Abstract
Peritoneal washing cytology (CY) in patients with pancreatic cancer is mainly used for staging; however, it may also be used to evaluate the intraperitoneal status to predict a more accurate prognosis. Here, we investigated the potential of deep learning of CY specimen images for predicting the 1-year prognosis of pancreatic cancer in CY-positive patients. CY specimens from 88 patients with prognostic information were retrospectively analyzed. CY specimens scanned by the whole slide imaging device were segmented and subjected to deep learning with a Vision Transformer (ViT) and a Convolutional Neural Network (CNN). The results indicated that ViT and CNN predicted the 1-year prognosis from scanned images with accuracies of 0.8056 and 0.8009 in the area under the curve of the receiver operating characteristic curves, respectively. Patients predicted to survive 1 year or more by ViT showed significantly longer survivals by Kaplan–Meier analyses. The cell nuclei found to have a negative prognostic impact by ViT appeared to be neutrophils. Our results indicate that AI-mediated analysis of CY specimens can successfully predict the 1-year prognosis of patients with pancreatic cancer positive for CY. Intraperitoneal neutrophils may be a novel prognostic marker and therapeutic target for CY-positive patients with pancreatic cancer.
Similar content being viewed by others
Introduction
Pancreatic cancer is now the third leading cause of cancer-related death in the United States and fourth in Japan1,2, and its incidence is increasing; therefore, it is predicted to be the second leading cause of cancer-related death in the United States by 20303. Pancreatic cancer has a poor prognosis, with a 5-year survival rate of < 10% despite multidisciplinary treatment combining surgery, chemotherapy, and radiotherapy4. As patients with pancreatic cancer have a variety of conditions, predicting their prognosis will be helpful in suggesting an appropriate treatment plan.
Peritoneal washing cytology (CY) is useful for assessing pancreatic cancer progression. Positive peritoneal washing cytology (CY+) is classified as distant metastasis by the American Joint Committee on Cancer and the National Comprehensive Cancer Network5,6. CY+ patients have a poorer prognosis than CY− patients7. Even in patients diagnosed with resectable pancreatic cancer, based on imaging studies, 30% of them were CY+ 8. Thus, CY is becoming increasingly important for pancreatic cancer, and the number of CY performed is expected to increase further in the future. Moreover, peritoneal lavage fluid contains a variety of cells, including peritoneal mesothelial cells, lymphocytes, neutrophils, and macrophages9. CY allows the observation of cells in the peritoneal cavity and may provide useful clinical information in addition to evaluating cancer progression.
Recently, remarkable advances have been made in artificial intelligence (AI), particularly in medical imaging studies using machine learning. In cytopathology, deep learning techniques can help assess malignant cells in fine-needle aspiration specimens of the mammary glands and pancreas with high accuracy10,11. Furthermore, AI discriminates whether the primary tumor of urothelial carcinoma is invasive or non-invasive from a urine cytology specimen12, suggesting that AI-mediated analysis of cytology specimens may provide additional information beyond the conventional diagnosis of malignancy made by pathologists. This study aimed to examine whether AI can predict a more accurate prognosis from positive CY specimens in patients with pancreatic cancer. Hence, we investigated the potential of deep learning of images of CY specimens for predicting the 1-year prognosis of CY+ patients with pancreatic cancer.
Results
Patient characteristics
The study profile is shown in Fig. 1. This study included 126 patients with pancreatic cancer who were diagnosed as CY+ for the first time during their disease course at Tohoku University Hospital between January 2011 and December 2022. Of these, 38 patients were excluded, including 2 who died from other diseases, 26 for whom the prognosis within 1 year after CY collection was unknown, and 10 for whom the cytology specimens were lost. Ultimately, 88 CY+ patients were included in the analysis and classified into poor (survival < 1 year; n = 28) and good (survival ≥ 1 year; n = 60). Table 1 shows the patient characteristics. There were no significant differences in age, sex, liver metastases, carbohydrate antigen 19-9 (CA19-9) levels, or white blood cell (WBC) counts between the poor and good prognostic groups; only C-reactive protein (CRP) levels were significantly different between the groups (p < 0.05).
