Abstract
This study aimed to explore physicians’ and pharmacists’ knowledge, attitudes, and practice (KAP) regarding the prevention and treatment of cardiovascular toxicity associated with cancer treatment. A multicenter cross-sectional study included physicians and pharmacists between April 2023 and June 2023. The study included 918 participants (514 physicians and 404 pharmacists). The average scores of knowledge, attitudes, and practice were 11.6 ± 3.39, 24.7 ± 2.6, and 26.3 ± 6.8 points. Sufficient knowledge was significantly associated with age ≥ 41 years (odds ratio (OR) = 2.745, 95% confidence interval (CI) 1.086–6.941, P = 0.033), male (OR = 2.745, 95% CI 1.150–2.223, P = 0.005), bachelor’s degree (OR = 0.084, 95% CI 0.013–0.533, P = 0.009), master’s degree and above (OR = 0.096, 95% CI 0.015–0.609, P = 0.013), physician occupation (OR = 7.601, 95% CI 1.337–43.207, P = 0.022), pharmacy department (OR = 18.858, 95% CI 3.245–109.57, P = 0.001), oncology department (OR = 4.304, 95% CI 2.426–7.634, P < 0.001), cardiology department (OR = 3.001, 95% CI 1.387–6.492, P = 0.005), hospitals located in Eastern China (OR = 1.957, 95% CI 1.120–3.418, P = 0.018), and hospitals located in Western China (OR = 3.137, 95% CI 1.783–5.518, P < 0.001). Positive attitudes were significantly associated with a senior professional title (OR = 2.989, 95% CI 1.124–7.954, P = 0.028) and hospitals located in Eastern China (OR = 0.424, 95% CI 0.257–0.698, P = 0.001), Western China (OR = 0.231, 95% CI 0.136–0.394, P < 0.001), and Southern China (OR = 0.341, 95% CI 0.198–0.587, P < 0.001). Proactive practice was significantly associated with male (OR = 1.414, 95% CI 1.029–1.943, P = 0.033), senior professional title (OR = 3.838, 95% CI 1.176–12.524, P = 0.026), oncology department (OR = 3.827, 95% CI 2.336–6.272, P < 0.001), and cardiology department (OR = 2.428, 95% CI 1.263–4.669, P = 0.008). Both physicians and pharmacists had positive attitudes toward the prevention and treatment of cardiovascular toxicity associated with cancer treatment, while their knowledge and practice were not as proactive.
Similar content being viewed by others
Introduction
Emerging cancer therapies could assist cancer patients with more treatment modalities to improve their survival and decrease the recurrence rate. However, such new therapies are inevitably associated with a higher incidence of toxicity1,2. Cardiovascular toxicity is one of the most important adverse reactions associated with cancer treatment3,4. Cancer treatment may affect the cardiovascular system through multiple potential mechanisms, including directive cellular toxicity, influencing the coagulation system, arrhythmogenic effects, hypertensive effects, and myocardial inflammation, which may lead to subclinical myocardial dysfunction to irreversible heart failure, or even death5,6. A recent study demonstrated that in patients receiving anticancer therapy who are at moderate or high risk of cardiotoxicity, cardiotoxicity was identified in 37.5% of patients at follow-up7. Furthermore, cases with severe cardiotoxicity were found to be at a significantly increased risk of all-cause mortality4. The overall beneficial effects of cancer therapy may be negatively affected by the potential damage to the patient’s cardiovascular health, and the development of cardiovascular diseases may be deleterious to the optional doses and timing of lifesaving cancer therapy8. It is important for healthcare providers to profoundly understand the mechanisms of cardiovascular toxicity related to cancer treatment and appropriately monitor, prevent, and treat cancer-related heart disease9,10.
To date, few studies have concentrated on healthcare providers’ perspectives on the prevention and treatment of cardiovascular toxicity associated with cancer treatment. A qualitative study on breast cancer patients’ cardiac surveillance found that oncologists were unaware of the cardiotoxicity risk and the benefit of cardiac surveillance in cancer treatment11. Another interventional study also demonstrated that oncologists had unsatisfactory knowledge and cardiovascular screening practice at baseline12. Furthermore, one mixed-method study investigating the treatment of cancer patients found that oncologists have rarely discussed the potential for cardiotoxicity and risk modification strategies with patients, demonstrating the need to improve care management13. However, these studies are restricted by the small sample sizes and failure to include non-oncology physicians and pharmacists, playing an important role in the management of cancer treatment. A comprehensive study is therefore required to investigate physicians’ and pharmacists’ knowledge, attitudes, and practice (KAP) regarding the prevention and treatment of cardiovascular toxicity associated with cancer treatment. A KAP survey is a quantitative method that is widely used for health-related topics based on the principle that knowledge may affect behavior and practice of disease management14. The KAP of cardiovascular toxicity associated with cancer treatment among healthcare providers has not yet been studied.
