Abstract
Sepsis arises from diverse and incompletely understood dysregulated host response processes following infection that leads to life-threatening organ dysfunction. Here we showed that neutrophils and emergency granulopoiesis drove a maladaptive response during sepsis. We generated a whole-blood single-cell multiomic atlas (272,993 cells, n = 39 individuals) of the sepsis immune response that identified populations of immunosuppressive mature and immature neutrophils. In co-culture, CD66b+ sepsis neutrophils inhibited proliferation and activation of CD4+ T cells. Single-cell multiomic mapping of circulating hematopoietic stem and progenitor cells (HSPCs) (29,366 cells, n = 27) indicated altered granulopoiesis in patients with sepsis. These features were enriched in a patient subset with poor outcome and a specific sepsis response signature that displayed higher frequencies of IL1R2+ immature neutrophils, epigenetic and transcriptomic signatures of emergency granulopoiesis in HSPCs and STAT3-mediated gene regulation across different infectious etiologies and syndromes. Our findings offer potential therapeutic targets and opportunities for stratified medicine in severe infection.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
27,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
209,00 € per year
only 17,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
Raw data for whole-blood single-cell sequencing and HSC single-cell sequencing datasets are deposited on the European Genome–phenome Archive (EGAS00001006283) and derived data are at Zenodo (https://doi.org/10.5281/zenodo.7723202). For sequence-level raw datasets deposited at the European Genome–phenome Archive, access is managed by a Data Access Committee.
Code availability
Code used for every algorithm followed in data processing and analysis is fully referenced within the specific Methods sections.
References
Maslove, D. M. et al. Redefining critical illness. Nat. Med. 28, 1141–1148 (2022).
van der Poll, T., Shankar-Hari, M. & Wiersinga, W. J. The immunology of sepsis. Immunity 54, 2450–2464 (2021).
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315, 801–810 (2016).
Rudd, K. E. et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet 395, 200–211 (2020).
Davenport, E. E. et al. Genomic landscape of the individual host response and outcomes in sepsis: a prospective cohort study. Lancet Resp. Med. 4, 259–271 (2016).
Scicluna, B. P. et al. Classification of patients with sepsis according to blood genomic endotype: a prospective cohort study. Lancet Resp. Med. 5, 816–826 (2017).
Sweeney, T. E. et al. Unsupervised analysis of transcriptomics in bacterial sepsis across multiple datasets reveals three robust clusters. Crit. Care Med. 46, 915–925 (2018).
Reyes, M. et al. An immune-cell signature of bacterial sepsis. Nat. Med. 26, 333–340 (2020).
Qi, X. et al. Identification and characterization of neutrophil heterogeneity in sepsis. Crit. Care 25, 50 (2021).
Shen, X., Cao, K., Zhao, Y. & Du, J. Targeting neutrophils in sepsis: from mechanism to translation. Front. Pharm. 12, 644270 (2021).
Farkas, J. D. The complete blood count to diagnose septic shock. J. Thorac. Dis. 12, S16–S21 (2020).
Meghraoui-Kheddar, A. et al. Two new immature and dysfunctional neutrophil cell subsets define a predictive signature of sepsis useable in clinical practice. Am. J. Respir. Crit. Care Med. 205, 46–59 (2020).
Schulte-Schrepping, J. et al. Severe COVID-19 is marked by a dysregulated myeloid cell compartment. Cell 182, 1419–1440 (2020).
Sinha, S. et al. Dexamethasone modulates immature neutrophils and interferon programming in severe COVID-19. Nat. Med. 28, 201–211 (2022).
Uhel, F. et al. Early expansion of circulating granulocytic myeloid-derived suppressor cells predicts development of nosocomial infections in patients with sepsis. Am. J. Respir. Crit. Care Med. 196, 315–327 (2017).
Reddy, K. et al. Subphenotypes in critical care: translation into clinical practice. Lancet Resp. Med. 8, 631–643 (2020).
Cano-Gamez, E. et al. An immune dysfunction score for stratification of patients with acute infection based on whole-blood gene expression. Sci. Transl. Med. 14, eabq4433 (2022).
Burnham, K. L. et al. Shared and distinct aspects of the sepsis transcriptomic response to fecal peritonitis and pneumonia. Am. J. Respir. Crit. Care Med. 196, 328–339 (2017).
Antcliffe, D. B. et al. Transcriptomic signatures in sepsis and a differential response to steroids. From the VANISH randomized trial. Am. J. Respir. Crit. Care Med. 199, 980–986 (2019).
Cazalis, M. A. et al. Decreased HLA-DR antigen-associated invariant chain (CD74) mRNA expression predicts mortality after septic shock. Crit. Care 17, R287 (2013).