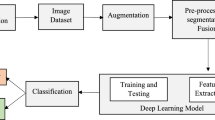
Classification using deep neural network
The patients were divided into a training dataset cohort (n = 56) with CY sampling conducted between 2011 and 2018, a test dataset cohort (n = 24) with CY sampling conducted between 2019 and 2021, and a validation dataset cohort (n = 8) with CY sampling conducted during 2022. Papanicolaou-stained CY specimens scanned at 40× magnification by the whole slide imaging device were segmented and subjected to deep learning with a Vision Transformer (ViT) and a Convolutional Neural Network (CNN). After deep learning using the training data, the test cohort of 24 patients was analyzed to evaluate whether they belonged to the poor or good prognosis groups. The total numbers of cell nuclei used for the analysis were 59,182 in the training data and 17,084 in the test data. Receiver operating characteristic (ROC) curves were created to determine the predictive ability of the binary classification of the systems. The areas under the curve (AUCs) for ViT and CNN using the test data were 0.8056 and 0.8009, respectively (Fig. 2 and Supplementary Fig. S1). Furthermore, the AUC for ViT using the validation data was 0.8333. A Kaplan–Meier survival analysis of patients with these binary predictions by ViT showed that the good prognosis group had significantly longer survival than did the poor prognosis group (p < 0.0001; Fig. 3). There was no significant difference in the Kaplan–Meier survival curves between patients prognostically classified using CNN (Supplementary Fig. S2).
Extraction of the top 5 cell nucleus images with high impact on poor or good prognosis
We extracted the top 5 cell nuclear images with high or low predicted probabilities for ViT (Fig. 4). Cell nuclei with high predicted probabilities, indicating a high likelihood of poor prognosis, showed segmented nuclei that were likely to be those of neutrophils. In contrast, cell nuclei with low predicted probabilities, indicating a high likelihood of a good prognosis, showed round nuclei and were morphologically considered peritoneal mesothelial cells or macrophages.
Top 5 cell nuclear images with high impact on poor or good prognosis. The cell nuclear images are listed from left to right, starting with the image with the highest predicted probabilities or the one with the lowest predicted probabilities. (A) Cell nuclei images associated with the poor prognosis. (B) Cell nuclei images associated with the good prognosis.
Immunocytochemistry of cells associated with good prognostic evaluation in ViT
We performed immunohistochemistry to evaluate cells with good prognosis by examining the expression of calretinin, a specific marker for peritoneal mesothelial cells. The results showed that the cells were negative compared to peritoneal mesothelial cells used as internal controls, indicating that the good prognostic cells were macrophages (Fig. 5A–C).
Results of immunocytochemistry. (A) Papanicolaou staining image of an analyzed sample. The red frame indicates a cell with low predicted probabilities of ViT (Original magnification, ×400). (B) Immunocytochemistry for calretinin. The cell was negative for calretinin expression (Red frame. Original magnification, ×400). (C) Internal control for the calretinin immunocytochemistry. Mesothelial cells were positive for calretinin staining (Original magnification, ×400). ViT, vision transformer.
Discussion
This is the first study to examine whether prognosis can be predicted using AI-mediated analysis of CY specimens from patients with pancreatic cancer. In this study, deep learning using ViT and CNN was able to predict the 1-year prognosis from CY+ specimens of patients with pancreatic cancer, with an accuracy of more than AUC 0.8. In addition, the prediction accuracy was higher for the ViT than for the CNN. Segmented nuclei were found among the cell nuclei with high predicted probabilities of ViT, suggesting a poor prognosis. These cells were most likely neutrophils. The round cell nuclei had low predicted probabilities, suggesting a good prognosis, which were macrophages based on negative immunocytochemical staining for calretinin.