Understanding physicians’ and pharmacists’ KAP on this topic may effectively promote the management of cancer treatment-related cardiovascular toxicity. Therefore, the present study aimed to assess the KAP toward the prevention and treatment of cardiovascular toxicity associated with cancer treatment among physicians and pharmacists and to identify factors influencing KAP.
Results
Demographic characteristics
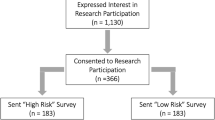
A total of 1,196 questionnaires were distributed, and 918 questionnaires were included in the analysis (76.8%). More than half of the participants were 31–40 years old (60.2%), female (52.6%), and physicians (56.0%) (Table 1). The majority of them obtained a master’s degree or above (71.9%). Most of the participants had intermediate titles (60.0%), followed by senior titles (20.4%) and primary titles (16.0%). Over one-third had 6–10 years of work experience, followed by those with ≤ 5 years (25.9%), 11–15 years (19.8%), and ≥ 16 years (19.3%). Around 42% of participants worked in the pharmacy department, followed by the oncology department (28.2%), the cardiology department (6.2%), and other departments (23.6%). Over 80% of participants worked in tertiary hospitals. Northern China had the largest number of hospitals (35.6%).
Scores of knowledge, attitudes, and practice dimensions
The average score of knowledge dimension was 11.6 ± 3.39 (range, 0–17) points (Table 1). Knowledge-based questions on the negative effects and the primary prevention of cardiovascular toxicity had higher correct rates (89.0–90.1%), while questions regarding drug properties (e.g., first-line antihypertensive drugs, cardiotoxicity of chemotherapy, and correct administration of targeted therapy with chemotherapeutic drugs) had lower correct rates (13.9–46.6%) (Table 2).
The average score of attitude dimension was 24.7 ± 2.6 (range, 6–30) points (Table 1). Supplementary Fig. S2 shows the distribution of the attitudes. The average score of practice dimension was 26.3 ± 6.8 (range, 8–40) points (Table 1). The distribution of the practice evaluation is presented in Supplementary Fig. S3.
A comparison of the correct rates of questions related to the knowledge dimension revealed that participants from the oncology department and those from hospitals in Western China tended to have higher correct rates (Supplementary Table 1). Physicians, those who worked in the oncology department, and those from hospitals in Northern China were more likely to rate Strongly Agree on questions related to the attitude dimension (Supplementary Table 2). Physicians, those who worked in oncology departments, and those from hospitals in Eastern China were more likely to participate in the development of treatment plans; physicians, those who worked in non-oncology clinical departments, and those from hospitals in Northern China tended to receive training on cardiovascular toxicity associated with cancer treatment (Supplementary Table 3).
Correlations between the knowledge, attitude, and practice scores
Pearson correlation analysis (Table 3) revealed that the knowledge score was significantly positively correlated with the attitude score (r = 0.208, P < 0.001) and practice score (r = 0.277, P < 0.001). There was also a positive correlation between the attitude and practice scores (r = 0.268, P < 0.001).
Factors associated with KAP
The results of multivariable logistic regression analysis revealed that sufficient knowledge was significantly associated with age ≥ 41 years (odds ratio (OR) = 2.745, 95% confidence interval (CI) 1.086–6.941, P = 0.033), male (OR = 2.745, 95% CI 1.150–2.223, P = 0.005), bachelor’s degree (OR = 0.084, 95% CI 0.013–0.533, P = 0.009), master’s degree and above (OR = 0.096, 95% CI 0.015–0.609, P = 0.013), physician occupation (OR = 7.601, 95% CI 1.337–43.207, P = 0.022), pharmacy department (OR = 18.858, 95% CI 3.245–109.57, P = 0.001), oncology department (OR = 4.304, 95% CI 2.426–7.634, P < 0.001), cardiology department (OR = 3.001, 95% CI 1.387–6.492, P = 0.005), hospitals located in Eastern China (OR = 1.957, 95% CI 1.120–3.418, P = 0.018), and hospitals located in Western China (OR = 3.137, 95% CI 1.783–5.518, P < 0.001) (Table 4).
