NK activity and resistance to metastasis: possible clinical implications. Br. J. Cancer 83, 1747–1754 (2000).
Faas, M. et al. The immune response during the luteal phase of the ovarian cycle: a Th2-type response? Fertil. Steril. 74, 1008–1013 (2000).
White, H. D. et al. CD3+CD8+ CTL activity within the human female reproductive tract: influence of stage of the menstrual cycle and menopause. J. Immunol. 158, 3017–3027 (1997).
Chua, A. C., Hodson, L. J., Moldenhauer, L. M., Robertson, S. A. & Ingman, W. V. Dual roles for macrophages in ovarian cycle-associated development and remodelling of the mammary gland epithelium. Development 137, 4229–4238 (2010).
Liu, C. et al. Niche inflammatory signals control oscillating mammary regeneration and protect stem cells from cytotoxic stress. Cell Stem Cell 31, 89–105 (2024).
Hodson, L. J., Chua, A. C., Evdokiou, A., Robertson, S. A. & Ingman, W. V. Macrophage phenotype in the mammary gland fluctuates over the course of the estrous cycle and is regulated by ovarian steroid hormones. Biol. Reprod. 89, 65 (2013).
Wood, P. A., Bove, K., You, S., Chambers, A. & Hrushesky, W. J. Cancer growth and spread are saltatory and phase-locked to the reproductive cycle through mediators of angiogenesis. Mol. Cancer Ther. 4, 1065–1075 (2005).
Kashuba, A. D. et al. Quantification of intraindividual variability and the influence of menstrual cycle phase on CYP2D6 activity as measured by dextromethorphan phenotyping. Pharmacogenetics 8, 403–410 (1998).
Wagner, K. U. et al. Cre-mediated gene deletion in the mammary gland. Nucleic Acids Res. 25, 4323–4330 (1997).
Snippert, H. J. et al. Intestinal crypt homeostasis results from neutral competition between symmetrically dividing Lgr5 stem cells. Cell 143, 134–144 (2010).
Ventura, A. et al. Restoration of p53 function leads to tumour regression in vivo. Nature 445, 661–665 (2007).
McLean, A. C., Valenzuela, N., Fai, S. & Bennett, S. A. Performing vaginal lavage, crystal violet staining, and vaginal cytological evaluation for mouse estrous cycle staging identification. J. Vis. Exp. 67, e4389 (2012).
Mourao, L., Ciwinska, M., van Rheenen, J. & Scheele, C. Longitudinal intravital microscopy using a mammary imaging window with replaceable lid. J. Vis. Exp. https://doi.org/10.3791/63326 (2022).
Kedrin, D. et al. Intravital imaging of metastatic behavior through a mammary imaging window. Nat. Methods 5, 1019–1021 (2008).
Pinheiro, J. C. & Bates, D. M. Mixed-effects Models in S and S-PLUS (Springer, 2000).
Rizopoulos, D. Joint Models for Longitudinal and Time-to-Event Data (Chapman and Hall/CRC, 2012).
Wickham, H. Cetinkaya-Rundel, M & Grolemund, G. R for Data Science, 2nd edn (O’Reilly Media, Inc., 2023).
Lindstrom, M. L. & Bates, D. M. Nonlinear mixed effects models for repeated measures data. Biometrics 46, 673–687 (1990).
Acknowledgements
We thank M. Liefaard and E. Lips for the kind donation of a serum sample from their clinical study. We thank the staff at the NKI animal, animal pathology and flow-cytometry facilities; and the preclinical intervention unit of the Mouse Clinic for Cancer and Ageing at NKI for their technical support in performing some of the animal experiments. This work was supported by Boehringer Ingelheim Foundation (PhD fellowship); an EMBO postdoctoral fellowship (grant no. ALTF 1035-2020) and the Beug Metastasis Prize to C.L.G.J.S.; a PhD fellowship of the Flanders Research Organization (FWO, grant no. 11O4423N) to M.C.; the Ammodo Science Award; the Doctor Josef Steiner Foundation; and the Netherlands Organization for Scientific Research (NWO, Gravitation programme IMAGINE!, project no. 24.005.009 and VICI project no. 09150182110004) to J.v.R. This manuscript was edited at Life Science Editors, and edited for typos and style by ChatGPT.
