Abstract
This study examines tuberculosis (TB) incidence among students in Jilin Province, China, focusing on spatial, temporal, and demographic dynamics in areas of social inequality. Variation in incidence rate of TB was analyzed using the joinpoint regression method. Spatial analyses techniques included the global and local Moran indices and Getis-Ord Gi* analysis. Demographic changes in new cases were analyzed descriptively, and the Geodetector method measured the influence of risk factors on student TB incidence. The analysis revealed a declining trend in TB cases, particularly among male students. TB incidence showed geographical heterogeneity, with lower rates in underdeveloped rural areas compared to urban regions. Significant spatial correlations were observed, with high-high clusters forming in central Jilin Province. Hotspots of student TB transmission were primarily concentrated in the southwestern and central regions from 2008 to 2018. Socio-economic factors exhibited nonlinear enhancement effects on incidence rates, with a dominant bifactor effect. High-risk zones were predominantly located in urban centers, with university and high school students showing higher incidences than other educational stages. The study revealed economic determinants as being especially important in affecting TB incidence among students, with these factors having nonlinear interacting effects on student TB incidence.
Similar content being viewed by others
Introduction
Tuberculosis (TB), a chronic infectious illness spread through the respiratory system, mostly affects those with reduced immunity and is easily transferred in congregating groups1. In recent years, the student population (aged 6–31 years) has been the focus of TB prevention and control, accounting for the fourth highest incidence. At this age, especially high school children (15–17) and college students (18–21), experience increased academic pressures, as well as significant mental stress, limited physical activity, and high dietary requirements, all of which can be exacerbated by decreasing resistance2,3. At the same time, the majority of high school students board at schools and gather in common areas. Crowded classrooms and diverse risk profiles among them may contribute to the fast spread of TB in school settings4. The reported incidence of TB among Chinese students fell from 20.64/100,000 in 2010 to 13.39/100,000 in 2015, but rose to 17.50/100,000 in 20195,6,7. In higher education institutions of Ethiopia, the mean proportion of student TB cases among the total students enrolled was nearly 0.38%. Meanwhile, a study conducted in Argentina indicated a TB prevalence rate of 6.1% among students. Additionally, research by Alejandro et al. assessed the latent infection rate among school contacts to be between 3.4% and 11.6%8,9,10.
In the past few decades, several research have utilized the Joinpoint regression model (JPR) and spatial autocorrelation to evaluate the temporal and geographical patterns and trends of TB cases in the entire population7,11, and have discovered that TB occurrence is seasonal and spatially dependent. At the same time, studies have demonstrated that the prevalence of TB is directly associated to social determinants, socioeconomic features, and other variables, all of which contribute considerably to patient morbidity and death12. Students are one of the high-risk groups being infected by Mtb, for living in schools such a highly concentrated places of people, descending immunity by high pressure of studies. Tuberculosis outbreaks in school were rather common nowadays13. When tuberculosis occurs in schools, it is easily transferred and may eventually lead to an epidemic14. The high TB rate and lengthy treatment duration of TB have a negative impact on students' physical and mental health, as well as disrupting the instructional process at schools and perhaps affecting social stability15.
However, the role of transmission heterogeneities of Mycobacterium TB (Mtb) in TB among students remains unclear, particularly those heterogeneities driven by time, geography and demography. Therefore, The aim of our analysis is to extend current knowledge of the following three aspects: (1) to synthesize the temporal-spatial pattern of TB among students in four regions of China in the past decades; (2) to understand the main demographical characteristics of the student TB patients, including the age and sex distribution of cases; and (3) to analyze the factors associated with TB among students.
Results
Demographic pattern of newly notified student TB cases
A total of 11,320 cases of student PTB were reported in Jilin Province from 2008 to 2018 (Fig. 1). There were 57.6% male and 42.4% female with a 1.4 sex ratio. PTB affected all age groups and each group with more male than female cases (Fig. S5). The highest burden was among university students who accounted for 53.0% (6000) of all cases, compared with 25.2% (2588) of high school students and 2.4% (277) of primary school students (Table 1, Table 2).
Temporal pattern for changes in newly notified TB cases in Jilin Province
The number of cases decreased yearly (Fig. S1), the incidence also decreased from 6.65/100,000 people in 2008 to 1.99/100,000 people in 2018 (Table 3). The TB case numbers showed distinct seasonality and periodicity, with a higher number of cases in 2009 than in other years and seasonal peaks in March and September of each year, with the lowest case numbers in December.