Veglia, F., Perego, M. & Gabrilovich, D. Myeloid-derived suppressor cells coming of age. Nat. Immunol. 19, 108–119 (2018).
Bayik, D. et al. Myeloid-derived suppressor cell subsets drive glioblastoma growth in a sex-specific manner. Cancer Discov. 10, 1210–1225 (2020).
Alshetaiwi, H. et al. Defining the emergence of myeloid-derived suppressor cells in breast cancer using single-cell transcriptomics. Sci. Immunol. 5, eaay6017 (2020).
Hao, Y. et al. Integrated analysis of multimodal single-cell data. Cell 184, 3573–3587 (2021).
Granja, J. M. et al. Single-cell multiomic analysis identifies regulatory programs in mixed-phenotype acute leukemia. Nat. Biotechnol. 37, 1458–1465 (2019).
Hay, S. B., Ferchen, K., Chetal, K., Grimes, H. L. & Salomonis, N. The Human Cell Atlas bone marrow single-cell interactive web portal. Exp. Hematol. 68, 51–61 (2018).
Hirai, H. et al. C/EBPβ is required for ‘emergency’ granulopoiesis. Nat. Immunol. 7, 732–739 (2006).
Manz, M. G. & Boettcher, S. Emergency granulopoiesis. Nat. Rev. Immunol. 14, 302–314 (2014).
Böiers, C. et al. Expression and role of FLT3 in regulation of the earliest stage of normal granulocyte-monocyte progenitor development. Blood 115, 5061–5068 (2010).
Makishima, H. et al. Somatic SETBP1 mutations in myeloid malignancies. Nat. Genet. 45, 942–946 (2013).
COMBAT Consortium. A blood atlas of COVID-19 defines hallmarks of disease severity and specificity. Cell 185, 916–938 (2022).
Giladi, A. et al. Single-cell characterization of haematopoietic progenitors and their trajectories in homeostasis and perturbed haematopoiesis. Nat. Cell Biol. 20, 836–846 (2018).
Demers, M. et al. Cancers predispose neutrophils to release extracellular DNA traps that contribute to cancer-associated thrombosis. Proc. Natl Acad. Sci. USA 109, 13076–13081 (2012).
Dunning, J. et al. Progression of whole-blood transcriptional signatures from interferon-induced to neutrophil-associated patterns in severe influenza. Nat. Immunol. 19, 625–635 (2018).
Bos, L. D. J. et al. Understanding heterogeneity in biologic phenotypes of acute respiratory distress syndrome by leukocyte expression profiles. Am. J. Respir. Crit. Care Med. 200, 42–50 (2019).
Wong, H. R. et al. Identification of pediatric septic shock subclasses based on genome-wide expression profiling. BMC Med. 7, 34 (2009).
Martin, P. et al. Mouse neutrophils express the decoy type 2 interleukin-1 receptor (IL-1R2) constitutively and in acute inflammatory conditions. J. Leukoc. Biol. 94, 791–802 (2013).
Weber, G. F. et al. Interleukin-3 amplifies acute inflammation and is a potential therapeutic target in sepsis. Science 347, 1260–1265 (2015).
Kwok, I. et al. Combinatorial single-cell analyses of granulocyte-monocyte progenitor heterogeneity reveals an early uni-potent neutrophil progenitor. Immunity 53, 303–318 (2020).
Reyes, M. et al. Plasma from patients with bacterial sepsis or severe COVID-19 induces suppressive myeloid cell production from hematopoietic progenitors in vitro. Sci. Transl. Med. 13, eabe9599 (2021).
Zekavat, S. M. et al. Hematopoietic mosaic chromosomal alterations increase the risk for diverse types of infection. Nat. Med. 27, 1012–1024 (2021).
Mitroulis, I. et al. Modulation of myelopoiesis progenitors is an integral component of trained immunity. Cell 172, 147–161 (2018).
Pietras, E. M. et al. Chronic interleukin-1 exposure drives haematopoietic stem cells towards precocious myeloid differentiation at the expense of self-renewal. Nat. Cell Biol. 18, 607–618 (2016).
Li, X. et al. Maladaptive innate immune training of myelopoiesis links inflammatory comorbidities. Cell 185, 1709–1727 (2022).
Naik, S. & Fuchs, E. Inflammatory memory and tissue adaptation in sickness and in health. Nature 607, 249–255 (2022).
de Laval, B. et al. C/EBPβ-dependent epigenetic memory induces trained immunity in hematopoietic stem cells. Cell Stem Cell 26, 793 (2020).
Zhang, H. et al. STAT3 controls myeloid progenitor growth during emergency granulopoiesis. Blood 116, 2462–2471 (2010).