Author information
Authors and Affiliations
Contributions
L.B. and C.L.G.J.S. conceived the idea and designed, performed and analysed most of the experiments. L.J.v.W., M.L. and H.H.v.R. designed, performed and analysed serum progesterone level experiments. B.d.B. performed IVM in ovariectomized mice. N.P., M.B. and M.v.d.V. performed ovariectomy experiments. J.O.L., M.C., G.B. and E.N.D. helped with performing and analysing experiments. A.B. acquired and managed patient samples at NKI. V.C.M.G. acquired patient data. R.M. and L.A. conceived and designed the nonlinear nested mixed model. Using this model, L.A. performed longitudinal analysis of the animal experiments. R.M. carried out all general statistical tests as outlined in Supplementary File 1. N.d.G. and J.R.K. collected patient samples and data from the DIRECT study. J.W., S.L. and M.K. interpreted and supervised patient data from NKI. J.v.R. conceived the idea, designed experiments and supervised the project. L.B., C.L.G.J.S. and J.v.R. wrote the manuscript, which has been reviewed and approved by all authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature thanks Wendy Ingman, Nicholas Turner and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Fig. 1 Oestrous cycle dependent proliferation of tumour cells during oestrus stage in genetic MMTV-PyMT model.
a, Left panel: Schematic of healthy mammary gland turnover during the oestrous cycle (centre) and representative immunofluorescent images (3D rendered) of tumour-free mammary ducts during dioestrus (left) and oestrus (right) stage. Right panel: representative immunofluorescent image of tumour-free mammary ducts in an ovariectomized mouse. Mammary ducts are labelled with smooth muscle actin (white). Scale bars, 100 µm. b, Schematic representation of R26-CreERT2 and R26R-Confetti constructs, which were crossed with different tumour models to enable lineage tracing in a subset of tumour cells. Upon injection of low dose of tamoxifen, some tumour cells will recombine the confetti construct leading to stochastic expression of one of the four confetti colours. These single cells can be followed over multiple days using IVM. c, Clone growth rate of all quantified clones from multiday IVM imaging of the genetic MMTV-PyMT tumour model in physiologically cycling mice (top) or ovariectomized mice (bottom). Each line represents a clone, and coloured lines highlight growth of individual clones. Top panels show coordinated clonal growth, which is abolished in the ovariectomized conditions (bottom panels). d, Images of crystal violet stained vaginal smears in oestrus (left) and dioestrus (right) representative for n > 30 mice. The proportion of epithelial cells and leukocytes was used to determine the cycle stage. Scale bars, 100 µm. e, Serum levels of progesterone in different oestrous cycle stages, determined by cytology of the vaginal smear. n = 9 (oestrus) and n = 10 (dioestrus) mice. f, Representative immunofluorescent images of EdU incorporation in tumours derived from the genetic MMTV-PyMT mouse model during oestrus and dioestrus phase. Scale bars, 1 mm. g, Expression of the gene PyMT in different oestrous stages depicted as violin plot. n = 10 mice per oestrous stage. Data is depicted as violin plots thick solid line represents median and solid lines indicate the 25th and 75th percentiles (e,g). Dots represent different mice (e) and tumours from different mice (g). Statistical analysis was performed using one-sided (e) and two-sided (g) Wilcoxon-Mann-Whitney test. *P < 0.05. More details on statistical analysis can be found in Supplementary File 1.
Extended Data Fig. 2 Oestrous cycle dependent proliferation of tumour cells during oestrus stage can be reproduced in the MMTV-Wnt1 tumour model.
a, Schematic representation of the multiday intravital microscopy setup (left) with overview images (single Z-plane) (centre) of the first imaging session (top) and the following imaging session (bottom) that are presentative for 6 experiments. Rectangles indicate example clones represented over multiple imaging days (right). Scale bar, 100 µm (overview), 50 µm (zoom). b, Clone growth rate of all quantified clones from multiday IVM imaging of transplanted MMTV-Wnt1 model. Each line represents a clone, and coloured lines highlight coordinated growth of individual clones. c, Immunofluorescent images (left) and violin plots depicting quantification (right) of EdU incorporation in the genetic MMTV-Wnt1 model representative for n = 5 (oestrus) and n = 4 (dioestrus) mice. Scale bar, 100 µm. Data is depicted as violin plots, thick solid line represents median and solid lines indicate the 25th and 75th percentiles, each dot represents a tumour (c). Statistical analysis was performed using one-sided Wilcoxon-Mann-Whitney test (c). *P < 0.05. More details on statistical analysis can be found in Supplementary File 1.