As for the prefecture-level regions. JL and SY had the highest incidence and a greater degree of decline, whereas SP had steady yearly downward trends (Fig. S2). In SY, the incidence decreased from 8.84/100,000 people in 2008 to 0.90/100,000 people in 2016 but rebounded to 2.07/100,000 people in 2018 (Table 3). The highest TB incidence rate registered in Jilin Province was in 2009 (Table 3), in both men and women (8.06/100,000 in males and 6.45/100,000 in females), decreasing around 13% in males at the end of the period (2018) (Table 3).
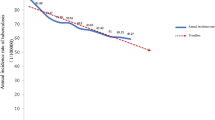
Cases of high school decreased (APC = −13.97, P < 0.001) from 2008 to 2013 and increased (APC = 9.25, P < 0.001) from 2013 to 2018, and all the other cases showed a decreasing trend (Fig. 2a–e, Table 4). There were 3 joinpoints for females, the significant APC was from 2010 to 2014 (APC = −25.58%). Figure 2g displays the decreasing trend of the crude incidence rate by gender, which is more pronounced in males (p < 0.001). The final selected model in Jilin Province was the 3 joinpoint model with an APC of − 8.85 (2008–2010, P > 0.001), −21.35 (2010–2014, P < 0.001) and −2.17 (2014–2018, P > 0.001) (Fig. 2f, Table 4).
Trend in crude incidence rate by sex according to the join points identified by the analysis. (A) represents the whole population, (B) represents the population of primary school students, (C) represents the population of middle school students, (D) represents the population of high school students, I represents the population of university students, (F) represents the population of advanced educational institutions students, (G) represents the whole population by gender.
Spatial patterns and clusters of newly notified TB cases
The geographical distribution of PTB cases
Most cases were in Changchun (3837, 33.9%), Jilin (2820, 24.9%) and Yanbian (1086, 9.6%), with the smallest shares in Liaoyuan (212, 1.9%) (Tables 1, 2). PTB cases at county level have regional aggregation (Fig. S3). There was high clustering in 2 counties, covering 1 county-level city of CC (No 57: Yushu) and 1 county-level city of YB (No 54: Yanji). The descriptive analysis gave a rough impression that 2 prefecture-level cities (CC, YB) had a higher PTB burden than other prefectures. Clustering distribution is further tested by spatial autocorrelation analysis.
Global spatial autocorrelation
As for the global spatial autocorrelation analysis, it suggested that the significant clustering distribution has been detected at the county level in Jilin Province since 2008, with the significance level of 0.05 (Table S2). The spatial pattern is classified as “cluster” in most years, and we can find five high-clusters (Table S3) in 2009, 2010, 2014, 2017, and 2018.
Local spatial autocorrelation
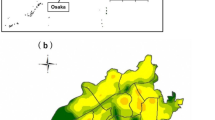
The detected PTB HH clusters stably located in the center of Jilin over the reporting years, mainly aggregating in 8 counties (No: 0, 1, 2, 3, 4, 5, 6, 7) (Fig. 3). The results are basically consistent with those from the geographically descriptive analysis above. Meanwhile, 3 counties (No: 51, 56, 57) were found as a HH cluster in 2017 and 2018, respectively. The results also showed that LL clusters were consistently located in diverse counties over the reported years, excluding the southeast part. Yearly, LH clusters were scattered in 7 counties in the east (No: 2, 5, 6, 17, 19, 21, 22), while four years reported no LH clusters (2011, 2013, 2017, 2018). HL clusters disappeared in most years and appeared in only four years (2009, 2014, 2015, 2016), which shows a random pattern in ___location.
Cold-hot spots analysis
There are two regions including hot spots of PTB incidence, located in the southwest and center, and some cities in southeast once showed the characteristics of hot spots (Fig. S4). Counties in the center have been showing a trend of high-value aggregation. In recent years, the center of gravity of high-value aggregation area in the center of Jilin has moved further east. The cold spot areas are located in the western and southeast areas.
Correlation with social factors in Jilin Province
Factor detection
Based on GD model, the student TB incidence and environmental factors from 2008 to 2018 were selected as samples to explore the similarity between the spatial distribution of them. Figure 4a shows the results of GD model. Among the selected environmental factors, PDIR (Per capita disposable income of rural residents) did not pass the significance test of single factor detection when choosing number of cases as dependent variable. This indicates an apparent correlation between these factors and student TB incidence from the perspective of geographical distribution.
GeoDetector results for association of environmental factors with student TB incidence (Land area: LA; Per capita disposable income of rural residents: PDIR; Per capita disposable income of urban residents: PDIU; Number of permanent residents: NPR; Number of primary school populations: NPP; Number of middle school populations: NMP; Number of high school populations: NHP; Number of undergraduate populations: NUP; Number of post-graduate populations: NGP; Gross Domestic Product: GDP; GDP per capita: PGDP; Number of health institutions: NHI; Number of health technicians per unit population: NHT; Number of beds in health care facilities: NB; Y: patients per 100,000 population. The first row represents the results of factor detection analysis from the perspective of patients per 100,000 population (a); The second row represents the results of interaction detection analysis from the perspective of patients per 100,000 population (b).