Walker, F. et al. IL6/sIL6R complex contributes to emergency granulopoietic responses in G-CSF- and GM-CSF-deficient mice. Blood 111, 3978–3985 (2008).
Hamilton, F. et al. Therapeutic potential of IL6R blockade for the treatment of sepsis and sepsis-related death: findings from a Mendelian randomisation study. PLoS Med. 20, e1004174 (2023).
The REMAP-CAP Investigators. Interleukin-6 receptor antagonists in critically ill patients with COVID-19. N. Engl. J. Med. 384, 1491–1502 (2021).
Mellhammar, L. et al. NEWS2 is superior to qSOFA in detecting sepsis with organ dysfunction in the emergency department. J. Clin. Med. 8, 1128 (2019).
Sinha, S. et al. Dexamethasone modulates immature neutrophils and interferon programming in severe COVID-19. Nat. Med. 28, 201–211 (2022).
Kaminow, B., Yunusov, D. & Dobin, A. STARsolo: accurate, fast and versatile mapping/quantification of single-cell and single-nucleus RNA-seq data. Preprint at bioRxiv https://doi.org/10.1101/2021.05.05.442755 (2021).
Lun, A. T. L. et al. EmptyDrops: distinguishing cells from empty droplets in droplet-based single-cell RNA sequencing data. Genome Biol. 20, 63 (2019).
Gayoso, A. et al. Joint probabilistic modeling of single-cell multi-omic data with totalVI. Nat. Methods 18, 272–282 (2021).
Bergen, V., Lange, M., Peidli, S., Wolf, F. A. & Theis, F. J. Generalizing RNA velocity to transient cell states through dynamical modeling. Nat. Biotechnol. 38, 1408–1414 (2020).
Cano-Gamez, E. et al. An immune dysfunction score for stratification of patients with acute infection based on whole blood gene expression. Sci. Transl. Med. 14, eabq4433 (2022).
Dann, E., Henderson, N. C., Teichmann, S. A., Morgan, M. D. & Marioni, J. C. Differential abundance testing on single-cell data using k-nearest neighbor graphs. Nat. Biotechnol. 40, 245–253 (2022).
Robinson, M. D., McCarthy, D. J. & Smyth, G. K. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics 26, 139–140 (2010).
Wilk, A. J. et al. A single-cell atlas of the peripheral immune response in patients with severe COVID-19. Nat. Med. 26, 1070–1076 (2020).
Kotliar, D. et al. Identifying gene expression programs of cell-type identity and cellular activity with single-cell RNA-Seq. eLife 8, e43803 (2019).
Janky, R. et al. iRegulon: from a gene list to a gene regulatory network using large motif and track collections. PLoS Comput. Biol. 10, e1003731 (2014).
Yu, G., Wang, L. G., Han, Y. & He, Q. Y. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS 16, 284–287 (2012).
Granja, J. M. et al. ArchR is a scalable software package for integrative single-cell chromatin accessibility analysis. Nat. Genet. 53, 403–411 (2021).
Corces, M. R. et al. The chromatin accessibility landscape of primary human cancers. Science 362, eaav1898 (2018).
Zheng, R. et al. Cistrome Data Browser: expanded datasets and new tools for gene regulatory analysis. Nucleic Acids Res. 47, D729–D735 (2019).
Kamimoto, K., Hoffmann, C. M. & Morris, S. A. Dissecting cell identity via network inference and in silico gene perturbation. Nature 614, 742–751 (2023).
Pliner, H. A. et al. Cicero predicts cis-regulatory dna interactions from single-cell chromatin accessibility data. Mol. Cell 71, 858–871 (2018).
Qiu, X. et al. Mapping transcriptomic vector fields of single cells. Cell 185, 690–711 (2022).
Korsunsky, I. et al. Fast, sensitive and accurate integration of single-cell data with Harmony. Nat. Methods 16, 1289–1296 (2019).
Ogishi, M. et al. Multibatch cytometry data integration for optimal immunophenotyping. J. Immunol. 206, 206–213 (2021).
Van Gassen, S. et al. FlowSOM: using self-organizing maps for visualization and interpretation of cytometry data. Cytom. A 87, 636–645 (2015).
Nowicka, M. et al. CyTOF workflow: differential discovery in high-throughput high-dimensional cytometry datasets. F1000Res. 6, 748 (2017).
Diggins, K. E., Greenplate, A. R., Leelatian, N., Wogsland, C. E. & Irish, J. M. Characterizing cell subsets using marker enrichment modeling. Nat. Methods 14, 275–278 (2017).
Street, K. et al. Slingshot: cell lineage and pseudotime inference for single-cell transcriptomics. BMC Genomics 19, 477 (2018).
