Abstract
A mismatch in footprints of cervical total disc arthroplasty (CTDA) implants occasionally occurred in Asian population and it had been attributed solely to ethnic factor. Yet, cervical degeneration process may play a role. Our purpose was to compare the cervical vertebra morphometric data with and without degeneration. The study included patients with CT scans of cervical spine from our hospital between January, 2019, and September, 2021. The total cervical degenerative index (TCDI) of each patient were collected by adding CDI score for 5 disc-levels. Patients were categorized into normal (TCDI 0–5) and degeneration groups (TCDI 6–60). Various measurements of the C3–C7 vertebral body and endplate were taken. Forty-nine patients in the normal group and 55 in the degeneration group were included. No significant difference was noted in gender, BH, BW, or BMI except age and TCDI (p < .001). During degeneration, disproportional endplate size changes were observed, with an increment ratio of 12–20% in the anteroposterior and 5–17% in the mediolateral plane throughout C3–C7, while vertebral body height remained constant. In conclusion, degeneration process, besides ethnic factor, causes the endplate size and shape mismatch. This information can help spine surgeon choose appropriate implants in CTDA surgery.
Similar content being viewed by others
In individuals aged over 50 years, intervertebral disc degeneration affects more than 90% of both men and women, with nearly half of the cases involving cervical disc degeneration1. Treatment options include nonoperative measures and surgical interventions such as laminectomy, foraminotomy, and total disc arthroplasty. Disc replacement or arthroplasty has been suggested to preserve the motion of the cervical spine and prevent adjacent-level degenerative disease related to cervical fusion2. During cervical total disc arthroplasty (CTDA) surgery, discectomy is performed, and cartilage attached to the bony endplates, posterior osteophytes, thickened posterior longitudinal ligament, and anterior osteophytes are removed. Surgeons confirm the height of the disc space and determine the appropriate implant size during the surgery3,4. However, challenges may arise in inserting the artificial disc implant due to a shape or size mismatch occasionally5. This may necessitate the removal of additional bony structures, potentially affecting the trabecular bone structure of the vertebral body, the mechanical properties, and kinetic movement of the cervical spine6, resulting in implant subsidence and migration7.
Undoubtedly, understanding the morphology of the cervical spine is essential for improving preoperative planning and optimizing surgical outcomes. Studies have investigated the geometric characteristics of the vertebral body and endplate of the cervical spine, using both cadaver skeletons8,9 and computed tomography (CT)-derived three-dimentional (3D) models10,11,12,13,14,15. Differences in the size of endplates have been pointed out to occur mostly between Asian and Western populations5,16,17. In one study, Wang et al. discovered a notable gap in cervical anatomical data between Chinese patients and the dimensions of the prostheses commonly used5. Yet, the mismatch in footprints has been attributed solely to ethnic factors, without considering cervical spinal degeneration12,13,14,15.
We hypothesize that despite ethnic differences, degenerative changes have an impact on cervical endplate geometry. This study aims to assess a comprehensive morphometric database of the cervical vertebral bodies and endplates of the subaxial cervical spine using 3D-reconstructed CT images of the Asian population with varying degrees of degeneration.
Materials and methods
Data collection
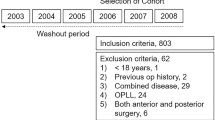
This retrospective study collected Digital Imaging and Communications in Medicine (DICOM) files of CT scans of the cervical spine, head and neck, or paranasal sinus from January 1, 2019, to September 30, 2021, after internal review board (IRB) approval from our institute. All research was performed in accordance with relevant guidelines and regulations, and the IRB approves the waiver of the participants' consent. The inclusion criteria were 1.Slice thickness of 1.0 mm; and 2.Good pixel resolution around the region of interest in the cervical spine. A total of 249 consecutive CT scans was initially collected. Of these, 130 CT scans meeting the inclusion criteria were reviewed. The study excluded following CT scans: those not including the whole cervical spine, repeated scans of an individual at different time points, and CT scans of foreign patients. After exclusion, 104 CT scans were further reviewed and included in this study (Fig. 1). Clinical parameters such as age, gender, body height (BH), body weight (BW), and body mass index (BMI) were also collected.
3D reconstruction of cervical vertebral models
To generate the 3D-reconstructed models of the CT cervical spinal structure and calculate specific geometric parameters, the raw CT data from DICOM files were sent to a partner institution for processing. The cervical vertebral models were reconstructed and segmented three-dimensionally using Materialize Mimics software version 23 (Materialise NV, Leuven, Belgium)18. The X, Y, and Z axes of each 3D-reconstructed model were determined using the minimum bounding box (MBB) algorithm19 in Materialize Magic software version 26 (Materialise NV, Leuven, Belgium). This algorithm creates a rectangular box, with each side parallel to the X, Y, and Z axes, to minimally enclose the 3D-reconstructed CT cervical spine. Subsequently, individual aspects of the vertebral models were captured, and measurements of the captured images were taken using ImageJ software20. The schematic flow chart of the 3D model reconstruction process is presented in Fig. 2.
