Abstract
The purpose of this study was to investigate whether patients with colorectal cancer (CRC) combined with hyperuricemia remitted 1 year after CRC surgery. CRC patients combined with hyperuricemia who underwent radical surgery were included from a single clinical center from Jan 2016 to Dec 2021. Baseline characteristics was compared between the remission group and the non-remission group. Multivariate logistic regression was used to find the possible predictive factors of hyperuricemia remission. A total of 91 patients were included for data analysis, retrospectively. There were 34 (37.4%) patients in the remission group and 57 (62.6%) patients in the non-remission group. The mean preoperative weight and body mass index (BMI) were 61.2 ± 10.7 (kg) and 24.1 ± 3.3 (kg/m2). 21 (23.1%) patients had a history of drinking. We found that the weight and BMI were not significantly different before and 1 year after CRC surgery (P > 0.05). In contrast, uric acid values were significantly decreased (P < 0.01). Meanwhile, the outcomes showed there were no significant differences in the baseline characteristics between the remission and non-remission groups (P > 0.05). According to multivariate logistic regression, we found that the history of drinking was a predictive factor of hyperuricemia remission (OR = 0.046, 95% CI 0.005–0.475, P = 0.010). CRC patients with hyperuricemia had a 37.4% remission from hyperuricemia 1 year after CRC surgery. Tumor ___location, tumor stage, and tumor size did not predict the remission of hyperuricemia. Notably, the history of drinking was a predictive factor of hyperuricemia remission.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the most common cancer of the digestive system and the third most common cancer in the world1,2. Approximately 35,000 new CRC cases are diagnosed each year, accounting for 20% of all cancer diagnoses2,3. CRC is also the second most death-related cancer in the world, with approximately 16,000 cancer-related deaths each year2. At present, surgery is the most effective means of treating CRC4,5.
Uric acid (UA) is the product of purine metabolism in all cells. UA is produced by the oxidation of xanthine and hypoxanthine through xanthine oxidoreductase, which is a necessary reaction to remove nitrogenous waste products from the body6. UA values in normal individuals range from 178 to 400 (μmol/L)7. Hyperuricemia is caused by the abnormal UA metabolism, including the urate overproduction and decreased UA excretion8,9. In recent years, the prevalence of hyperuricemia in developing countries has been rising10,11. Studies have shown that hyperuricemia may be associated with increased predictive of cancer incidence and metastasis and is associated with the risk of cancer death12,13.
Notably, a previous study suggests that patients with concurrent CRC and type 2 diabetes mellitus (T2DM) have a remission 1 year after CRC surgery14. Recent evidence has demonstrated that patients with concurrent CRC and hypertension had a remission rate 1 year after CRC surgery as well3. Hypertension, T2DM, and hyperuricemia are both forms of metabolic syndrome. However, there is no report showing whether patients with concurrent CRC and hyperuricemia have a remission after CRC surgery. Therefore, this study is to investigate whether patients with concurrent CRC and hyperuricemia remitted 1 year after CRC surgery.
Method
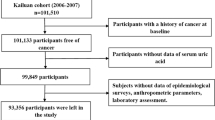
Patients
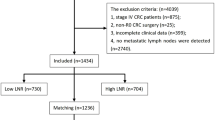
This retrospective study enrolled 91 CRC patients combined with hyperuricemia and underwent surgery from a single clinical center from Jan 2016 to Dec 2021. This study was approved by the Institutional Ethics Committee of the First Affiliated Hospital of Chongqing Medical University (2022-133-2).
Inclusion and exclusion criteria
The CRC patients combined with hyperuricemia who underwent radical surgery were included from a single clinical center (n = 270). The exclusion criteria were as follows: 1, tumor stage IV patients (n = 3); 2, incomplete post-operative information (n = 94); 3, unreachable patients (n = 82). Finally, 91 patients were included for data analysis.
Data collection
We obtained preoperative baseline information and postoperative recovery of the patient through electronic medical records and telephone follow-up. The preoperative information included age, sex, hypertension, T2DM, weight, body mass index (BMI), smoking, drinking, albumin, hemoglobin, tumor ___location, tumor nodes metastasis (TNM) stage, and tumor size. As for postoperative information, weight, BMI, and UA were collected.
