Abstract
Despite the increasing burden of hypertrophic cardiomyopathy (HCM) on healthcare resources, data on emergency department (ED) utilization in HCM are lacking. This nationwide population-based study extracted 14,542 HCM patients from the National Health Insurance Service database between 2015–2016, and investigated their ED utilization during a one-year period. The reason for ED utilization was defined as the primary diagnosis upon discharge from EDs. The clinical outcome was defined as hospitalization or all-cause mortality within 90 days after the ED visits. A total of 3209 (22.1%) HCM patients visited EDs within a one-year period (mean age, 66.8 ± 13.8 years; male, 57.4%). The majority (71.1%) of HCM patients who visited the EDs were aged ≥ 60 years. The ED utilization rate was higher in women than in men (26.3% versus 19.7%, P < 0.001). Cardiovascular diseases were the most common reason for ED visits (n = 1333, 41.5%). Among HCM patients who visited EDs, 1195 (37.2%) were hospitalized, and 231 (7.2%) died within 90 days. ED visits for cardiovascular disease was associated with a higher 90-day all-cause mortality (adjusted odds ratio, 2.72; 95% confidence interval 1.79–4.12). These findings would serve as a basis for future research to establish medical policies on ED utilization in HCM.
Similar content being viewed by others
Introduction
Hypertrophic cardiomyopathy (HCM) is a genetic cardiomyopathy caused by sarcomeric gene mutations with autosomal dominant transmission1. Epidemiologic studies have reported that the prevalence of HCM is about 0.2% in the general population, but its prevalence seems to be increasing2,3. Over the last decade, HCM has been highlighted as a major cause of sudden cardiac death in young adults4,5, and most research on HCM has focused on early diagnosis and risk stratification to prevent sudden cardiac death6,7,8. Thanks to recent progress in the management of HCM, however, the life expectancy of patients with HCM has significantly increased, leading to changes in the main causes of morbidity and mortality in HCM population9.
The emergency department (ED) provides an important source of medical care, and the number of visits to the ED has significantly increased, disproportionately exceeding the growth of the general population10. Considering the expanded lifespan of HCM patients, the utilization of EDs is expected to progressively increase, which will inevitably be accompanied by a dramatic increase in the cost of healthcare10. Given this situation, understanding the utilization of EDs in this population is of practical value from the perspective of medical resource allocation.
This study aimed to investigate the characteristics of ED utilization in HCM patients in the era of contemporary management and explore the outcomes of those who were discharged from EDs.
Results
Baseline characteristics
A total of 3209 patients visited EDs within the specified one-year period (average age, 66.8 ± 13.8 years; male, 57.4%). The majority of HCM patients who visited the EDs were ≥ 60 years old (n = 2281, 71.1%). This was especially true for women, in whom the proportion of patients aged ≥ 60 years approached 84.5% (n = 1154) (Supplementary Fig. 1).
Compared to those who did not visit EDs, HCM patients who visited EDs had a higher proportion with low-income status, and had a higher prevalence of comorbidities such as hypertension, diabetes mellitus, heart failure, stroke/transient ischemic attack (TIA)/thromboembolism, myocardial infarction, atrial fibrillation/flutter, chronic obstructive pulmonary disease, and chronic kidney disease (Table 1). Among HCM patients who visited EDs, 836 of 855 (97.8%) patients with a history of stroke/TIA/thromboembolism were on oral anticoagulants, whereas among those who did not visit EDs, 1316 of 1629 (80.8%) were taking oral anticoagulants. A history of implantable cardioverter-defibrillator (ICD) implantation was more frequently reported in HCM patients who visited EDs than those who did not (n = 75, 2.34% versus. n = 210, 1.85%, P = 0.047). The duration of disease in those who visited EDs was significantly shorter than that in those who did not (61.3 ± 65.6 months versus 70.0 ± 64.4 months, P < 0.001).
EDs utilization
During the specified one-year period, 8.8 HCM patients per day utilized EDs. Annual ED visit rate was 22.1% (3209 out of 14,542); 16.8% (928 out of 5513) by HCM patients aged < 60 years, and 25.3% (2281 out of 9029) of those aged ≥ 60 years. Overall, the ED visit rate was significantly higher in women than in men (1366 out of 5188, 26.3% versus 1843 out of 9354, 19.7%, P < 0.001). Higher ED visit rates in women were consistent in almost all age groups (Fig. 1).