Definition of each parameter
Nine linear parameters of the cervical vertebral bodies (C3 to C7) were measured following procedures detailed in other studies8,10. These measurements included 4 parameters of the superior vertebral body, 2 of the inferior vertebral body, and 3 distinct measurements of the vertebral body height. All linear measurements were recorded in millimeters, and the definitions and illustrations of each parameter are provided in Fig. 3 and Table 1.
Illustration and definition of vertebral body measurements from Table 1 the normal and degeneration groups.
The parameters were further categorized into 3 groups:
-
Coronal (mediolateral) parameters, including superior vertebral body length (SVBL), superior vertebral internal length (SVIL), and inferior vertebral body length (IVBL);
-
Sagittal (anteroposterior) parameters, including superior vertebral body depth (SVBD), superior vertebral internal depth (SVID), and inferior vertebral body depth (IVBD); and
-
Height parameters, including anterior vertebral body height (CVH1), posterior vertebral body height (CVH2), and central vertebral body height (CVH3) (Table 1).
Definition of degenerative status
The degenerative status of the cervical spine CT images was rated using the cervical degenerative index (CDI), a quantitative radiographic scoring system for cervical spondylosis developed by Ofiram et al.21. It consists of four factors: disc space narrowing, endplate sclerosis, osteophyte formation, and olisthesis. Each of the four factors was individually assessed for each disc level from C2 to C7, with a quantitative score assigned ranging from 0 to 3 for each factor. The total CDI (TCDI) score for each patient was collected by adding the CDI scores (ranging from 0 to 12) for five disc levels, resulting in a possible TCDI score between 0 and 60. All imaging studies were blinded and reviewed by a third-party radiologist (C.L.F). Based on the TCDI score, the dataset was further classified into two groups:
-
Patients with an overall TCDI score of 5 or less were considered normal.
-
Those with an overall TCDI score of more than 6 were considered to have degenerative changes.
Statistical analysis
Data were analyzed using SPSS software version 27.0 (SPSS Inc., Chicago, Illinois). Descriptive data are presented as means and SDs. Student's t-tests were used to compare continuous variables between the two groups that were continuous, normally distributed, and homoscedastic. Chi-square tests and Fisher's exact tests were applied to evaluate differences between the two groups in other categorical variables. Differences during the postoperative follow-up period in both groups were analyzed by one-way variance analysis. A P-value of less than 0.05 was considered statistically significant. The intraclass correlation coefficients (ICCs) for both the reconstruction and measurement of the 3D cervical models were calculated, and their 95% confidence intervals were used to summarize the intertester reliability of the radiographic measurements. These were calculated using a 2-way random-effects model, assuming a single measurement and absolute agreement. For intratester reliability for each reconstruction, one author (C.W.T) reconstructed the same vertebral model 3 times, with intervals of 3–5 days between reconstructions. Moreover, to construct a reliable 3D reconstruction model, we verified our reconstruction method. Three authors (M.Y.L, T.T.T, and C.W.T) independently reconstructed the same 1-mm cut 3D CT image, and 3 reconstruction results were measured by one blinded author (C.J.F).
Results
A total of 104 CT scans were reviewed, comprising 79% paranasal sinus CT scans and 21% head and neck CT scans. The average age of the patients was 45.9 years (range 18–85 years), with 51.0% being women. The average body height (BH) was 162.8 cm, and the mean BMI was 23.7 kg/m2. The CT scans were conducted for various indications, including chronic rhinosinusitis (63%), foreign body in the esophagus (12%), nasal polyps or septal deviation (8%), cancer of head and neck structures (6%), trauma to neck structures (4%), cervical spine ossification of the posterior longitudinal ligament (OPLL) (1%), cervical disc herniation (CDH) (1%), and anatomy surveys for various reasons, including neck lymph nodes, sleep disturbance, maxillary headache, and skull base infection (6%). It is noteworthy that most of the pathologies listed above did not bear any relevance to or contribute to the intended objective of collecting CDI data, except for OPLL and CDH, classified into the degenerative group. The patients were categorized into two groups, with 49 in the normal group and 55 in the degeneration group.
-
In the normal group, 22 patients (45%) were women, with a mean age of 31.8 years, a mean total CDI score of 1.0, a mean BH of 164.0 cm and a mean BMI of 22.9 kg/m2;
-
In the degeneration group, 31 patients (56%) were women, with a mean age of 58.6 years, a mean total CDI score of 10.8, a mean BH of 161.7 cm, and a mean BMI of 24.5 kg/m2
A significant difference in age and TCDI score was found between the groups (P < 0.001). However, no significant differences were found in gender, CT scan data sources, CT indications, BH, BW, and BMI (Table 2).