Argelaguet, R. et al. MOFA+: a statistical framework for comprehensive integration of multi-modal single-cell data. Genome Biol. 21, 111 (2020).
Newman, A. M. et al. Determining cell type abundance and expression from bulk tissues with digital cytometry. Nat. Biotechnol. 37, 773–782 (2019).
Acknowledgements
We thank the patients and healthy donors who participated for their generous contribution to this study and the Emergency Medicine Research Oxford team and wider clinical staff, in particular A. Brent, A. Novak, A. Kingwill and R. Sayeed and Oxford University NHS Hospital Trusts recruiting hospitals involved in patient recruitment and sample collection. We thank the Oxford Genomics Centre for sequencing support, in particular A. Lee for project management and I. Nassiri for bioinformatic support. We thank the Wellcome Centre for Human Genetics and Jenner Institute flow facilities for assistance in sorting experiments. We are grateful to M. Attar, F. Curion, K. Kedzierska, P. Maclean, G. Scozzafava and members of the Knight laboratory for support and critical discussion. We also thank the COMBAT consortium for access to data for re-analysis.
We acknowledge the support of the National Institute for Health Research (NIHR) through the Comprehensive Clinical Research Network for patient recruitment. This research was funded by the Medical Research Council (MR/V002503/1) (to J.C.K. and E.E.D.), Wellcome Trust Investigator Award (204969/Z/16/Z, to J.C.K.; 209422/Z/17/Z, to I.A.U.), Chinese Academy of Medical Sciences Innovation 537 Fund for Medical Science (2018-I2M-2-002; to J.C.K.), Croucher Foundation (to A.J.K.), Wellcome Trust Grants (090532/Z/09/Z and 203141/Z/16/Z) to core facilities Wellcome Centre for Human Genetics, Wellcome Trust core funding to the Wellcome Sanger Institute (grant numbers WT206194 and 108413/A/15/D) and NIHR Oxford Biomedical Research Centre (to J.C.K.). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the UK Department of Health. For the purpose of Open Access, the author has applied a CC BY public copyright license to any Author Accepted Manuscript version arising from this submission.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization was the responsibility of A.J.K. and J.C.K. Data curation was conducted by A.J.K. Formal analysis was conducted by A.J.K., E.C.-G., A.A., M.S. and Y.-X.Z. Funding was acquired by J.C.K. and E.E.D. Investigation was carried out by A.J.K., A.A., M.S. and R.C.F. Methodology was the responsibility of A.J.K., E.C.-G. and K.L.B. Project administration was carried out by J.C.K., C.M., I.A.U., J.A.T. and E.E.D. Resources were the responsibility of A.J.K., E.C.-G., J.C.K., A.J.M., S.M. and C.J.H. Software was the responsibility of A.J.K. and E.C.-G. Supervision was carried out by J.C.K., I.A.U. and C.M. Visualization was carried out by A.J.K. and J.C.K. Writing of the original draft was conducted by A.J.K. and J.C.K. Review and editing was carried out by all authors who read, provided input on and approved the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Immunology thanks John Marshall and Renato Ostuni for their contribution to the peer review of this work. Primary Handling Editor: Ioana Visan, in collaboration with the Nature Immunology team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 scWB single-cell RNA and cell surface profiling annotation, clustering and neutrophil RNA velocity analysis.
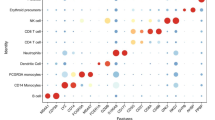
a, UMAP of 272,993 cells with TotalVI denoised surface protein marker expression overlaid for selected lineage defining markers. b, Cell surface expression of proteins denoting neutrophil maturation stages for annotated neutrophil subsets. Boxplots denote minimum and maximum with whiskers and bottom quartile, median and upper quartile with the box. c, Comparison of broad annotations (Methods ‘Whole blood single cell multi-omic analysis (scWB)’) with data driven algorithmic labeling of cell identity by SingleR based on reference bulk RNA-seq profiles of pure cell populations from the Blueprint Consortium. d, Proportions of neutrophils and lymphocytes and HLA-DRA and HLA-DRB1 gene expression in classical monocytes in healthy controls (HC) (n = 6), sepsis (n = 26) and post-cardiac surgery (CS) (n = 7) samples. Boxplots denote minimum and maximum with whiskers and bottom quartile, median and upper quartile with the box. e, Clustering results at varying resolutions (0.8–1.1) for fine annotation strategy. f–i, Heat maps of gene markers for (f) PADI4+ immature neutrophils (g) IL1R2+ immature neutrophils (h) MPO+ immature neutrophils/progenitors and (i) cycling neutrophil progenitors. j, UMAP of neutrophils (excluding degranulating neutrophils) with RNA velocity stream directions plotted. k, Partition-based graph abstraction analysis of RNA velocity predicted cellular trajectory transitions. Neu, neutrophils.
