Abstract
The study aims to investigate the distress level and its influencing factors in Chinese pulmonary nodules patients. A total of 163 outpatients in a tertiary hospital in Xi'an, China, were recruited and investigated by using the Impact of Event Scale, Decision Conflict Scale, Consultation Care Measure, Lung Cancer Worry Scale and a demographic questionnaire. The logistic regression model was used to identify the factors of distress. The mean IES score was 37.35 ± 16.65, which was a moderate level. Patients aged 50–60 years, with higher decision conflicts scores, lower physician–patient communication quality score, and who are anxious about the results of future tests or treatments had higher distress score. Distress levels were moderate in patients with pulmonary nodules. Communication between medical staff and patients is extremely important for the management of pulmonary nodules, which affects the quality of the patient's decision-making and his level of distress.
Similar content being viewed by others
Introduction
Lung Cancer has the second-highest incidence rate and the highest mortality rate in the world1, and it is the most common cancer in China with new cases and deaths accounting for nearly 40% in the whole world2. Early detection is important for lung cancer prevention and management. Results of the National Lung Screening Trial (NLST) showed that screening with low-dose computed tomography (LDCT) can reduce lung cancer mortality by 20%3. The latest study shows that one-off LDCT screening in high-risk populations in China can reduce lung cancer mortality by 30%4. In 2012, the Chinese government launched a key national plan for public health, Cancer Screening Program in Urban China (CANSPUC), in which participants at high risk aged 40–74 were provided free LDCT test for lung cancer screening5.
With the widespread use of computed tomography (CT) technology, pulmonary nodules are becoming more common. Nearly 26.3% of pulmonary nodules were found on annual routine checkups6. After being diagnosed, patients have questions about the meaning of the nodules.
With the increasing prevalence of non-smoking related lung cancer in Asian countries, LDCT screening for non-smoking population is widely utilized in Asian countries and regions, such as China, Taiwan (province of China), Korea, Japan. Population anxiety about lung cancer was high in China due to patients died of stage IV lung cancer, unknown risk factors for non-smoking lung cancer, and safe strategies culture in Asian population culture, especially in non-smoking and female populations7.
Since pulmonary nodules have the potential to become early lung cancer lesions, patients may become anxious and depressed. Harris et al. believed that this "near cancer" diagnosis would bring various harms to patients, including physical harms, psychological harms, financial strain, and opportunity costs8. It is worth noting that very few patients benefit from lung cancer screening (most of them are benign), but nearly all patients are at risk of different types of harms from detection and evaluation of a pulmonary nodule3,9.
It is difficult to make an accurate judgment of benign and malignant after the first detection of pulmonary nodules. Patients care about the next step in the diagnosis and treatment plan10. Common options for the management of pulmonary nodules in the guidelines include CT surveillance, biopsy, and excision. However, each option has its advantages and disadvantages11, and it is a challenge for doctors and patients to choose which one to use. It involves the characteristics of the nodule itself, the patient's history of exposure to lung cancer risk factors, the doctor's judgment, and the patient's personal preference. Patients may be caught in a decision-making dilemma.
Decision conflict is when individuals face choices involving risks or unknown outcomes, they need to evaluate the potential benefits and risks corresponding to the options, weigh the value of making a decision, and prepare for losing the advantages of the rejected options12. Decision conflict can lead to delayed decision-making, reduce treatment compliance, and affect the patient's psychology. Studies on breast cancer and diabetes patients have shown that there is a positive correlation between decision conflict and distress, and the uncertainty in decision-making can lead to individual psychological and emotional distress13,14. Communication between doctors and patients is very important for this kind of decision conflict faced by patients. This communication is not just the simple transmission of medical information, but also requires emotional exchange. Some researchers believe that high-quality communication can effectively alleviate the distress level of patients.
In the context of the high incidence of lung cancer, the distress level of patients with pulmonary nodules in China is unknown. Since the nature of pulmonary nodules requires the patient to further choose a certain way to determine, the patient needs to communicate with the medical staff during the decision-making process, and decisional conflict, communication quality with doctor, and lung cancer worry are closely related to the patient in this process. The purpose of this study was to investigate the distress level and its influencing factors in Chinese patients with incidental pulmonary nodules.