Among the 14 environmental factors examined, the q value of PDIU (Per capita disposable income of urban residents) was the largest (0. 4255), indicating that the PDIU factor had the highest geographical distribution similarity with student TB incidence, and it had the highest potential impact. The order of q value for environmental factors is PDIU > PDIR > NMP > NPP > NB > LA > NHP > GDP > NGP > NPR > NHI > NUP. Influence of economic factors on TB incidence is stronger than that of medical and social factors.
Interaction detection
The interaction results between environmental factors are shown in Fig. 4b. The interaction between per capita disposable income of urban residents and land area (0.8888) is the highest similarity with the geographical distribution of TB incidence. The interaction between land area and economic factors has a stronger influence on TB incidence than most other factors. This indicates that areas with obvious land areas and economic characteristics need more attention.
Discussion
The APC of student TB incidence in Jilin Province was from − 2.17 to − 21.35, which is better than the world annual reduction of only about 2%16. The reason for the decline in student TB incidence is the rising economy power, high urbanization, and the widespread modern control strategy for schools17. The most remarkable result to emerge from the data is that the increasing trend in incidence rates among high school students, which reveals a concerning epidemiological scenario for TB in the population of students. This trend was also observed in other studies18 that corroborate our findings. These data signal an alert situation, since students in high school may indicate a high transmission among the population due to dense contacts.
Our study provides additional support for considerable insight into spatial pattern of student TB patients. This study reflects risks for illness in different regions and changes in the pattern of the disease over the years. The center of gravity of high-value aggregation area in the center of Jilin has moved further east. The possible explanation is the unbalanced economic development in these areas19, and the migratory process of people from the peripheries to the center region of the province looking for better living conditions in the more economically developed areas. Some studies20,21 have demonstrated that there has positive correlations between the poverty level of regions, families or individuals and the incidence of TB. The Moran map pointed to the central region of Jilin with a higher concentration of cases and significant spatial dependence, which may induce, in the near future, the continuous spread of the disease and new infections, even in neighbouring prefecture-level cities. Health systems need to respond better and faster to these challenges of a changing world22. Therefore, the identification of the main risk areas based on geographical units and the planning of health promotion and prevention actions based on the real needs of the exposed population are necessary for the development of public policies19.
These results offer crucial evidence for demographical characteristics among student patients. We found the highest prevalence group is university students, followed by high-school students. Our findings corroborate with previous result, a systematical review on school outbreaks in China also revealed that outbreaks that occurred at universities or colleges had a relatively higher attack rate than those occurred in senior middle schools23. In recent years, the Bacillus Calmette-Guérin (BCG) vaccination rate of Chinese infants after birth is 99%24, but persistence of the immune response induced by BCG vaccination is not persistent25. Previous studies indicated protection can last for up to 60 years in North American Indians26, 10–15 years in a review analysis27. Moreover, the unique Chinese education system are the source of special illness experience of TB patients in high school28, because of high pressure in college entrance examination29. Thus, they are prone to get sick faced with pressure and decreasing immunity. Hence, target actions should be taken for outbreaks at high schools and universities. Furthermore, our study found that the incidence rate is higher in males than in females, consistent with the findings of Odongo et al.30,31,32. This may be related to the higher awareness of tuberculosis prevention and control among females, as well as their better hygiene practices and health consciousness33. Meanwhile, males tend to have a wider range of activities and may have more frequent interactions with others31. However, Xiao et al.34 found that females have a greater rate of delayed medical consultation, which may impact the reporting of female cases. Additionally, a review by Victoria et al.35 found that gender disparities in incidence rates may vary by region due to differences in lifestyle, socioeconomic status, norms, and healthcare systems, suggesting that more research is needed.
This study found that income levels and regional economic development were important variables affecting the transmission of tuberculosis among students. Previous studies, such as the one by Li et al.36,37, utilized GeoDetector to analyze the relationship between diseases like COVID-19 and bacillary dysentery with socioeconomic factors, finding that socioeconomic factors are closely related to disease occurrence. Similarly, Li Wang38 examined the association between socioeconomic characteristics and the incidence of tuberculosis in the elderly using GeoDetector, and her findings were in line with our results. It is universally acknowledged that a high level of economy can facilitate the control of diseases. Previous studies also indicated that per capita GDP was significantly associated with TB incidence at the country or provincial level39,40,41. Socioeconomic behavior, which depends on factors such as economic development and sanitary conditions, significantly influences disease transmission and incidence. Meanwhile, low income may increase TB transmission rates through a direct interaction with poor living conditions and inadequate nutrition. In this study, the per capita disposable income of urban residents was a significant predictor of regional-level variation in student TB incidence, with urban income levels having a greater influence on incidence than rural income levels. Thus, in Jilin Province, variations of student TB incidence were associated with unbalanced regional economic development.