The average number of ED utilization per year was 1.7 ± 1.8, and most of these patients (n = 2061, 64.2%) utilized EDs only once during a 1-year follow-up period. There were 107 (3.33%) HCM patients who visited EDs more than four times a year. HCM patients in their 20 s had the lowest frequency of ED utilization (1.4 ± 0.6), while those in their 30 s had the highest frequency (2.0 ± 2.6), followed by those in their 40 s (1.8 ± 4.3), 50 s (1.6 ± 1.3), and those 60 or over (1.7 ± 1.4) without a statistical difference between them. (Supplementary Table 2).
Among the disease categories according to the primary diagnosis upon discharge from the EDs, cardiovascular disease was the most frequently reported primary reason for ED utilization (n = 1344, 41.9%) irrespective of age category (n = 359, 38.7% for patients aged < 60 years; n = 985, 43.2% for patients aged ≥ 60 years) (Supplementary Table 3). Within the category of the cardiovascular disease, HCM was the most common single diagnosis in patients aged both < 60 years (n = 273, 29.4%) and ≥ 60 years (n = 557, 24.4%), followed by cerebrovascular event (n = 38, 4.1% and n = 177, 7.8%, respectively), arrhythmia (n = 34, 3.7% and n = 97, 4.3%, respectively), and heart failure (n = 6, 0.7% and n = 56, 2.5%, respectively) (Fig. 2). Atrial fibrillation/flutter as an individual diagnosis accounted for half of arrhythmias in patients aged < 60 years (n = 17, 50.0%) and over half in those aged ≥ 60 years (n = 60, 61.9%). Detailed diagnoses for cerebrovascular events and arrhythmias based on International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10-CM) codes are described in Supplementary Table 4.
Undiagnosed cardiovascular symptoms including chest pain, dizziness, palpitations, dyspnea, and syncope, recorded as the presenting complaint at discharge, accounted for 8.4% (n = 268) of the primary diagnosis of all the ED visits; 9.3% (n = 86) in those aged < 60 years, and 8.0% (n = 182) in those aged ≥ 60 years (Supplementary Table 3). Among undiagnosed cardiovascular symptoms, chest pain was the most common in both patients aged < 60 years (n = 45, 4.9%), and those aged ≥ 60 years (n = 79, 3.5%), followed by dizziness (n = 19, 2.1% and n = 47, 2.1%, respectively). The third most common undiagnosed cardiovascular symptom in patients aged < 60 years was palpitations (n = 9, 1.0%), while it was syncope in those aged ≥ 60 years (n = 25, 1.1%) (Fig. 2).
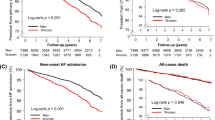
Short-term outcomes after ED utilization
Of 3209 HCM patients who visited EDs, 1195 (37.2%) were hospitalized, and 231 (7.2%) died within 90 days of ED discharge. Of the 231 deaths, cardiovascular causes accounted for 123 (53.2%). Among patients aged 60 years and above, 105 of 207 (50.7%) died from cardiovascular causes, whereas only 30 (14.5%) died from cancer (Supplementary Table 5). HCM patients aged ≥ 60 years were associated with a higher 90-day hospitalization (adjusted odds ratio [OR] 1.78, 95% confidence interval [CI] 1.48–2.14) and all-cause mortality (adjusted OR 3.30, 95% CI 2.10–5.18). Sex difference in mortality was also noted; men had higher all-cause mortality than women within 90 days after ED discharge (adjusted OR 1.35, 95% CI 1.01–1.80). Among the pre-specified subgroups, those with a previous history of stroke/TIA/thromboembolism and atrial fibrillation/flutter, and ICD implantation were significantly associated with a higher 90-day hospitalization rate (Table 2). In addition, HCM patients who visited EDs for cardiovascular disease showed a significant association with a higher 90-day all-cause mortality (adjusted OR 2.72, 95% CI 1.79–4.12).
Discussion
This study provides some important epidemiological findings in patients with HCM in terms of ED utilization. The annual ED visit rate of HCM patients was 22.1%, in whom elderly HCM patients aged ≥ 60 years accounted for more than two-thirds of total ED utilization. Among the HCM patients who visited EDs, 37.2% were hospitalized, and 7.2% died within 90 days after discharge from EDs. As expected, elderly patients aged ≥ 60 years were associated with a higher 90-day hospitalization rate and all-cause mortality. Of note, the proportion of ED visits was significantly and consistently higher in women than in men at almost all age groups, and men were associated with higher all-cause mortality. The most common reasons for ED utilization in HCM patients were the manifestations of cardiovascular diseases. More importantly, patients visiting EDs for cardiovascular disease had a higher all-cause mortality rate within 90 days after discharge from EDs compared to those for non-cardiovascular disease.
