Abstract
Β2-microglobulin (β2-M) is associated with various malignancies. However, the relationship between β2-M and colorectal cancer (CRC) remains unclear. We explored the association between β2-M and CRC among inpatients who underwent colonoscopy and explored factors that may modify the association. All consecutive inpatients who underwent colonoscopy were enrolled in a tertiary hospital between April 2015 and June 2022. Inpatients with initial CRC or normal colonoscopies were considered eligible as cases or controls, respectively. Baseline characteristics and laboratory indicators of the participants were collected from electronic medical records. Logistic regression analysis, smooth curve fitting, sensitivity analysis, and subgroup analysis were conducted in the present study. After adjusting for baseline clinical characteristics and laboratory parameters, β2-M was positively associated with CRC (odds ratio [OR] 1.32; 95% confidence interval [CI] 1.11–1.58) among inpatients. When the β2-M level was assigned as tertiles, participants in the highest tertile presented with a higher risk of CRC (OR 2.33; 95% CI 1.57–3.48). A positive linear association was observed between β2-M and CRC with smooth curve fitting. In particular, it may be of great importance to monitor β2-M levels for predicting CRC patients.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the second most fatal malignancy and third most common cancer1. The burden of CRC is increasing globally owing to its increasing prevalence. Studies have shown that CRC has the highest all-age incidence in China (607,900, 95% uncertainty interval [UI] 521,805–708,420])2. Although early diagnosis can significantly improve prognosis, patients with CRC often have no typical clinical presentation or present with only non-specific signs in the early stages, which leads to a low early diagnosis rate. The study of risk factors for CRC could open up further opportunities for the prevention, diagnosis, and treatment of CRC, which faces enormous challenges.
β2-microglobulin (β2-M), a well-known housekeeping protein, is non-glycosylated3. It not only has a tumor immunological role: it presents antigenic peptides to cytotoxic T lymphocytes, actively binding and lysing antigen-presenting cancer cells upon recognition of exogenous antigenic peptides on the cell surface4,5,6,7. β2-M also has both tumor-promoting and tumor-suppressing functions and is cancer cell background-dependent8. In addition, it has been shown that β2-M is widely implicated in the regulation of cancer cell growth, survival, apoptosis, and even metastasis9,10.
Under physiological conditions, β2-M exists at low levels in serum, urine, and other body fluids11. However, evidence has linked β2-M levels to various malignancies. Increased β2-M levels in body fluids (such as serum, plasma, or urine) are seen in patients with malignancies, including breast cancer, renal cell carcinoma, oral squamous cell carcinoma, lung cancer, gastrointestinal tract cancer, prostate cancer, lymphocytic malignancies, and multiple myeloma12,13,14,15,16,17, and can promote tumor growth through specific axes18. However, a previous study in 1980 showed no direct correlation between elevated β2-M levels and gastrointestinal cancer19.
Based on the fact that the relevance of β2-M to CRC is unclear, the association of β2-M with CRC still deserves to be studied. Our study was aimed to explore the association between β2-M and CRC in more different characteristics.
Result
Baseline characteristics
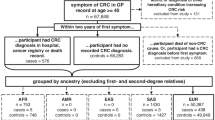
A total of 3589 consecutive inpatients were enrolled in this study between April 2015 and June 2022 (Fig. 1). The detailed characteristics of the individuals by case and control are presented in Table 1. CRC was associated with several variables such as age, sex, weight, smoking status, drinking status, β2-M, and several blood indicators.
Relationship between β2-microglobulin and colorectal cancer
We performed smooth curve fitting and found a positive linear association between β2-M and the risk of CRC (P for non-linearity: 0.229, only 99% of data is shown in Fig. 2).
Linear relationship between β2-microglobulin and colorectal cancer among inpatients (Only 99% of the data is shown). Adjustment by sex, age, weight, drinking status, smoking status, glomerular filtration rate, total cholesterol, apoprotein A1, lipoprotein(a), alanine aminotransferase, albumin, total protein, aspartate aminotransferase, alkaline phosphatase, glucose, urea, cholinesterase, total bilirubin, total bile acid, hyperlipidemia, hypertension, diabetes mellitus, and liver disease.