Method
Aim
The study aims to investigate the distress level and its influencing factors in Chinese pulmonary nodules patients.
Design
This is a cross-sectional study and adhered to the STROBE checklist for observational research.
Sample
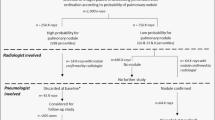
Participants were eligible for this study if they were 18 years of age or older with a diagnosis of pulmonary nodule (with diameter less than 30 mm) after opportunistic CT examination for the first time. People who had mental illnesses or any type of cancer were excluded. Kendall et al.15 suggested that the study sample size should be 5–10 times of the study factors. This study contains 12 variables, considering the sample loss of 20%, the sample size of this study needs to be at least 150 participants. Using convenience sampling, 165 pulmonary patients at the respiratory clinic of a tertiary hospital in Xi’an were recruited from July 2021 to October 2021. Two patients declined to participate for time reasons, and 163 participants were eventually included in the study.
Data collection
All the questionnaire and scales were completed by the patient alone. After the participants completed the questionnaire, the researchers immediately checked the questionnaire and collected it on the spot. The data collection timing flow chart see Fig. 1.
Social-demographic characteristics
Socio-demographic questionnaire included age, gender, education level, marital status, employment status, income level, residence, smoking history, relatives with lung cancer, if the patients worried about getting lung cancer someday, and if the patients anxious about the results of future tests/treatments.
Distress
Impact of Event Scale (IES) was used to measure distress. IES, originally designed by Horowitz in 1979, measures an individual's current level of subjective distress due to the impact of a specific event. In 2003, Zhao et al. translated it into a Chinese version16. The scale contains 15 items and 2 dimensions, including intrusion (7 items) and avoidance (8 items). Each item was scored on a 4-point scale (0 = not at all, 1 = rarely, 3 = sometimes, and 5 = often). The total scale score ranges from 0 to 7517, with higher scores indicating a greater frequency of intrusive thoughts and attempts at avoidance. In this study, according to other research, a total score of 0–25 was classified as mild or below level, and above 26 was considered moderate or high level18.
Decision conflict
The Decision Conflict Scale (DCS) was used to measure the decision conflict of patients with pulmonary nodules when deciding the next treatment or surveillance plan. DCS was originally designed by O’Connor in 12 and was later translated into a Chinese version by Li et al.19 The scale contains 16 items divided into 3 subscales: including information and values, decision support and effectiveness and decision uncertainty. The scale was scored using the Likert 5-level scoring method, and the initial score was converted into 0–100 points to obtain the total score.
Communication quality with doctor
Consultation Care Measure (CCM) is used to measure the quality of communication between doctors and patients about pulmonary nodules. The CCM is designed based on a patient-centered communication model20,21 to measure patients' perceptions of communication quality after communicating with doctors. The primary measure of the perception of communication was the statement, “The overall quality of communication with your provider (who is caring for your nodule) is excellent,” rated on a 7-point Likert scale from “very strongly disagree” to “very strongly disagree” strongly agree.”18. Higher scores indicate that patients perceive the higher quality of communication.
Lung cancer worry
The Lung cancer worry scale (LCWS)was used to measure fear and anxiety in patients with pulmonary nodules about being diagnosed with lung cancer in the future. The scale was modified from the cancer worry scale by changing breast cancer to lung cancer and by changing mammograms to future tests/treatments22. Clark et al. applied it for the first time in patients with pulmonary nodules, and there were four questions in the scale. Since we included patients diagnosed for the first time, only two questions were included: “How worried are you about getting lung cancer someday?” and “What is your current anxiety level about the results of future tests/treatments?" These two questions were dichotomized as "not worried" vs. "worried" and "not anxious" vs. "anxious".