AI techniques are being used in a variety of fields, and in pathology they are being applied to diagnose benign and malignant conditions and tumor subtypes, evaluate pathological features and biomarkers, and predict prognosis13. In the cytological field, a deep learning system was able to classify malignant cells and predict tumor origins from cytology images of pleural and ascitic fluids, achieving an AUC of 0.95 and better14. Previous studies on prognosis prediction by deep learning using histopathology specimens have reported that survival prediction was successful for gastric cancer, liver cancer, and glioma with C-indexes of 0.657, 0.78, and 0.754, respectively, and for soft-tissue sarcoma with AUC accuracy of 0.9115,16,17,18. For pancreatic cancer, which was the subject of this study, CT images were used to predict prognosis with an accuracy of AUC 0.72319. All of these previous studies used CNN-based machine learning. The accuracy of survival prediction in this study was demonstrated in 0.8 of AUC, which seems to be sufficiently high. Furthermore, our team has also shown that combining clinical information with machine learning of histopathology specimen images improves prediction accuracy of patients with pancreatic cancer undergoing surgery and adjuvant therapy20. Training AI by integrating clinical and molecular data, such as genomic and RNA sequencing information, with imaging information, such as that obtained in this study, could provide a more accurate assessment of therapeutic options. Recently, attention mechanisms have gained prominence in deep learning. A model consisting solely of an attention mechanism was first developed in the field of machine translation21. Subsequently, ViT classified images with higher accuracy than CNN which has been widely used for prognosis prediction based on image data22. In this study, the AUC for predicting 1-year prognosis was only slightly higher for ViT than for CNN. A Kaplan–Meier survival analysis of patients using ViT predictions in this study showed that the good prognosis group had significantly longer survival than the poor prognosis group. However, there was no significant difference in survival curves between the groups classified by CNN. We used data for cell nuclei, which allowed us to over 50,000 image data for training. The large amount of data may enable ViT to efficiently learn the cell nuclei that are more likely to influence on prognosis, and thereby improving classification accuracy23. In addition, although segmentation was performed for each cell, morphological annotation of each cell was not performed during the training phase. We previously reported a deep learning system without morphological annotation for histopathological specimens24. These approaches not only save the physician time regarding the need for annotation but also have the potential to uncover new findings.
The cell nuclei in the poor prognosis group were most likely those of neutrophils. An elevated neutrophil-to-lymphocyte ratio in the peripheral blood and an increased number of intratumoral neutrophils have been reported as poor prognostic factors in patients with pancreatic cancer25,26, and meta-analyses of multiple cancer types have shown similar findings27,28. The present results suggest that intraperitoneal neutrophils are a poor prognostic factor in patients with pancreatic cancer. To the best of our knowledge, there have been no reports examining the relationship between intraperitoneal neutrophils and prognosis in patients with cancer. Findings of intraperitoneal neutrophils have been reported in mouse models. Intraperitoneal neutrophils increased in a mouse model of peritoneal dissemination of ovarian cancer29 and intraperitoneal neutrophil extracellular traps (NETs) promoted intraperitoneal dissemination in mice transplanted with human gastric cancer cells30. In recent years, the relationship between tumor cells and immune cells has attracted much attention, and various findings have been reported for neutrophils. Neutrophils have been shown to promote tumor cell proliferation. Elastase produced by neutrophils degrades insulin receptor substrate-1 when taken up by tumor cells, resulting in enhanced interaction between phosphatidylinositol 3-kinase (PI3K) and platelet-derived growth factor receptor. The subsequent activation of the PI3K pathway promotes tumor growth31. In addition, neutrophils also promote tumor metastasis. Previous studies have shown that NETs formed by neutrophils capture circulating tumor cells and provide a foothold for metastasis32, and that the interaction of β2 integrin on neutrophils with intercellular adhesion molecule 1 on tumor cells promotes tumor cell anchorage to the vascular endothelium and invasion into the