When β2-M was evaluated as a continuous variable, multivariable-adjusted regression analysis (adjustment for age, sex, weight, drinking status, smoking status, glomerular filtration rate [GFR], total cholesterol [TC], apoprotein A1 [Apo A1], lipoprotein(a) [Lp(a)], total protein [TP], albumin [ALB], alanine aminotransferase [ALT], aspartate aminotransferase [AST], alkaline phosphatase [ALP], glucose [GLU], urea, total bile acid [TBA], cholinesterase [ChE], total bilirubin [TBIL], diabetes mellitus [DM], liver disease, hypertension, and hyperlipidemia [HLP]) demonstrated that there was a 32% higher risk of CRC with each 1 mg/L increment in β2-M level (Table 2, Model II, OR 1.32; 95% CI 1.11–1.58]). When β2-M was analyzed as tertiles, also in a fully adjusted model (Table 2, Model II, P for trend was < 0.001), the adjusted OR for CRC in tertile 2 and tertile 3 were 1.35 (95% CI 0.90–2.02) and 2.33 (95% CI 1.57–3.48), respectively, with tertile 1 as reference. This means that the risk of CRC increased with increasing β2-M levels.
Sensitivity analysis
Subgroup analysis (Fig. 3) was conducted to investigate the effect of β2-M on CRC in different subgroups. The relationship between β2-M and CRC was adjusted for the following subgroups: age, sex, HLP, hypertension, liver disease, ischemic cerebrovascular disease, coronary heart disease (CHD), kidney disease, and DM. P values < 0.05 for interactions in age, sex, and kidney disease subgroups may not be statistically significant based on multiple testing. However, in the DM subgroup, a stronger association between β2-M and CRC was observed among inpatients without DM.
Subgroup analyses of the β2-microglobulin and colorectal cancer among inpatients. Adjusted for sex, age, weight, drinking status, smoking status, glomerular filtration rate, total cholesterol, apoprotein A1, lipoprotein(a), alanine aminotransferase, albumin, total protein, aspartate aminotransferase, alkaline phosphatase, glucose, urea, cholinesterase, total bilirubin, total bile acid, hyperlipidemia, hypertension, liver disease, and diabetes mellitus.
After the exclusion participants with missing data, there were 2210 participants and the association between β2-M and CRC remained robust in the multivariable logistic regression models (Supplementary Table S1). When β2-M was analyzed as a continuous variable, multivariable-adjusted regression analysis demonstrated (adjustment for age, sex, weight, drinking status, smoking status, GFR, TC, Apo A1, Lp(a), ALT, ALB, TP, ALP, AST, GLU, urea, ChE, TBIL, TBA, HLP, hypertension, liver disease, and DM) that there was a 19% higher risk of CRC with each 1 mg/L increment in β2-M level (Model II, OR 1.19 [95% CI 1.01–1.4]). When β2-M was analyzed as tertiles, also in a fully adjusted model (Model II, P for trend was < 0.001), with tertile 1 as reference, the adjusted OR for CRC in tertile 2 and tertile 3 were 1.22 (95% CI 0.73–2.04) and 2.73 (95% CI 1.65–4.5), respectively.
In addition, propensity score matching (PSM) indicated that the relationship between β2-M and CRC was robust (Supplementary Table S2).
Discussion
The present study revealed a positive linear relationship between β2-M and CRC among inpatients in China.
The relationship between β2-M and CRC has been previously examined but is inconclusive. An earlier study reported no direct relationship between β2-M and gastrointestinal cancer19. This finding is inconsistent with ours, probably because of differences in cancer populations and sample sizes. Furthermore, in a cohort study, a 121% increased risk of colorectal cancer (n = 255) was found in participants in the highest and lowest quartiles of serum β2-M concentration16. This finding was consistent with the present study. In addition, this study found a positive linear association between β2-M and colorectal cancer. This may be due to region and sample size.
In this study, we considered the possibility that unknown confounding factors might influence the relationship between β2-M and colorectal cancer. Therefore, we collected all available clinical factors and adjusted for additional confounding factors to exclude such effects. Our finding that DM modified the association between β2-M and CRC among inpatients requires further exploration. As shown in Fig. 3, a stronger positive relationship was observed in individuals without DM, which requires further exploration.
