Abstract
Limited evidence is available on apparent temperature (AT) and hospital admissions for acute cardiac events. We examined the associations of AT with admissions for acute cardiac events and acute coronary syndrome (ACS), and explored the effect difference between ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction ACS (NSTE-ACS). Poisson regression with distributed lag non-linear model was applied to examine the temperature-lag-admission associations. Stratified analyses were performed by gender and age-groups for acute cardiac events. A total of 11,657 acute cardiac events admissions were collected from hospital-based chest pain centers in Beijing, during 2017–2019. The single day effect of low AT (− 11 °C, 2.5th percentile) appeared on the 2nd day and persisted until the 11th day, with estimated relative risk (RR) ranging from 1.44 (95% CI: 1.159, 1.790) to 1.084 (95% CI: 1.022, 1.150) for acute cardiac events and from 1.034 (95% CI: 1.010, 1.059) to 1.006 (95% CI: 1.000, 1.011) for ACS. The single day effect of high AT (34 °C, 97.5th percentile) was only observed on the current day. The cold effect on acute cardiac events was more pronounced among female and older patients. The cumulative effect of high AT on STEMI admissions and low AT on NSTE-ACS reached a peak RR peak of 2.545 (95% CI: 1.016, 6.375) and 3.71 (95% CI: 1.315, 10.469) on lag 0–6 days, respectively. Both high and low ATs were associated with increased risk of acute cardiac events and ACS admissions. STEMI admissions may be more sensitive to high AT while NSTE-ACS to low AT.
Similar content being viewed by others
Introduction
Ranking the first cause of disability adjusted life years (DALYs) in 50-years-and-older population in 2019, ischemic heart disease (IHD) has been one of the ten most important drivers of increasing disease burden over the past three decades worldwide1. In China, IHD ranked the second leading cause of death and approximately 1.7 million deaths were attributable to IHD in 20162. Acute coronary syndrome (ACS) represents an acute manifestation of IHD with a high risk of death, encompassing unstable angina (UA), non-ST-elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI). According to the latest guidelines, UA and NSTEMI were categorized as non-ST-elevation acute coronary syndromes (NSTE-ACS) because of the similarity in clinical manifestation and management strategies3,4. Given the vital importance of immediate medical care for patients with urgent or emergent causes of ACS, it is necessary to identify some modifiable risk factors and take precautionary measures to avoid treatment delays as much as possible, which may help reduce the mortality.
Meteorological factors including ambient temperature, humidity, sunshine, atmospheric pressure, have been reported to be associated with mortality or morbidity of cardiovascular events such as myocardial infarction, out-of-hospital cardiac arrest5,6,7,8,9,10,11. Extreme temperatures were also linked to increased daily number of hospital admissions, emergency department visits and ambulance dispatches12,13,14,15,16. The chest pain is one of the most common chief complaint among the emergency department patients and is associated with potential life-threatening acute cardiac events. Although a number of studies have reported the association between temperature and morbidity of AMI (several were on STEMI), few studies investigated the association stratified by subtypes of AMI. Besides, previous studies indicated an important role for temperature in the incidence of ACS17. However, epidemiological studies evaluating the effect of temperature on incidence of ACS are relatively scarce, let alone on effect differences between STEMI and NSTE-ACS11,18,19,20,21,22. In view of a threefold increase in the rate of hospitalization for NSTEMI whereas a small reduction for STEMI, improving awareness of the preventive and medical care for NSTE-ACS is important23.
In addition, some studies proposed that raw temperature indicator may not accurately describe the true thermal effects, because human perception of ambient temperature depends on both temperature and other meteorological factors such as humidity and wind speed24,25. As a combination of meteorological indicators, including ambient temperature, relative humidity and wind velocity, apparent temperature (AT) has been proven to reflect the thermal sensations experienced by the human body more objectively than ambient temperature alone26. AT has been adopted to represent the combined exposure of temperature and humidity in several studies exploring the impact of temperature on mental health, behavior and some other diseases27,28,29. However, the study using AT to quantify relationship between temperature and onset of acute cardiac events has not yet been reported.
The aim of our study was to explore the impacts of AT on daily hospital admissions due to acute cardiac events in Beijing, China, from 2017 and 2019. Furthermore, we sought to explore whether the AT-admissions associations varied by gender, age and types of ACS.