tissue33. Moreover, neutrophils are an important source of matrix metallopeptidase 9, which releases vascular endothelial growth factor from the extracellular matrix and is thought to promote angiogenesis by malignant tumors34,35. Further to the above, neutrophils have been shown to induce apoptosis of CD8 T cells in the presence of tumor necrosis factor α and nitric oxide, which may favor tumor cells by suppressing cellular immunity36. In contrast, neutrophils exert antitumor effects by causing tumor cell death37, inhibiting neovascularization38, and promoting T cell proliferation39. Thus, neutrophils have a dual function with respect to tumor cells, and factors affecting their functional polarization have been investigated40. In our study results, intraperitoneal neutrophils were associated with poor prognosis. Intraperitoneal neutrophils in pancreatic cancer patients with CY+ may exert a variety of functions that promote the tumorigenic effects described above, thereby worsening their prognosis. Regarding patient characteristics, the only significant difference between the good and poor prognostic groups was CRP level, indicating that a high CRP level was associated with poor prognosis. CRP is a systemic inflammatory marker; therefore, this result may indicate an association between systemic inflammation and patient prognosis. However, the difference in mean CRP levels between the 2 groups was small, and a prospective study is needed to clarify whether this difference is clinically significant. Furthermore, the relationship between intraperitoneal neutrophils and systemic inflammation was obscure in this study, although some cases revealed the presence of intraperitoneal neutrophils even in the absence of significant inflammation proved by hematological examination.
These intraperitoneal neutrophils could be therapeutic targets and are currently under investigation. The removal of intraperitoneal neutrophils in a mouse model of peritoneal dissemination of ovarian cancer caused an increase in regulatory T cells and a decrease in CD8+ T cells, suggesting that they may promote tumor growth41. In contrast, it has been reported that type 1 interferon induces the antitumor function of neutrophils and that neutrophil elastase selectively kills cancer cells42,43. These reports suggest that enhancing the antitumor effects of neutrophils by modulating their functions with inflammatory cytokines, rather than eliminating them, could be a therapeutic strategy.
Cells with low predicted probabilities of ViT were determined to be macrophages, which are broadly classified as M1 macrophages with inflammatory effects or M2 macrophages with anti-inflammatory effects; however, the polarization state of macrophages is plastic, and their activation state is composed of a spectrum44. The macrophages identified in this study may have M1-like polarity, which may contribute to an improved prognosis. The interaction between tumor and immune cells has been studied mainly in tumor tissues, but much remains unknown regarding the immune environment in the peritoneal cavity. Further clarification of these issues may lead to a better understanding of the mechanisms underlying the intraperitoneal invasion and peritoneal dissemination of cancer cells, which would help control these processes.
The limitations of this study include its retrospective design, small number of cases, heterogeneous patient background, single-center design and chronological differences in analyzed cohorts. The results should be validated in future studies involving a large number of patients. Chronological differences in obtaining the CY specimens in training dataset cohort (2011–2018), test dataset cohort (2019–2021), and validation dataset cohort (2022) may cause unexpected biases in qualities of materials and trivial differences in clinical treatment and medications. Revalidation of the results of our study using contemporaneous CY specimens may be desirable. Furthermore, future stratification of patients according to treatment methods and other factors may enable the use of CY specimens to predict treatment efficacy.
Using deep learning, we were able to predict the 1-year prognosis of patients with pancreatic cancer from CY+ specimens. Our results may help to optimize the treatment of pancreatic cancer patients with CY+ by stratifying their prognosis. Neutrophil exudation into the peritoneal cavity may promote tumor progression and influence prognosis. Thus, intraperitoneal neutrophils may be a new therapeutic target in patients with CY+ pancreatic cancer. Peritoneal washing fluid is a clinical specimen of interest not only for determining the stage of cancer but also for obtaining new clinical information, which may lead to the development of new treatment methods.