Extended Data Fig. 3 Disruption of physiological oestrous cycle after chemotherapy.
a, Representative plots depicting the gating strategy to determine PI+ tumour cells by flow cytometry analysis. b, Representative examples of crystal violet stained vaginal smears in mice with a disrupted cycle after treatment with chemotherapy. c, H&E image of physiological murine ovary, indicating the different follicle stages: PrF: Primordial follicle; PF: Primary follicle; SF: Secondary follicle; AF: Antral follicle and CL: Corpus luteum. Images are representative for n = 10 treatment naïve mice per stage. d, H&E images of ovaries from mice pretreatment, 7 days after initial treatment or long-term (LT) after treatment at endpoint, oestrus (top) or dioestrus (bottom). Images are representative for n = 10 mice (oestrus, Day 0), n = 7 mice (oestrus, Day 7), n = 4 mice (oestrus, LT), n = 10 mice (dioestrus, Day 0), n = 7 mice (dioestrus, Day 7), n = 8 mice (dioestrus, LT). e, Bar graph depicting the amount of PrF: Primordial follicles; PF: Primary follicles; SF: Secondary follicles per mm2 in ovaries of mice, pretreatment, 7 days after initial treatment or at endpoint of long-term (LT) experiment. n = O0 = 10; O7 = 7; OLT = 4; D0 = 10; D7 = 7; DLT = 8. Scale bars, 100 µm (b), 1 mm (c, overview image, d), 100 µm (c, zoom).
Extended Data Fig. 4 Differential response in oestrous cycle stages independent of T cell presence.
a,b, Representative immunohistochemistry staining and quantification of CD4+ T cells (a) and CD8+ T cells (b) in treatment naïve MMTV-PyMT mammary tumours during different stages of the oestrous cycle. n = 3 mice per oestrous stage and 2 tumours per animal. c, Schematic representation of the experimental setup. Mice were treated with depletion antibodies prior to doxorubicin treatment, which was initiated at a cumulative tumour mass of 500–750 mm3 in either oestrus (O) or dioestrus (D) stage. d, Representative immunohistochemistry staining of CD4+ T cells (top) and CD8+ T cells (bottom) in 36 tumours of 9 mice receiving T cell depletion antibodies (α-CD4 + α-CD8). e,f, Violin plots depicting percentage of dying tumour cells identified by positive staining for propidium iodide (e) and tumour volume change compared to baseline (f) for mice receiving T cell depletion antibodies (α-CD4 + α-CD8) and treated with doxorubicin. n = Oa-CD4/8 = 5 mice/20 tumours, Da-CD4/8 = 4 mice/16 tumours. Data in a,b,e,f is depicted as violin plots, thick solid line represents median and solid lines indicate the 25th and 75th percentiles. Dots represent individual tumours (a,b,e) or mice (f). Scale bars, 500 µm (a,b,d). Statistical analysis was performed using linear mixed effects models (e), a two way anova (a,b) and a one-sided Wilcoxon-Mann-Whitney test (f). *P < 0.05. More details on statistical analysis can be found in Supplementary File 1.
Extended Data Fig. 5 Gating strategy for flow cytometry analysis of depletion experiments.
Representative plots depicting the gating strategy to determine PI+ tumour cells by flow cytometry analysis of depletion experiments.
Extended Data Fig. 6 Retrospective analysis of menstrual cycle-dependent sensitivity to neoadjuvant chemotherapy in BC patients.
a, Patients with HR+HER2− BC were divided into the progesterone-low (<2.2 nmol/L) or progesterone-high (>2.2 nmol/L) group based on the progesterone level in their sera within five days of initiating NAC. b-f, Table and comparison of standard clinicopathological parameters of 30 premenopausal patients with HR+HER2− BC. g, Patients with TNBC were divided into the progesterone-low (<2.2 nmol/L) or progesterone-high (>2.2 nmol/L) group based on the progesterone level in their sera within five days of initiating NAC. h-l, Table and comparison of standard clinicopathological parameters of 25 premenopausal patients with TNBC Data in c,d,e,i,j is depicted as violin plots, thick solid line represents median and solid lines indicate the 25th and 75th percentiles. Statistical analysis was performed using two way anova (c,d,e), or two-sided Wilcoxon-Mann-Whitney test (i,j). #P < 0.1. More details on statistical analysis can be found in Supplementary File 1.
Supplementary information
Supplementary File 1
Overview of statistical tests, analytical methods and P values.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bornes, L., van Winden, L.J., Geurts, V.C.M. et al. The oestrous cycle stage affects mammary tumour sensitivity to chemotherapy. Nature 637, 195–204 (2025). https://doi.org/10.1038/s41586-024-08276-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-024-08276-1