Remarkably, in this study, the population density of education stages (middle and high school) was significantly associated with TB incidence among students, and it was more powerful than the total population on TB incidence. Some previous studies reported a high TB incidence in areas of high population density40,42, which denoted the population density calculated by total population. However, our study quantified the impacts of subgroups of the total population. Schools are distinct agglomeration areas for disease transmission. Thus, TB incidence in these areas were high in our study.
We should evaluate some existing norms and measures that lack scientific basis from the perspective of professional and empathy, so that school TB prevention and control measures and regulations are more scientific, more humane, and more acceptable to students, parents and schools, so as to alleviate the contradiction between administrators and the managed, and make school TB prevention and control work more scientific and orderly.
It is plausible that a number of limitations could have influenced the results obtained. Limitations highlight the difficulty of collecting data on the incidence of TB of students in various regions of China, so the extrapolation of the results is limited. Another possible source of error is when analyzed only ecological characteristics and not individual characteristics and their risk factors. Furthermore, we did not use alternative spatial analysis techniques to evaluate the relationship between tuberculosis incidence and sociodemographic variables, such as the Integrated nested Laplace approximations (INLA) and conditional autoregressive regression (CAR) regression. Additionally, the impact of COVID-19 was not considered in this study.
Methods
Study design and area
Jilin Province is located in the northeast of China with 8 prefectures and 1 autonomous prefecture (Fig. 1). In recent years, Jilin Province has steadily expanded expenditure in tuberculosis prevention and control, implementing a variety of measures. Nonetheless, the PTB epidemic remains serious. For example, from 2018 to 2020, Jilin Province's overall drug resistance rate (36.80%) was greater than the national average, with a varied and complicated spectrum of drug resistance.
Joinpoint regression analysis was used to explore the trend of increasing or decreasing incidence of TB in students over time. Spatial analysis was applied to identify spatial distribution characteristics of TB incidence during 2008–2018 in Jilin province from quantitative level. Geodetector was used to analyze the social-economic factors affecting the student TB incidence.
Population, case definition and inclusion criteria
This ecological study used data on the number of students TB patients grouped according to sex and within an educated-year-difference (age groups from 6 to 31 years old) from China National Notifiable Disease Surveillance System (NNDSS). Data collection was carried out in 10 prefecture-level regions and 60 county-level regions of Jilin Province, and the detailed names were in Table S4, respectively.
The data collected for all study units are from January 1, 2008 to December 31, 2018. The terms of education levels used in this study are defined below. China’s 9-year compulsory education for all citizens includes (a) primary school (aged 6–11 years) and (b) middle school (aged 12–14 years); Then a student enters (c) high school (aged 15–17 years) and then d) university (aged 18–21 years) as well as (e) advanced educational institutions (aged 22–31 years). The PTB cases are classified as follows, “pathogen positive (including sputum smear positive and only sputum culture positive PTB)”, “pathogen negative (including sputum smear negative PTB)”, “rifampicin resistant”, “no pathogenic findings (including without sputum PTB and tuberculous pleurisy”43. The rifampicin-resistant category was officially reported in 2019 and comprises only a small portion of the collected data (< 5%). Therefore, to maintain consistency in the overall data, we excluded these cases from our analysis. Population information was obtained from the permanent population data of the National Bureau of Statistics.
Variables and data sources
The indicators related to economic, social, medical and ecological environment dimensions as the independent variables Xi (Table S1). All the data were available from Jilin Provincial Bureau of Statistics (http://tjj.jl.gov.cn/tjsj/tjnj/).
Data processing and analysis
Descriptive statistics were used for quantitative data analysis across study areas and in order to compare patients classified by gender and education levels. The epidemiological and operational indicators analyzed in this study were the annual incidence rates, gender, age group (classified as more than 6 years and less than 31 years by education levels).
Data were stored in Microsoft Excel spreadsheets (Windows version 2019, Microsoft Corporation; Redmond, WA, EUA). All analyses were conducted using SPSS for Windows (version 17, SPSS Inc, Chicago, IL, USA). All statistical tests were two-sided, and P-values less than 0.05 were considered statistically significant.