Materials and methods
Study population
This study included 126 patients with pancreatic cancer and who were found to be CY+ for the first time in their disease course at Tohoku University Hospital between January 2011 and December 2022. As depicted in Fig. 1, excluded patients comprised 2 who died from other diseases, 26 who had an unknown prognosis within 1 year after CY collection, and 10 for whom the cytology specimens were lost. Finally, 88 patients were enrolled in this study. These cases were binarily classified into a good prognostic group consisting of patients with survival ≥ 1 year and a poor prognostic group consisting of patients with survival < 1 year based on the CY collection. Alternatively, these cases were divided into a training dataset cohort consisting of 56 cases, including 20 cases from the poor prognostic group subjected to CY collection before January 2019, and a test dataset cohort consisting of 24 cases, including 6 cases from the poor prognostic group subjected to CY collection between December 2018 and April 2021, and a validation dataset cohort consisting of 8 cases, including 2 cases from the poor prognostic group subjected to CY collection between January 2022 and December 2022. This study was approved by the Ethics Committee of Tohoku University Graduate School of Medicine (reference 2021-1-499, 2024-1-124) and RIKEN (Wako 2022-07 (2)). Informed consent to use clinically obtained specimens for non-specified research purposes was obtained from all patients when the peritoneal washing fluid was collected. The Ethics Committee of Tohoku University Graduate School of Medicine gave exemption for the requirement of informed consent from the participants for this specific study; participants were granted the opportunity to decline study participation in an opt-out manner. All methods were performed in accordance with the relevant guidelines and regulations.
Preparation of pathology images
Peritoneal washing fluid was initially collected during surgery. Saline solution (100 mL) was injected into the peritoneal cavity via laparotomy or laparoscopy. The peritoneal washing fluid (50 mL) was collected using a Nelaton catheter and centrifuged. Cytosmears were prepared by the auto-smear method using a Cyto-Tek® 2500 Cytocentrifuge (Sakura Finetek Japan Co. Ltd., Tokyo, Japan). Cytosomes were fixed with 95% ethanol and stained using the Papanicolaou staining method. One of the stained slides from each case was scanned using a whole-slide imaging scanner (NanoZoomer S60 Digital Slide Scanner, Hamamatsu Photonics K. K., Hamamatsu, Japan) at 40× magnification.
Segmentation of cell nuclei
Cells observed in the cytology specimens formed overlapping clusters. Therefore, to improve the recognition accuracy of individual cells, segmentation of cell nuclei and other regions was performed using Ilastik (Version 1.3.3)45 on 10 randomly selected images (230 × 230 µm per image) from a single image at 40× magnification, except for the picture frame-shaped areas of each 1/4 width of the scanning area.
Classification using a deep neural network
ViT22 and CNN were used to predict the prognosis from the imaging data. ViT is a model composed of an attention mechanism without the use of CNN. In this study, we used as input data the cell nucleus images created through segmentation, divided into patches of 16 × 16 pixels each, and used ViT-L_16_imagenet21k+imagenet2012.npz as the transition learning model. We used a simple CNN model for which the structure is shown in Supplementary Fig. S3. A learning model was constructed using the cell nuclear data extracted by segmentation and the prognostic information of the training data. Predictions of poor prognosis were made from individual cell nuclear data from the test dataset cohort. A cell nucleus with the predicted probability of 0.5 or higher was defined as a poor prognostic nucleus. If the percentage of nuclei evaluated as poor prognostic to the total number of cell nuclei extracted from 10 magnified images exceeded a threshold value, the specimen was judged to have a poor prognosis. ROC and Kaplan–Meier curves were generated to evaluate prediction accuracy. To construct the Kaplan–Meier curves, we used the prognostic results with the threshold set to maximize the sum of sensitivity and specificity (0.155). Moreover, we identified 5 cell nuclei, each with a high probability of predicting poor and good prognosis based on the predicted probability of ViT. Cells were examined morphologically by pathologists and cytologists. Poor prognostic cells were determined to be neutrophils with characteristic segmental nuclei, whereas good prognostic cells could not be identified morphologically. Therefore, immunocytochemical staining was performed to identify the characteristics of good prognostic cells.