ED utilization is progressively increasing around the world, and thus overcrowding in EDs is now a global issue11,12. In addition to the increase in the volume of ED visits exceeding the growth rate of the population, medical costs per ED visit have also significantly increased13. Cardiovascular diseases were previously reported to be one of the most common reasons for ED utilization11. This study, which included HCM patients, also demonstrated that the most common disease category for ED utilization was cardiovascular disease. Given the increased longevity of HCM patients, this observation is not surprising, and we can also expect that cardiovascular events other than sudden cardiac death will be increasing in HCM patients as the main reason for ED utilization in the upcoming era. More importantly, this study noted that ED utilization due to cardiovascular diseases was associated with an increase in the 90-day all-cause mortality after ED discharge, and therefore, further studies for improving the prognosis in these patients are warranted.
The diagnosis of HCM is increasing in the elderly population, possibly owing to advanced imaging modalities and enhanced physician awareness3,14. Many observational cohort studies have found that most patients with HCM can enjoy a normal life expectancy without functional disability related to disease-associated clinical events nor the necessity for therapeutic intervention14,15,16. On the contrary, the current study has two different revelations; i) older HCM patients visiting EDs and ii) a higher frequency of comorbidities. It has been reported that elderly HCM patients carry multiple chronic comorbidities, which inevitably lead to frequent utilization of EDs17. In fact, the present study demonstrated that a quarter of HCM patients aged ≥ 60 years visited EDs at least once a year, and they accounted for more than 70% of the total HCM population who utilized EDs. Particularly, we found that HCM patients who visited EDs were not only older but had a higher prevalence of comorbidities such as hypertension, diabetes mellitus, heart failure, stroke/TIA/thromboembolism, myocardial infarction, atrial fibrillation/flutter, chronic obstructive pulmonary disease, and chronic kidney disease compared to those who did not visit EDs. When these facts are taken together, it is not surprising that HCM patients who visited EDs, especially elderly patients, had a higher hospitalization rate and all-cause mortality within 90 days after ED visits. Therefore, given the increasing frequency of HCM diagnosis and frequent ED utilization in the elderly HCM population, it is the right moment to discuss healthcare strategy for this population, which can be helpful for providing enhanced medical care and reducing the frequency of ED utilization, and ultimately improving their prognosis18.
Whereas the prevalence of HCM is higher in men in the general population, women with HCM tend to be older and have more symptoms with greater impairment in exercise performance and more frequent sudden cardiac death events compared to men with HCM6,19,20. We observed in the present study that the annual ED visit rate was significantly higher in women than in men. Moreover, the proportion of ED visits was consistently higher in women than in men at almost all age groups. These findings are in line with those of previous studies reporting the presence of sex differences in ED utilization21,22, implying the vulnerability of female HCM patients23. However, all-cause mortality within 90 days after ED visits was significantly higher in male HCM patients. This finding contrasts with previous observations showing no difference in HCM-related mortality between men and women in the general HCM population23,24. Sex differences in all-cause mortality after discharge from ED might be attributed to a variety of factors, such as disease severity and the presence of comorbidities25,26. Specifically, compared to the previous study23, HCM patients enrolled here were older and thus had a higher incidence of comorbidities such as hypertension, heart failure, and coronary artery disease like myocardial infarction, which could lead to an increase in non-HCM related mortality. Therefore, men with HCM (esp. those aged ≥ 60 years) who visited EDs with several comorbidities need to be regarded as those at increased risk and should be monitored closely. Further studies are required to investigate factors that are associated with sex differences in ED-related prognosis.
Ischemic stroke and atrial fibrillation/flutter are well-known complications of HCM27. In the current study, cerebrovascular events and arrhythmias were the second and third most common primary diagnoses upon discharge from EDs. Particularly, stroke is a devastating event leading to death or severe disability and has been reported to occur more frequently in HCM patients with atrial fibrillation/flutter than in those without27,28. In this respect, every effort should be made in HCM patients to detect atrial fibrillation/flutter early, and establish effective anticoagulation therapy in the outpatient clinic for preventing embolic events; this will lead to reduced stroke rates and less frequent ED utilization in HCM patients, finally helping to reduce medical costs and improve prognosis29,30.