The accuracy of 3D reconstruction model was validated. Table 3 illustrates the intratester and intertester reliability of the measurement of cervical parameters, showing excellent reliability. The 3D reconstruction model using the MBB method was found to be reproducible and reliable.
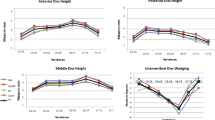
Data for measurements of vertebral body parameters in the subaxial cervical spine are categorized by gender and further divided into endplate width, depth, and vertebral height parameters (Fig. 4A–C). Generally, men had significantly larger cervical vertebral bodies than women across almost all parameters from C3 to C7 (P < 0.05). Additionally, coronal parameters (SVBL, SVIL, and IVBL) increased linearly from C3–C7, without gender differences. Conversely, sagittal endplate parameters (SVBD, SVID, and IVBD) increased, peaking at C6, and then slightly decreased from C6 to C7. The trend in vertebral body height varied, with height parameters slightly decreasing from C3–C5 or C6 and then increasing, with C7 height almost the same or slightly higher than C3. This trend from C3–C7 remained consistent across both the normal and degeneration groups.
The degeneration change is defined as the ratio of the average value of each parameter between the normal group and the degeneration group (Table 4 and Fig. 5A–E). The cervical vertebrae elongated significantly in the sagittal plane by 12–20% as a result of degeneration, as seen in SVBD, SVID, and IVBD. On the other hand, the cervical vertebrae became wider in the coronal plane by 5–17%, with the most prominent changes occurring at C5 and C6. As a result, the endplate surface becomes oval with sagittal-located long axis. Additionally, vertebral body height parameters remained relatively stable during degenerative changes, with a nonsignificant decrease observed in CVH3.
Discussion
The current study is the first to report on the degeneration process causing disproportionate increases in size in both the sagittal and coronal planes among the Asian population. General practice has already established that CTDA can preserve motion in the cervical spine and prevent adjacent-level degenerative disease related to cervical fusion16,22. Although the mismatch in size and shape of CTDA has been exclusively asserted in Asian populations12,13,14,15, it appears that ethnic factors alone may not be the sole cause of such differences. In our population, we observed similar disproportional size changes with degeneration, with an increment ratio of 12–20% anteroposteriorly and 5–17% mediolaterally, especially at C5 and C6. Wang et al.5 found significant width changes with aging at C5/C6 and C6/C7 by comparing age groups of < 35 to 35–49. Ezra et al.8,9 reported that changes in size due to degeneration mostly occurred at the anterior and lateral aspects of the vertebral bodies and annular epiphyses, with changes in length dimensions being more pronounced than those in width dimensions. These findings supported the size changes due to the degenerative factor. Additionally, the shape of the endplates may change correspondingly, including a reduction in curvature with aging, resulting from alterations in the concavity and surface area of the annular epiphyses, as reported in studies involving various populations9,15,23. The observed change in endplate shape is supported by our findings, which indicate that the changes in linear parameters of the annular epiphyses (SVIL and SVID) were consistently more pronounced than those of the endplates (SVBL and SVBD). Overall, these findings demonstrate that the degeneration process itself, rather than ethnic factors alone, can lead to the size and shape mismatches encountered in CTDA surgery.
Ethnic differences
While some studies have claimed differences in endplate size primarily between Asian and Western populations5,16,17, it is evident that certain ethnic discrepancies do exist. In Fig. 6, we compared key parameters for CTDA from the current cohort with those found in Korean11, Chinese15, and American populations8 using exactly the same measurement method24. First, the superior vertebral endplate length (SVIL) was, on average, 2–3 mm larger for the American population8 than for all the Asian groups (Fig. 6A). Second, the two sagittal endplate parameters (SVBD and IVBD) closely aligned with those observed in Korean and Chinese patients (Fig. 6B,C). To be more precise, the vertebral bodies in American populations were wider in the coronal plane but with nearly the same anteroposterior distance compared to Asian cohorts. As several studies12,13,14,15 have found mismatches when performing CTDA surgery in Asian populations, the above findings help to explain the specific distinctness among populations.