Immunocytochemistry of peritoneal washing lavage
We performed immunocytochemical staining to identify the cell types of the 5 cell nuclei that were determined to be good prognostic factors based on the ViT results. Regions containing the 5 cell nuclei were transferred using the cell transfer method46 to new glass slides and stained automatically using BenchMark ULTRA PLUS (Roche, Basel, Switzerland). Antigen activation with CC1 buffer (#951-124) was performed for 8 min, and mesothel-specific calretinin expression was detected using an anti-calretinin antibody (#790-4467) and a VENTANA OptiView DAB Universal Kit (# 760-700).
Statistical analysis
Patient characteristics of the good and poor prognostic groups were compared using the Wilcoxon rank-sum test for continuous values and Fisher’s exact test for discontinuous values. ROC curves were plotted using the R package (pROC, version 4.0.1). Kaplan–Meier curves were compared using the log-rank test. Significant P values were established as < 0.05. We used JMP Pro software version 16.0.0 (SAS Institute Inc., Cary, NC, USA) for statistical analyses.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 70, 7–30 (2020).
Center for Cancer Control and Information Services. Cancer statistics graph database (2022, accessed 10 Nov 2022). http://ganjoho.jp/reg_stat/statistics/dl/index.html.
Rahib, L. et al. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 74, 2913–2921 (2014).
Ilic, M. & Ilic, I. Epidemiology of pancreatic cancer. World J. Gastroenterol. 22, 9694–9705 (2016).
Brierley, J. D., Gospodarowicz, M. K. & Wittekind, C. TNM Classification of Malignant Tumours 8th edn. (Wiley, Uk, 2017).
Tempero, M. A. et al. Pancreatic adenocarcinoma, Version 2.2017, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 15, 1028–1061 (2017).
Tsuchida, H. et al. Prognostic importance of peritoneal washing cytology in patients with otherwise resectable pancreatic ductal adenocarcinoma who underwent pancreatectomy: A nationwide, cancer registry-based study from the Japan Pancreas Society. Surgery 166, 997–1003 (2019).
Warshaw, A. L. Implications of peritoneal cytology for staging of early pancreatic cancer. Am. J. Surg. 161, 26–30 (1991).
Kubicka, U. et al. Normal human immune peritoneal cells: Subpopulations and functional characteristics. Scand. J. Immunol. 44, 157–163 (1996).
Subbaiah, R. M., Dey, P. & Nijhawan, R. Artificial neural network in breast lesions from fine-needle aspiration cytology smear. Diagn. Cytopathol. 42, 218–224 (2014).
Momeni-Boroujeni, A., Yousefi, E. & Somma, J. Computer-assisted cytologic diagnosis in pancreatic FNA: An application of neural networks to image analysis. Cancer Cytopathol. 125, 926–933 (2017).
Nojima, S. et al. A deep learning system to diagnose the malignant potential of urothelial carcinoma cells in cytology specimens. Cancer Cytopathol. 129, 984–995 (2021).
Jiang, Y., Yang, M., Wang, S., Li, X. & Sun, Y. Emerging role of deep learning-based artificial intelligence in tumor pathology. Cancer Commun. 40, 154–166. https://doi.org/10.1002/cac2.12012 (2020).
Tian, F. et al. Prediction of tumor origin in cancers of unknown primary origin with cytology-based deep learning. Nat. Med. 30, 1309–1319. https://doi.org/10.1038/s41591-024-02915-w (2024).
Huang, B. et al. Accurate diagnosis and prognosis prediction of gastric cancer using deep learning on digital pathological images: A retrospective multicentre study. EBioMedicine 73, 103631. https://doi.org/10.1016/j.ebiom.2021.103631 (2021).