Though once regarded as a rare, intractable condition with a grave prognosis and limited management options, HCM is now recognized as a worldwide, relatively common, and treatable form of genetic cardiomyopathy31. As HCM affects approximately 20 million people worldwide, the volume of patients presenting to the ED for management of acute problems is also expected to increase4. To the best of our knowledge, this is the first study to investigate and characterize the pattern of ED utilization in HCM patients. We expect our findings to serve as a basis for future research on high-risk HCM patients for ED utilization to better establish medical resource allocation policies. Moreover, future studies must focus on what preventive strategies are needed to reduce ED utilization of elderly HCM subjects with the better clinical management of comorbidities.
Several limitations need to be addressed. First, the current nationwide cohort study only included patients who had a record of HCM diagnosis in the NHIS database between 2015 and 2016 and reviewed their one-year history of ED utilization. Hence, data on annual trends, long-term and subsequent prognosis were not available. Second, the inherent limitation of the NHIS claims database did not allow for detailed data on special investigations such as echocardiography or electrocardiography, as well as information on a history of ICD shock and the ___location and circumstances of death. Thus, the minor possibility of misdiagnosis cannot be completely excluded. However, the diagnosis of HCM was formally verified with reviews by independent medical experts and healthcare professionals according to a governmental act on national health insurance. Besides, we also previously performed validation of the diagnosis27. Finally, due to the nature of claims data on ED utilization, only the main diagnosis recorded was used for analysis.
Conclusion
In conclusion, we can state that a quarter of HCM patients utilized EDs at least once a year after HCM diagnosis. Cardiovascular diseases such as cerebrovascular events, arrhythmias, and heart failure were the most common reasons for ED utilization. Thus, given the expanded life expectancy and improved preventive strategies for sudden cardiac death associated with HCM, greater emphasis should be placed on the continued surveillance of risk factors and their modification to prevent complications in the contemporary HCM population.
Methods
Study design and database
This study is a nationwide population-based epidemiological study using the National Health Insurance Services (NHIS) database. The NHIS is an obligatory universal health insurance program managed by the Korean government since 1989, and offers comprehensive medical care covering 97.2% of the entire Korean population. The NHIS database is based on individual medical bill expenses claimed by NHIS, and includes each patient’s demographics, diagnoses, healthcare utilization, and prescription data32.
The Institutional Review Board of Seoul National University Hospital approved the study protocol (E-2004-016-1114) and waived informed consent because the analysis used fully anonymized information. The study conformed to the ethical guidelines of the Declaration of Helsinki.
Study population
From the NHIS database, we extracted data on HCM patients between January 2015 and December 2016 by using the information on (1) claims for the diagnostic codes (ICD-10-CM) of I42.1 or I42.2 with at least one admission or outpatient clinic visit, and (2) registration in the rare intractable disease (RID) program. To investigate adult patients with HCM, we excluded patients aged 18 years or below.
The government-implemented RID program is a welfare policy extending health insurance coverage of up to 90% of medical costs for patients with RID (including HCM since 2008). Therefore, consistent with the act established by the Ministry of Health and Welfare, RID registration is tightly controlled by verification with clinical and imaging evidence, attending physician’s certification, and independent reviews by medical experts and health insurance professionals. This definition of HCM was validated with 1110 patients with HCM by showing that sensitivity and specificity of HCM diagnosis in combination with RID code was 91.5% and 100%, respectively, and the accuracy was 92.6%6.
Measurements
We obtained data on the utilization of ED during a one-year period in patients with HCM. Individuals who visited EDs were defined by codes for emergency medical management charges from the NHIS database (AC101, AC103, AC105, V1100, V1200, V1210, V1300, V1310, V1320, and V1400).
The comorbidities were defined as one or more relevant diagnostic codes during hospitalization, or at least two records of diagnostic codes in outpatient clinics prior to study enrollment. A low income indicated that the patient belonged to the lowest quartile (25%) of income level. Disease duration of HCM was defined as the time from the date of the first HCM diagnosis recorded in the NHIS database to the date of study enrollment. Specific definitions for comorbidities based on ICD-10-CM codes are described in more detail in Supplementary Table 1. These definitions have been previously validated3,32,33,34.