Material and methods
Study area
Beijing is a typical northern city of China and is located at latitude 39°56′N and longitude 116°20′E, with a permanent population of 21.54 million in 2018 (Beijing Statistical Yearbook 2019 published by China Statistics Press). Beijing has a monsoon influenced humid continental climate with hot humid summers and cold windy dry winters. The annual average temperature ranges from 10 to 12 °C, with average daily minimum temperature of − 6 °C and average daily maximum temperature of 33 °C28,30.
Data collection
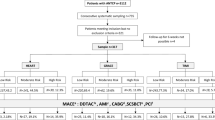
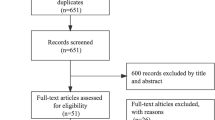
Data on admissions due to acute cardiac events in 10 hospital-based chest pain centers in Beijing from March 1st, 2017 to February 28th, 2019 were obtained from the China Chest Pain Center Data Reporting Platform (http://data.chinacpc.org/). All of the ten hospitals passed chest pain center accreditation in 2017 (rather than general hospital) and are designated hospitals for patients with an acute cardiac event in Beijing. Therefore, the data collected from China Chest Pain Center Data Reporting Platform is enough to represent patients with an acute cardiac event during the study period in Beijing. This data reporting platform served as a national surveillance system to evaluate the characteristics, treatments, and outcomes of patients hospitalized with acute cardiac events, launched by the Chinese Cardiovascular Association. To be eligible, we included data from those who meet the following criteria: (1) are aged 18 years or older; (2) are admitted by all kinds of modes including directly by self, via emergency medical services, transferred-in or in-hospital; (3) have a primary diagnosis of cardiogenic chest pain, including the STEMI, NSTEMI, UA, aortic dissection, pulmonary embolism, and others.
We derived meteorological data from the China Meteorological Data Sharing Service System (http://data.cma.cn/). Air pollution data including carbon monoxide (CO), nitrogen dioxide (NO2), particulate matter with aerodynamic diameter less than 10 µm (PM10), particulate matter with aerodynamic diameter less than 2.5 µm (PM2.5), sulfur dioxide (SO2) and ozone (O3) was collected from Beijing Municipal Ecological and Environmental Monitoring Center (http://www.bjmemc.com.cn/). We averaged the daily mean concentrations of air pollutants from the available monitoring data across seven national air monitoring stations evenly distributed in urban districts of Beijing. Extreme low and high daily temperatures are defined as those daily mean temperatures that fall below the 2.5th percentile and above the 97.5th percentile of the total daily apparent temperature distribution, respectively31,32. Using this percentile-based definition, the extreme low temperature threshold is less than or equal to − 11 °C, and the high extreme threshold is greater than or equal to 34 °C for the period studied.
Calculation of AT
The AT was calculated by the common meteorological indicators, including daily mean temperature, relative humidity, wind velocity and water vapor pressure using the following equations25,28,33:
In Eq. (1), T, e and WS denote the daily mean temperature (°C), water vapor pressure (hPa) and average wind velocity (m/s), respectively. The water vapor pressure e is calculated from Eq. (2) using the daily mean temperature and relative humidity (RH, %).
Statistic analysis
Firstly, a descriptive analysis was conducted for daily hospital admissions, meteorological variables and air pollutants datasets. Then, time series analyses were conducted to investigate the effects of exposure to extreme apparent temperature (low and high) on daily hospital admissions.
A generalized linear model (GLM) approach with a quasi-likelihood Poisson distribution for dispersion data was conducted to investigate the association between daily hospital admissions and extreme temperature conditions (both low and high). A natural cubic B-spline with seven degrees of freedom per year was used to control for the long-term trend and seasonal cycles32,34. The model included the following confounding factors: day of week (DOW), public holidays (Holiday), PM10 and O3. The lagged and potential non-linear effect of AT were evaluated by distributed lag non-linear model (DLNM)19,27,31,35 by adding a cross-basis function with up to 14 lag days, using a quadratic B-spline with three internal knots at the 10th, 75th, and 90th percentiles ___location of AT distributions and three knots in log response34,36.
