Abstract
To explore the advantages and disadvantages of 3D Slicer reconstruction and 3D printing localization combined with transcranial neuroendoscope in the surgical treatment of deep cerebral micro cavernous hemangiomas. Method The clinical data of patients with deep cerebral micro cavernous hemangiomas treated by our hospital from June 2022 to February 2023 using 3D Slicer reconstruction and 3D printing localization technology combined with transcranial endoscopic surgery were retrospectively analyzed. A total of 5 cases with complete data were collected, including 2 males and 3 females, aged 9–59 years. All 5 patients had deep supratentorial cavernous hemangiomas with a diameter of less than 1.5 cm, and had clinical symptoms such as headache or epilepsy, and had been diagnosed by CT or MRI. Repeated bleeding from small cavernous hemangiomas in the deep brain can lead to clinical symptoms such as recurrent headache and epilepsy, and is required surgical treatment. However, cavernous hemangiomas often have smaller lesions and are difficult to locate in the deep part. Without neuronavigation, surgery can become extremely difficult. Our team’s newly developed 3D Slicer reconstruction and 3D printing localization technology which could provide new options for surgical treatment of small cavernous hemangiomas or other small lesions in the deep brain, but its accuracy and safety still need to be verified by further clinical research.
Similar content being viewed by others
Introduction
Cerebral cavernous hemangioma (CCH) is a benign intracranial vascular malformation, usually asymptomatic or characterized by seizures as the first clinical manifestation. Its pathological characteristics are composed of a “mulberry like” dilated thin-walled capillary mass surrounded by deposits of hemosiderin1. The incidence rate in the general population is 0.4–0.8%, accounting for 5–15% of all central nervous system vascular malformations, of which about 70–80% cases are located on the supratentorial2,3. According to the literature1, about 15% of symptomatic cases had experienced headache, 5–10% of cases had experienced experience epilepsy, and 1–2% of cases had experienced experience cerebral hemorrhage. However, cerebral angiography is often difficult to detect cavernous hemangiomas, also known as “occult vascular malformations”. Most asymptomatic CCH can be treated conservatively, while symptomatic cavernous hemangiomas are usually recommended for complete surgical resection, because headache, epilepsy, etc. are often associated with recurrent bleeding. In recent years, the development of medical imaging technology combined with virtual reality and 3D printing technology4,5 has greatly promoted the development of surgeons’ surgical planning and preoperative precise positioning technology, improving surgical efficiency, reducing surgical risks, and reducing the incidence of surgical side injuries and various diseases. This retrospective clinical study is based on the combination of 3D Slicer reconstruction technology and 3D printing precise positioning system. During the operation, the advantages of neuroendoscope such as good illumination, flexible degrees of freedom, and close observation5 are utilized to assist in the minimally invasive surgical treatment of deep intracerebral micro cavernous hemangiomas, achieving good results.
Materials and methods
General information
This retrospective clinical study collected the clinical data of patients with deep cerebral micro cavernous hemangiomas treated by our hospital from June 2022 to February 2023 using 3D Slicer reconstruction and 3D printing localization technology combined with transcranial endoscopic surgery. A total of 5 cases with complete data were collected, including 2 males and 3 females, aged 9–59 years. All 5 patients had deep supratentorial cavernous hemangiomas with a diameter of less than 1.5 cm, and had clinical symptoms such as headache or epilepsy. The diagnosis was confirmed by CT or MRI. One month after discharge, all patients had no neurological symptoms during outpatient or telephone follow-up. The detailed clinical information is showed in Table 1.
