Abstract
Efficacy of systemic corticosteroid therapy (CS) for long-term kidney survival in patients with IgA nephropathy (IgAN) is controversial. Therefore, prospective studies evaluating targeted therapies to lymphatic tissues in mucosal immune system responsible for production of nephritogenic IgA have been desired worldwide. Here, we aimed to evaluate the associations of CS and combination therapy of CS and tonsillectomy (CS + Tx) with kidney survival, using database from a nationwide multicenter prospective cohort study on IgAN. Primary outcome was a 50% increase in serum creatinine from baseline or dialysis induction. The analysis included 941 patients (CS/CS + Tx/non-CS 239/364/338), 85 (9.0%) of whom reached outcomes during median follow-up of 5.5 (interquartile range 2.0–8.0) years. On overlap weighting analysis with balanced baseline characteristics, CS and CS + Tx were associated with lower risk of kidney events when compared with non-CS (hazard ratio [HR] 0.51, 95% confidence interval [CI] 0.29–0.88 and HR 0.20, 95%CI 0.09–0.44, respectively). Notably, when compared with the CS, CS + Tx was associated with a lower risk of kidney events (HR 0.40, 95%CI 0.18–0.91). Present study demonstrated, keeping with favorable association of systemic CS with kidney survival, concurrent tonsillectomy as one of targeted interventions to lymphatic tissues may provide additional improvement to kidney survival in patients with IgAN.
Similar content being viewed by others
Introduction
Immunoglobulin A nephropathy (IgAN) is the most common type of glomerulonephritis worldwide, and 30–40% of affected patients develop end-stage kidney disease (ESKD) within 20 years from its onset1. The KDIGO international clinical practice guideline recommends the systemic administration of corticosteroids (CS) in patients with IgAN who remain at high risk of ESKD despite maximal supportive care2,3,4,5,6,7. Nevertheless, the effect of CS on kidney events among patients with IgAN has been controversial2,3,6,8,9,10,11. Lv et al. demonstrated the efficacy of CS on kidney survival by the largest randomized controlled study (RCT) for IgAN4,5. On the contrary, Rauen et al. found no differences in kidney survival in IgAN patients randomized to receive added CS on top of supportive care compared to supportive care alone3,12. In addition, adverse effects of CS which cannot be overlooked were observed in some studies3,4,5. Therefore, new strategies improving the efficacy and safety of CS have been desired worldwide13.
Targeted therapies to lymphatic tissues in mucosal immune system responsible for production of nephritogenic IgA may improve kidney survival in patients with IgAN14,15,16,17,18,19,20. Mucosa-associated lymphoid tissue includes gut-associated lymphoid tissue (GALT) and nasal/upper respiratory mucosa-associated one (NALT). Regarding GALT, an enteric targeted-release formulation of budesonide excellently reduced proteinuria in patients with IgAN in the recent NEFIGAN trial14. The long-term kidney survival on budesonide treatment may be clarified elsewhere. Gross hematuria following acute upper respiratory infections and COVID-19 may indicate the apparent association between NALT and IgAN21,22. Compared to CS alone, reduction in proteinuria by tonsillectomy combined with CS (CS + Tx) has been demonstrated in two RCTs from East Asia15,16. A meta-analysis in 2017, our recent matched study in 2019 and other retrospective studies after 2020 reported an association between tonsillectomy and kidney survival17,18,23,24. However, these two studies were retrospective in nature and did not include an assessment of wide spectrum baseline clinicopathological characteristics. Therefore, further clinical implications of CS + Tx should be clarified by long-term prospective observational studies.
Using data from the nationwide prospective cohort study (Japan IgA Nephropathy Prospective Cohort Study [J-IGACS])25, the current study assessed associations of CS and CS + Tx with kidney survival compared to non-corticosteroid use (non-CS) and further compared CS + Tx with CS on kidney survival.
Results
Study cohort and kidney outcomes
In total, 1130 participants were registered in J-IGACS spanning 33 university hospitals and 11 local leading hospitals in Japan (Fig. 1, Supplementary Table S1). After excluding 88 patients with a missing mean arterial blood pressure (MAP) measurement, 1 with a missing estimated glomerular filtration rate (eGFR) measurement, 6 with a missing proteinuria measurement, and 9 with a missing hematuria measurement at the index date, 51 patients missing kidney biopsy data and 34 with missing data regarding outcomes, the final analysis set comprised 941 participants (Fig. 1, covariate set 1 in Table 1, covariate set 2 in Supplementary Table S2). The median baseline hematuria (number of urinary sediment red blood cells [uRBC]/high power filed [HPF]) and MAP in these 941 patients was 20/HPF and 88.7 mmHg, respectively. Therefore, they were categorized into two groups: uRBC > 20/HPF and uRBC ≤ 20/HPF, and ≥ 90 mmHg and < 90 mmHg, respectively. During median follow-up of 5.5 (interquartile range [IQR] 2.0–8.0) years, 85 (9.0%) of the 941 patients reached the outcomes.
Patient flowchart. MAP, mean arterial blood pressure; eGFR, estimated glomerular filtration rate; IPW-ATT, inverse probability treatment weighting on the average treatment effect in the population that received CS + Tx; IPW-ATU, inverse probability treatment weighting on the average treatment effect in the non-CS group.