Joinpoint regression models
We used the Joinpoint Regression Program (Statistical Methodology and Applications Branch, Surveillance Research Program of the National Cancer Institute, Bethesda, MD, EUA, June 2017, Version 4.5.0.1) to calculate the temporal trends of TB frequency of cases recorded with a model based on the assumption of a minimum number of points (Joinpoint). The annual percentage change (APC) was used to quantify the time trend of TB incidence rates (Eq. 1)44,45. APC assumes that the annual incidence change is continuously stable throughout the observed period, according to the same percentage as the previous year for log-linear change to describe the trend of incidence over time, is a common indicator for the evaluation of the temporal trend of incidence. In this analysis for calculating APC, the response variable was the natural logarithm of the incidence rate, and the independent variable was the year. The Bayesian information criterion (BIC) was used to select the model with the best fit. Once a joinpoint was determined, the annual percentage changes and 95% confidence intervals (CIs) of each period (segment) was determined. The APC is calculated as follows, where θ is the regression coefficient; APC of 100*(1 − δ)% confidence interval is calculated as above, where α is the degree of freedom, s is the standard error of the regression coefficient θ, and \({t}_{{\upalpha }}^{-1}\left(q\right)\) is the q percentile of the t distribution with degree of freedom α.
Spatial analysis
Spatial auto-correlation analysis was used to examine the spatial heterogeneity. Here, we used three auto-correlation statistics for the outcome indicators46,47.
(1) First, The Global Moran’s I was employed to investigate whether the distribution follows a random pattern or conforms to specified spatial arrangements. The global Moran's I value ranges from − 1 to + 1, with values near to zero indicating geographic randomness, 0 to + 1 indicating positive spatial autocorrelation, and -1 to 0 indicating negative spatial autocorrelation. A significance level of 5% is used.
(2) Then the local indicators of spatial association (LISA), which indicate the influence of individual locations on the magnitude of the global statistic and the locations and types of clusters48. There are four possible scenarios: high-high clustering (A surrounded by areas with high incidence rates), low-low clustering (A surrounded by areas with low incidence rates), high-low clustering (A is a high-incidence area surrounded by low-incidence areas), and low–high clustering (A is a low-incidence area surrounded by high-incidence areas).
(3) Last, the local G statistics, which is also called hotspot analysis. When the calculated Z-score is high and positive, it indicates the presence of high-value clusters or hotspots, and conversely, it indicates the presence of low-value clusters or cold spots.
The spatial weights were created using the rook contiguity rule, and applied to describe the spatial relationships among provinces. ArcGIS version 10.2 (ESRI, Redlands, CA, USA) was used to perform the spatial auto-correlation analysis and to plot the maps. The following equations are for three auto-correlation statistics.
where, n represents the number of study objects, xi and xj are observed values of study units i and j, \(\overline{x }\) is the average of xi, Wij is a spatial weight matrix, and s is the standard deviation of the incidence rate over the overall region.
Geodetector
The core idea of the Geodetector(GD) assumes that if an independent variable has a significant influence on a dependent variable49, the spatial distribution of the independent and dependent variables should be similar50. GD offers 4 functions of factor detection, interaction detection, risk detection, and ecology detection. In this paper, two functions of GD are used to study the spatial differentiation of TB in China cities and its driving mechanisms, where the variables are the number of patients per 100,000 people.
Factor detection enables the analysis of the influence of the independent variable Xi on the dependent variable Yi. The value of q, in a range of [0, 1], is used to represent the strength of influence, and a larger value implies a greater influence. With h representing the number of strata or classifications of the independent variables, Nh and N representing the number of cities in stratum h and the study area, σh2 and σ2 representing the variance of the dependent variable in stratum h and the study area, respectively, SSW representing the Within Sum of Squares, and SST representing the Total Sum of Squares in the study area, the calculation equation for q is:
The occurrence of disease is a comprehensive process. Different influencing factors may have synergistic or antagonistic effects on the impact of disease. The interaction between the two factors will weaken or enhance the impact of a single factor on the disease. Interaction detection calculates the q value q(x, y) when the spatial distribution of the two influencing factors is superimposed, and compares q(x), q(y) and q(x, y) to determine the type of interaction (Fig. S6).