A new metric Minimum Admission Apparent Temperature (MAAT) at minimum relative risk was defined in this study, which is similar to Minimum Mortality Temperature (MMT) defined by previous studies14,32. MAAT represents the minimum of the exposure–response or the temperature at the lowest risk obtained from specific model. Thus, the cold and heat effects were defined as the hospital admission risks at the 2.5th and 97.5th temperature percentiles, compared with the minimum-hospital admission temperature percentile. The approach is well documented37,38 and has been used to estimate the impact of temperature on mortality. Stratified analyses were performed by gender and age groups for acute cardiac events admissions. And the analyses for different diagnostic types of diseases (ACS, STEMI and NSTE-ACS) were also conducted through the above steps. The RR for each category was compared to the reference MAAT and reported with both 95% confidence intervals (CI). All statistical analyses were carried out in R software (version 3.6.3) using “dlnm” package38.
Ethical approval
Ethical approval for the study was obtained from the institutional review boards of the GUSU group ethics committee (GUSU19005), established by Chinese Cardiovascular Association. The need for informed consent was waived by the Institutional Review Board because the health information was primarily the hospital specific daily count of admissions, i.e., summarized data (overall, and by age and sex subgroups) without any individual identifiers. The study was performed in accordance with the Declaration of Helsinki.
Results
Descriptive statistics of daily admissions and meteorological variables
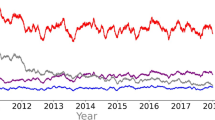
We included a total of 14,447 chest pain admissions (11,657 admissions were due to acute cardiac events) in 10 public hospitals in Beijing between March, 1st 2017 to February, 28th 2019 (730 days). Among these acute cardiac events admissions, male and patients aged above 65 years accounted for 65.1% and 42.3%, respectively (Table 1). The descriptive statistics for the meteorological and air pollution parameters were summarized in Table 2. Daily average AT was 11.9 °C, slightly lower than mean ambient temperature (13.8 °C). The time-series distribution of daily admissions due to acute cardiac events exhibited a seasonal pattern, with more hospital admissions due to acute cardiac events in lower temperature days (Fig. 1).
The impact of extreme low and high AT on daily admissions due to acute cardiac events
The exposure–response curves between AT and daily admissions due to chest pain were shown in Fig. 2, with MAAT of 23.0 °C (70.8th percentile) for all cause-chest pain and 22.0 °C (69.0th percentile) for acute cardiac events and, respectively. Both all cause-chest pain and acute cardiac events show more of a U type curve. Figure 3 showed non-linear relationships between AT and daily admissions for subtypes of ACS. The MAAT for STEMI and NSTE-ACS were found to be − 11 °C and 34 °C, respectively, suggesting that the extreme high AT tended to have a larger effect on admissions caused by STEMI while low extremes tended to have a greater effect on NSTE-ACS admissions.
Exposure–response relationship between apparent temperature (AT) and daily hospital admissions due to acute coronary syndrome (ACS) in disease-specific groups (with reference of the Minimum Admission Apparent Temperature, MAAT). Abbreviations: ACS, acute coronary syndrome; STEMI, ST-segment-elevated myocardial infarction; NSTE-ACS, Non-STEMI acute coronary syndrome. Notes: MAAT for ACS, STEMI and NSTE-ACS was − 10 °C, − 11 °C and 34 °C, respectively.
The single lag effect of low AT and high AT on subtype causes of chest pain were presented in Table 3. Both extreme low and high ATs were associated with increased risks (RR > 1) for all-cause chest pain, acute cardiac events and ACS compared with MAAT, whereas admissions caused by NSTE-ACS were only associated with increased risks at extreme high AT. The MAATs for chest pain admissions caused by STEMI and NSTE-ACS were − 11 °C and 34 °C, corresponding to the extreme low AT and extreme high AT in this study. Hence, we did not exhibit the results of cold effect and heat effect for them (RR = 1).
The single day effects of extreme low AT on admissions for all-cause chest pain, acute cardiac events and ACS could be observed from the 2nd day to the 11th day of exposure, but not continuously (Table 3). The highest risk associated with low AT for all three causes emerged on the 2nd day. While for extreme high AT, the single day effect was only observed on the 6th lag day for all-cause chest pain, and on the 1st lag day for acute cardiac events and ACS. For example, the risk of admission due to all-cause chest pain, acute cardiac events and ACS admission increased by 33.6% (RR = 1.336, 95% CI: 1.088–1.640), 44% (RR = 1.440, 95% CI: 1.159–1.790) and 3.4% (RR = 1.034, 95% CI: 1.010–1.059), respectively at the extreme low AT.