Associations of corticosteroid therapy and concurrent tonsillectomy with kidney outcomes
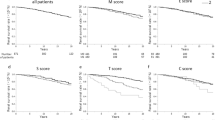
After performing an overlap weighting analysis (Fig. 1), the distribution of baseline covariates among the initial treatment categories (non-CS, CS, and CS + Tx) was well-balanced (Table 1, Fig. 2, Supplementary Table S2). Overlap-weighted incidence of composite kidney events was significantly lower in the CS group compared to the non-CS group (Fig. 3 and Table 2). CS was also associated with a lower risk of composite kidney events compared with non-CS. Notably, CS + Tx was associated with a lower risk of composite kidney events compared to non-CS and CS. As demonstrated in Fig. 3, a stepwise reduction in risk of kidney outcomes was observed from the non-CS group to the CS group, followed by the CS + Tx group.
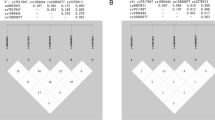
All pairwise absolute standardized differences (PASDs) in baseline characteristics among the initial treatment categories before and after overlap-weighting analysis. Distribution of all baseline characteristics in covariate set 1 according to the treatment groups (non-CS, CS, and CS + Tx) was balanced after overlap-weighting analysis as shown by PASD. The rate of variables showing PASD ≤ 0.1 in covariate set 1 increased from 25.6% in the unweighted analysis to 87.2% in the weighted analysis. The maximums of the pairwise absolute standardized differences in each baseline characteristic are also shown in Table 1. PASD, all pairwise absolute standardized difference; non-CS, non-corticosteroid use; CS corticosteroid monotherapy; CS + Tx, corticosteroid therapy combined with tonsillectomy; MAP, mean arterial blood pressure; eGFR, estimated glomerular filtration rate; M, mesangial hypercellularity score; E, endocapillary hypercellularity score; S, segmental sclerosis score; T, tubulointerstitial fibrosis/atrophy score; C, crescent score; RAASi, renin–angiotensin–aldosterone system inhibitor.
Cumulative incidence estimates, incidence rate, and hazard ratio for kidney outcome in the overlap-weighting analysis. (a) Weighted cumulative incidence estimates by initial treatment categories. The date of kidney biopsy was considered as the index date for all patients. In overall, composite kidney events were defined as > 50% increase in serum creatinine from baseline (among patients aged ≥ 20 years; the number of events [%] was 96.6/849.1 [11.4] in the overlap-weighting analysis) or > 25% reduction in eGFR (among patients aged < 20 years; the number of events [%] was 5.4/94.3 [5.7] in the overlap-weighting analysis). These definitions were used because all patients who received maintenance dialysis during follow-up reached these end points prior to the induction of dialysis. The median observation time by initial treatment categories were 5.5 years (IQR, 2.0–7.5 years) in the non-CS group, 6.0 years (IQR, 3.0–8.0 years) in the CS group, and 5.0 years (IQR, 2.0–7.5 years) in the CS + Tx group. During follow-up, the median initiated time of the treatments was 0.0 years (IQR, 0.0–0.0 years) in the non-CS group, 0.0 years (IQR, 0.0–0.5 years) in the CS group, and 0.0 years (IQR, 0.0–0.5 years) in the CS + Tx group. (b) Weighted incidence rate per 1000 patient-years and weighted hazard ratio by initial treatment categories. Actual data are shown in Table 2. PY, patient-years; HR, hazard ratio; CI, confidence interval; non-CS, non-corticosteroid use; CS, corticosteroid monotherapy; CS + Tx, corticosteroid combined with tonsillectomy.
Interactions between baseline characteristics and the initial treatment for kidney outcomes
The associations between initial treatments and kidney outcomes described above were not affected by almost any baseline characteristic stratifications with explored overlap weighting analyses and multivariate adjusted analyses (Fig. 4). In these subgroup analyses, a gradual decrease in the risk of kidney outcomes from the non-CS group to the CS group, and then to the CS + Tx group, was consistently observed. For instance, those favorable associations were found in both higher proteinuria (≥ 1.0 g/day) and lower proteinuria (< 1.0 g/day) subgroups. In addition, three significant interactions on kidney outcomes were identified, which were between the initial treatment and each of the following baseline characteristics: microscopic hematuria (Fig. 4a), endocapillary hypercellularity, and crescent (Fig. 4b). In patients with greater microscopic hematuria, a more pronounced decrease in the risk of kidney outcomes was observed from the non-CS group to the CS group, followed by the CS + Tx group (Fig. 4a). Conversely, patients with lesser baseline hematuria had worse treatment outcomes. No significant risk reduction was observed in either the CS or CS + Tx group compared to the non-CS group. Similar results were seen in endocapillary hypercellularity (E1/E0) and crescent (C1 + 2/C0) subgroups.
Stepwise reduction in risk of kidney outcomes, in order, by non-corticosteroid use, corticosteroid monotherapy, and combining corticosteroid with tonsillectomy according to baseline characteristic subgroups. The association between initial treatments and kidney outcomes (already shown in Fig. 3 and Table 2) was not modified by a majority of the baseline characteristic subgroups (p for interaction > 0.1). (a) Clinical subgroup analyses. One significant interaction between hematuria and initial treatment was observed. (b) Pathological subgroup analyses. Two significant interactions between each of endocapillary hypercellularity and crescent and initial treatment were observed. Hazard ratios were not weighted but adjusted with all variables in covariate set 1, except for each stratifying factor. N, number of patients; PY, weighted patient-years; CI, confidence interval; P for interaction, p value for interaction between initial treatments and each of the baseline characteristic subgroups on kidney outcome; non-CS, non-corticosteroid use; CS, corticosteroid monotherapy; CS + Tx, corticosteroid therapy combined with tonsillectomy; MAP, mean arterial pressure; eGFR, estimated glomerular filtration rate; RAASi, renin–angiotensin–aldosterone system inhibitor; M, mesangial hypercellularity; E, endocapillary hypercellularity; S, segmental sclerosis; T tubular atrophy/interstitial fibrosis; C, crescent; ND, not determined because of small sample size.