β2-M is an interesting protein with multiple biological functions that are closely associated with cancer. Under normal conditions, β2-M acts as a friend to humans, forming complexes with the heavy chain of major histocompatibility complex class I molecules (MHC-I) in a well-known manner, presenting antigenic peptides to cytotoxic T cells, thereby allowing T cells to recognize foreign peptide antigens on the cell surface to destroy tumor cells and act as immune surveillance agents5,20,21,22. However, in the early stages of cancer, tumor cells exhibit impaired β2-M expression, resulting in defective antigen processing and presentation, thereby evading immune surveillance23. In cancer patients, β2-M acts as an enemy in humans and as an oncogenic factor that stimulates the growth and progression of cancers24,25,26, in particular, β2-M acts directly on tumor cells to increase their growth, survival, and invasiveness by inducing epithelial-to-mesenchymal transition26. In an animal study, Josson et al. showed that β2-M overexpression promoted the growth and progression of human lung, breast, prostate, and kidney tumor cells, leading to metastatic and lethal findings27. However, there were no participants with colorectal cancer in these studies, and further research is needed.
Under normal physiological conditions, β2-M exists at low levels in human fluids. This is because the cell-associated form of β2-M is not anchored to the cell membrane, allowing dissociation and balanced exchange with soluble β2-M circulating in the extracellular fluid. β2-M is metabolized in the glomerulus after its dissociation from the MHC-I heavy chain to maintain stability in humans28,29. Although elevated serum β2-M levels suggest an abnormal condition seen in a variety of malignancies12,15,17,25,30,31, our study adds to the evidence on colorectal cancer that β2-M may serve as a potential biomarker for colorectal cancer18. Furthermore, there is considerable evidence that colorectal cancer is associated with immune response and inflammation32,33,34,35, and we believe that β2-M probably plays a role in early CRC.
There are two possible explanations for the elevated serum β2-M in patients with colorectal cancer: first, the assembly of β2-M and class I heavy chain on the tumor cell membrane does not result from conformational changes in the heavy chains, leading to reduced expression of class I antigen on tumor cells and the accumulation of free β2-M in the serum; secondly, there is increased renewal of tumor cells in patients with colorectal cancer, resulting in increased shedding of β2-M from tumor cells and subsequently elevated serum levels.
This study had some limitations, such as missing data, due to the retrospective nature. However, the sensitivity and subgroup analyses showed that the results were robust. In addition, this study is not representative of the relationship between long-term β2-M levels and CRC because of the lack of data on repeated measurements of β2-M. Furthermore, the participants were from a tertiary hospital in China, which may limit their generalizability to other populations. And the effects of variables not available in this study cannot be excluded. Finally, Longitudinal studies are needed to confirm the causal relationship between β2-M and CRC.
In conclusion, our study indicated a positive linear association between β2-M and CRC in inpatients. Further studies are needed to investigate the potential mechanism of β2-M on CRC risk. β2-M may be used as a biomarker for the diagnosis and management of CRC in the future.
Materials and methods
Population
All consecutive inpatients who underwent colonoscopy were enrolled in a tertiary hospital between April 2015 and June 2022 in the current study. Inpatients with initial CRC or normal colonoscopy were considered eligible case (n = 469) or control (n = 3120) groups, respectively. Flowchart presents the screening of participants (Fig. 1), including the reasons for exclusion. Participants were included only once.
Ethics approval
This retrospective study was approved by the Ethics Review Board of Shijiazhuang Traditional Chinese Medicine Hospital (No.20220919029) and the requirement for informed consent was waived because of the retrospective nature of the study. All methods were performed in accordance with the relevant guidelines and regulations.