Table 4 provides the cumulative effect of exposure to extreme ATs compared with the reference. The cumulative effects of extreme high AT on STEMI admissions could be observed on the day of exposure until the 8th day, with RR varying from 3.308 (95% CI: 1.454, 7.526) at lag 0–1 days to 3.165 (95% CI: 1.015, 9.868) at lag 0–8 days. While for NSTE-ACS, the cumulative effects of extreme low AT could be observed on the 2nd day after exposure until the 7th day with RRs varying from 2.240 (95% CI: 1.086, 4.621) at lag 0–2 days of to 2.545 (95% CI: 1.016–6.375) at lag 0–6 days. However, we did not observe significant cumulative effects of extreme ATs for all-cause chest pain, acute cardiac events and ACS.
The effects of extreme low AT seemed to be more evident among the female and the patients aged over 65 years, compared with the male and the population aged below 65 years, respectively (Figs. 4, 5, Tables S1, S2). For instance, the maximum RR of cold effect were 1.718 (95% CI: 1.151, 2.564) for patients aged over 65 years at the 2nd lag day while 1.410 (95% CI: 1.085, 1.833) for patients aged below 65 years. The highest RR was 1.785 (95% CI: 1.126, 2.831) for the female and 1.499 (95% CI: 1.165, 1.930) for the male. However, the cold effect for patients below 65 years and the male were longer lasting and could still be observed at lag 8–11 days. With respect to heat effect, the highest RR was observed for patients below 65 on the current day of exposure (RR = 1.704, 95% CI: 1.195, 2.429).
The single day effects of extreme apparent temperature for admissions due to acute cardiac events cross different lag day(s) in gender-specific groups, with the reference of the Minimum Admission Apparent Temperature (MAAT) of each group. Notes: MAAT for male and female group was 33 °C and 22 °C, respectively.
Discussion
Our findings support non-linear relationships between AT and chest pain admissions caused by ACS (including STEMI and NSTE-ACS), such that the risk of acute cardiac events onset is higher at both extreme high and low ATs relative to the MAAT. The effect of low AT on acute cardiac event admissions appeared one day after the exposure and can still be observed on the 8th and 11th days after the exposure whereas the effect of high AT was immediate and relatively short-lived. In addition, the current study found that MAAT of STEMI is close to extreme low temperatures, indicating increased risks at high temperature. Conversely, the minimum risk temperature of NSTE-ACS is close to extreme high temperatures, indicating that extreme low AT tend to have significant effect on NSTE-ACS rather than high AT.
Overall, our findings contribute to the limited epidemiological evidence for the adverse effects of non-optimum extreme temperatures on the onset of acute cardiac events and incidence of ACS in the area of subtropical monsoon climate, and may be of major population and clinical implications. We adopted the new comprehensive index of AT as a potential warning index, which may be a more realistic and objective measure than ambient temperature alone. The associations of extreme ATs with acute cardiac events admissions may offer implications regarding mobilization and improved utilization of public and emergency resources in the city. For example, in high- or low-temperature weather conditions, public service announcement or ads and banners could be used to alert the public. Similarly, emergency medical system and emergency medical staff could also be alerted for a possible surge in calls and services. Adaptation strategies such as using air conditioners in summer and adequate hydration should be considered. Although the risk of climate and environmental triggers to any single individual is relatively small compared with the effect of well-documented risk factors (e.g. smoking), the public health relevance is considerable, and small percentage increases can translate into substantial absolute increases, because the incidence of chest pain are common and exposure to temperature can be ubiquitous.
Our findings are consistent with several studies reporting the impact of extreme temperature on admissions due to ACS or chest pain. A study exploring impact of extreme temperatures on ambulance dispatches in London reported that the minimum ambulance dispatch temperature (TMADT) for chest pain was less than the 1st temperature percentile and found increased risks only at higher temperature. Whereas the TMADT for acute cardiac events was above the 99th percentile indicating increased risks only at higher temperatures14. Our study showed that the TMAAT for all-cause chest pain (23 °C) and acute cardiac events (22 °C) admissions were close to each other. We found significant increased risks for both at extreme low and high ATs, and the RRs for acute cardiac events were larger than those for all-cause chest pain. In addition, the heat effect for acute cardiac events could be observed on the current day while it could not be observed until on the 6th day after exposure for all-cause chest pain. This inconsistency in research findings could be due to the major difference in dataset used, study population, analytical method as well as temporal and spatial properties.