Sensitivity analyses
The inverse probability treatment weighting on the average treatment effect in the population that received CS + Tx (IPW-ATT) cohort had the highest frequency of patients with greater hematuria, E1 and C1 + 2, followed by the overlap-weighting and inverse probability treatment weighting on the average treatment effect in the non-CS group (IPW-ATU) cohorts (Supplementary Table S3). Conversely, the highest rate of adverse predictors commonly observed in patients with chronic kidney disease (e.g., MAP ≥ 90 mmHg and eGFR < 60 ml/min/1.73 m2) was seen in the IPW-ATU cohort, followed by the overlap-weighting and IPW-ATT cohorts.
A weighted Cox regression model applied to the IPW-ATT cohort demonstrated the robustness of the association between the initial treatment categories and kidney outcomes (Table 2). CS and CS + Tx were associated with a lower risk of kidney events compared to non-CS. CS + Tx was further associated with a lower risk of kidney events compared to CS. In contrast, the IPW-ATU analysis did not show any significant difference in kidney outcomes between the CS and non-CS groups. However, CS + Tx was still associated with a lower risk of kidney events compared to CS and non-CS. The E-values indicated that unmeasured confounders were unlikely to sufficiently attenuate the main finding shown in Fig. 3 and Table 2 and negate a causal relationship between corticosteroid treatments and kidney outcomes.
Discussion
Overlap propensity score analysis in the present study achieved good balance among patients with IgAN subjected to different initial treatments and demonstrated that corticosteroid monotherapy and concurrent tonsillectomy were independently associated with better kidney outcomes. Those associations were especially pronounced in patients with endocapillary hypercellularity, crescent, and greater microscopic hematuria at baseline. These results may be of clinical significance in facilitating better identification of subgroups of patients with IgAN who will benefit from corticosteroid therapy and tonsillectomy, and in avoiding potential overtreatment2.
Our results demonstrating the association of corticosteroid monotherapy with better kidney outcomes are in line with the findings of previous studies (Fig. 3 and Table 2)6,7,26. Zhang et al. reported a meta-analysis reviewing six RCTs published between 1993 and 201726. The meta-analysis revealed that the use of corticosteroids can significantly decrease the risk for ESKD. Two observational studies matched by propensity score, the VALIGA and Tokyo cohorts, also confirmed the association of corticosteroid therapy with better kidney survival6,7. In contrast, the STOP-IgAN trial compared immunosuppression based on corticosteroids with standard care but did not find kidney benefits3. The reasons for these contradictory findings are not clear but may be related to the heterogeneity of MEST-C scores (Supplementary Table S4) and patient clinical characteristics. For example, the occurrence of endocapillary hypercellularity and crescent in STOP-IgAN appeared to be lower than that in most other studies reporting an advantage of corticosteroid treatment in kidney survival. Our sensitivity analysis with the IPW-ATU cohort also had lower occurrence of endocapillary hypercellularity and crescent (Supplementary Table S3) and found no significant difference in kidney outcomes between the CS and non-CS groups. Different prognoses and/or therapeutic responses have been proposed among various races or ethnicities. Barbour et al. described in a Canadian observational study that persons of Pacific Asian origin might be at an increased risk of disease progression27.
The favorable association between corticosteroid use and kidney outcomes was greater in patients in the CS + Tx group than in the CS group (Fig. 2 and Table 2). Two RCTs from East Asia demonstrated a significant antiproteinuric effect of CS + Tx compared with CS15,16. A multicenter matched study in Japan revealed the association of tonsillectomy with better kidney survival independently from corticosteroid use17. The recent international clinical guideline added a special recommendation of tonsillectomy for Japanese patients with IgAN receiving corticosteroid therapy2. In contrast, the association of tonsillectomy with better kidney survival was not confirmed in European studies28,29. The reasons for these discrepant findings are not clear, but may relate to patient characteristics and the sample size of patients who underwent tonsillectomy. A genome-wide association study from Danish health registries demonstrated the association of one genetic variant with tonsillectomy risk (owing to severe tonsillitis or massive tonsillar hypertrophy) and IgAN susceptibility30. The same variant was also associated with IgAN progression in other studies31,32. Similar to the recent NEFIGAN trial, which was designed to deliver an enteric targeted-release formulation of budesonide to the distal ileum in patients with IgAN and demonstrated a significant antiproteinuric effect of the drug, tonsillectomy may be associated with better kidney outcome as one of the targeted therapies to lymphatic tissues responsible for production of nephritogenic IgA14. Recent findings from basic research indicate that tonsillar B lymphocytes or nasal-associated lymphoid tissue play a pivotal role in the production of nephritogenic IgA1, providing substantial support for this hypothesis33,34. In a similar vein, Kawabe et al. reported that conducting a tonsillectomy one year after kidney transplantation was correlated with a reduced incidence of histological recurrence of IgAN35. Further studies are needed to clarify how overtreatment with CS + Tx can be reduced, as the present study demonstrates that CS alone is associated with lower adverse kidney outcomes compared with non-CS treatment.
As indicated in KDIGO Guideline 2021, the present study found a significant association between initial treatment and kidney outcome among individuals with severe proteinuria (≥ 1.0 g/day). Meanwhile, there was no significant interaction observed between the proteinuria level (≥ 1.0 g/day and < 1.0 g/day) and the type of initial treatment (non-CS/CS/CS + Tx), as depicted in Fig. 4a. This observation aligns with findings from prior studies17,36,37. It is worth emphasizing that physicians should not hesitate unduly to administer corticosteroid treatment (+/− tonsillectomy) to patients with lower proteinuria than 1.0 g/day, in addition to providing supportive care. This perspective is substantiated by a study from China, which reported that patients with time-averaged proteinuria levels ranging from 0.5 to 1.0 g/day exhibited worse kidney outcomes38. However, it is crucial to highlight that our findings should be validated through further extensive observational studies and RCTs to establish their reliability.