Outcomes
The reasons for ED utilization were defined from the primary diagnoses recorded upon discharge from the EDs, and were categorized into cardiovascular disease, gastrointestinal disease, respiratory disease, trauma, etc. Meanwhile, non-specific complaints, such as chest pain (that was not typical of angina), dizziness, palpitations, shortness of breath, and syncope, were classified as ‘undiagnosed cardiovascular symptoms.’ We investigated the clinical outcomes of interest as follows: (1) hospitalization and (2) all-cause mortality, both within 90 days after ED visit. Deaths and their causes were confirmed using the National Death Registration Records of Korea. Death from cardiovascular disease was defined based on the ICD-10-CM code of I00-I99, and death from cancer was determined based on the ICD-10-CM code of C00-D49.
Statistical analysis
For comparison of baseline characteristics, categorical variables (frequencies and percentages) were compared using the χ2 test or Fisher’s exact test, while continuous variables (mean ± standard deviation) were compared with the Student’s t-test or Wilcoxon’s signed rank-sum test for independent samples. The number of ED visits was presented as mean ± standard deviation, and frequencies and percentages, according to age and sex.
The clinical outcomes were evaluated in the pre-specified subgroups, which were defined according to the baseline characteristics, such as age, sex, a previous history of stroke/TIA/thromboembolism and atrial fibrillation/flutter, ICD implantation, and the reasons for ED utilization (cardiovascular versus non-cardiovascular disease). Multivariate logistic regression analysis was performed to estimate the association between the pre-specified subgroups and outcomes after adjustments for age, sex, low-income, hypertension, diabetes mellitus, dyslipidemia, heart failure, stroke/TIA/thromboembolism, myocardial infarction, atrial fibrillation/flutter, chronic obstructive pulmonary disease, chronic kidney disease, and ICD implantation. The OR was presented with the corresponding 95% CI.
SAS software version 9.4 (SAS, Cary, NC, USA) was used in all statistical analyses, and a P-value of < 0.05 was considered statistically significant.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to the data from NHIS that can be analyzed in a designated place.
References
Marian, A. J. & Roberts, R. Recent advances in the molecular genetics of hypertrophic cardiomyopathy. Circulation 92, 1336–1347 (1995).
Maron, B. J. et al. Prevalence of hypertrophic cardiomyopathy in a general population of young adults. Echocardiographic analysis of 4111 subjects in the CARDIA Study. Coronary artery risk development in (Young) adults. Circulation 92, 785–789 (1995).
Moon, I. et al. Trends of the prevalence and incidence of hypertrophic cardiomyopathy in Korea: A nationwide population-based cohort study. PLoS ONE 15, e0227012. https://doi.org/10.1371/journal.pone.0227012 (2020).
Maron, B. J. Clinical course and management of hypertrophic cardiomyopathy. N. Engl. J. Med. 379, 1977 (2018).
Maron, B. J. et al. Hypertrophic cardiomyopathy in adulthood associated with low cardiovascular mortality with contemporary management strategies. J. Am. Coll. Cardiol. 65, 1915–1928 (2015).
Choi, Y. J. et al. Validation of the hypertrophic cardiomyopathy risk-sudden cardiac death calculator in Asians. Heart 105, 1892–1897 (2019).
O’Mahony, C. et al. A novel clinical risk prediction model for sudden cardiac death in hypertrophic cardiomyopathy (HCM risk-SCD). Eur. Heart J. 35, 2 (2014).
Authors, T. F. et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 35, 2733–2779 (2014).
Rowin, E. J. et al. Impact of effective management strategies on patients with the most extreme phenotypic expression of hypertrophic cardiomyopathy. Am. J. Cardiol. 124, 113–121 (2019).
Berchet, C. Emergency Care Services: Trends, Drivers and Interventions to Manage the Demand. OECD Health Working Papers, 83, OECD Publishing, Paris doi.org/https://doi.org/10.1787/18152015 (2015).
Di Somma, S. et al. Overcrowding in emergency department: An international issue. Intern. Emerg. Med. 10, 171–175 (2015).
Sun, R et al. Trends in Hospital Emergency Department Visits by Age and Payer, 2006–2015: Statistical Brief #238. Agency for Healthcare Research and Quality, https://www.hcup-us.ahrq.gov/reports/statbriefs/sb238-Emergency-Department-Age-Payer-2006-2015.jsp (2018)
Yun, J., Oehlman, K. & Johansen, M. Per visit emergency department expenditures by insurance type, 1996–2015. Health Aff (Millwood) 37, 1109–1114 (2018).
Maron, B. J., Casey, S. A., Hauser, R. G. & Aeppli, D. M. Clinical course of hypertrophic cardiomyopathy with survival to advanced age. J. Am. Coll. Cardiol. 42, 882–888 (2003).