Our results did not find cumulative effects of extreme ATs on acute cardiac events admissions though they showed large RR values for cold effect on the second day after exposure and on the present day for heat effect. This might be inconsistent with what past studies found with their data. One possible explanation is that widespread use of central heating system in Beijing, a typical northern city in China, have improved the adaptation to cold ambient temperature in winter and usage of air conditioner in summer could relieve the hot stress in summer39,40. Besides, the ethnicity of the study participants, the climatic conditions of study area and the environmental background may contribute to the differences in the results41. These discrepant findings indicate that further large-scale epidemiological studies and subsequent meta-analyses are thus needed in different climate zones to determine these relationships with certainty.
In addition, the present study observed larger size of cold effect estimates in those over 65 years old. Several previous studies reported similar findings that extremely low temperature was more likely to induce an acute cardiovascular event in susceptible individuals such as the elderly18,26,41,42,43,44. A possible explanation for this increased susceptibility in the elderly relates to a reduced thermoregulation, together with a decreased capacity in perception of changes in body temperature42,45.
A novelty of this study is the comparative investigation on the relationship between AT and specific subtypes of time-sensitive acute cardiac events and ACS (STEMI and NSTEACS) whilst most previous studies have examined emergency department visits in general or a single disease (e.g. STEMI, AMI). There is no agreed conclusion about how effects of temperature may vary on different subtypes of ACS. In the present study, admissions due to STEMI was only affected by extreme high AT while NSTE-ACS admission was found to be only affected by extreme low AT. Contrary to the association of AT and STEMI in the present study, a study conducted in two large Italian urban areas reported that colder days were the days of higher risk of STEMI6. However, a research from Japan found that both lower mean temperature and increased maximum temperature from the previous day were independently associated with the STEMI occurrence throughout the year46. With regard to the difference between the impact of temperature on STEMI and NSTEMI, a study comparing the seasonal variation of STEMI and NSTEMI in Israel demonstrated significant increases in STEMI cases during the winter months whereas no statistically significant differences in the seasonal variation were found for NSTEMI47. Furthermore, seasonal variations in the incidence of ACS could reflect differences in the underlying pathobiology48. Although our results are not the same, these findings do support the concept that the underlying pathophysiology of STEMI is different than that of remaining types of ACS. And inconsistency in these findings merits further investigation focusing especially on the comparative investigation of differences in relationship between temperature and subtypes of ACS. Also, further larger scale original studies or systematic reviews concerning the causal effect of short-term exposure to extreme temperature on subtypes of ACS risk are needed to resolve this discrepancy.
Another novelty in the present study is that we employ a biometeorological index AT as exposure measurement to evaluate the effects of temperature on acute cardiac events, rather than daily mean, minimum or maximum temperature. Human body is exposed to a set of atmospheric parameters simultaneously and AT could capture the reaction of the human body to the combined conditions of the thermal environment. It has been used in some studies exploring the impact of ambient temperature on mental and behavioral health24,27,28 and identified as the main predictor of heat-related mortality49. To date, however, the relationship between AT and admissions due to acute cardiac events or ACS has not been reported in literature. Compared with previous studies using daily mean temperature as exposure variable, AT can provide a measure of the combined effect of environmental variables on human health and wellbeing, and can estimate the human perception of temperature50.
There are several potential limitations of this study. First, this is a retrospective ecological study and the ecologic fallacy cannot be ruled out. While causation cannot be directly inferred from our work, ATs were all individually capable of predicting risk well before the adverse event. Second, the single-center and relatively small sample size of this study may limit the generalization of these findings to the whole population. And thus, the association of AT with acute cardiac events and whether the effect varies by subtypes of ACS should be explored in future studies. Third, meteorological data were extracted from fixed monitoring sites rather than individual exposure measures, which may lead to measurement errors. However, we linked the daily emergency admissions of each hospital to the daily meteorological measures in the corresponding district to minimize the misclassification. Fourth, seasonal influenza was associated with an increase in MI-associated deaths and hospitalizations in previous studies51. However, our analysis failed to control for influenza as a possible confounder due to the unavailability of data, and the results may show an overestimate of the effect in cold seasons.