Positive attitudes were significantly associated with a senior professional title (OR = 2.989, 95% CI 1.124–7.954, P = 0.028) and hospitals located in Eastern China (OR = 0.424, 95% CI 0.257–0.698, P = 0.001), Western China (OR = 0.231, 95% CI 0.136–0.394, P < 0.001), and Southern China (OR = 0.341, 95% CI 0.198–0.587, P < 0.001) (Table 4).
Proactive practice was significantly associated with male (OR = 1.414, 95% CI 1.029–1.943, P = 0.033), senior professional title (OR = 3.838, 95% CI 1.176–12.524, P = 0.026), oncology department (OR = 3.827, 95% CI 2.336–6.272, P < 0.001), and cardiology department (OR = 2.428, 95% CI 1.263–4.669, P = 0.008) (Table 4).
Structural equation modeling
Figure 1 presents the SEM. Knowledge directly affected attitudes (β = 0.406, P < 0.001) and practice (β = 0.353, P < 0.001). Attitudes directly affected practice (β = 0.316, P < 0.001). Knowledge indirectly affected practice by influencing occupation (β = 0.240, P = 0.004), which, in turn, influenced practice (β = 0.232, P < 0.001).
Discussion
This KAP study concluded that both physicians and pharmacists had positive attitudes toward the prevention and treatment of cardiovascular toxicity associated with cancer treatment, while their knowledge and practice were not proactive. The regression analyses demonstrated that age > 41 years, male, bachelor’s degree, master’s degree and above, physician occupation, pharmacy department, oncology department, cardiology department, hospitals located in Eastern China, and hospitals located in Western China were associated with adequate knowledge; senior professional titles and working at hospitals from Central China were associated with positive attitudes; male gender, senior professional titles, and working at the oncology and cardiology departments were associated with proactive practice. The above-mentioned factors related to each dimension are valuable in identifying individuals who need further training and intervention.
The average score of the knowledge dimension was 11.6 out of 17 points (< 70%), which is consistent with findings of similar studies on oncologists and other healthcare providers15,16,17. In an international survey on the knowledge of cardiac complications related to cancer treatment, 66.9% of healthcare providers demonstrated that they were familiar with guidelines for managing cardiotoxicity15. While more participants were aware of the negative effects of cardiotoxicity associated with cancer treatment, fewer correctly answered questions related to the properties of cancer drugs. The knowledge gap was also recognized in other studies15,16. Additional efficient strategies are therefore required to fill in the knowledge gap regarding the prevention and treatment of cardiotoxicity associated with cancer treatment. The present study also revealed that participants who worked in oncology, cardiology, and pharmacy departments had better knowledge than others. Although physicians from other clinical departments can have to treat cancer patients in routine care, they might not have relevant knowledge about cardiotoxicity associated with cancer treatment. Among non-oncology physicians, cardiology specialists play a critical role in the management of cardiotoxicity in cancer patients because the risk of post-treatment recurrence is noteworthy18. Therefore, it is important to train non-oncology and non-cardiology physicians on the knowledge related to this topic. Furthermore, the survey revealed that a higher educational level was not necessarily an indicator of a greater level of knowledge, and healthcare providers with different educational levels should be assisted with relevant educational and training programs.
The present study demonstrated a satisfactory level of attitudes toward the prevention and treatment of cardiotoxicity in cancer treatment among physicians and pharmacists. The average score of attitude dimension was 24.7 out of 30 points (> 70%). Similar studies have previously reported mixed results. On the one hand, a qualitative study conducted by Knowle et al. found that the majority of healthcare providers were aware of the risk of cardiotoxicity in cancer treatment and agreed that it is an important issue to address17. On the other hand, Kozhukhov et al. reported that most healthcare providers did not agree that increased cardiac monitoring can prevent cardiotoxicity in cancer patients or improve cancer patients’ quality of life19. However, those with more positive attitudes demonstrated that their colleagues’ lack of knowledge on the topic was a major barrier. Notably, a lack of knowledge on the topic could negatively affect healthcare providers’ perceptions17.