The association of corticosteroid monotherapy with better kidney outcomes was not observed in patients with lesser baseline hematuria but in those with greater baseline hematuria in a subgroup analysis (Fig. 4a). To the best of our knowledge, this is the first study to focus on the different associations between corticosteroid use and kidney outcomes based on baseline hematuria levels. Despite the cardinal diagnostic importance of hematuria at baseline in IgAN, only a few studies have analyzed its influence on the outcome of the disease, and the results have been discordant38,39,40,41. Nagai et al. reported higher 2-year eGFR slope and improved eGFR trajectory after methylprednisolone pulse therapy in patients with greater baseline hematuria whereas eGFR was stable in those with relatively mild hematuria42. A recent meta-analysis reported that baseline macroscopic hematuria was associated with a decreased risk of ESKD whereas baseline microscopic hematuria was associated with an increased risk for ESKD43. Overall, isolated hematuria at the time of biopsy might have increased the sensitivity for early detection of IgAN. The non-significant association between corticosteroid use and kidney outcomes in patients with lesser hematuria noted in this study may provide a clue to avoiding overtreatment with CS in the clinical management of IgAN3. However, this issue should be examined in future studies.
Two glomerular acute lesions including endocapillary hypercellularity and crescent formation statistically influenced the response to CS and CS + Tx. Similar results were observed in a VALIGA sub-study and a Tokyo cohort sub-study6,7. Implications of those two acute glomerular lesions may be limited by that of microscopic hematuria as some previous studies have reported an association between baseline microscopic hematuria and those pathological glomerular acute lesions42,44. Future studies with pathological data from repeated kidney biopsy after corticosteroid therapy may help identify the effects of corticosteroid therapy on pathological changes in patients with IgAN.
This study has several limitations. Despite robust statistical techniques due to the nature of the observational study, possibility of residual and unmeasured confounding remains. Regimens for corticosteroid therapy and tonsillectomy, adverse events after initial treatment and relapse/recurrence during follow-up might affect kidney prognosis. Subsequent studies to investigate those issues are planned. Longer follow-up data from observational studies are required to assess whether the effects of initial corticosteroid therapy are sustained over time. The present cohort included only Japanese patients and data from Japanese clinical practices. Racial differences in the susceptibility genes for IgAN have been suggested in genome-wide association studies31,45. East Asia is known as a region with patients with the highest susceptibility to IgAN. Therefore, the applicability of these findings to other populations is unknown.
In conclusion, a favorable kidney survival response to corticosteroid monotherapy and an even more favorable response with combined corticosteroid therapy and tonsillectomy was demonstrated in a nationwide prospective observational overlap-weighted cohort. More attention to baseline microscopic hematuria and glomerular acute lesions including endocapillary hypercellularity and crescent may improve the clinical practice of IgAN and may avoid overtreatment in corticosteroid-treated patients with IgAN.
Methods
Data sources and study population
J-IGACS is a nationwide, multicenter, electronic health record-based registry of patients with biopsy-proven primary IgAN described elsewhere25. Briefly, the registration period in J-IGACS was from April 1, 2005, to August 31, 2015. The database contains information on all inpatient and outpatient encounters, prescriptions, diagnostic codes, laboratory measurements, and pathologic data collected between April 1, 2005, and May 31, 2021. Clinical datasets were uploaded every 6 months to the J-IGACS website by each investigator. Patients were followed up from the date when kidney biopsy was performed until migration or departure from the practice or database, death, or the last date of data collection.
For the current analyses, we selected records of patients from J-IGACS database who had kidney pathological data and measurements of arterial BP, eGFR, proteinuria, and uRBC when kidney biopsy was performed and at least one follow-up measure of kidney outcomes.
The study was approved by the Ethical Committee of the Jikei University School of Medicine (16–174 [4402]) and each local ethics committee where participants were enrolled. The current study was performed according to the Declaration of Helsinki and adhered to STROBE reporting guidelines. All patients and/or parents/guardians provided written informed consent before enrollment in J-IGACS.
Exposures
The exposure of interest was corticosteroid treatments comprising two types: CS and CS + Tx. Both were defined by initiation within 1 year after kidney biopsy. Each of the two exposure groups was compared to a group of patients who did not receive corticosteroid treatment within 1 year after kidney biopsy (non-CS). In further analyses, the CS + Tx group was compared with the CS group. Thus, the initial treatment categories included CS, CS + Tx, and non-CS, following intention-to-treat approach. Although the regimen of corticosteroid administration depended on each institute, principle one was one of two regimens: the Italian method and the Sendai method8,46. Both regimens involved corticosteroid pulse therapy, although the treatment duration varied between them (six versus twelve months).
Kidney outcome
For patients aged ≥ 20 years when kidney biopsy was performed, the primary outcome was a composite endpoint of dialysis induction or a ≥ 50% increase in serum creatinine from baseline (confirmed by subsequent measurements)8,17,47. For patients < 20 years of age when kidney biopsy was performed, the primary outcome was a composite endpoint of dialysis induction or a reduction in eGFR of ≥ 25% (confirmed by subsequent measurement). Patients were followed up from the date when kidney biopsy was performed until the occurrence of the outcome of interest or the last examination date.