Conclusion
Both high and low extreme ATs were found to be risk factors for hospital admissions due to acute cardiac events and ACS. The study also observed detrimental effect of high extreme AT on STEMI and low extreme AT on NSTE-ACS. These findings may help better understand the relationship between temperature and the onset of acute cardiac events, and will contribute to developing public health intervention measures, as well as planning of clinical service and emergency resources to reduce mortality caused by untimely emergency treatment in ACS patients. Further multi-center studies aiming to differentiate the effect of non-optimal temperature on ACS subtypes are warranted.
Data availability
The associated study protocol and data collection tools will be made available upon request from the corresponding author. Datasets are partly available from the corresponding author upon reasonable request after the completion of primary analyses and results dissemination.
References
GBD. Risk Factors Collaborators. 2020. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet 396, 1223–1249 (2019).
Zhou, M. et al. Mortality, morbidity, and risk factors in china and its provinces, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet 394, 1145–1158 (2019).
Amsterdam, E. A. et al. 2014 aha/acc guideline for the management of patients with non-st-elevation acute coronary syndromes: Executive summary: A report of the American college of cardiology/American heart association task force on practice guidelines. Circulation 130, 2354–2394 (2014).
Chinese Society of Cardiology, Editorial Board of Chinese Journal of Cardiology. CSC guidelines for the diagnosis and treatment of acute coronary syndromes in patients presenting without persistent st-segment elevation. Chin. J. Cardiol. 5 (2017).
Abrignani, M. G. et al. Effects of ambient temperature, humidity, and other meteorological variables on hospital admissions for angina pectoris. Eur. J. Prev. Cardiol. 19, 342–348 (2012).
Biondi-Zoccai, G. et al. Impact of environmental pollution and weather changes on the incidence of st-elevation myocardial infarction. Eur. J. Prev. Cardiol. https://doi.org/10.1177/2047487320928450 (2020).
Cannistraci, C. V., Nieminen, T., Nishi, M., Khachigian, L. M., Viikila, J., Laine, M., et al. "Summer shift": A potential effect of sunshine on the time onset of st-elevation acute myocardial infarction. J. Am. Heart Assoc. 7 (2018).
Claeys, M. J., Rajagopalan, S., Nawrot, T. S. & Brook, R. D. Climate and environmental triggers of acute myocardial infarction. Eur. Heart J. 38, 955–960 (2017).
Hong, Y., Graham, M. M., Rosychuk, R. J., Southern, D. & McMurtry, M. S. The effects of acute atmospheric pressure changes on the occurrence of st-elevation myocardial infarction: A case-crossover study. Can. J. Cardiol. 35, 753–760 (2019).
Ma, Y. et al. Short-term effect of extreme air temperature on hospital emergency room visits for cardiovascular diseases from 2009 to 2012 in Beijing, China. Environ. Sci. Pollut. Res. Int. 27, 38029–38037 (2020).
Vasconcelos, J., Freire, E., Almendra, R., Silva, G. L. & Santana, P. The impact of winter cold weather on acute myocardial infarctions in Portugal. Environ Pollut 183, 14–18 (2013).
Cheng, J. et al. Assessment of heat- and cold-related emergency department visits in cities of china and Australia: Population vulnerability and attributable burden. Environ. Res. 166, 610–619 (2018).
Hu, J., Wen, Y., Duan, Y., Yan, S., Liao, Y., Pan, H., et al. The impact of extreme heat and heat waves on emergency ambulance dispatches due to external cause in Shenzhen, China. Environ. Pollut. 261, 114156 (2020).
Sangkharat, K., Mahmood, M. A., Thornes, J. E., Fisher, P. A. & Pope, F. D. Impact of extreme temperatures on ambulance dispatches in London, UK. Environ. Res. 182, 109100 (2020).
Williams, A. A., Allen, J. G., Catalano, P. J., Buonocore, J. J. & Spengler, J. D. The influence of heat on daily police, medical, and fire dispatches in Boston, Massachusetts: Relative risk and time-series analyses. Am. J. Public Health 110, 662–668 (2020).
Wong, H. T. & Lin, J. J. The effects of weather on daily emergency ambulance service demand in Taipei: A comparison with Hong Kong. Theor. Appl. Climatol. https://doi.org/10.1007/s00704-020-03213-4:1-10 (2020).