3D Slicer reconstruction of lesion model and design of localization system
Preoperative acquisition of thin slice CT or CTA raw data of the patient’s brain in the format of DICOM, import the above data into the 3D-Slicer system (https://www.slicer.org) , reconstruct the lesion and scalp, and create a 3D virtual reality model and a 3D printing positioning guide plate model. The 3D virtual reality model helps us understand the ___location of the lesion within the brain and the structural relationship between the surrounding areas. The 3D printing positioning guide can assist in determining the ___location of the lesion’s body surface and assist in preoperative positioning. Based on our previous clinical experience, the guide plate we designed is centered on the lesion and made a vertical line to the surface of the brain tissue to determine the projection position of the lesion on the scalp’s surface. The surgery uses a minimally invasive skin incision and keyhole bone window approach, so we do not need a full head haircut. The following points need to be noted when using a 3D positioning guide: (1) The design of the guide needs to be 1-3 mm larger than the actual reconstructed scalp (because it is attached to the outside of the scalp during use), and it must include the contours of both eyebrow arches and one outer ear (3 points to determine the plane). (2) The positioning point is generally designed as a vertical point from the deep lesion to the surface of the brain tissue. (3) When using, it is also necessary to pay attention to tightly fitting both eyebrow arches and one outer ear contour to the scalp to avoid errors caused by human operation.
Typical cases
Case 1
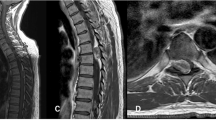
A 31 years female patient, admission due to “recurrent headache for 1 year”. No previous unconsciousness, hypertension, diabetes and other medical history. After admission, brain CT revealed tiny high-density shadows in the right temporal lobe (Fig. 1A), and brain MRI revealed abnormal signals in the right temporal lobe. Cavernous hemangiomas were considered (Fig. 1B and C). We import DICOM data from preoperative thin slice CT of the patient’s brain into 3D Slicer software for reconstruction processing, create a 3D virtual reality image (Fig. 1D), and then design a 3D printing positioning guide plate to confirm the depth of the lesion (Fig. 1E). The guide plate needs to include the contours of both eyes and one side of the auricle. Before surgery, the body surface position of the lesion was accurately located using a 3D printing positioning guide plate (Fig. 1F), local hairdressing was performed, and a minimally invasive arc incision was designed (Fig. 1K). During the operation, we used neuroendoscope assistance to quickly locate the lesion and completely resect it (Fig. 1G and H). Postoperative reexamination of the brain CT revealed that the lesion was completely removed (Fig. 1I), with a bone window size of about 2.8 cm (Fig. 1J). Pathological examination revealed a cavernous hemangioma (Fig. 1L).
Case 2
A 31 years female patient, admission due to “sudden syncope for 3 days”. The child has a previous history of multiple syncope, and the local brain MRI shows abnormal signals in the right temporal lobe, considering a cavernous hemangioma (Fig. 2B). After admission, brain CT showed small high-density lesions in the right temporal lobe (Fig. 2A). We imported DICOM data from preoperative thin slice CT of the patient’s brain into 3D Slicer software for reconstruction processing (Fig. 2H), produced 3D virtual reality images, and then designed 3D printing positioning guides (Fig. 2C and D). Before surgery, accurately locate the body surface position of the lesion using a 3D printing positioning guide, perform local hairdressing, and design a minimally invasive linear incision (Fig. 2F and G). During the operation, we used neuroendoscope assistance to quickly locate the lesion and completely resect it (Fig. 2E, I, and J). After the operation, the brain CT scan showed that the lesion was completely resected (Fig. 2K), with a bone window size of about 2.6 cm (Fig. 2L). The pathological examination showed a cavernous hemangioma (Fig. 2M).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the ethics committee of Clinical Research, Renmin Hospital of Wuhan University (WDRY2022-K099).
Clinical significance
-
1.
Recurrent bleeding from intracranial cavernous hemangioma may lead to headaches, epilepsy, and other conditions, seriously endangering the patient's health and quality of life.
-
2.
2. Intracranial cavernous hemangioma is usually a small lesion with a size of about 1cm, located in deep brain tissue, and has difficulty in localization. Conventional surgery can cause significant trauma and complications.
-
3.
3. 3D Slicer reconstruction and 3D printing positioning technology are simple, cheap and accurate, which can provide good guidance for neurosurgery surgery positioning.
-
4.
4. Neuroendoscopy has the advantages of good lighting, flexible degrees of freedom, and close observation, which can provide minimally invasive technical support for the surgery of deep intracranial lesions.