Kidney function and other measurements
Serum creatinine and spot urine specimens were collected for each participant. Serum creatinine was assayed using an enzymatic method. In patients aged ≥ 20 years, eGFR was derived using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation modified by a Japanese coefficient48. In patients aged < 20 years at the time of kidney biopsy, eGFR was calculated using Uemura’s equation, and their follow-up eGFR measurements, collected at age > 20 years, were calculated using the revised CKD-EPI equation for Japanese adults49. The following equation was used to estimate mean arterial BP (MAP): MAP (mmHg) = 1/3 × pulse pressure + diastolic BP. The magnitude of microscopic hematuria was classified into two groups by its median value in the overall population. Regarding histological variables, we used the Oxford classification method (MEST-C score)50,51. The MEST-C score includes mesangial hypercellularity (M, M0/M1), endocapillary hypercellularity (E, E0/E1), segmental sclerosis (S, S0/S1), tubular atrophy/interstitial fibrosis (T, T0/T1 + 2), and crescents (C, C0/C1 + 2). The collected virtual slides were analyzed by five pathologists who were blinded to the clinical data. Final determinations of MEST-C scores were based on the agreement of three or more pathologists. Regarding renin–angiotensin–aldosterone system inhibitors (RAASi) use, if patients had already received RAASi at the time of kidney biopsy, such therapies with RAASi were also recorded as an initial prescription.
Statistical analysis
Descriptive statistics are presented as means and standard deviations (SDs), median and interquartile range (IQR), and numbers and proportions as appropriate. Incidence rates for the primary outcome were calculated as the frequency of the outcome per 1,000 person-years of follow-up.
A multinomial logistic regression model was used to estimate the generalized propensity score of treatment with CS or CS + Tx compared with non-CS, conditional on patient covariates measured at baseline52. In total, 25 baseline covariates, which were grouped into covariate set 1 and covariate set 2, were chosen a priori as potential confounders and included in the propensity score models. There were 13 variables in covariate set 1: age, gender, diabetes mellitus, MAP, eGFR, proteinuria, uRBC, five types of MEST-C scores, and RAASi use. Covariate set 2 included 12 variables: hypertension, past history of macrohematuria, body mass index, serum uric acid, serum IgA, serum complement 3, Japanese clinical grading score53, Japanese histological grading score54, antiplatelet use, registered year, registered hospital area, and category of registered hospital (university or local leading one). Covariate set 1 had no missing data. A multivariate singular value decomposition imputation method was used for selected variables in covariate set 2 if data were missing.
An overlap-weighting approach was then used to construct a weighted cohort of patients receiving CS, CS + Tx, and non-CS52,55. Balance in baseline covariates among CS, CS + Tx, and non-CS groups before and after overlap weighting was assessed using a measure of absolute standardized difference (ASD), where a standardized difference of ≤ 0.1 was considered to ensure balance between groups52,56. Two types of ASD were measured: max of the pairwise ASDs (MASD) and all of the pairwise ASDs (PASD).
The weighted cumulative incidence rate of the primary kidney outcome according to the initial treatment categories was evaluated using Kaplan–Meier analysis. The weighted incidence rate in each group was calculated as the weighted number of incident events divided by the weighted overall number of 1000 person-years at risk. For the main analysis, weighted Cox proportional hazards models were used to estimate the weighted hazard ratios (HRs) for the study outcome in comparisons of CS with non-CS, CS + Tx with non-CS, and CS + Tx with CS. The consistency of findings observed in the main analysis was assessed by the test to determine the interaction p values within each stratum of baseline characteristics57. Multivariate Cox proportional hazard modeling adjusted with all variables in covariate set 1, except for stratifying factor, was performed in this subgroup analysis; however, overlap weighting was used to estimate survival curves according to initial treatment and incidence rate of kidney outcomes in each stratum per 1000 patient-years. A statistically significant interaction was defined as p value for interaction < 0.1. All statistical analyses were performed using R 4.2.1 with package PSweight, JMP13.2.0 (SAS Institute, Inc, Cary, NC), and STATA MP16.1 (STATA Corp.). Statistical significance was defined as a two-sided p < 0.05.
Sensitivity analysis
Different inverse probability treatment weighting (IPW) analyses were employed in sensitivity analysis. Patients were weighted to derive the average treatment effect in the population that received CS + Tx (IPW-ATT) and the average treatment effect in the non-CS group (IPW-ATU)52. To assess the potential effects of unmeasured confounders on the identified associations between the exposures and the primary outcome, E-values were calculated58.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to ethical restrictions.
References
Wyatt, R. J. & Julian, B. A. MEdical progress: IgA nephropathy. N. Engl. J. Med. 368(25), 2402–24014. https://doi.org/10.1056/NEJMRA1206793/SUPPL_FILE/NEJMRA1206793_DISCLOSURES.PDF (2013).
Rovin, B. H. et al. KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int. 100(4), S1–S276. https://doi.org/10.1016/J.KINT.2021.05.021 (2021).
Rauen, T. et al. Intensive supportive care plus immunosuppression in IgA nephropathy. N. Engl. J. Med. 373(23), 2225–2236. https://doi.org/10.1056/NEJMoa1415463 (2015).
Lv, J. et al. Effect of oral methylprednisolone on clinical outcomes in patients with IgA nephropathy: The TESTING randomized clinical trial. JAMA 318(5), 432–442. https://doi.org/10.1001/jama.2017.9362 (2017).
Lv, J. et al. Effect of oral methylprednisolone on decline in kidney function or kidney failure in patients with IgA nephropathy: The TESTING randomized clinical trial. JAMA 327(19), 1888–1898. https://doi.org/10.1001/JAMA.2022.5368 (2022).
Tesar, V. et al. Corticosteroids in IgA nephropathy: A retrospective analysis from the VALIGA study. J. Am. Soc. Nephrol. 26(9), 2248–2258. https://doi.org/10.1681/ASN.2014070697 (2015).