Ethics and consent statement
Our research was approved by the Medical Ethics Review Committee of the First Affiliated Hospital of Xian Jiaotong University, and all methods were performed in accordance with the relevant guidelines and regulations. Patients were informed about the study and invited to participate the survey. The data were anonymous, and coded using participant-created codes.
Data analyses
IBM SPSS Statistics software version 26.0 was used to analyse data. The demographic data were summarized as the means, standard deviations, and ranges for continuous variables and as frequency counts (percentages) for categorical variables. We calculated the means and standard deviations of distress and 2 dimensions, and reported low or mild and moderate or high levels using frequencies and percentages. The differences in distress according to demographic characteristics were analysed using t-tests and one-way analysis of variance (ANOVA). Pearson's correlation analyses were used to investigate the correlations between distress and both decision conflict and communication quality score. Multivariate logistic regression model was constructed to explore the influencing factors of distress among pulmonary nodules patients. All socio-demographic factors, decision conflict, communication quality, lung cancer worry were included in the multilevel analysis. An alpha level of 0.05 was used for the assessment of statistical significance.
Validity and reliability
All manually entered data were double-checked. The Cronbach’s α of IES, the intrusion and avoidance subscale are 0.90, 0.88 and 0.81, respectively16. DCS has good reliability and validity, with Cronbach’s α coefficient of 0.897 and content validity index of 0.95023. Cronbach’s α for LCWS used in relation to breast and prostate cancer ranges from 0.71 to 0.86.
Results
Demographic characteristics
A total of 163 patients with incidental pulmonary nodules were included in this study, with an average age of 54 years (SD = 12.9, range 27–85), of whom 91 (55.8%) were female. Most participants were married (93.9%). Nearly half (47.2%) of patients with pulmonary nodules were worried about being diagnosed with lung cancer in the future, and about 33.7% were worried about the results of their next test. Detailed demographic characteristics are shown in Table 1.
Distress, decision conflict, and communication quality
The mean and standard deviation of distress, decision conflict, and communication quality scores were 37.6 (SD = 16.7), 51.32 (SD = 19.5), and 3.3 (SD = 1.7), respectively.
About 73.6% (n = 120) of patients reported a moderate or high level of distress. (Table 2).
Relationships among distress, demographic characteristics, decision conflict, lung cancer worry, and communication quality
Table 1 shows the relationship between distress and demographic characteristics and lung cancer worry. The correlation analyses showed that decision conflict was positive associated with distress (r = 0.597, p < 0.001) while communication quality was negatively associated with distress (r = 0.403, p < 0.001).
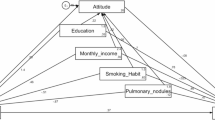
Influencing factors of distress among incidental pulmonary nodules patients
The logistic regression results showed that decision conflict, age, communication quality, and anxiety level about future test results were the main factors that influenced distress among incidental pulmonary nodules patients. (Table 3).
Discussion
Distress level of pulmonary nodule patients
This study investigated the distress level and its influencing factors in Chinese patients with incidental pulmonary nodules. It was found that the vast majority of patients developed a certain level of distress after being diagnosed with a pulmonary nodule. This result is similar to that of Moseson and Slatore, who used IES to investigate patients with pulmonary nodules18,24.
Many patients with pulmonary nodules have certain anxiety and distress emotions25. Although only about 4% of pulmonary nodules will eventually be diagnosed as lung cancer3, it is difficult to make an accurate judgment immediately26, so the “near-cancer” diagnosis is a big burden to patients. Some patients even thought they had cancer immediately after being diagnosed with a pulmonary nodule27.
Horowitz described the connotations of the 2 dimensions of event impact. Intrusions are thoughts and images that spontaneously, involuntarily appear in the mind, with troubled dreams, strong pangs, and waves of feelings. Avoidance responses include ideational constriction, denial of the meaning and outcome of events, numbness of sensations, inhibition of behavior, or counterphobic activity 28. This study showed that patients with pulmonary nodules have moderate scores in both dimensions, suggesting that the two types of thoughts exist in patients. When a patient is diagnosed with a pulmonary nodule, there is a spot in the lung, which reminds the patient from time to time that he has a pulmonary nodule and it has the potential to become lung cancer. However, since most pulmonary nodules require regular follow-up, under the advice of doctors, patients will take the initiative to suggest to themselves and try to avoid thinking about it.