Saillard, C. et al. Predicting survival after hepatocellular carcinoma resection using deep learning on histological slides. Hepatology 72, 2000–2013. https://doi.org/10.1002/hep.31207 (2020).
Mobadersany, P. et al. Predicting cancer outcomes from histology and genomics using convolutional networks. Proc. Natl. Acad. Sci. U. S. A. 115, E2970–E2979. https://doi.org/10.1073/pnas.1717139115 (2018).
Foersch, S. et al. Deep learning for diagnosis and survival prediction in soft tissue sarcoma. Ann. Oncol. 32, 1178–1187 (2021).
Yao, J. et al. Deep learning for fully automated prediction of overall survival in patients undergoing resection for pancreatic cancer: A retrospective multicenter study. Ann. Surg. 278, e68–e79. https://doi.org/10.1097/SLA.0000000000005465 (2023).
Yamaguchi, R. et al. Machine learning of histopathological images predicts recurrences of resected pancreatic ductal adenocarcinoma with adjuvant treatment. Pancreas 53, e199–e204. https://doi.org/10.1097/MPA.0000000000002289 (2024).
Vaswani, A. et al. Attention is all you need. arXiv. https://doi.org/10.48550/arXiv.1706.03762 (2017).
Dosovitskiy, A. et al. An image is worth 16x16 words: Transformers for image recognition at scale. arXiv. https://doi.org/10.48550/arXiv.2010.11929 (2020).
Raghu, M., Unterthiner, T., Kornblith, S., Zhang, C. & Dosovitskiy, A. Do vision transformers see like convolutional neural networks? arXiv. https://doi.org/10.48550/arXiv.2108.08810v2 (2022).
Yamamoto, Y. et al. Automated acquisition of explainable knowledge from unannotated histopathology images. Nat Commun. 10, 5642 (2019).
Sierzega, M. et al. Preoperative neutrophil-lymphocyte and lymphocyte-monocyte ratios reflect immune cell population rearrangement in resectable pancreatic cancer. Ann. Surg. Oncol. 24, 808–815 (2017).
Chen, X. et al. Intratumoral neutrophil extracellular traps are associated with unfavorable clinical outcomes and immunogenic context in pancreatic ductal adenocarcinoma. Front. Immunol. 13, 1027459. https://doi.org/10.3389/fimmu.2022.1027459 (2022).
Templeton, A. J. et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: A systematic review and meta-analysis. J. Natl. Cancer Inst. 106, dju124. https://doi.org/10.1093/jnci/dju124 (2014).
Shen, M. et al. Tumor-associated neutrophils as a new prognostic factor in cancer: A systematic review and meta-analysis. PLoS One. 9, e98259. https://doi.org/10.1371/journal.pone.0098259 (2014).
Yoshida, M. et al. Modification of the tumor microenvironment in KRAS or c-MYC-induced ovarian cancer-associated peritonitis. PLoS One. 11, e0160330. https://doi.org/10.1371/journal.pone.0160330 (2016).
Kanamaru, R. et al. Low density neutrophils (LDN) in postoperative abdominal cavity assist the peritoneal recurrence through the production of neutrophil extracellular traps (NETs). Sci. Rep. 8, 632 (2018).
Houghton, A. M. et al. Neutrophil elastase-mediated degradation of IRS-1 accelerates lung tumor growth. Nat. Med. 16, 219–223 (2010).
Cools-Lartigue, J. et al. Neutrophil extracellular traps sequester circulating tumor cells and promote metastasis. J. Clin. Invest. 123, 3446–3458 (2013).
Huh, S. J. et al. Transiently entrapped circulating tumor cells interact with neutrophils to facilitate lung metastasis development. Cancer Res. 70, 6071–6082 (2010).
Deryugina, E. I. et al. Tissue-infiltrating neutrophils constitute the major in vivo source of angiogenesis-inducing MMP-9 in the tumor microenvironment. Neoplasia 16, 771–788 (2014).