Definition
The tumor node metastasis stage was diagnosed according to the AJCC 8th Edition 15. The remission group was defined as a return to normal UA values or a significant decrease in postoperative gout compared to preoperative levels by 1 year after CRC surgery. Weight change was defined as the postoperative weight minus preoperative weight.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD). Categorical variables were expressed as n (%). The Chi-square test was used to analyze categorical variables and the t-test was used to analyze continuous variables between the remission group and the non-remission group. Paired-sample t-test was used to analyze continuous variables before and 1 year after surgery. Statistical analysis was performed by the SPSS (version 22.0) software. P-value of < 0.05 was considered statistically significant.
Ethics approval and informed consent
The study was approved by the ethics committee of our institution (The First Affiliated Hospital of Chongqing Medical University, 2022-133-2), and all patients signed informed consent. This study was conducted in accordance with the World Medical Association Declaration of Helsinki as well.
Results
Patients
A total of 91 patients were included in this study according to the inclusion and exclusion criteria. The age of included patients was 63.7 ± 11.5 years old. There were 31 (34.1%) males and 60 (65.9%) females. The mean preoperative weight and BMI were 61.2 ± 10.7 (kg) and 24.1 ± 3.3 (kg/m2). 24 (26.4%) patients had a history of smoking, and 21 (23.1%) patients had a history of drinking. In addition, more details including hypertension, T2DM, albumin, hemoglobin, tumor ___location, TNM stage, and tumor size were shown in Table 1.
Comparison before and 1 year after CRC surgery
Table 2 showed the changes of weight, BMI, and UA before and 1 year after CRC surgery. As Table 2 suggested, the UA after CRC surgery (522.3 ± 57.8, umol/L) was significantly lower than the UA before CRC surgery (428.1 ± 81.7, umol/L) (P < 0.01). However, there were no significant differences in weight and BMI before and 1 year after CRC surgery (P > 0.05).
Baseline characteristics between the remission and non-remission groups
Patients were divided into the remission group and the non-remission group. There were 34 (37.4%) patients in the remission group and 57 (62.6%) patients in the non-remission group. We compared the baseline characteristics including age, sex, hypertension, T2DM, weight, BMI, smoking, drinking, albumin, hemoglobin, tumor ___location, TNM stage, and tumor size between the remission and non-remission groups. After data analysis, the outcomes showed there were no significant differences in the baseline characteristics between the remission and non-remission groups (P > 0.05). (Table 3).
Multivariate logistic regression of hyperuricemia remission
Multivariate logistic regression was used to find the possible predictive factors of hyperuricemia remission. Pre-operative weight, weight change, drinking, and tumor stage were collected for multivariate logistic regression analysis. After data analysis, we found that the history of drinking was a predictive factor of hyperuricemia remission (OR = 0.272, 95% CI 0.076–0.975, P = 0.046). However, pre-operative weight (OR = 1.030, 95% CI 0.979–1.083, P = 0.251), weight change (OR = 1.016, 95% CI 0.947–1.090, P = 0.661), and tumor stage (OR = 1.629, 95% CI 0.880–3.018, P = 0.121) were not associated with hyperuricemia remission. (Table 4).
Discussion
We enrolled 91 CRC patients with hyperuricemia who underwent surgery for analysis. There were 34 patients in the remission group, and the remission rate was 37.4%. After data analysis, there were no significant differences in the baseline characteristics including age, sex, hypertension, T2DM, weight, BMI, smoking, drinking, albumin, hemoglobin, tumor ___location, TNM stage, and tumor size between the remission and non-remission groups. However, we found that less preoperative drinking was a predictor of remission of postoperative hyperuricemia in the multivariate logistic regression.
UA was the product of nucleotide metabolism and was produced by the liver, muscle, and intestine16. High levels of UA were often observed in patients with metabolic syndrome. Some studies reported that high levels of UA might contribute to the onset and development of metabolic syndrome17,18. Hyperuricemia was partly responsible for insulin resistance, which was a key factor in the metabolic syndrome. Furthermore, Hyperinsulinemia due to insulin resistance could impair the excretory function of the kidneys and led to hyperuricemia19. Thus, there might be a bidirectional causal relationship between hyperuricemia and insulin resistance. Insulin resistance was a cause of T2DM. Both hyperuricemia and T2DM were metabolic syndromes. Metabolic disorders were quite associated with central obesity, insulin resistance, hypertension and hyperlipemia in previous studies20,21,22.