Influencing factors of distress
Decision conflict is an important influencing factor of patients' distress. Pulmonary nodules are poorly understood by patients27, and their decisions require a wealth of information from their doctors, as well as an understanding of the pros and cons of each option. However, doctors give patients less information due to several factors. This may be related to the fact that pulmonary nodules are very common, doctors need to deal with a large number of patients, and their time and energy are limited26. In addition, physicians may be worried that giving too much information would be overwhelming and might actually increase patient distress, so they seldom directly inform the risk of lung cancer and other details about surveillance to their patients29. Based on the current context, the British Thoracic Society guidelines suggest that the involvement of lung cancer nurses in further communication with patients would be beneficial30. However, these nurses need to be skilled in the prevention and management of lung cancer and pulmonary nodules, such as epidemiology, risk factors, screening methods, and further management of pulmonary nodules (including advantages and disadvantages). In this process, the idea of shared decision-making can be applied. In addition, since in-depth conversation with patients may involve patients in decision-making, nurses need to receive specialized training to provide decision-making Support for patients, such as The Ottawa Decision Support Tutorial31.
The communication quality score was also entered into the regression model. It is similar to the results of Slatore et al., the higher the quality of patient self-rated communication, the lower the distress level24. In the current clinical decision-making, the paternalistic or informed model is mostly used, which has problems such as low degree of information sharing and low decision satisfaction23. A core criterion for high-quality decision-making is whether the choice is in line with the patient's values, goals, and preferences. This requires medical staff to learn more about patients' thoughts and consider personal preferences during the communication process. In addition, the communication between doctors and patients about the decision-making of the next diagnosis and treatment plan is not only a one-way information transfer of medical knowledge, but also an emotional exchange. Patients’ distress decreases when their clinicians were empathic and generated trust27,32.
The regression results showed that age is also a factor affecting distress. Compared with people younger than 50 years old, patients aged 50–60 years have a higher risk of distress. This may be because the age of 50–60 is still the backbone of the society and the family in the current Chinese society, bearing the heavy burden of the society and the family. When a certain disease is diagnosed, the negative emotions caused by it are heavier. Bivariable analysis by Freiman et al. showed that age over 65 years was a protective factor for distress in patients with pulmonary nodules33. Similarly, the results of Li et al. showed that patients with pulmonary nodules between the ages of 40 and 60 had the highest proportion of anxiety, but it was not statistically significant34. Further research is needed on the association of age with distress in patients with pulmonary nodules.
We found that anxiety about the next test result, but not worry about lung cancer, was an influencing factor of distress. Similar to breast cancer screening, when an individual has a false-positive screening result, it may experience a period of distress. The difference is that distress in false-positive individuals of breast cancer screening is transient, and it disappears immediately after a negative biopsy result26. Many patients with pulmonary nodules may be required to follow regular surveillance, leaving them in a state of uncertainty for months or even years. Consequently, the next test results were more closely and directly related to their mood compared with cancer.
Limitations
We should mention that this study has several limitations. Since the design is a cross-sectional study, there may be attentional bias and selection bias in the study. The researchers investigated outpatient patients with pulmonary nodules in a tertiary hospital of a provincial capital city. The level of medical care varies among hospitals of different levels, which may affect the distress among patients with pulmonary nodules. Due to differences in the description of pulmonary nodules in imaging reports among different physicians, the characteristics of individual pulmonary nodules were not included in this study. In addition, the quality of doctor-patient communication is measured through patient self-assessment. To truly reflect the quality of communication, it is beneficial to comprehensively consider the evaluation of communication quality by doctors and third parties. Due to the limited sample size, the odds ratio of age group 50–60 might inflated35. Finally, Due to the limitations of the cross-sectional study, the causal relationship between the variables needs to be further investigated.