Hodzic, E., Perla, S., Iglica, A. & Vucijak, M. Seasonal incidence of acute coronary syndrome and its features. Mater. Sociomed. 30, 10–14 (2018).
Guo, S. et al. Association between ambient temperature and daily emergency hospitalizations for acute coronary syndrome in Yancheng, China. Environ. Sci. Pollut. Res. Int. 27, 3885–3891 (2020).
Lam, H. C. Y., Chan, J. C. N., Luk, A. O. Y., Chan, E. Y. Y. & Goggins, W. B. Short-term association between ambient temperature and acute myocardial infarction hospitalizations for diabetes mellitus patients: A time series study. PLoS Med. 15, e1002612 (2018).
Mohammadi, R., Soori, H., Alipour, A., Bitaraf, E. & Khodakarim, S. The impact of ambient temperature on acute myocardial infarction admissions in Tehran, Iran. J. Therm. Biol. 73, 24–31 (2018).
Nastos, P. T., Giaouzaki, K. N., Kampanis, N. A. & Matzarakis, A. Acute coronary syndromes related to bio-climate in a mediterranean area. The case of ierapetra, Crete Island, Greece. Int. J. Environ. Health Res. 23, 76–90 (2013).
Thu Dang, T. A. et al. Short-term effects of temperature on hospital admissions for acute myocardial infarction: A comparison between two neighboring climate zones in Vietnam. Environ Res 175, 167–177 (2019).
Zhao, D., Liu, J., Wang, M., Zhang, X. & Zhou, M. Epidemiology of cardiovascular disease in China: Current features and implications. Nat Rev Cardiol 16, 203–212 (2019).
Basu, R., Gavin, L., Pearson, D., Ebisu, K. & Malig, B. Examining the association between apparent temperature and mental health-related emergency room visits in California. Am. J. Epidemiol. 187, 726–735 (2018).
Steadman, R. G. Norms of apparent temperature in Australia. Aust. Meteorol. Mag. 43, 1–16 (1994).
Baccini, M. et al. Heat effects on mortality in 15 European cities. Epidemiology 19, 711–719 (2008).
Liu, X., Wen, Y., Zhang, K., Duan, Y., Li, H., Yan, S., et al. Examining the association between apparent temperature and incidence of acute excessive drinking in Shenzhen, China. Sci. Total Environ. 741, 140302 (2020).
Niu, Y., Gao, Y., Yang, J., Qi, L., Xue, T., Guo, M., et al. Short-term effect of apparent temperature on daily emergency visits for mental and behavioral disorders in Beijing, China: A time-series study. Sci. Total Environ. 733, 139040 (2020).
Wiru, K. et al. The influence of apparent temperature on mortality in the kintampo health and demographic surveillance area in the middle belt of Ghana: A retrospective time-series analysis. J. Environ. Public Health 2020, 5980313 (2020).
Beijing Meteorological Service. Available: http://bj.cma.gov.cn/. Accessed 16th June 2021.
Chen, R., Yin, P., Wang, L., Liu, C., Niu, Y., Wang, W., et al. Association between ambient temperature and mortality risk and burden: Time series study in 272 main Chinese cities. BMJ 363, k4306 (2018).
Gasparrini, A. et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 386, 369–375 (2015).
Krstic, G. Apparent temperature and air pollution vs. Elderly population mortality in metro Vancouver. PLoS ONE 6, 25101 (2011).
Yang, J. et al. The burden of stroke mortality attributable to cold and hot ambient temperatures: Epidemiological evidence from china. Environ Int 92–93, 232–238 (2016).
Luo, Y. et al. The cold effect of ambient temperature on ischemic and hemorrhagic stroke hospital admissions: A large database study in Beijing, china between years 2013 and 2014-utilizing a distributed lag non-linear analysis. Environ. Pollut. 232, 90–96 (2018).
Gasparrini, A. & Leone, M. Attributable risk from distributed lag models. BMC Med. Res. Methodol. 14 (2014).
Gasparrini, A., Armstrong, B. & Kenward, M. G. Distributed lag non-linear models. Stat. Med. 29, 2224–2234 (2010).
Gasparrini, A. Distributed lag linear and non-linear models in r: The package dlnm. J. Stat. Softw. 43, 1–20 (2011).