Extended Data Fig. 2 ScWB healthy control (HC)-post-cardiac surgery (CS) and CS-sepsis cell type/state differential abundance (DA) analysis and sepsis neutrophil-CD4+ T cell immunosuppression.
a, DA analysis using graph neighborhood-based method to detect enrichment of neighborhoods between CS and HC samples, with UMAP of sampled neighborhoods and statistically significant enrichment colored (spatial FDR < 0.05 with generalized linear modeling). b, Beeswarm plot of CS-HC DA analysis with cluster labels of neighborhoods depicted. c, UMAP of DA analysis between CS and sepsis. Nhood, neighborhood; logFC, log fold change. d, Proportions of immature neutrophil populations as a percentage of total neutrophils across comparator groups (n = 26 sepsis, n = 6 HC, n = 7 CS). Boxplots denote minimum and maximum with whiskers and bottom quartile, median and upper quartile with the box. e, Percentage of live, non-apoptotic CD4+ T cells after 72–96 hours of co-culture with either HC or sepsis neutrophils. Error bars denote standard error of the mean. f, Correlations (Spearman’s Rho) of proportions of each neutrophil subset as measured from single-cell RNA and cell surface protein profiling from sepsis patients with neutrophil-CD4+ T cell co-culture suppression readouts (n = 11). g, Percentage of CD4+ T cells proliferating, expressing PD-1 or expressing CD69 in sepsis neutrophil-allogeneic T cell co-cultures with various treatments compared to untreated (UT) control (n = 6). Untreated (UT), 15 μM TG6−10-1 (PG EP2 receptor antagonist), 15 μM GW-627368 (PG EP4 receptor antagonist), 10 μM indomethacin (COX inhibitor), 10 ng/mL anti-PD-L1/2, 1 mM L-arginine + 1 μM arginase-1 inhibitor. Boxplots denote minimum and maximum with whiskers and bottom quartile, median and upper quartile with the box. h, Gene set enrichment analysis of MsigDB C2 prostaglandin related pathways for sepsis vs. HC neutrophil differential gene expression. i, Violin plots of gene set scoring of mature and immature neutrophils in sepsis and healthy control (HC) samples by gene signatures of granulocytic myeloid-derived suppressor cells (G-MDSC)22,23. P-values for gene set scoring were calculated with two-sided Wilcoxon rank-sum tests while P-values for co-culture inhibition reversal were calculated with two-sided Wilcoxon signed-rank tests. Neu, neutrophils; Cycling progen, cycling neutrophil progenitors; IL1R2+/IL1R2+ immature, IL1R2+ immature neutrophils; MPO+, MPO+ immature neutrophils or progenitors; PADI4+, PADI4+ immature neutrophils; PG, prostaglandin; COX, cyclo-oxygenase; NES, normalized enrichment score; FDR, false discovery rate. *P < 0.05, ****P < 0.0001.
Extended Data Fig. 3 scWB convalescent sepsis neutrophil analysis and scHSPC hematopoietic stem and progenitor cell (HSPC) RNA based identity mapping.
a, Boxplots of proportions of neutrophil states in HC vs. convalescent sepsis samples from scWB. Boxplots denote minimum and maximum with whiskers and bottom quartile, median and upper quartile with the box. b, Proliferative fraction of anti-CD3/28 bead-stimulated CD4+ T cells after co-culture with neutrophils at a 4 neutrophil:1 T cell ratio, compared to positive controls of CD4+ T cells cultured with anti-CD3/28 beads alone (n = 10 HC, n = 9 convalescent sepsis). Boxplots denote minimum and maximum with whiskers and bottom quartile, median and upper quartile with the box. c,d, HSPC (right) mapping to (c) Seurat bone marrow mononuclear cell (BMMC) dataset24 (left) and (d) healthy donor BMMC dataset from Granja et al.25 (left). e, UMAP of HSPCs clustered on Harmony batch corrected RNA and chromatin reduced dimensions after non-HSPCs were filtered out (46,156 cells; Methods). f, UMAP colored by RNA prediction identities from HSPC mapping to Seurat BMMC dataset. g, UMAP of progenitor cells alone clustered on Harmony batch corrected RNA and chromatin reduced dimensions (16,820 cells; Methods). h, Boxplots of progenitor cell clusters as a proportion of total progenitor cells (n = 15 acute sepsis, n = 7 HC). Boxplots denote minimum and maximum with whiskers and bottom quartile, median and upper quartile with the box. i, Heat map of genes defining progenitor clusters with known lineage defining genes highlighted. j, Boxplots of HSC clusters as a proportion of total HSCs (n = 15 acute sepsis, n = 7 HC). Boxplots denote minimum and maximum with whiskers and bottom quartile, median and upper quartile with the box. k, UMAP of CD34+ HSPCs from annotated Human Cell Atlas bone marrow mononuclear cell (BMMC) scRNA-seq data26 for deriving granulopoiesis gene set (Methods). Neu, neutrophils; c/pDC, conventional/plasmacytoid dendritic cell; GMP, granulocyte monocyte progenitor; LMPP, lymphoid-primed multipotential progenitors; NK, natural killer; Prog, progenitor; Mk, megakaryocyte; RBC, red blood cell; Eryth, erythrocyte; CMP, common myeloid progenitor; Mono, monocyte; CD4 N1/2, CD4+ naïve T cell 1/2; CD4 M, memory CD4+ T cell; CD8 CM, central memory CD8+ T cell; PC, plasma cell; MDP, monocyte/dendritic cell progenitor; MultiLin, multilineage progenitor; MEP, megakaryocyte/erythroid progenitor; MKP megakaryocyte progenitor; ERP, erythrocyte progenitor; Eo, eosinophil; Mast, mast cell.