Itami, S., Moriyama, T., Miyabe, Y., Karasawa, K. & Nitta, K. A novel scoring system based on Oxford classification indicating steroid therapy use for IgA nephropathy. Kidney Int. Rep. 7(1), 99–107. https://doi.org/10.1016/J.EKIR.2021.10.007 (2021).
Pozzi, C. et al. Corticosteroids in IgA nephropathy: A randomised controlled trial. Lancet (London, England) 353(9156), 883–887 (1999).
Manno, C., Torres, D. D., Rossini, M., Pesce, F. & Schena, F. P. Randomized controlled clinical trial of corticosteroids plus ACE-inhibitors with long-term follow-up in proteinuric IgA nephropathy. Nephrol. Dial. Transplant. 24(12), 3694–3701. https://doi.org/10.1093/ndt/gfp356 (2009).
Lv, J. et al. Combination therapy of prednisone and ACE inhibitor versus ACE-inhibitor therapy alone in patients with IgA nephropathy: A randomized controlled trial. Am. J. Kidney Dis. 53(1), 26–32. https://doi.org/10.1053/j.ajkd.2008.07.029 (2009).
Katafuchi, R. et al. Controlled, prospective trial of steroid treatment in IgA nephropathy: A limitation of low-dose prednisolone therapy. Am. J. Kidney Dis. 41(5), 972–983 (2003).
Rauen, T. et al. After ten years of follow-up, no difference between supportive care plus immunosuppression and supportive care alone in IgA nephropathy. Kidney Int. https://doi.org/10.1016/J.KINT.2020.04.046 (2020).
Habas, E. et al. IgA nephropathy pathogenesis and therapy: Review & updates. Medicine (Baltimore) 101(48), E31219. https://doi.org/10.1097/MD.0000000000031219 (2022).
Fellström, B. C. et al. Targeted-release budesonide versus placebo in patients with IgA nephropathy (NEFIGAN): A double-blind, randomised, placebo-controlled phase 2b trial. Lancet 389(10084), 2117–2127. https://doi.org/10.1016/S0140-6736(17)30550-0 (2017).
Kawamura, T. et al. A multicenter randomized controlled trial of tonsillectomy combined with steroid pulse therapy in patients with immunoglobulin A nephropathy. Nephrol. Dial. Transplant. 29(8), 1546–1553. https://doi.org/10.1093/ndt/gfu020 (2014).
Yang, D. et al. The efficacy of tonsillectomy on clinical remission and relapse in patients with IgA nephropathy: A randomized controlled trial. Ren. Fail. 38(2), 242–248. https://doi.org/10.3109/0886022X.2015.1128251 (2016).
Hirano, K. et al. Association between tonsillectomy and outcomes in patients with immunoglobulin a nephropathy. JAMA Netw. Open https://doi.org/10.1001/jamanetworkopen.2019.4772 (2019).
Duan, J., Liu, D., Duan, G. & Liu, Z. Long-term efficacy of tonsillectomy as a treatment in patients with IgA nephropathy: A meta-analysis. Int. Urol. Nephrol. 49(1), 103–112. https://doi.org/10.1007/s11255-016-1432-7 (2017).
Kiyono, H. & Fukuyama, S. NALT- versus Peyer’s-patch-mediated mucosal immunity. Nat. Rev. Immunol. 4(9), 699–710. https://doi.org/10.1038/NRI1439 (2004).
Yuki, Y. & Kiyono, H. New generation of mucosal adjuvants for the induction of protective immunity. Rev. Med. Virol. 13(5), 293–310. https://doi.org/10.1002/RMV.398 (2003).
Clarkson, A. R. et al. IgA nephropathy: A syndrome of uniform morphology, diverse clinical features and uncertain prognosis. Clin. Nephrol. 8(5), 459–471 (1977).
Ueda, H. et al. Gross hematuria following SARS-CoV-2 infection in IgA nephropathy: A report of 5 cases. Kidney Med. 5(6), 100627. https://doi.org/10.1016/J.XKME.2023.100627 (2023).
Aratani, S. et al. Tonsillectomy combined with steroid pulse therapy prevents the progression of chronic kidney disease in patients with immunoglobulin A (IgA) nephropathy in a single Japanese institution. Cureus https://doi.org/10.7759/CUREUS.15736 (2021).
Li, Y. et al. Efficacy and indications of tonsillectomy in patients with IgA nephropathy: A retrospective study. PeerJ https://doi.org/10.7717/PEERJ.14481 (2022).
Joh, K. et al. Structural modeling for Oxford histological classifications of immunoglobulin A nephropathy. PLoS One https://doi.org/10.1371/JOURNAL.PONE.0268731 (2022).
Zhang, Z., Yang, Y., Jiang, S. M. & Li, W. G. Efficacy and safety of immunosuppressive treatment in IgA nephropathy: A meta-analysis of randomized controlled trials. BMC Nephrol. https://doi.org/10.1186/S12882-019-1519-3 (2019).
Barbour, S. J. et al. Individuals of Pacific Asian origin with IgA nephropathy have an increased risk of progression to end-stage renal disease. Kidney Int. 84(5), 1017–1024. https://doi.org/10.1038/KI.2013.210 (2013).
Rasche, F. M., Schwarz, A. & Keller, F. Tonsillectomy does not prevent a progressive course in IgA nephropathy. Clin. Nephrol. 51(3), 147–152 (1999).
Feehally, J. et al. Tonsillectomy in a European cohort of 1,147 patients with IgA nephropathy. Nephron 132(1), 15–24. https://doi.org/10.1159/000441852 (2016).