Conclusion
Understanding the spatial, temporal and demographical dynamics of TB can allow for improved targeting of strategies for disease prevention and control. High-risk zones were located mainly in urban centers, far from rural areas. Students in university and high school have a higher incidence than those in other education stages. The study identified the risk of TB incidence among students at different educational levels, as well as important factors such as education stages, medical conditions and the economic development level, and these factors had a non-linear interactive effect on student TB incidence. This study can help health planning by refining the focus of attention to student TB control.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TB:
-
Tuberculosis
- JPR:
-
Joinpoint regression method
- APC:
-
Annual percent change
- Mtb:
-
Mycobacterium tuberculosis
- GD:
-
Geodetector
- CC:
-
Changchun
- JL:
-
Jilin
- TH:
-
Tonghua
- BS:
-
Baishan
- LY:
-
Liaoyuan
- SP:
-
Siping
- BC:
-
Baicheng
- SY:
-
Songyuan
- YB:
-
Yanbian Korean Autonomous Prefecture
- NNDSS:
-
National notifiable disease surveillance system
- PTB:
-
Pulmonary tuberculosis
- BIC:
-
Bayesian information criterion
- CI:
-
Confidence interval
- LISA:
-
Local indicators of spatial association
- BCG:
-
Bacillus Calmette–Guérin
- AIDS:
-
Acquired immune deficiency syndrome
- LA:
-
Land area
- PDIR:
-
Per capita disposable income of rural residents
- PDIU:
-
Per capita disposable income of urban residents
- GDP:
-
Gross Domestic Product
- PGDP:
-
GDP per capita
- NHI:
-
Number of health institutions
- NHT:
-
Number of health technicians per unit population
- NB:
-
Number of beds in health care facilities
- NPR:
-
Number of permanent residents
- NPP:
-
Number of primary school populations
- NMP:
-
Number of middle school populations
- NHP:
-
Number of high school populations
- NUP:
-
Number of undergraduate populations
- NGP:
-
Number of post-graduate populations
References
Chinese Centre for Disease Control and Prevention. Core messages for TB control, <https://www.chinacdc.cn/jkzt/crb/zl/jhb/xgsp/202205/t20220526_259414.html> (2022).
Yu, H. et al. Whole-genome sequencing and epidemiological analysis of a tuberculosis outbreak in a high school of southern China. Infect. Genet. Evol. 83, 104343 (2020).
You NN, Liu Q, Li ZQ & Yang HT. Forecast of tuberculosis incidence in different regions of Jiangsu Province based on ARIMA model. J. Nanjing Med. Univ. Nat. Sci. 40, 909–914, 916 (2020).
Rahevar, K. et al. Tuberculosis outbreaks in schools: Experiences from the Western Pacific Region. West. Pac. Surveill. Response J 12, 1 (2021).
Xia, Y.-Y., Ma, Y., Chen, W. & Cheng, S.-M. Epidemic features of pulmonary tuberculosis in students in China: Data mining based on national disease surveillance system. Chin. J. Antituberc. 35, 871 (2013).
Du, X. et al. Characteristics analysis of national student reported incidence of tuberculosis, 2004–2008. Chin. J. Health Educ. 25, 803–810 (2009).
Chen, W., Chen, Q.-L., Xia, Y.-Y. & Cheng, S.-M. Analysis of the characteristics of national TB epidemic situation in schools from 2008 to 2012. Chin. J. Antituberc. 35, 948 (2013).
Tibebu, H. & Hebo, H. J. The proportion of student tuberculosis cases and treatment outcome at Jimma University Medical Center: 5-Year Retrospective Study (11 Sep. 2010–10 Sep. 2015). Tuberc. Res. Treat. 2019, 4597154. https://doi.org/10.1155/2019/4597154 (2019).
Blumenfeld, A., Rubinstein, F., Mancini, P. & Knopoff, E. G. Prevalence of latent tuberculosis infection and incidence of tuberculin conversion among school contacts older than 5 years in the City of Buenos Aires. Archivos Argentinos de Pediatria, e202202813-e202202813 (2023).
Karla, J. et al. Incidencia de infección tuberculosa latente en un estudio de contactos escolares comparando dos puntos de corte de la prueba de tuberculina (2020).
Wang, L. & Wang, W. Temporal trends in notification and mortality of tuberculosis in China, 2004–2019: A joinpoint and age–period–cohort analysis. Int. J. Environ. Res. Public Health 18, 5607 (2021).
Santos, B. A. et al. Tuberculosis among children and adolescents: an epidemiological and spatial analysis in the state of Sergipe, Brazil, 2001–2017. (2020).
Dhamnetiya, D. et al. Trends in incidence and mortality of tuberculosis in India over past three decades: A joinpoint and age–period–cohort analysis. BMC Pulm. Med. 21, 1–14 (2021).
Lin, Y. et al. Transmission of Mycobacterium tuberculosis in schools: A molecular epidemiological study using whole-genome sequencing in Guangzhou, China. Front. Public Health 11, 1156930 (2023).
Ma, B. Z. et al. Analysis of tuberculosis epidemic among school students in Qinghai Province from 2011 to 2017. Chin. J. School Health 40, 141–143. https://doi.org/10.16835/j.cnki.1000-9817.2019.01.040 (2019).
Chakaya, J. et al. Global Tuberculosis Report 2020–Reflections on the Global TB burden, treatment and prevention efforts. Int. J. Infect. Dis. 113, S7–S12. https://doi.org/10.1016/j.ijid.2021.02.107 (2021).