In previous study, Peng et al.14. in a retrospective study of 296 patients with CRC with T2DM found a remission 1 year after surgery. Moreover, they also reported that higher weight loss and shorter duration of T2DM contributed to T2DM remission. Furthermore, Chen et al. 3 found patients with concurrent CRC and hypertension had a remission rate 1 year after CRC surgery as well through analysis of 387 patients. As public known, hypertension, type 2 diabetes and hyperuricemia were all associated with metabolic disorders. Theoretically, hyperuricemia could also be alleviated after CRC surgery. However, there were no studies reported whether CRC patients with hyperuricemia had a remission 1 year after surgery. Therefore, it was necessary to investigate whether hyperuricemia in patients with CRC combined with hyperuricemia remitted 1 year after CRC surgery and potential predictive factors for remission.
In this study, we found a 37.4% remission rate of hyperuricemia one after CRC surgery. Furthermore, patients who drank less could contribute hyperuricemia remission. The mechanisms were not yet clear, but the reasons might be as follows: First, patients’ dietary structure changed after surgery. There were some studies suggesting a correlation existed between the composition of the diet and hyperuricemia23,24,25. Meat and poultry could contribute to elevated UA26. Second, patients reduced alcohol consumption. Alcohol was a recognized group of carcinogens, and its dangers were self-evident. Men who were currently drinking alcohol were at higher risk of developing hyperuricemia, and drinking was a risk factor for hyperuricemia27,28,29. In general, patients would reduce or even refuse to drink after surgery due to increased awareness of the dangers of alcohol. Third, with resection of the primary tumor, correction of endocrine dysregulation, reduction of the pro-inflammatory response or remodeling of the tumor microenvironment might result in a decrease in UA. Forth, previous studies found that remission of hypertension or T2DM might be related to hormones, including renin, angiotensin, aldosterone, ghrelin, glucagon-like peptide (GLP)-1 and GLP-23,14,30,31. This reason might also bring relief from hyperuricemia, which was also a metabolic disease. Uric acid was a dynamic parameter and was influenced by diverse factors, such as age32, sex27, ___location33, smoking34,35, gout, thiaside use, and increased cell cycle situations. There was a lack of knowledge about these factors. The patient might have changed his or her lifestyle after the surgery, resulting in a change in uric acid.
To our knowledge, this was the first study to investigate whether hyperuricemia in patients with CRC combined with hyperuricemia remitted 1 year after CRC surgery and potential predictive factors for remission. The baseline characteristics were not significantly different between the remission group and the non-remission group, which could make our outcomes convincing. However, there were still some limitations. First, the sample size of this study was small. Second, the patients in this study were from a single clinic center, which might cause selected bias. Thus, more research should be conducted in the future.
In conclusion, CRC patients with hyperuricemia had a 37.4% remission from hyperuricemia 1 year after CRC surgery. Tumor ___location, tumor stage, and tumor size did not predict the remission of hyperuricemia. Notably, the history of drinking was a predictive factor of hyperuricemia remission.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Siegel, R. L., Miller, K. D. & Jemal, A. Colorectal cancer mortality rates in adults aged 20–54 years in the United States, 1970–2014. JAMA 318(6), 572–574. https://doi.org/10.1001/jama.2017.7630 (2017).
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68(6), 394–424. https://doi.org/10.3322/caac.21492 (2018).
Cheng, Y. X. et al. Hypertension remission after colorectal cancer surgery: A single-center retrospective study. Nutr. Cancer. 74(8), 2789–2795. https://doi.org/10.1080/01635581.2021.2025256 (2022).
Dru, R. C. et al. Impact of anaemia at discharge following colorectal cancer surgery. Int. J. Colorect. Dis. 35(9), 1769–1776. https://doi.org/10.1007/s00384-020-03611-0 (2020).
Osterman, E. & Glimelius, B. Recurrence risk after up-to-date colon cancer staging, surgery, and pathology: Analysis of the entire swedish population. Dis. Colon Rectum. 61(9), 1016–1025. https://doi.org/10.1097/DCR.0000000000001158 (2018).
Hille, R. Molybdenum-containing hydroxylases. Arch. Biochem. Biophys. 433(1), 107–116. https://doi.org/10.1016/j.abb.2004.08.012 (2005).