Covariates
Baseline characteristics and laboratory indicators were collected from electronic medical records. The data analyzed in this study are listed in Table 1, including demographic data, comorbidities (including hypertension, ischemic cerebrovascular disease, CHD, HLP, liver disease, kidney disease, and DM), and laboratory indicators (including β2-M, GFR, triglyceride [TG], TC, low-density lipoprotein (LDL), high-density lipoprotein (HDL), Apo A1, Lp(a), apolipoprotein B [Apo B], ALB, TP, ALT, gamma-glutamyl transferase [GGT]; ALP, AST, GLU, CREA, urea, uric acid [UA], ChE, 5′-nucleotidase [5′-NT], TBA, direct bilirubin [DBIL], and TBIL). Drinking and smoking statuses were divided into four groups: never, former, current, and NA (not recorded). Liver disease included cirrhosis, fatty liver disease, and hepatitis. Kidney disease included chronic kidney disease [CKD], kidney cysts, and kidney stones. GFR was calculated using the modification of diet in renal disease equation36. Laboratory data were the first eligible results obtained during hospitalization (before colonoscopy).
Statistical analysis
The participants’ characteristics were assessed according to the following groups: CRC and control groups. Depending on the nature of the variables, we used the Chi-square test, Fisher's exact test, Mann–Whitney U test, or Student's t test, respectively.
We considered β2-M as a continuous variable in the primary analysis, calculated the odds ratios (ORs) per 1 standard deviation (SD) increment, and presented P for trend. We also classified β2-M into tertiles and calculated ORs using the lowest tertile as the reference. Three logistic regression models were used. The unadjusted model had no adjustment for covariates. The minimally adjusted model only included sex and age. The fully adjusted model further included weight, drinking status, smoking status, GFR, TC, Apo A1, Lp(a), ALT, ALB, TP, ALP, AST, GLU, urea, ChE, TBIL, TBA, HLP, hypertension, liver disease, and DM to account for the potential confounding by β2-M and CRC. These potential confounders were screened according to a change in the effect estimate ≥ 10% and significant covariates in the univariate analysis (P < 0.05). We used the multiple imputation method for the covariates with missing data. Smooth curve fitting was performed to evaluate the relationship between β2-M levels and CRC. Additionally, participants were matched for the fully adjusted model using a one-to-one nearest neighbor technique with a caliper width of 0.2 in PSM. ORs and 95% confidence intervals (95% CIs) for the association between β2-M and CRC were calculated using the logistic regression model.
Furthermore, potential modifications of the relationship between β2-M and CRC were assessed, including the following subgroups: sex, age (< 65 vs. ≥ 65 years), HLP, hypertension, liver disease, kidney disease, ischemic cerebrovascular disease, CHD, and DM. Subgroup heterogeneity was assessed by multivariate logistic regression and subgroup interactions by likelihood ratio testing.
A 2-tailed P < 0.05 was recognized as statistically significant. All analyses were conducted using the statistical software packages R 3.3.2 (http://www.R-project.org, the R Foundation) and Free Statistics software version 1.7.1.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Siegel, R. L. et al. Colorectal cancer statistics, 2020. CA Cancer J. Clin. 70, 145–164. https://doi.org/10.3322/caac.21601 (2020).
Sharma, R. et al. Global, regional, and national burden of colorectal cancer and its risk factors, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet Gastroenterol. Hepatol. 7, 627–647. https://doi.org/10.1016/S2468-1253(22)00044-9 (2022).
Hofbauer, D. et al. β2-microglobulin triggers NLRP3 inflammasome activation in tumor-associated macrophages to promote multiple myeloma progression. Immunity 54, 1772-1787.e1779. https://doi.org/10.1016/j.immuni.2021.07.002 (2021).
Barbosa, C. R. R., Barton, J., Shepherd, A. J. & Mishto, M. Mechanistic diversity in MHC class I antigen recognition. Biochem. J. 478, 4187–4202. https://doi.org/10.1042/BCJ20200910%JBiochemicalJournal (2021).
Salter, R. D. et al. A binding site for the T-cell co-receptor CD8 on the alpha 3 ___domain of HLA-A2. Nature 345, 41–46. https://doi.org/10.1038/345041a0 (1990).
Brennick, C. A., George, M. M., Srivastava, P. K. & Karandikar, S. H. Prediction of cancer neoepitopes needs new rules. Semin. Immunol. 47, 101387. https://doi.org/10.1016/j.smim.2020.101387 (2020).