Qian, G. A. O. & Jian, M. Reflections on the prevention and control of tuberculosis among Chinese students. Chin. J. Antituberc. 42, 195–199. https://doi.org/10.3969/j.issn.1000-6621.2020.03.003 (2020).
Chen, H., Xia, Y. Y., Zhang, C. Y., Cheng, J. & Hui, Z. Epidemic trends and characteristics of pulmonary tuberculosis in students in China from 2014 to 2018. Chin. J. Antituberc. 41, 662–668 (2019).
Li, X.-X. et al. Spatial variations of pulmonary tuberculosis prevalence co-impacted by socio-economic and geographic factors in People’s Republic of China, 2010. BMC Public Health 14, 1–12 (2014).
Vassall, A. et al. Cost-effectiveness of Xpert MTB/RIF for tuberculosis diagnosis in South Africa: a real-world cost analysis and economic evaluation. Lancet Glob. Health 5, e710–e719 (2017).
Newman, L., Baum, F., Javanparast, S., O'Rourke, K. & Carlon, L. Addressing social determinants of health inequities through settings: a rapid review. Health promotion international 30, ii126-ii143 (2015).
Reid, M. J. A. et al. Building a tuberculosis-free world: The Lancet Commission on tuberculosis. The Lancet 393, 1331–1384. https://doi.org/10.1016/S0140-6736(19)30024-8 (2019).
Bao, H. et al. Tuberculosis outbreaks among students in mainland China: A systematic review and meta-analysis. BMC infectious diseases 19, 1–12 (2019).
Zhang, W. Vaccination coverage in China from 1990 to 2019, by vaccine. , <https://www.statista.com/statistics/943957/china-vaccination-coverage-by-vaccine/ > (2023).
Weir, R. E. et al. Persistence of the immune response induced by BCG vaccination. BMC Infect. Dis. 8, 9. https://doi.org/10.1186/1471-2334-8-9 (2008).
Stensballe, L. G. et al. Acute lower respiratory tract infections and respiratory syncytial virus in infants in Guinea-Bissau: A beneficial effect of BCG vaccination for girls: Community based case–control study. Vaccine 23, 1251–1257 (2005).
Shann, F. The non-specific effects of vaccines. Arch. Dis. Child. 95, 662–667 (2010).
Zhang, S., Li, X., Zhang, T., Fan, Y. & Li, Y. The experiences of high school students with pulmonary tuberculosis in China: A qualitative study. BMC Infect. Dis. 16, 758. https://doi.org/10.1186/s12879-016-2077-y (2016).
Zhang, S. R. et al. The experience of college students with pulmonary tuberculosis in Shaanxi, China: A qualitative study. BMC Infect. Dis. 10, 174. https://doi.org/10.1186/1471-2334-10-174 (2010).
Odongo, D. O., Wakhungu, W. & Stanley, O. Causes of variability in prevalence rates of communicable diseases among secondary school Students in Kisumu County, Kenya. J. Public Health 25, 161–166 (2017).
Xiao, X. et al. Analysis of the epidemiological characteristics of tuberculosis students in Shanghai from 2009 to 2017. Chin. J. Antituberc. 42, 498–502 (2020).
Ma, X. X. et al. Epidemiological characteristics of pulmonary tuberculosis in schools in Guizhou, 2011–2019. Dis. Surveill. 36, 1133–1137 (2021).
Liu, Z. Q., Wu, Y. H., Zhang, Y. M. & Zeng, T. X. Current situation of KAP of tuberculosis prevention and control and analysis of influencing factors in two universities students in Baiyin city. Bull. Dis. Control Prev. 39, 30–34. https://doi.org/10.13215/j.cnki.jbyfkztb.2310007 (2024).
Xiao, Y., Xia, Y., Li, Y. K., Xiong, Y. & Xia, L. Epidemiological characteristics and treatment delay of pulmonary tuberculosis in schools in Sichuan Province from 2012 to 2021. J. Prev. Med. Inf. 40, 622–629. https://doi.org/10.19971/j.cnki.1006-4028.240033 (2024).
Peer, V., Schwartz, N. & Green, M. S. Gender differences in tuberculosis incidence rates—A pooled analysis of data from seven high-income countries by age group and time period. Front. Public Health 10, 997025 (2023).
Li, W., Zhang, P., Zhao, K. & Zhao, S. The geographical distribution and influencing factors of COVID-19 in China. Trop. Med. Infect. Dis. 7, 45 (2022).
Wang, X., Zhang, Y. & Ma, J. Factors influencing the incidence of bacterial dysentery in parts of southwest China, using data from the geodetector. Zhonghua Liuxingbingxue Zazhi 40, 953–959 (2019).