Feenstra, B. et al. Genome-wide association study identifies variants in HORMAD2 associated with tonsillectomy. J. Med. Genet. 54(5), 358–364. https://doi.org/10.1136/jmedgenet-2016-104304 (2017).
Kiryluk, K., Li, Y., Sanna-Cherchi, S. et al. Geographic Differences in Genetic Susceptibility to IgA Nephropathy: GWAS Replication Study and Geospatial Risk Analysis. McCarthy MI, ed. PLoS Genet. 8(6), e1002765. https://doi.org/10.1371/journal.pgen.1002765 (2012)
Shi, M. et al. IgA nephropathy susceptibility loci and disease progression. Clin. J. Am. Soc. Nephrol. 13, 1330–1338. https://doi.org/10.2215/CJN.13701217 (2018).
Muto, M. et al. Toll-like receptor 9 stimulation induces aberrant expression of a proliferation-inducing ligand by tonsillar germinal center B cells in IgA nephropathy. J. Am. Soc. Nephrol. 28(4), 1227–1238. https://doi.org/10.1681/ASN.2016050496 (2017).
Kano, T., Suzuki, H., Makita, Y., Fukao, Y. & Suzuki, Y. Nasal-associated lymphoid tissue is the major induction site for nephritogenic IgA in murine IgA nephropathy. Kidney Int. 100(2), 364–376. https://doi.org/10.1016/J.KINT.2021.04.026 (2021).
Kawabe, M. et al. Association between galactose-deficient IgA1 derived from the tonsils and recurrence of IgA nephropathy in patients who underwent kidney transplantation. Front. Immunol. https://doi.org/10.3389/FIMMU.2020.02068 (2020).
Shirai, S. et al. Prognostic factors of IgA nephropathy presenting with mild proteinuria at the time of diagnosis (a multicenter cohort study). Clin. Exp. Nephrol. 27(4), 340–348. https://doi.org/10.1007/S10157-023-02316-2 (2023).
Ogura, S., Moriyama, T., Miyabe, Y., Karasawa, K. & Nitta, K. Evaluation of appropriate treatment for IgA nephropathy with mild proteinuria and normal renal function. Clin. Exp. Nephrol. 2086;25, 1103–1110. https://doi.org/10.1007/s10157-021-02086-9
Le, W. et al. Long-term renal survival and related risk factors in patients with IgA nephropathy: Results from a cohort of 1155 cases in a Chinese adult population. Nephrol. Dial. Transplant. 27(4), 1479–1485. https://doi.org/10.1093/ndt/gfr527 (2012).
Iwasaki, C., Moriyama, T., Tanaka, K., Takei, T. & Nitta, K. Effect of hematuria on the outcome of immunoglobulin A nephropathy with proteinuria. J. Nephropathol. 5(2), 72–78. https://doi.org/10.15171/jnp.2016.12 (2016).
Yu, G. et al. Persistent hematuria and kidney disease progression in IgA nephropathy: A cohort study. Am. J. Kidney Dis. 76(1), 90–99. https://doi.org/10.1053/J.AJKD.2019.11.008 (2020).
Deng, W. et al. Gender-related differences in clinicopathological characteristics and renal outcomes of Chinese patients with IgA nephropathy. BMC Nephrol. https://doi.org/10.1186/S12882-018-0829-1 (2018).
Nagai, M., Kobayashi, N., Izumi, N., Ohbayashi, T., Osamu, H. & Hamano, T. Pre-treatment hematuria and crescents predict estimated glomerular filtration rate trajectory after methylprednisolone pulse therapy with tonsillectomy for IgA nephropathy Graphic abstract Keywords IgA nephropathy · Methylprednisolone pulse therapy with tonsillectomy · Severity of pre-treatment hematuria · Cellular/fibrocellular crescent. J. Nephrol. 123AD;1:3. https://doi.org/10.1007/s40620-021-01064-4
He, P., Wang, H., Huang, C. & He, L. Hematuria was a high risk for renal progression and ESRD in immunoglobulin a nephropathy: A systematic review and meta-analysis. Ren. Fail. 43(1), 488–499. https://doi.org/10.1080/0886022X.2021.1879852 (2021).
Tang, X., Wen, Q., Zhou, Q. & Chen, W. Clinicopathological characteristics and prognosis of patients with IgA nephropathy and renal vasculitic lesions. BMC Nephrol. https://doi.org/10.1186/S12882-021-02556-Y (2021).
Magistroni, R., D’Agati, V. D., Appel, G. B. & Kiryluk, K. New developments in the genetics, pathogenesis, and therapy of IgA nephropathy. Kidney Int. 88(5), 974–989. https://doi.org/10.1038/ki.2015.252 (2015).
Sato, M. et al. Cohort study of advanced IgA nephropathy: Efficacy and limitations of corticosteroids with tonsillectomy. Nephron Clin. Pract. https://doi.org/10.1159/000070233 (2003).
Praga, M., Gutiérrez, E., González, E., Morales, E. & Hernández, E. Treatment of IgA nephropathy with ACE inhibitors: A randomized and controlled trial. J. Am. Soc. Nephrol. 14(6), 1578–1583 (2003).
Matsuo, S. et al. Revised equations for estimated GFR from serum creatinine in Japan. Am. J. Kidney Dis. 53(6), 982–992. https://doi.org/10.1053/j.ajkd.2008.12.034 (2009).
Uemura, O. et al. Creatinine-based equation to estimate the glomerular filtration rate in Japanese children and adolescents with chronic kidney disease. Clin. Exp. Nephrol. 18(4), 626–633. https://doi.org/10.1007/s10157-013-0856-y (2014).