Ma, W., Chen, R. & Kan, H. Temperature-related mortality in 17 large Chinese cities: How heat and cold affect mortality in China. Environ. Res. 134, 127–133 (2014).
Ostro, B., Rauch, S., Green, R., Malig, B. & Basu, R. The effects of temperature and use of air conditioning on hospitalizations. Am. J. Epidemiol. 172, 1053–1061 (2010).
Wang, X. et al. Association between air temperature and the incidence of acute coronary heart disease in Northeast China. Clin Interv Aging 15, 47–52 (2020).
Medina-Ramon, M., Zanobetti, A., Cavanagh, D. P. & Schwartz, J. Extreme temperatures and mortality: Assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ. Health Perspect. 114, 1331–1336 (2006).
Stafoggia, M. et al. Vulnerability to heat-related mortality: A multicity, population-based, case-crossover analysis. Epidemiology 17, 315–323 (2006).
Zheng, S., Wang, M., Li, B., Wang, S., He, S., Yin, L., et al. Gender, age and season as modifiers of the effects of diurnal temperature range on emergency room admissions for cause-specific cardiovascular disease among the elderly in Beijing. Int. J. Environ. Res. Public Health 13 (2016).
Mercer, J. B. Cold—An underrated risk factor for health. Environ. Res. 92, 8–13 (2003).
Yamaji, K. et al. Relation of st-segment elevation myocardial infarction to daily ambient temperature and air pollutant levels in a Japanese nationwide percutaneous coronary intervention registry. Am. J. Cardiol. 119, 872–880 (2017).
Leibowitz, D., Planer, D., Weiss, T. & Rott, D. Seasonal variation in myocardial infarction is limited to patients with st-elevations on admission. Chronobiol. Int. 24, 1241–1247 (2007).
Kurihara, O., Takano, M., Yamamoto, E., Yonetsu, T., Kakuta, T., Soeda, T., et al. Seasonal variations in the pathogenesis of acute coronary syndromes. J. Am. Heart Assoc. 9, e015579 (2020).
Zhang, K., Li, Y., Schwartz, J. D. & O’Neill, M. S. What weather variables are important in predicting heat-related mortality? A new application of statistical learning methods. Environ. Res. 132, 350–359 (2014).
Roye, D., Zarrabeitia, M. T., Fdez-Arroyabe, P., Alvarez Gutierrez, A. & Santurtun, A. Role of apparent temperature and air pollutants in hospital admissions for acute myocardial infarction in the North of Spain. Rev. Esp. Cardiol. (Engl. Ed.) 72, 634–640 (2019).
Warren-Gash, C. et al. Circulating influenza virus, climatic factors, and acute myocardial infarction: A time series study in England and Wales and Hong Kong. J Infect Dis 203, 1710–1718 (2011).
Acknowledgements
We thank the China Chest Pain Center Headquarters who helped guide this study. We appreciate Yi Wang at the China Chest Pain Center Headquarters for the assistance in developing and implementing this study.
Funding
This study is funded by the Beijing Natural Science Foundation (No. 9204025). The study sponsor has no role in study design, data analysis and interpretation of data, the writing of manuscript, or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
Z.Z. and J.Y. developed the study design. L.N. drafted the study protocol. M.J., Z.Y., M.P. and L.F. revised the study protocol. J.Y. and L.N. developed the analytic and statistical plan. All authors participated in the study implementation and have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, N., Ma, J., Liu, F. et al. Associations of apparent temperature with acute cardiac events and subtypes of acute coronary syndromes in Beijing, China. Sci Rep 11, 15229 (2021). https://doi.org/10.1038/s41598-021-94738-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-94738-9
This article is cited by
-
Effect of PM2.5 and its constituents on hospital admissions for cardiometabolic multimorbidity in Urumqi, China
Scientific Reports (2025)
-
Thermal indices for assessing the impact of outdoor thermal environments on human health: a systematic review of epidemiological studies
International Journal of Biometeorology (2025)
-
The impact of apparent temperature on the emergency visits for traumatic fractures in Hangzhou, China
BMC Public Health (2024)
-
Investigating the impact of extreme weather events and related indicators on cardiometabolic multimorbidity
Archives of Public Health (2024)
-
Exploring the relationship between land use/land cover and apparent temperature in China (1996–2020): implications for urban planning
Scientific Reports (2024)