Gersh, B. J. et al. 2011 ACCF/AHA Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J. Am. Coll. Cardiol. 58, e212-260. https://doi.org/10.1016/j.jacc.2011.06.011 (2011).
Maron, B. J. et al. Hypertrophic cardiomyopathy with longevity to 90 years or older. Am. J. Cardiol. 109, 1341–1347 (2012).
Castillo, E. M. et al. Factors associated with geriatric frequent users of emergency departments. Ann. Emerg. Med. 74, 270–275 (2019).
Stephenson, M. D. et al. The impact of integrated care for people with chronic conditions on hospital and emergency department utilization: A rapid review. Int. J. Evid.-Based Hea 17, 14–26 (2019).
Olivotto, I. et al. Gender-related differences in the clinical presentation and outcome of hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 46, 480–487 (2005).
Geske, J. B. et al. Women with hypertrophic cardiomyopathy have worse survival. Eur. Heart J. 38, 3434-U3420 (2017).
Anson, O., Carmel, S. & Levin, M. Gender differences in the utilization of emergency department services. Women Health 17, 91–104 (1991).
McCormack, L. A., Jones, S. G. & Coulter, S. L. Demographic factors influencing nonurgent emergency department utilization among a Medicaid population. Health Care Manag. Sc. 20, 395–402 (2017).
Rowin, E. J. et al. Impact of sex on clinical course and survival in the contemporary treatment era for hypertrophic cardiomyopathy. J. Am. Heart Assoc. 8, e012041. https://doi.org/10.1161/JAHA.119.012041 (2019).
Siontis, K. C. et al. Sex, survival, and cardiomyopathy: Differences between men and women with hypertrophic cardiomyopathy. J. Am. Heart Assoc. 8, e014448. https://doi.org/10.1161/JAHA.119.014448 (2019).
Stefanovski, P. H. et al. Analysis of mortality in the emergency department at a university hospital in Pleven. J. Int. Med. Res. 45, 1553–1561. https://doi.org/10.1177/0300060517707901 (2017).
Gunnarsdottir, O. S. & Rafnsson, V. Mortality of the users of a hospital emergency department. Emerg. Med. J. 23, 269–273 (2006).
Choi, Y. J. et al. Temporal trends of the prevalence and incidence of atrial fibrillation and stroke among Asian patients with hypertrophic cardiomyopathy: A nationwide population-based study. Int. J. Cardiol. 273, 130–135 (2018).
Lee, H. J. et al. Clinical impact of atrial fibrillation in a nationwide cohort of hypertrophic cardiomyopathy patients. Ann. Transl. Med. 8, 1386 (2020).
Mehrotra, A., Weinick, R. & Burns, R. How many emergency department visits could be managed at urgent care centers or retail clinics?. J. Gen. Intern. Med. 25, 298–298 (2010).
Enard, K. R. & Ganelin, D. M. Reducing preventable emergency department utilization and costs by using community health workers as patient navigators. J. Healthc. Manag. 58, 412–427 (2013).
Maron, B. J. et al. Hypertrophic cardiomyopathy: Present and future, with translation into contemporary cardiovascular medicine. J. Am. Coll. Cardiol. 64, 83–99 (2014).
Choi, E. K. Cardiovascular research using the Korean national health information database. Korean Circ. J. 50, 754–772 (2020).
Lee, H. J. et al. Novel oral anticoagulants for primary stroke prevention in hypertrophic cardiomyopathy patients with atrial fibrillation. Stroke 50, 2582–2586 (2019).
Kwak, S. et al. De novo malignancy risk in patients undergoing the first percutaneous coronary intervention: A nationwide population-based cohort study. Int. J. Cardiol. 313, 25–31 (2020).
Author information
Authors and Affiliations
Contributions
K.H.K.: supervision. K.H.K., J.B.P., H.L., H.J.L., Y.J.C.: conceptualization and Methodology. K.H.K., Y.J.C., B.K., K.H.: investigation, and data curation. B.K., K.H., Y.J.C.: formal analysis and visualization. K.H.K., Y.J.C.: writing-original draft preparation, S.P.L., Y.J.K., K.H.K., Y.J.C., J.B.P.: reviewing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Choi, YJ., Kim, B., Lee, HJ. et al. Emergency department utilization in patients with hypertrophic cardiomyopathy: a nationwide population-based study. Sci Rep 12, 3534 (2022). https://doi.org/10.1038/s41598-022-07463-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-07463-2