Cattran, D. C. et al. The Oxford classification of IgA nephropathy: Rationale, clinicopathological correlations, and classification. Kidney Int. 76(5), 534–545. https://doi.org/10.1038/ki.2009.243 (2009).
Coppo, R. et al. Validation of the Oxford classification of IgA nephropathy in cohorts with different presentations and treatments. Kidney Int. 86(4), 828–836. https://doi.org/10.1038/ki.2014.63 (2014).
Li, F. A. N. & Li, F. A. N. Propensity score weighting for causal inference with multiple treatments. Ann. Appl. Stat. 13(4), 2389–2415. https://doi.org/10.1214/19-AOAS1282 (2019).
Okonogi, H. et al. A grading system that predicts the risk of dialysis induction in IgA nephropathy patients based on the combination of the clinical and histological severity. Clin. Exp. Nephrol. 23(1), 16–25. https://doi.org/10.1007/s10157-018-1657-0 (2019).
Kawamura, T. et al. A histologic classification of IgA nephropathy for predicting long-term prognosis: Emphasis on end-stage renal disease. J. Nephrol. 26(2), 350–357. https://doi.org/10.5301/jn.5000151 (2013).
Thomas, L. E., Li, F. & Pencina, M. J. Overlap weighting: A propensity score method that mimics attributes of a randomized clinical trial. JAMA 323(23), 2417–2418. https://doi.org/10.1001/JAMA.2020.7819 (2020).
Austin, P. C. Assessing balance in measured baseline covariates when using many-to-one matching on the propensity-score. Pharmacoepidemiol. Drug Saf. 17(12), 1218–1225. https://doi.org/10.1002/PDS.1674 (2008).
Austin, P. C. Variance estimation when using inverse probability of treatment weighting (IPTW) with survival analysis. Stat. Med. 35(30), 5642–5655. https://doi.org/10.1002/SIM.7084 (2016).
VanderWeele, T. J. & Ding, P. Sensitivity analysis in observational research: Introducing the E-value. Ann. Intern. Med. 167(4), 268. https://doi.org/10.7326/M16-2607 (2017).
Acknowledgements
We thank all study participants and clinicians for their kind cooperation. We would like to thank A.S. for processing the data. We would like to thank the additional primary investigators*, co-investigators, clinicians, research personnel, study team, and families who participated in J-IGACS. In addition, we would like to express our gratitude and remembrance to Dr. Satoshi.Hisano who is one of the five pathologists. This study was supported in part by a Grant-in-Aid for Progressive Renal Diseases Research, Research on Rare and Intractable Disease, from the Ministry of Health, Labour and Welfare of Japan. This research was supported by AMED under grant number JP19ek0109261. *Primary investigators in J-IGACS. Yasuda T, Shirai S, St. Marianna University School of Medicine; Yoshimura M, Kitagawa K, Kanazawa Medical Center; Hattori M, Akioka Y, Nitta K, Moriyama T, Tokyo Women’s Medical University; Nishino T, Nagasaki University; Shibata T, Showa University School of Medicine; Endo M, Tokai University School of Medicine; Wada A, Osaka National Hospital; Yamanaka M, Kyusyu Medical Center; Mitsuiki K, Japanese Red Cross Fukuoka Hospital; Sasatomi Y, Fukuoka University Hospital; Wada T, Kanazawa University Hospital; Muso E, Kitano Hospital; Fujimoto S, Sato Y, University of Miyazaki Hospital; Ito T, Shimane University Hospital; Yamagata K, University of Tsukuba Hospital; Hiromura K, Gunma University Hospital; Nishi S, Goto S, Kobe University Hospital; Yanagita M, Kyoto University Hospital; Tsuchimoto A, Yamada S, Kyushu University Hospital; Fukunaga K, Toyonaka Municipal Hospital; Ishikawa M, Kawaguchi Municipal Medical Center; Nagata D, Sato R, Jichi Medical University Hospital; Okada D, Yamada Y, Tottori University Hospital; Ichikawa K, Yamagata University Hospital; Sato M, Sendai Hospital; Nakagawa N, Asahikawa Medical University Hospital; Yuzawa Y, Takahashi K, Fujita Health University Hospital; Hataya H, Tokyo Metropolitan Tama Medical Center; Sakai Y, Nippon Medical School Hospital; Uchida S, Fujigaki Y, Teikyo University School of Medicine; Urushihara M, Kagami S, Tokushima University Hospital; Ishimura E, Nakatani S, Osaka Metropolitan University Hospital; Kobayashi M, Tokyo Medical University Ibaraki Medical Center; Takeda T, Kawamoto S, Dokkyou Medical University Saitama Medical Center.
Author information
Authors and Affiliations
Contributions
T.K. and K.H. designed the study; A.S., K.J., R.K., and A.H. scored histological grading; K.K., K.H., and M.N. analyzed the data; K.H. and K.K. created the figures; T.K. K.H., M.N., K.K., and Y.Y. drafted the manuscript; T.K., K.H., K.K., M.N., A.S., K.J., R.K., K.H, K.M., S.M., N.T., I.N., Y.Y., T.Y., and Y.S. revised the manuscript; all authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kawamura, T., Hirano, K., Koike, K. et al. Associations of corticosteroid therapy and tonsillectomy with kidney survival in a multicenter prospective study for IgA nephropathy. Sci Rep 13, 18455 (2023). https://doi.org/10.1038/s41598-023-45514-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45514-4
This article is cited by
-
A case of IgA nephropathy associated with Crohn’s disease treated with enteric-coated budesonide
CEN Case Reports (2025)
-
Effect of tonsillectomy combined with steroid pulse therapy upon IgA nephropathy depending on proteinuria status at diagnosis: a nationwide multicenter cohort study in Japan
Clinical and Experimental Nephrology (2024)