Extended Data Fig. 4 scWB scRNA-seq data substructure and concordance with transcriptomic sepsis response signature (SRS) endotypes.
a, First two principal components from principal components analysis of pseudobulked single-cell expression profiles of sepsis samples colored by SRS assignment. b, Pearson’s correlation of fold change in gene expression between SRS1 vs. non-SRS1 (sample level pseudobulks) in scWB and cohort in which SRS was originally derived5. c, Consensus clustering of pseudobulked single-cell gene expression profiles of sepsis samples (all cells per sample) at the level of two clusters. d, Overlaps of consensus clustering classification vs. SRS classification. e, Unsupervised hierarchical clustering of pseudobulked single-cell expression profiles of sepsis samples. SRS, sepsis response signature.
Extended Data Fig. 5 scWB scRNA-seq SRS gene expression analysis and SRS neutrophil functional interrogation.
a, b, Volcano plots of DGE analysis between SRS groups for pseudobulked (a) neutrophil states and (b) mononuclear cells (red denoting genes with fold change > 1.2 and FDR < 0.1) (positive fold change denoting upregulation in SRS1). c, Correlation (Spearman’s Rho 95% confidence interval) of SRS1 sample median neutrophil IL1R2 gene expression as measured by scRNA-seq with median neutrophil IL1R2 cell surface protein expression as measured by flow cytometry (n = 14). d, Proliferative fraction of anti-CD3/28 bead-stimulated CD4+ T cells after co-culture with neutrophils at a 4 neutrophil:1 T cell ratio, compared to positive controls of CD4+ T cells cultured with anti-CD3/28 beads alone (n = 6 SRS1, n = 13 non-SRS1). Boxplots denote minimum and maximum with whiskers and bottom quartile, median and upper quartile with the box. e, Neutrophil phagocytosis with and without GM-CSF stimulation (n = 15). Boxplots denote minimum and maximum with whiskers and bottom quartile, median and upper quartile with the box. P-values for neutrophil functional assays were calculated with two-sided Wilcoxon rank-sum tests. SRS, sepsis response signature; FDR, false discovery rate; ns, not significant. Neu, neutrophils.
Extended Data Fig. 6 MmV validation of neutrophil immaturity underlying SRS1.
a, First two principal components from principal components analysis of n = 42 sepsis patient samples (36 individuals) for peripheral blood bulk RNA-seq (23,063 genes). b, Kaplan-Meier survival by SRS (log-rank test P-value, 95% confidence intervals). c, Heat map of 15 immune cell clusters (with neutrophil clusters merged; Methods) from clustering on 41 protein markers for n = 41 sepsis (36 individuals) and n = 11 healthy control (HC) samples. d, UMAP of nine broad immune cell types (2,287,410 cells) from CyTOF immunophenotyping. e, Marker enrichment modeling (MEM) score heat map of eight neutrophil clusters (1,921,471 cells), identified from neutrophil subclustering on 17 selected protein markers. f, g, UMAP of (f) neutrophil subsets showing (g) density-based distribution by SRS/healthy control (HC) status. h, Neutrophil cluster frequency as a proportion of all cells with proportional differences across SRS analyzed by generalized linear mixed models (n = 41 samples, 36 individuals). i, Diffusion map dimensionality reduction of neutrophils. Boxplots denote minimum and maximum with whiskers and bottom quartile, median and upper quartile with the box. j, Diffusion components 1 and 2 with black line depicting trajectory identified by principal curve fitting. Color reflects pseudotime value of cell with red indicating early pseudotime and blue late pseudotime. k, Dotplot of neutrophil subsets according to pseudotemporal ordering from principal curve trajectory with median and interquartile range. l, Density distribution of neutrophils over pseudotime with Kolmogorov-Smirnov test for SRS1 vs. non-SRS1 distributions. m, CyTOF PCA using proportions of all cells (left), only mononuclear cells (MNC, middle) and only neutrophils (right) with 95% data ellipses (assuming a multivariate t-distribution). SRS, sepsis response signature; cMono, classical monocyte; ncMono, non-classical monocyte; NK cell, natural killer cell; Neu, neutrophil; pro-neu, pro-neutrophil; pre-neu, pre-neutrophil; imm neu, immature neutrophil; int neu, intermediate neutrophil; int inf neu, intermediate inflammatory neutrophil; mature neu, mature neutrophil; MNP, mononuclear phagocytes; DC, diffusion component; FDR, false discovery rate. * FDR < 0.05, ** FDR < 0.01, *** FDR < 0.001.