Nozawa, H., Chiu, C. & Hanahan, D. Infiltrating neutrophils mediate the initial angiogenic switch in a mouse model of multistage carcinogenesis. Proc. Natl. Acad. Sci. U. S. A. 103, 12493–12498 (2006).
Michaeli, J. et al. Tumor-associated neutrophils induce apoptosis of non-activated CD8 T-cells in a TNFα and NO-dependent mechanism, promoting a tumor-supportive environment. Oncoimmunology 6, e1356965. https://doi.org/10.1080/2162402X.2017.1356965 (2017).
Dallegri, F. et al. Tumor cell lysis by activated human neutrophils: Analysis of neutrophil-delivered oxidative attack and role of leukocyte function-associated antigen 1. Inflammation 15, 15–30 (1991).
Loffredo, S. et al. Group V secreted phospholipase A2 induces the release of proangiogenic and antiangiogenic factors by human neutrophils. Front. Immunol. 8, 443 (2017).
Eruslanov, E. B. et al. Tumor-associated neutrophils stimulate T cell responses in early-stage human lung cancer. J. Clin. Invest. 124, 5466–5480 (2014).
Grecian, R., Whyte, M. K. B. & Walmsley, S. R. The role of neutrophils in cancer. Br. Med. Bull. 128, 5–14 (2018).
Yoshida, M. et al. Intraperitoneal neutrophils activated by KRAS-induced ovarian cancer exert antitumor effects by modulating adaptive immunity. Int. J. Oncol. 53, 1580–1590 (2018).
Andzinski, L. et al. Type I IFNs induce anti-tumor polarization of tumor associated neutrophils in mice and human. Int. J. Cancer 138, 1982–1993 (2016).
Cui, C. et al. Neutrophil elastase selectively kills cancer cells and attenuates tumorigenesis. Cell 184, 3163-3177.e21 (2021).
Boutilier, A. J. & Elsawa, S. F. Macrophage polarization states in the tumor microenvironment. Int. J. Mol. Sci. 22, 6995 (2021).
Berg, S. et al. ilastik: Interactive machine learning for (bio)image analysis. Nat. Methods 16, 1226–1232 (2019).
Gong, Y., Joseph, T. & Sneige, N. Validation of commonly used immunostains on cell-transferred cytologic specimens. Cancer 105, 158–164 (2005).
Acknowledgements
The authors thank to Professor Takashi Suzuki, Department of Anatomic Pathology, Tohoku University Graduate School of Medicine, Sendai, Japan, and Dr. Fumiyoshi Fujishima, Department of Pathology, Tohoku University Hospital, Sendai, Japan, for their supervising of this study.
Funding
This study was partly supported by JST Moonshot R&D (Grant Number JPMJMS2022).
Author information
Authors and Affiliations
Contributions
A.N., R.Y., T.F., and Y.Y. designed the study. A.N. wrote the manuscript and performed cell nucleus segmentation and data analysis. Y.N. implemented the deep learning algorism and generated the resulting figures related to AI. T.S. performed immunostaining of the cytologic specimen. H.M. provided expert knowledge on immunostaining and cytology. T.S., H.M., K.K., and Y.A. performed peritoneal washing cytology specimen preparation and obtained clinical data. M.I., T.K., D.D., T.M., K.A., S.N., S.M., H.O., M.M., K.N., J.A., I.M., M.U., Y.Y, and T.F. supervised the study. Y.N., H.M., and Y.Y provided expert knowledge on deep learning. Y.Y. and T.F. edited and finalized the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Noguchi, A., Numata, Y., Sugawara, T. et al. Deep learning predicts the 1-year prognosis of pancreatic cancer patients using positive peritoneal washing cytology. Sci Rep 14, 17059 (2024). https://doi.org/10.1038/s41598-024-67757-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67757-5