Crawley, W. T., Jungels, C. G., Stenmark, K. R. & Fini, M. A. U-shaped association of uric acid to overall-cause mortality and its impact on clinical management of hyperuricemia. Redox Biol. 51, 102271. https://doi.org/10.1016/j.redox.2022.102271 (2022).
Hediger, M. A., Johnson, R. J., Miyazaki, H. & Endou, H. Molecular physiology of urate transport. Physiology (Bethesda) 20, 125–133. https://doi.org/10.1152/physiol.00039.2004 (2005).
El Ridi, R. & Tallima, H. Physiological functions and pathogenic potential of uric acid: A review. J. Adv. Res. 8(5), 487–493. https://doi.org/10.1016/j.jare.2017.03.003 (2017).
Fini, M. A., Elias, A., Johnson, R. J. & Wright, R. M. Contribution of uric acid to cancer risk, recurrence, and mortality. Clin. Transl. Med. 1(1), 16. https://doi.org/10.1186/2001-1326-1-16 (2012).
Huang, J., Ma, Z. F., Tian, Y. & Lee, Y. Y. Epidemiology and prevalence of gout in Mainland China: An updated systematic review and meta-analysis. SN Compr. Clin. Med. 2(9), 1593–1606. https://doi.org/10.1007/s42399-020-00416-8 (2020).
Fini, M. A. et al. Brief report: The uricase mutation in humans increases our risk for cancer growth. Cancer Metab. 9(1), 32. https://doi.org/10.1186/s40170-021-00268-3 (2021).
Strasak AM, Lang S, Kneib T, Brant LJ, Klenk J, Hilbe W, VHM&PP Study Group. Use of penalized splines in extended Cox-type additive hazard regression to flexibly estimate the effect of time-varying serum uric acid on risk of cancer incidence: a prospective, population-based study in 78,850 men. Ann Epidemiol. 19(1), 15–24. https://doi.org/10.1016/j.annepidem.2008.08.009 (2009).
Peng, D., Liu, X. Y., Cheng, Y. X., Tao, W. & Cheng, Y. Improvement of diabetes mellitus after colorectal cancer surgery: A retrospective study of predictive factors for type 2 diabetes mellitus remission and overall survival. Front. Oncol. 6(11), 694997. https://doi.org/10.3389/fonc.2021.694997 (2021).
Peng, D. et al. Onco-metabolic surgery: A combined approach to gastric cancer and hypertension. Cancer Manag. Res. 26(12), 7867–7873. https://doi.org/10.2147/CMAR.S260147 (2020).
Huang, J. et al. Geographical distribution of hyperuricemia in mainland China: a comprehensive systematic review and meta-analysis. Glob. Health Res. Policy 5(1), 52. https://doi.org/10.1186/s41256-020-00178-9 (2020).
Caliceti, C., Calabria, D., Roda, A. & Cicero, A. F. G. Fructose intake, serum uric acid, and cardiometabolic disorders: A critical review. Nutrients. 9(4), 395. https://doi.org/10.3390/nu9040395 (2017).
Sharaf El Din, U. A. A., Salem, M. M. & Abdulazim, D. O. Uric acid in the pathogenesis of metabolic, renal, and cardiovascular diseases: A review. J. Adv. Res. 8(5), 537–548. https://doi.org/10.1016/j.jare.2016.11.004 (2017).
Li, C., Hsieh, M. C. & Chang, S. J. Metabolic syndrome, diabetes, and hyperuricemia. Curr. Opin. Rheumatol. 25(2), 210–216. https://doi.org/10.1097/BOR.0b013e32835d951e (2013).
Tefera, W., Shuremu, M., Tadelle, A., Abdissa, D. & Banjaw, Z. Magnitude of central obesity and associated factors among adults working in government offices in Bedele town, Buno Bedele zone, Southwest Ethiopia. SAGE Open Med. 29(10), 20503121221105990. https://doi.org/10.1177/20503121221105993 (2022).
SavaşErdoğan, S., FalayGür, T., Özkur, E. & Doğan, B. Insulin resistance and metabolic syndrome in patients with seborrheic dermatitis: A case-control study. Metab. Syndr. Relat. Disord. 20(1), 50–56. https://doi.org/10.1089/met.2021.0063 (2022).