Mishra, A. K., Ali, A., Dutta, S., Banday, S. & Malonia, S. K. Emerging trends in immunotherapy for cancer. Diseases 10, 60 (2022).
Nomura, T. et al. β2-microglobulin-mediated signaling as a target for cancer therapy. Anti-Cancer Agents Med. Chem. 14, 343–352. https://doi.org/10.2174/18715206113139990092 (2014).
Shi, C., Zhu, Y., Su, Y., Chung, L. W. & Cheng, T. Beta2-microglobulin: Emerging as a promising cancer therapeutic target. Drug Discov. Today 14, 25–30. https://doi.org/10.1016/j.drudis.2008.11.001 (2009).
Yang, J. & Yi, Q. Killing tumor cells through their surface beta(2)-microglobulin or major histocompatibility complex class I molecules. Cancer 116, 1638–1645. https://doi.org/10.1002/cncr.24953 (2010).
Saito, A. & Gejyo, F. Current clinical aspects of dialysis-related amyloidosis in chronic dialysis patients. Ther. Apher. Dial. 10, 316–320. https://doi.org/10.1111/j.1744-9987.2006.00383.x (2006).
Sequeira, J., Sengupta, S. & Mhatre, B. Serum beta-2 microglobulin analysis in patients with oral squamous cell carcinoma. Natl. J. Maxillofac. Surg. 12, 227–232. https://doi.org/10.4103/njms.NJMS_242_20 (2021).
Jongvilaikasem, S. et al. Serum β-2 microglobulin levels are associated with distant metastasis in patients with breast cancer. Mol. Clin. Oncol. 14, 118. https://doi.org/10.3892/mco.2021.2280 (2021).
Maaroufi, A., Khadem-Ansari, M.-H., Khalkhali, H.-R. & Rasmi, Y. Serum levels of bone sialoprotein, osteopontin, and β2-microglobulin in stage I of multiple myeloma. J. Cancer Res. Ther. 16, 98. https://doi.org/10.4103/JCRT.JCRT_666_16 (2020).
Zhang, Y.-X. et al. Correlation of serum β2-microglobulin levels with prostate-specific antigen, Gleason score, clinical stage, tumor metastasis and therapy efficacy in prostate cancer. Arch. Med. Res. 44, 259–265. https://doi.org/10.1016/j.arcmed.2013.03.008 (2013).
Prizment, A. E. et al. Circulating beta-2 microglobulin and risk of cancer: The atherosclerosis risk in communities study (ARIC). Cancer Epidemiol. Biomark. Prev. 25, 657–664. https://doi.org/10.1158/1055-9965.EPI-15-0849 (2016).
Nissen, M. H., Bjerrum, O. J., Plesner, T., Wilken, M. & Rørth, M. Modification of beta-2-microglobulin in sera from patients with small cell lung cancer: Evidence for involvement of a serine protease. Clin. Exp. Immunol. 67, 425–432 (1987).
Amiri, F. S. Serum tumor markers in chronic kidney disease: As clinical tool in diagnosis, treatment and prognosis of cancers. Renal Fail. 38, 530–544. https://doi.org/10.3109/0886022X.2016.1148523 (2016).
Staab, H. J., Anderer, F. A., Hiesche, K., Wehrle, E. & Rodatz, W. Is serum beta 2-microglobulin a tumor marker in gastrointestinal cancer?. Clin. Chim. Acta 106, 309–317. https://doi.org/10.1016/0009-8981(80)90315-0 (1980).
Lee, M. Y., Jeon, J. W., Sievers, C. & Allen, C. T. Antigen processing and presentation in cancer immunotherapy. J. Immunother. Cancer 8, e001111. https://doi.org/10.1136/jitc-2020-001111 (2020).
Rock, K. L., Reits, E. & Neefjes, J. Present yourself! By MHC class I and MHC class II molecules. Trends Immunol. 37, 724–737. https://doi.org/10.1016/j.it.2016.08.010 (2016).
Altman, J. D. & Davis, M. M. MHC-peptide tetramers to visualize antigen-specific T cells. Curr. Protoc. Immunol. 115, 17.13.11-17.13.44. https://doi.org/10.1002/cpim.14 (2016).