The average score of the practice dimension was 26.3 out of 40 points (< 70%), representing a less-than-satisfactory level of practice among physicians and pharmacists. This finding is consistent with the literature. In an international survey, 12% of oncologists agreed that cardiotoxicity should be monitored in asymptomatic cancer patients, and only 2.1% felt comfortable treating cardiovascular complications associated with cancer therapy15. In Clark et al.’s study, cancer patients who developed cardiotoxicity raised the concern that oncologists did not discuss the potential for cardiotoxicity with them before treatment, and no risk modification strategy was applied13. Additionally, the necessary diagnostic tools, such as biomarkers, have not been well utilized by healthcare providers19,20. This is an important concern that needs to be addressed to provide high-quality cancer treatment and improve patients’ outcomes. The present study also indicated that pharmacists and physicians from non-oncology and non-cardiology departments had lower scores in the practice dimension, reflecting the necessity of additional training for such healthcare providers.
The present study had several limitations. Firstly, due to the self-reporting nature of the study, the results might deviate from the actual practice. The questionnaire was distributed through professional WeChat groups, and no general list of registered physicians/pharmacists was used was used, possibly leading to bias. Secondly, the majority of participants positively answered the questions related to the attitude dimension, and the results might be affected by the social desirability bias. Thirdly, there might be non-response bias from the use of online surveys. However, this study collected data from all regions in China, which enhanced the representativeness of the findings.
In conclusion, the present cross-sectional study demonstrated satisfactory attitudes toward the prevention and treatment of cardiovascular toxicity associated with cancer treatment among physicians and pharmacists, while the levels of knowledge and practice were less satisfactory. Effective educational and training programs are needed for this population, especially in the weaker areas, such as the properties of anticancer drugs. Various factors associated with the level of KAP were also identified. It is important to take these factors into account when designing training programs. For instance, physicians from non-oncology and non-cardiology departments may need additional education and training to enhance their knowledge and practice in this area. Educational tools, including electronic learning guidelines, case discussions, and multidisciplinary team consultations, are potentially advantageous in improving KAP toward the prevention and treatment of cardiovascular toxicity associated with cancer treatment. Future studies should explore effective interventions to enhance this population’s KAP.
Methods
Study design and participants
The present cross-sectional study was conducted in China between April 2023 and June 2023, and the participants were Chinese physicians and pharmacists.
The inclusion criteria were as follows: (1) Physicians who were experts in cancer treatment and were certified as occupational physicians; (2) Physicians who had experience treating cancer patients in non-oncology departments and were certified as occupational physicians; and (3) Pharmacists who had experience of anti-tumor treatment and were certified as occupational pharmacists.
The present study was approved by the Ethics Committee of the Third Hospital of Hebei Medical University (2023-015-1), and informed consent was obtained from all participants.
Questionnaire design
The questionnaire was designed with reference to the Chinese Society of Clinical Oncology Guidelines for the Prevention and Treatment of Cardiovascular Toxicity Associated with Cancer Treatment (2021)21, and it was then modified based on 6 senior experts’ comments. In total, 41 physicians and pharmacists (22 physicians and 19 pharmacists) were selected by random sampling to examine the reliability of the questionnaire, with a Cronbach’s α coefficient of 0.8380, suggesting a satisfactory internal consistency.
The final questionnaire included four dimensions: demographic characteristic dimension (age, gender, occupation, professional title, work experience, department, level of hospital, and the region of the hospital (Supplementary Fig. S1), knowledge dimension, attitude dimension, and practice dimension. In China, junior, intermediate, and senior professional titles are used to reflect the technical level, ability, and academic achievement of healthcare professionals. Healthcare professionals gain professional designations when they meet the requirements for each title, including reaching the minimum years of work experience for the position, successfully completing the relevant examinations, and completing the various specialty- and ___location-specific requirements. Qualified physicians who have not yet been accredited in their specialty (e.g., trainee psychiatrists) have no professional title; they receive the junior title once they obtain their certification. The system is similar for other healthcare professionals (e.g., pharmacists and nurses)22. The knowledge dimension included 17 questions, including 1 point for correct answers and 0 points for wrong or unclear answers, and the score ranged from 0 to 17 points. The attitude dimension consisted of 6 questions, and a 5-point Likert scale was used, in which positive attitude questions rated from “Strongly Agree” (5 points) to “Strongly Disagree” (1 point) and the negative attitude question (Question 5) was rated reversely, ranging from 6 to 30 points. The practice dimension consisted of 9 questions, and a 5-point Likert scale was utilized, ranging from “Always” (5 points) to “Never” (1 point). Question 9 was not included in the total practice score, and therefore, the practice dimension ranged from 8 to 40 points.