Zalewska, E., Kmieć, P. & Sworczak, K. Role of catestatin in the cardiovascular system and metabolic disorders. Front. Cardiovasc. Med. 19(9), 909480. https://doi.org/10.3389/fcvm.2022.909480 (2022).
Feng, Q. et al. Metabolic syndrome-related hyperuricemia is associated with a poorer prognosis in patients with colorectal cancer: A multicenter retrospective study. Cancer Manag. Res. 24(13), 8809–8819. https://doi.org/10.2147/CMAR.S338783 (2021).
Zhang, Q. et al. Diet diversity and nutritional status among adults in southwest China. PLoS One. 12(2), e0172406. https://doi.org/10.1371/journal.pone.0172406 (2017).
Ma, G. Food, eating behavior, and culture in Chinese society. J. Ethn. Foods 2, 195–199 (2015).
Miao, Z. et al. Dietary and lifestyle changes associated with high prevalence of hyperuricemia and gout in the Shandong coastal cities of Eastern China. J. Rheumatol. 35(9), 1859–1864 (2008).
Song, P. et al. Prevalence and correlates of hyperuricemia in the middle-aged and older adults in China. Sci. Rep. 8(1), 4314. https://doi.org/10.1038/s41598-018-22570-9 (2018).
Choi, H. K., Atkinson, K., Karlson, E. W., Willett, W. & Curhan, G. Alcohol intake and risk of incident gout in men: A prospective study. Lancet. 363(9417), 1277–1281. https://doi.org/10.1016/S0140-6736(04)16000-5 (2004).
Choi, H. K. & Curhan, G. Beer, liquor, and wine consumption and serum uric acid level: The third national health and nutrition examination survey. Arthritis. Rheum. 51(6), 1023–1029. https://doi.org/10.1002/art.20821 (2004).
Russel, S. M. et al. Physiologic mechanisms of type II diabetes mellitus remission following bariatric surgery: A meta-analysis and clinical implications. J. Gastrointest. Surg. 24(3), 728–741. https://doi.org/10.1007/s11605-019-04508-2 (2020).
Fenske, W. K. et al. Effect of bariatric surgery-induced weight loss on renal and systemic inflammation and blood pressure: A 12-month prospective study. Surg. Obes. Relat. Dis. 9(4), 559–68. https://doi.org/10.1016/j.soard.2012.03.009 (2013).
Kuo, C. F., Grainge, M. J., Zhang, W. & Doherty, M. Global epidemiology of gout: Prevalence, incidence and risk factors. Nat. Rev. Rheumatol. 11(11), 649–662. https://doi.org/10.1038/nrrheum.2015.91 (2015).
Song, F. & Cho, M. S. Geography of food consumption patterns between South and North China. Foods 6(5), 34. https://doi.org/10.3390/foods6050034 (2017).
Haj Mouhamed, D. et al. Effect of cigarette smoking on plasma uric acid concentrations. Environ. Health Prev. Med. 16(5), 307–312. https://doi.org/10.1007/s12199-010-0198-2 (2011).
Wang, W. & Krishnan, E. Cigarette smoking is associated with a reduction in the risk of incident gout: Results from the Framingham heart study original cohort. Rheumatology (Oxford) 54(1), 91–95. https://doi.org/10.1093/rheumatology/keu304 (2015).
Acknowledgements
The authors are grateful to all the colleagues who helped in the preparation of this article. Especially, Yin Huang and Meng-Hua Zeng made a huge contribution to the manuscript revision. Xun Lei helped us in our knowledge of statistics.
Funding
Chongqing medical scientific research project (Joint project of Chongqing Health Commission and Science and Technology Bureau) (2023QNXM020).
Author information
Authors and Affiliations
Contributions
All authors contributed to data collection. F.L. wrote the first manuscript. Y.H. prepared the figures. Z.W.L., X.R.L., X.Y.L., Q.L., X.P.S., L.S.L., Y.T., and W.Z. performed the data collection. M.H.Z. and D.P. analyzed the data and reviewed the manuscript. All the authors have agreed on the manuscript that will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, F., Huang, Y., Li, ZW. et al. Hyperuricemia remission after colorectal cancer surgery for colorectal cancer patients. Sci Rep 13, 18867 (2023). https://doi.org/10.1038/s41598-023-46348-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-46348-w