Discussion
A large study6 has shown that the prevalence of CCH is about 0.1–0.5%, accounting for 10–20% of all intracranial vascular malformations. The age of onset is typically between 20 and 30 years or older, and about 40% of the patients have no neurological symptoms. The other patients may have recurrent headaches, hemorrhagic fevers, seizures, or focal neurological deficits. Although there are a large number of literature reports on CCH, there are still disputes about its diagnosis and treatment. Due to the fact that the lesions are often small, without significant space occupying effects, and with a low risk of bleeding from the lesions, conservative treatment is usually recommended for incidental CCH7. Cavernous hemangiomas located in superficial and non-essential functional areas or have symptoms while are easily accessible for surgery can be removed by microsurgery. For symptomatic CCH, if located in deep important functional areas or in the brain stem, considering the enormous surgical risks and the possibility of serious surgical complications, surgical treatment is generally not recommended, and radiation therapy is recommended3. However, a cohort study8 showed that among patients without a history of bleeding, the annual bleeding rate of CCH was relatively low, about 0.6%, while among patients with a history of bleeding, the rate of rebleeding is about 4.5%. Other studies7 have shown that when clinical and radiological findings indicate a history of bleeding twice, the annual rate of rebleeding can be as high as 34%. The risk of bleeding from CCH varies depending on ___location, and lesions located in the deep brain have a higher risk of bleeding, with a yearly risk of rebleeding ranging from 5 to 60%6. Understanding the risks of bleeding and rebleeding in these lesions can help clinicians make correct decisions and provide appropriate treatment options, such as early surgical treatment for deep lesions after their first bleeding.
3D Slicer is a free image analysis and processing software jointly developed by Harvard University and Massachusetts Institute of Technology. It does not require high workstation requirements and can be run on daily home computers. It can reconstruct image data obtained from MRI, CT, etc. before surgery, and construct a multimodal virtual 3D visualization model to provide a large amount of accurate three-dimensional anatomical information, and help doctors dynamically observe intracranial lesions and intuitively understand the relationship between the lesion tissue and surrounding structures, providing scientific basis for formulating and implementing surgical plans9. In recent years, the optimization and upgrade of 3D Slicer has gradually broadened its application field4,5. 3D printing is a newly developed tool for surgical planning based on 3D reconstruction technology to better create surgical plans. Using a 3D virtual reality model before surgery can allow patients and surgeons to visually observe intracranial lesions, help doctors better observe the relationship between the lesions and surrounding tissues, develop the most appropriate surgical plan, and help doctors more easily explain the surgical plan to patients when communicating with them about their condition. Using 3D printing positioning guides to accurately locate intracranial lesions before surgery can help improve surgical efficiency and success rate. Adding 3D printing to surgical practice has been proven to improve patient satisfaction and contribute to good surgical results5,10.
Considering the risk of bleeding from cavernous hemangiomas in the deep brain and the positive signs of the nervous system such as headache and epilepsy that have been caused. Our team integrates relevant clinical experience and advocates active surgical treatment. However, for small cavernous hemangiomas in the deep brain (with a maximum diameter of less than 1.5 cm), accurate localization without neuronavigation assistance is extremely difficult. Our previous clinical study introduced a case of successfully using 3D Slicer reconstruction combined with virtual reality technology for precise positioning and minimally invasive resection of brainstem cavernous hemangiomas4. Recently, we have developed a new 3D printing positioning guide technology5 based on this technology for the surgical treatment of small cavernous hemangiomas in the deep brain, and achieved good results. Our team uses 3D Slicer reconstruction technology to build a multimodal 3D visual virtual reality model of small cavernous hemangiomas in the deep brain, and uses corresponding technical means to create a 3D printing positioning guide plate to assist in accurate positioning. Before surgery, we develop a detailed surgical plan for accurate and minimally invasive surgery. During the entire perioperative period, we only need to have a haircut in the local area of the surgical site, meeting the patient’s requirements for rapid restoration of preoperative appearance. At the same time, precise positioning allows for small surgical incisions, high surgical efficiency, and fewer surgical side injuries, greatly shortening the surgical time and postoperative rehabilitation time, and improving the patient’s surgical experience and satisfaction.