Conclusion
We found that distress levels were moderate in patients with pulmonary nodules. Age, higher decision conflicts scores, lower physician–patient communication quality score, and being anxious about the results of future tests or treatments are influencing factors of distress among pulmonary nodule patients.
Practice implications
In the screening process, in addition to the patients who are finally diagnosed with lung cancer, patients with positive results after screening also need more attention. Due to the heavy clinical tasks of doctors, nurses may play an important role in the health guidance of patients with pulmonary nodules. In this process, patients are informed of the alternative pulmonary nodules management options and the pros and cons of each option. Patient's own decision-making preferences needs more attention, and therapeutic alliance needs to be established between doctor, nurse and patients. This patient-centered communication method can not only effectively eliminate the decision conflicts, but also allow patients to participate in decision-making, which greatly improves the quality of communication and decision. Of course, the feasibility and effectiveness of this model need further experiments to confirm.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Siegel, R. L., Miller, K. D., Fuchs, H. E. & Jemal, A. Cancer statistics, 2021. CA Cancer J. Clin. 71, 7–33 (2021).
Yuan, J. et al. Cost effectiveness of lung cancer screening with low-dose CT in heavy smokers in China. Cancer Prev. Res. 15, 37–44 (2022).
Aberle, D. R. et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 365, 395–409 (2011).
Li, N. et al. One-off low-dose CT for lung cancer screening in China: A multicentre, population-based, prospective cohort study. Lancet Respir. Med. 10, 378–391 (2022).
Guo, L. W. et al. Evaluation of a low-dose computed tomography lung cancer screening program in Henan, China. JAMA Netw. Open 3, e2019039 (2020).
He, Y. T. et al. Risk factors for pulmonary nodules in north China: A prospective cohort study. Lung Cancer 120, 122–129 (2018).
Wu, F. Z., Wu, Y. J., Chen, C. S. & Yang, S. C. Impact of smoking status on lung cancer characteristics and mortality rates between screened and non-screened lung cancer cohorts: Real-world knowledge translation and education. J. Pers. Med. 12, 26 (2022).
Harris, R. P. et al. The harms of screening: A proposed taxonomy and application to lung cancer screening. JAMA Intern. Med. 174, 281–285 (2014).
Yuan, J. et al. Cost-effectiveness of lung cancer screening combined with nurse-led smoking cessation intervention: A population-based microsimulation study. Int. J. Nurs. Stud. 134, 104319 (2022).
Wiener, D. C. & Wiener, R. S. Patient-centered, guideline-concordant discussion and management of pulmonary nodules. Chest 158, 416–422 (2020).
Bai, C. et al. Evaluation of pulmonary nodules: Clinical practice consensus guidelines for Asia. Ches. 150, 877–893 (2016).
O’Connor, A. M. Validation of a decisional conflict scale. Med. Decis Making. 15, 25–30 (1995).
Bruno, B. A., Choi, D., Thorpe, K. E. & Yu, C. H. Relationship among diabetes distress, decisional conflict, quality of life, and patient perception of chronic illness care in a cohort of patients with type 2 diabetes and other comorbidities. Diabetes Care. 42, 1170–1177 (2019).
Lam, W. W. et al. Psychometric assessment of the Chinese version of the decisional conflict scale in Chinese women making decision for breast cancer surgery. Health Expect. 18, 210–220 (2015).
Bonett, D. G. & Wright, T. A. Sample size requirements for estimating pearson, kendall and spearman correlations. Psychometrika 65, 23–28 (2000).
Zhao, C., Wang, X., Chang, L., Jin, Y. & Tian, F. Reliability and validity of the impact of event scale in Chinese traumatic event suffers. Chin. Mental Health J. 17, 679–681 (2003).
Joseph, S. Psychometric evaluation of Horowitz’s impact of event scale: A review. J. Trauma. Stress 13, 101–113 (2000).
Moseson, E. M. et al. Patient and clinician characteristics associated with adherence. A cohort study of veterans with incidental pulmonary nodules. Ann. Am. Thorac. Soc. 13, 651–659 (2016).