Wang, L. et al. Spatio-temporal variation in tuberculosis incidence and risk factors for the disease in a region of unbalanced socio-economic development. BMC Public Health 21, 1–11 (2021).
Ren, H., Lu, W., Li, X. & Shen, H. Specific urban units identified in tuberculosis epidemic using a geographical detector in Guangzhou, China. Infect. Dis. Poverty 11, 44. https://doi.org/10.1186/s40249-022-00967-z (2022).
Wang, Q. et al. Spatial distribution of tuberculosis and its socioeconomic influencing factors in mainland China 2013–2016. Trop. Med. Int. Health 24, 1104–1113 (2019).
Wubuli, A. et al. Socio-demographic predictors and distribution of pulmonary tuberculosis (TB) in Xinjiang, China: A spatial analysis. PLoS ONE 10, e0144010 (2015).
Liu, Y. et al. Investigation of space-time clusters and geospatial hot spots for the occurrence of tuberculosis in Beijing. Int. J. Tuberc Lung Dis. 16, 486–491. https://doi.org/10.5588/ijtld.11.0255 (2012).
National Health and Wellness Commission of the People’s Republic of China, National Health and Wellness Commission General Office on adjusting the classification of tuberculosis infectious disease reporting, National Health Office Disease Control Letter (2019) 296. <http://www.nhc.gov.cn/jkj/s3589/201903/d779ae48db6446c28d1f5371ef09f5ab.shtml> (2019).
Wu, Q.-J., Li, L.-L., Li, J., Zhou, C. & Huang, Y.-H. Time trends of neonatal mortality by causes of death in Shenyang, 1997–2014. Oncotarget 7, 16610 (2016).
Zeng, S. Q. Joinpoint regression models and their application to the analysis of epidemiological trends in infectious diseases. Chin. J. Health Stat. 36, 787–791 (2019).
Wang, H., Chen, Z. & Zhang, P. Spatial autocorrelation and temporal convergence of PM(2.5) concentrations in Chinese cities. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph192113942 (2022).
ArcGlS Pro. Global Moran’s I. <https://pro.arcgis.com/zh-cn/pro-app/latest/tool-reference/spatial-statistics/spatial-autocorrelation.htm. > (2023).
Chakaya, J. et al. The WHO Global Tuberculosis 2021 Report – not so good news and turning the tide back to End TB. Int. J. Infect. Dis. https://doi.org/10.1016/j.ijid.2022.03.011 (2021).
Wang, J.-F., Zhang, T.-L. & Fu, B.-J. A measure of spatial stratified heterogeneity. Ecol. Indic. 67, 250–256 (2016).
Xu, C. Spatio-temporal pattern and risk factor analysis of hand, foot and mouth disease associated with under-five morbidity in the Beijing-Tianjin-Hebei Region of China. Int. J. Environ. Res. Public Health 1, 4. https://doi.org/10.3390/ijerph14040416 (2017).
Funding
This study was supported by Self-supporting Program of Guangzhou Laboratory (Grant No. SRPG22-007) and Major Project of Guangzhou National Laboratory (Grant No. GZNL2024A01004). The funder had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
SY, YP, QC, QL, JW, JR, YG, LG, QZ, RF, MX, DP, and TC had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. SY, DP, and TC were responsible for study conception and design. JW, LG, MX, and QZ collected the data. SY, JW, JR and YG were responsible for data analysis and interpretation. SY, YP, QC and QL drafted the manuscript. DP and TC critically revised the manuscript for intellectual content. SY, YP, QC and QL contributed equally to this study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the institutional ethics committee of the Jilin Provincial Center for Disease Control and Prevention, Jilin, China. Consent requirement, either verbal or written, was waived by the institutional ethics committee of the Jilin Provincial Center for Disease Control and Prevention on the following grounds: (1) only anonymized records were used without the need for direct involvement nor active participation of patients; (2) neither medical intervention nor biological samples were involved; (3) study procedures and results would not affect clinical management of patients in any form. We confirm that all analyses were performed in accordance with relevant guidelines and regulations. This study utilized data from the statutory infectious disease surveillance system, which does not contain any personally identifiable or sensitive information. The research adheres strictly to data privacy protection principles, ensuring that the privacy rights of individuals are fully respected. Given the nature of the data used, this study was granted an ethical exemption.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yu, S., Pan, Y., Chen, Q. et al. Analysis of the epidemiological characteristics and influencing factors of tuberculosis among students in a large province of China, 2008–2018. Sci Rep 14, 20472 (2024). https://doi.org/10.1038/s41598-024-71720-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71720-9
Keywords
This article is cited by
-
Transmissibility and control of tuberculosis in school outbreaks: a modeling study based on four outbreaks in China
BMC Infectious Diseases (2024)