Summary
In summary, repeated bleeding from small cavernous hemangiomas in the deep brain can lead to clinical symptoms such as recurrent headache and epilepsy. Lesions located in important functional areas or in the brain stem can even lead to more serious adverse consequences. However, for deep lesions in brain tissue, especially small lesions, the difficulty and risk of surgery are extremely high without a neuronavigation neurosurgical unit, and improper operation may lead to serious consequences. Our team’s newly developed 3D Slicer reconstruction and virtual reality technology combined with 3D printing precise positioning guide plate technology can increase effective communication between doctors and patients, help doctors formulate more perfect and appropriate surgical plans, and provide new options for accurate and minimally invasive surgery for small cavernous hemangiomas or other small lesions in the deep brain. However, its accuracy and safety still need further clinical research and verification.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Chirchiglia, D. et al. An unusual association of headache, epilepsy, and late-onset Kleist’s pseudodepression syndrome in frontal lobe cavernoma of the cerebral left hemisphere. Int. Med. Case Rep. J. 10, 163–166 (2017).
Murata, T. “Kissing“ brainstem cavernous angiomas removed using a trans-fourth ventricular floor approach–case report. Neurol. Med. Chir. 51(10), 724–727 (2011).
Merlino, L. Cerebral cavernous malformation: Management and outcome during pregnancy and puerperium. A systematic review of literature. J. Gynecol. Obstet. Hum. Reprod. 50(1), 101927 (2021).
Zhou, L. Clinical application of 3D Slicer combined with Sina/MosoCam multimodal system in preoperative planning of brain lesions surgery. Sci. Rep. 12(1), 19258 (2022).
Zhou, L. Clinical application of 3D-Slicer + 3D printing guide combined with transcranial neuroendoscopic in minimally invasive neurosurgery. Sci. Rep. 12(1), 20421 (2022).
Liu, W. Y. A chinese family with cerebral cavernous malformation caused by a frameshift mutation of the CCM1 gene: A case report and review of the literature. Front. Neurol. 13, 795514 (2022).
Aydin, S. Secondary parkinsonism in a patient with a cerebral cavernous hemangioma treated with stereotactic radiosurgery. Cureus. 13(3), e14128 (2021).
Gomez-Paz, S. Symptomatic hemorrhage from cerebral cavernous malformations: Evidence from a cohort study. World Neurosurg. 135, e477–e487 (2020).
Liu, J. Effect of 3D slicer preoperative planning and intraoperative guidance with mobile phone virtual reality technology on brain glioma surgery. Contrast Med. Mol Imaging. 2022, 9627663 (2022).
Damon, A. Cost-effective method for 3-dimensional printing dynamic multiobject and patient-specific brain tumor models: Technical note. World Neurosurg. 140, 173–179 (2020).
Funding
This work was supported by National Natural Science Foundation of China (82271518; 81971158; 81671306); The Interdisciplinary Innovative Talents Foundation from Renmin Hospital of Wuhan University (JCRCFZ-2022-030); Guiding projects of traditional Chinese medicine in 2023–2024 by Hubei provincial administration of traditional Chinese medicine (ZY2023F038).
Author information
Authors and Affiliations
Contributions
Qiang Cai and Daofa Sun study concept and design, critical revision of manuscript for intellectual content, acquisition of data. Long Zhou, Zhiyang Li and Yong Cai collect and analysis data, and write manuscripts Huikai Zhang, Hangyu Wei, Ping Song, Li Cheng, Pan Lei, Lun Gao, Qiuwei Hua, Qianxue Chen, Hui Ye collection and interpretation of data.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhou, L., Li, Z., Cai, Y. et al. 3D Slicer and 3D printing localization combined with neuroendoscopic surgery for the treatment of deep cerebral cavernous hemangioma. Sci Rep 14, 18519 (2024). https://doi.org/10.1038/s41598-024-68068-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68068-5
Keywords
This article is cited by
-
A personalized 3D printed cranial shield using mirror-image modeling: design and clinical assessment
3D Printing in Medicine (2025)