Extended Data Fig. 7 MmV factor analysis (MOFA+) and brWB-CID validation of SRS1 IL1R2+ immature neutrophil expansion.
a-j MmV. a, Differentially expressed modules in whole blood bulk RNA-seq (FDR < 0.01, two-sided Wilcoxon rank-sum test) (n = 26 SRS1, n = 16 non-SRS1). Violin plots with median, 95% confidence interval and interquartile range. b, Enrichment of neutrophil related gene sets of weighted gene co-expression network analysis (WGCNA) modules upregulated in SRS1. c, Correlation (and 95% confidence interval) of module 10 eigengene expression with percentage of immature neutrophils from mass cytometry (CyTOF) per sample of mmV. d, Leading edge analysis for enrichment of scWB derived IL1R2+ immature neutrophil defining signature in module 10. e, IL1R2+ immature neutrophil (top) and cycling neutrophil progenitor (bottom) proportions following total leukocyte bulk transcriptomics deconvolution of n = 542 sepsis patients (brWB-CID microarray data)5,18. Boxplots denote minimum and maximum with whiskers and bottom quartile, median and upper quartile with the box. f, Input data into MOFA+77 model consisting of three modalities (105 plasma proteins, 33 module eigengenes (eigen) from WGCNA and 22 cell clusters from CyTOF) for n = 36 sepsis samples with one and six missing samples for CyTOF and plasma proteomics respectively. g, Scatter-plots of latent factor values for sepsis patients. h, Factor values by SRS groups (two-sided Wilcoxon rank-sum test) (n = 26 SRS1, n = 16 non-SRS1). Violin plots with median, 95% confidence interval and interquartile range. i, Variance decomposition showing percentage variance explained for individual modalities by each latent factor. j, Latent factor two weights per cell cluster (top) and gene module (bottom). k, Latent factor one weights per cell cluster (top) and gene module (bottom). SRS, sepsis response signature; Neu, neutrophil; imm neu, immature neutrophil; int inf neu, intermediate inflammatory neutrophil; pro-neu, pro-neutrophil; pre neu, pre-neutrophil; cMono, classical monocyte; ncMono non-classical monocyte; intMono, intermediate monocyte; cMono_1; Ki67+, cMono_2: CD163+CD354+Ki67+, cMono_3: CD163+, cMono_4: CD354+Ki67+. NES, normalized enrichment score; FDR, false discovery rate. * FDR < 0.05, ** FDR < 0.01, **** FDR < 0.0001, NS, not significant.
Extended Data Fig. 8 Hematopoietic stem cell (HSC) SRS differential abundance (DA) and clusters C5 and C7 peak set analysis.
a, HSC DA across SRS with UMAP showing sampled neighborhoods colored by statistically significant enrichment (spatial FDR < 0.05). b, c, Volcano plots of differentially accessible (DA) peaks (fold change > 1.5, FDR < 0.05) for HSC (b) cluster C5 vs. all other clusters and (c) cluster C7 s. all other clusters (Wilcoxon rank-sum test). d, e, Enrichment of bulk ATAC-seq profiles in differentially open peaks for clusters (d) C5 (184 peaks) and (e) C7 (718 peaks). f, g, Enrichment of transcription factor (TF) motifs of differentially open peaks for clusters (f) C5 and (g) C7. h, ChIP-seq overlap analysis for cluster C7 differentially open peaks. The Giggle score denotes a composite significance and effect size scoring (doi:10.1038/nmeth.4556). Nhood, neighborhood; SRS, sepsis response signature; FDR, false discovery rate; ChIP, chromatin immunoprecipitation.