Picard, E., Verschoor, C. P., Ma, G. W. & Pawelec, G. Relationships between immune landscapes, genetic subtypes and responses to immunotherapy in colorectal cancer. Front. Immunol. https://doi.org/10.3389/fimmu.2020.00369 (2020).
Huang, W. C. et al. beta2-microglobulin is a signaling and growth-promoting factor for human prostate cancer bone metastasis. Cancer Res. 66, 9108–9116. https://doi.org/10.1158/0008-5472.Can-06-1996 (2006).
Nomura, T. et al. Beta2-microglobulin promotes the growth of human renal cell carcinoma through the activation of the protein kinase A, cyclic AMP-responsive element-binding protein, and vascular endothelial growth factor axis. Clin. Cancer Res. 12, 7294–7305. https://doi.org/10.1158/1078-0432.Ccr-06-2060 (2006).
Nomura, T. et al. Targeting beta2-microglobulin mediated signaling as a novel therapeutic approach for human renal cell carcinoma. J. Urol. 178, 292–300. https://doi.org/10.1016/j.juro.2007.03.007 (2007).
Josson, S. et al. β2-microglobulin induces epithelial to mesenchymal transition and confers cancer lethality and bone metastasis in human cancer cells. Cancer Res. 71, 2600–2610. https://doi.org/10.1158/0008-5472.Can-10-3382 (2011).
Birn, H. et al. Megalin is essential for renal proximal tubule reabsorption and accumulation of transcobalamin-B(12). Am. J. Physiol. Renal Physiol. 282, F408-416. https://doi.org/10.1152/ajprenal.00206.2000 (2002).
Christensen, E. I. & Nielsen, R. Role of megalin and cubilin in renal physiology and pathophysiology. Rev. Physiol. Biochem. Pharmacol. 158, 1–22. https://doi.org/10.1007/112_0604 (2007).
Sun, J. et al. ATP5b and β2-microglobulin are predictive markers for the prognosis of patients with gallbladder cancer. J. Mol. Histol. 46, 57–65. https://doi.org/10.1007/s10735-014-9597-9 (2015).
Adil, A., Mohammed, A. & Ibrahim, A. Beta-2-microglobulin as a marker in patients with thyroid cancer. Iraqi Postgrad. Med. J. 18, 6 (2019).
Puntoni, M., Marra, D., Zanardi, S. & Decensi, A. Inflammation and cancer prevention. Ann. Oncol. 19(Suppl 7), vii225–vii229. https://doi.org/10.1093/annonc/mdn442 (2008).
Grivennikov, S. I., Greten, F. R. & Karin, M. Immunity, inflammation, and cancer. Cell 140, 883–899. https://doi.org/10.1016/j.cell.2010.01.025 (2010).
Grizzi, F., Bianchi, P., Malesci, A. & Laghi, L. Prognostic value of innate and adaptive immunity in colorectal cancer. World J. Gastroenterol. 19, 174–184. https://doi.org/10.3748/wjg.v19.i2.174 (2013).
Rhodes, J. M. & Campbell, B. J. Inflammation and colorectal cancer: IBD-associated and sporadic cancer compared. Trends Mol. Med. 8, 10–16. https://doi.org/10.1016/s1471-4914(01)02194-3 (2002).
Levey, A. S. et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann. Intern. Med. 145, 247–254. https://doi.org/10.7326/0003-4819-145-4-200608150-00004 (2006).
Funding
This work was supported by the Hebei Administration of Traditional Chinese Medicine (Grant Number 2023145); National Famous Old Traditional Chinese Medicine Experts Inheritance Studio Construction Program of National Administration of TCM (Grant Number: [2022] No. 75).
Author information
Authors and Affiliations
Contributions
H.W. and Hu.Z. conceived and designed the study; H.W., X.C., P.M., J.L., Z.W., C.Z., T.Z., and Ha.Z. collected and analyzed the data; HW wrote the manuscript; and H.W. and Hu.Z. revised the manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, H., Zheng, H., Cao, X. et al. β2-microglobulin and colorectal cancer among inpatients: a case–control study. Sci Rep 13, 12222 (2023). https://doi.org/10.1038/s41598-023-39162-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-39162-x