A score greater than 70% of the total was defined as sufficient knowledge, positive attitudes, and proactive practice23.
Data collection and quality control
The questionnaire content was reviewed and imported into the Sojump online platform (https://www.wjx.cn/app/survey.aspx), and a valid link was generated. In order to conduct the survey more objectively, we did not set a specific center, hospital, or clinic. The questionnaires were mainly distributed through relevant medical and pharmacy professional WeChat groups. A research staff introduced the purpose, content, and significance of the study to potential participants and screened them by convenient sampling for eligibility via WeChat. Eligible participants who agreed to participate in the survey were then invited to complete the online informed consent form, and a web link for the questionnaire was forwarded to each participant. Any inquiries raised by the participants could be answered promptly by the research staff. The questionnaire could not be submitted until all items had been completed by the participant to ensure that there were no missing items in the returned questionnaire. To prevent duplication of questionnaires, each participant could only submit the questionnaire once using an electronic device (e.g., a mobile phone or a computer). Reviewers could directly review the collected questionnaires by logging into the platform. Questionnaires with incomplete or contradictory answers determined by logical judgment were regarded as invalid questionnaires.
The sample size calculation was not carried out due to the large number of registered physicians and pharmacists in China.
Statistical analysis
SPSS 26.0 software (IBM Corp., Armonk, NY, USA) was used to perform statistical analysis. Continuous data were first tested for normality, in which normally distributed continuous data were expressed as mean ± standard deviation (SD) and abnormally distributed continuous data were expressed as median (range). The categorical data were presented as n (%) and analyzed using the chi-square test and Fisher’s exact probability test. Pearson correlation analysis was used to evaluate the correlations between the knowledge, attitude, and practice scores. Multivariable logistic regression analysis (variable screening: Enter) was used to explore the influential factors of KAP measured binary as ‘sufficient’ or ‘not sufficient’. The interactions among the KAP dimensions were evaluated using a structural equation model (SEM). It was hypothesized that knowledge directly affects attitudes and practice, while attitudes directly affect practice. P < 0.05 was considered statistically significant.
Data availability
All data generated or analysedanalyzed during this study are included in this published article [and its supplementary information files].
References
Saleh, Y., Abdelkarim, O., Herzallah, K. & Abela, G. S. Anthracycline-induced cardiotoxicity: Mechanisms of action, incidence, risk factors, prevention, and treatment. Heart Fail. Rev. 26, 1159–1173 (2021).
Floyd, J. D. et al. Cardiotoxicity of cancer therapy. J. Clin. Oncol. 23, 7685–7696 (2005).
Florescu, M., Cinteza, M. & Vinereanu, D. Chemotherapy-induced Cardiotoxicity. Maedica (Bucur) 8, 59–67 (2013).
Han, X., Zhou, Y. & Liu, W. Precision cardio-oncology: Understanding the cardiotoxicity of cancer therapy. NPJ Precis. Oncol. 1, 31 (2017).
Albini, A. et al. Cardiotoxicity of anticancer drugs: The need for cardio-oncology and cardio-oncological prevention. J. Natl. Cancer Inst. 102, 14–25 (2010).
Gillespie, H. S., McGann, C. J. & Wilson, B. D. Noninvasive diagnosis of chemotherapy related cardiotoxicity. Curr. Cardiol. Rev. 7, 234–244 (2011).
López-Sendón, J. et al. Classification, prevalence, and outcomes of anticancer therapy-induced cardiotoxicity: The CARDIOTOX registry. Eur. Heart J. 41, 1720–1729 (2020).
Curigliano, G. et al. Cardiotoxicity of anticancer treatments: Epidemiology, detection, and management. CA Cancer J. Clin. 66, 309–325 (2016).
Lenneman, C. G. & Sawyer, D. B. Cardio-oncology: An update on cardiotoxicity of cancer-related treatment. Circ. Res. 118, 1008–1020 (2016).