Li, Y. Construction and Application of Treatment Decision Aids for Early-Stage Primary Liver Cancer Patients (Naval Medical University, 2017).
Mead, N. & Bower, P. Patient-centredness: A conceptual framework and review of the empirical literature. Soc. Sci .Med. 51, 1087–1110 (2000).
Haes, H. & Bensing, J. Endpoints in medical communication research, proposing a framework of functions and outcomes. Patient Educ. Couns. 74, 287–294 (2009).
Lerman, C. et al. Mammography adherence and psychological distress among women at risk for breast cancer. J. Natl. Cancer Inst. 85, 1074–1080 (1993).
Zheng, H., Hu, J., Dong, B. & Yang, Y. Research progress on the messurements of Shared Decision Making among physicians and patients. Chin. J. Nurs. 53, 622–625 (2018).
Slatore, C. G., Golden, S. E., Ganzini, L., Wiener, R. S. & Au, D. H. Distress and patient-centered communication among veterans with incidental (not screen-detected) pulmonary nodules. A cohort study. Ann. Am. Thorac. Soc. 12, 184–192 (2015).
Wang, L. et al. Correlation between anxiety, depression and changes in Th17/Treg and inflammatory levels in patients with pulmonary nodules. Chin. J. Lung Cancer 23, 554–560 (2020).
Slatore, C. G. & Wiener, R. S. Pulmonary nodules: A small problem for many, severe distress for some, and how to communicate about it. Chest 153, 1004–1015 (2018).
Wiener, R. S., Gould, M. K., Woloshin, S., Schwartz, L. M. & Clark, J. A. What do you mean, a spot?: A qualitative analysis of patients’ reactions to discussions with their physicians about pulmonary nodules. Chest 143, 672–677 (2013).
Horowitz, M., Wilner, N. & Alvarez, W. Impact of Event Scale: A measure of subjective stress. Psychosom. Med. 41, 209–218 (1979).
Golden, S. E., Wiener, R. S., Sullivan, D., Ganzini, L. & Slatore, C. G. Primary care providers and a system problem: A qualitative study of clinicians caring for patients with incidental pulmonary nodules. Chest 148, 1422–1429 (2015).
Callister, M. E. et al. British Thoracic Society guidelines for the investigation and management of pulmonary nodules. Thorax 70(Suppl 2), i1-54 (2015).
Boland, L. et al. Evaluation of a shared decision making educational program: The Ottawa Decision Support Tutorial. Patient Educ. Couns. 102, 324–331 (2019).
Slatore, C. G. et al. What the heck is a “nodule”? A qualitative study of veterans with pulmonary nodules. Ann. Am. Thorac. Soc. 10, 330–335 (2013).
Freiman, M. R. et al. Patients’ knowledge, beliefs, and distress associated with detection and evaluation of incidental pulmonary nodules for cancer: Results from a multicenter survey. J. Thorac. Oncol. 11, 700–708 (2016).
Li, L., Zhao, Y. & Li, H. Assessment of anxiety and depression in patients with incidental pulmonary nodules and analysis of its related impact factors. Thorac. Cancer 11, 1433–1442 (2020).
Tzeng, I. S. To handle the inflation of odds ratios in a retrospective study with a profile penalized log-likelihood approach. J. Clin. Lab. Anal. 35, e23849 (2021).
Acknowledgements
The authors thank all the participants for their time and efforts and for revealing their experiences with frankness during the interviews.
Author information
Authors and Affiliations
Contributions
All authors had a substantial contribution to the manuscript. JY: Conceptualisation, Study design, Data collection, Data analysis, Data interpretation, Writing—original draft, Review and editing, Final approval; FX: Conceptualisation, Study design; MC and HR: Study design, Review and editing; SF: Study design, Review and editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yuan, J., Xu, F., Ren, H. et al. Distress and its influencing factors among Chinese patients with incidental pulmonary nodules: a cross-sectional study. Sci Rep 14, 1189 (2024). https://doi.org/10.1038/s41598-023-45708-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45708-w