Extended Data Fig. 9 Hematopoietic stem cell (HSC) trajectory and vector field analysis, and transcription factor (TF) knockout and overexpression analysis.
a, UMAP of HSCs with supervised pseudotime trajectory from cluster C6 (HC enriched) to cluster C7 (sepsis but not SRS1 enriched). b, STAT3 and CEBPB gene expression with pseudotime. c, Genes (left) and TF motifs (right) which change along C6−C7 pseudotime trajectory and correlate with each other (Pearson’s r > 0.5, FDR < 0.05). d, CEBPA gene expression with pseudotime. e, CellOracle68 in silico knockout (top) and overexpression (bottom) of CEBPA and CEBPB and effects on clusters C5/6/7, with arrows displaying predicted changes in cell fate after gene of interest is perturbed (Methods). f–i, HSC clusters C5/6/7 vector field analysis with dynamo70. f, UMAP of HSC clusters C5/6/7 with RNA velocity stream directions plotted. g, RNA velocity based pseudotime of HSC clusters C5/6/7. h, dynamo acceleration and curvature vector fields. i, In silico knockout of CEBPA (left), CEBPB (middle) and STAT3 (right) and effects on clusters C5/6/7 with arrows displaying predicted changes in cell fate after gene of interest is perturbed. j, dynamo Jacobian analysis of gene-gene regulatory relationships. Scatter-plots show normalized expression values of genes of interest along x and y axes. Blue denotes inhibition of the numerator gene by the denominator gene in the Jacobian partial derivative, while red denotes activation of the numerator by the denominator.
Extended Data Fig. 10 SRS1 signatures across differing clinical contexts of infectious disease.
a–e, BrWB-CID contexts 2–7. a, Cycling neutrophil progenitor proportions following whole blood bulk transcriptomics deconvolution in 6 cohorts of infectious disease patients defined by infecting organism (n = 77 COVID-19 and n = 109 influenza, top), source of infection (n = 438 community acquired pneumonia and n = 229 fecal peritonitis, middle) and clinical syndrome (n = 77 adult acute respiratory distress syndrome (ARDS) and n = 106 pediatric septic shock, bottom). Boxplots denote minimum and maximum with whiskers and bottom quartile, median and upper quartile with the box. Two-sided Wilcoxon rank-sum test comparing SRS1 and non-SRS1 groups. b, Gene set enrichment analysis of scWB STAT3 gene expression programs (GEPs) (the union of all three GEPs, STAT3-union-GEP) in SRS1 upregulated genes for each of the 6 cohorts. c, IL1R2+ immature neutrophil proportions in COVID-19 whole blood scRNA-seq cohort (n = 8) after referencing mapping of dataset to scWB reference single cell atlas. d, Violin plots of scWB neutrophil STAT3 GEP expression in COVID-19 neutrophils as defined by scWB neutrophil states. Two-sided Wilcoxon rank-sum test comparing SRS1 and non-SRS1 groups. e, Violin plots of scWB neutrophil STAT3-union-GEP expression in all COVID-19 neutrophils. Two-sided Wilcoxon rank-sum test comparing SRS1 and non-SRS1 groups. SRS, sepsis response signature; Neu, neutrophil. *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001.
Supplementary information
Supplementary Information
Supplementary Note 1.
Supplementary Table 1
Clinical data for cohorts 1 and 3.
Supplementary Table 2
Antibodies used for cell surface protein profiling for scWB on BD Rhapsody platform.
Supplementary Table 3
Gene markers for each annotated cell type/state in scWB single-cell profiling and top 50 genes of each program for neutrophil states from scWB neutrophil consensus non-negative matrix factorization.
Supplementary Table 4
MsigDB Hallmark pathways and prostaglandin gene sets enriched from scWB neutrophil consensus non-negative matrix factorization.
Supplementary Table 5
Differentially accessible peaks (fold change > 1.5, FDR < 0.05) for HSC clusters C5 and C7.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kwok, A.J., Allcock, A., Ferreira, R.C. et al. Neutrophils and emergency granulopoiesis drive immune suppression and an extreme response endotype during sepsis. Nat Immunol 24, 767–779 (2023). https://doi.org/10.1038/s41590-023-01490-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41590-023-01490-5
This article is cited by
-
Dysregulation of neutrophil in sepsis: recent insights and advances
Cell Communication and Signaling (2025)
-
Astragaloside IV- loaded biomimetic nanoparticles target IκBα to regulate neutrophil extracellular trap formation for sepsis therapy
Journal of Nanobiotechnology (2025)
-
Neutrophil single-cell analysis identifies a type II interferon-related subset for predicting relapse of autoimmune small vessel vasculitis
Nature Communications (2025)
-
Monocyte-macrophage membrane expression of IL-1R2 is a severity biomarker in sepsis
Cell Death & Disease (2025)
-
β-Glucan reprograms neutrophils to promote disease tolerance against influenza A virus
Nature Immunology (2025)