Jain, D., Ahmad, T., Cairo, M. & Aronow, W. Cardiotoxicity of cancer chemotherapy: Identification, prevention and treatment. Ann. Transl. Med. 5, 348 (2017).
Koop, Y. et al. Oncology professionals’ perspectives towards cardiac surveillance in breast cancer patients with high cardiotoxicity risk: A qualitative study. PLoS One 16, e0249067 (2021).
Albert, K., Pollard, D., Klemp, J., Kondapalli, L. & Tuffield, D. Assessment of oncology provider knowledge and cardiovascular screening practices: A call for heightened screening. J. Adv. Pract. Oncol. 12, 795–807 (2021).
Clark, R. A. et al. Cardiotoxicity after cancer treatment: A process map of the patient treatment journey. Cardiooncology 5, 14 (2019).
Ahmed, T. et al. Knowledge, attitude and practice (KAP) survey of canine rabies in Khyber Pakhtunkhwa and Punjab Province of Pakistan. BMC Public Health 20, 1293 (2020).
Peng, J. et al. An international survey of healthcare providers’ knowledge of cardiac complications of cancer treatments. Cardiooncology 5, 12 (2019).
Jovenaux, L. et al. Practices in management of cancer treatment-related cardiovascular toxicity: A cardio-oncology survey. Int. J. Cardiol. 241, 387–392 (2017).
Knowles, R., Kemp, E., Miller, M. & Koczwara, B. Reducing the impact of cardiovascular disease in older people with cancer: A qualitative study of healthcare providers. J. Cancer Surviv. 106, 1353 (2023).
Alexandre, J. et al. Cardiovascular toxicity related to cancer treatment: A pragmatic approach to the American and European Cardio-Oncology guidelines. J. Am. Heart Assoc. 9, e018403 (2020).
Kozhukhov, S. & Dovganych, N. Cardio-oncology educational program: National survey as the first step to start. Front. Cardiovasc. Med. 8, 697240 (2021).
Tan, L. L. & Lyon, A. R. Role of biomarkers in prediction of cardiotoxicity during cancer treatment. Curr. Treat. Options Cardiovasc. Med. 20, 55 (2018).
Chinese Society of Clinical Oncology Guidelines Working Committee. Chinese Society of Clinical Oncology (CSCO) Guidelines for Prevention and Treatment of cardiovascular toxicity associated with cancer treatment 2021. People's Medical Publishing House. (2021).
Sun, M. et al. Professional characteristics, numbers, distribution and training of China’s mental health workforce from 2000 to 2020: A scoping review. Lancet Reg. Health West Pac. 45, 100992 (2024).
Lee, F. & Suryohusodo, A. A. Knowledge, attitude, and practice assessment toward COVID-19 among communities in East Nusa Tenggara, Indonesia: A cross-sectional study. Front. Public Health 10, 957630 (2022).
Acknowledgements
We appreciate the support of Professor He Jingcheng and Chinese Information Pharmacists in this study.
Funding
This study was supported by the National Natural Science Foundation of China (Grant No. 82003878), the Natural Science Foundation of Hebei Province (Grant No. H2024206062 and H2020206554), the Scientific Research Project of Hebei Provincial Administration of Traditional Chinese Medicine (Grant No. 2024285), and the Hospital Pharmacy Project of Hebei Pharmaceutical Association (Grant No. 2020-Hbsyxhms0017).
Author information
Authors and Affiliations
Contributions
CXL, WY, and MLG carried out the studies, participated in collecting data, and drafted the manuscript. CXL, JTM, ZHZ, XJL, LZ, YG, and DXZ performed the statistical analysis and participated in its design. CXL and SG participated in acquisition, analysis, or interpretation of data and draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was carried out after the protocol was approved by the Ethics Committee of the Third Hospital of Hebei Medical University (2023-015-1). I confirm that all methods were performed in accordance with the relevant guidelines. All procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments, and informed consent was obtained from all participants.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, C., Yan, W., Gao, M. et al. Knowledge, attitudes, and practice of physicians and pharmacists regarding the prevention and treatment of cardiovascular toxicity associated with cancer treatment. Sci Rep 14, 20122 (2024). https://doi.org/10.1038/s41598-024-71015-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71015-z