Gender and vertebrae differences
The linear parameters were consistently larger in men than in women in our cohort, a finding that aligns with literature across different ethnic groups, including Americans, Chinese, and Koreans5,8,11,17. The current CTDA products on the market have already taken this difference into consideration by offering several available sizes. Furthermore, this concept could also apply to different vertebral levels where CTDA is to be implanted, as the majority of studies have reported linear increments in parameters from C3–C75,8,11,15,17. Nevertheless, Kim et al.11 and Tan et al.25 noted that from C3–C7, the lower endplate depth increased in size but peaked at C6 rather than C7 in Korean and Chinese Singaporean populations. In our cohort, we found more sagittal parameters adhering to this trend, and a possible hypothesis is that degeneration may also play an essential role. Tao et al.26 showed that the earliest degenerative findings appeared first at C5-C6 rather than C6-C7. This likely explains our findings of a more prominent C6 peak in sagittal endplate parameters, especially in the degeneration group. In other words, differences in gender, vertebral level, and degenerative status should all be considered by spine surgeons for ideal surgical planning.
TCDI score
We utilized the total Cervical degenerative Index (TCDI) score instead of age to effectively represent the overall degeneration status. Indeed, the process of degeneration occurs within the intervertebral disc and endplate, leading to disc height loss, osteophyte formation, and endplate sclerosis26. Ofiram et al.21 first introduced the CDI score as a quantitative radiographic scoring system for cervical spondylosis with good interobserver and intraobserver reliability. While others have either used age as the sole factor8,9 or defined "healthy" as the absence of signs of cervical spinal disorder5,13,15,17,27 , we adopted this scoring system for its simplicity, reproducibility, and generality in representing the overall process of degeneration. Some may argue about the cutoff value of 5 for normal and degeneration groups. On one hand, research has found that cervical disc degeneration mostly occurs in a contiguous pattern, with earlier findings including height loss and osteophyte formation26. On the other hand, based on a very similar grading system28, the overall degree of degeneration tends to be slightly underestimated. Consequently, we applied a very strict cutoff value for the normal group and assumed the common presentation of CDI scores of 2–3 in contiguous levels above or below C5-C6 as indicative of degeneration. In our study, the TCDI score not only showed a strong correlation with age but also encompassed details of ongoing changes in the disc and endplate.
How degeneration could be managed during perioperative period of CTDA
Although severe disc degeneration has just been tried to be added to the list of indications for CTDA29,30, there are still technical difficulties in carrying out the procedure. A safe sequence to modulate degeneration31,32 included 1. Appropriate gardening of anterior osteophytes for localization of disc space; 2. To shave along the disc space, use the side of angled curette or limited use of drill burr but not tip of the curette; 3. Balance uncovertebral resection; 4. No excessive posterior endplate decompression. Furthermore, since every implant design has a unique width and depth ratio, a spine surgeon could anticipate the best implant brand and size following endplate preparation prior to the CTDA surgery by paying meticulous attention to the degenerative changes.
Limitations
This study has several limitations. One primary constraint was the inability to accurately represent the exact shape and surface area of the endplate using the current method. While most measurements employed were linear parameters in morphometric analysis of cervical vertebral endplate studies24, surface area measurement would better exhibit the three-dimensional geometry of the cervical endplates. However, it also required specialized software and resulted in more interobserver differences. Second, cervical alignment was not studied. Patients always underwent CT scans in the supine position with a neutral neck alignment. In this retrospective study, with approximately half of the CT scans indicated for chronic rhinosinusitis, there were few lateral cervical spine radiographs of patients in the upright position for studying alignment. Third, since the original datasets of other population studies were not accessible, the lack of statistical comparison might render the above comparison between populations meaningless. Therefore, we provided all the data used in this paper in the “Supplementary Information” for statistical comparison in the future.
Conclusion
The current study compiled a comprehensive database of cervical vertebrae and revealed changes in several parameters of cervical vertebral bodies during degeneration, with the vertebral bodies becoming more elongated than wider. Moreover, ethnic differences in parameters related to CTDA design were noted when comparisons were made with other Asian populations and an American population. The 3D reconstruction data provided valuable insights into the anatomy of the cervical spine as degeneration progressed, laying the foundation for the future development of CTDA implants that are better matched to Asian populations.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Teraguchi, M. et al. Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: The Wakayama Spine Study. Osteoarthrit. Cartil. 22, 104–110. https://doi.org/10.1016/j.joca.2013.10.019 (2014).
Todd, A. G. Cervical spine: Degenerative conditions. Curr. Rev. Musculoskelet. Med. 4, 168–174. https://doi.org/10.1007/s12178-011-9099-2 (2011).
Spetzger, U., Frasca, M. & König, S. A. Surgical planning, manufacturing and implantation of an individualized cervical fusion titanium cage using patient-specific data. Eur. Spine J. 25, 2239–2246. https://doi.org/10.1007/s00586-016-4473-9 (2016).
Leven, D., Meaike, J., Radcliff, K. & Qureshi, S. Cervical disc replacement surgery: Indications, technique, and technical pearls. Curr. Rev. Musculoskelet. Med. 10, 160–169. https://doi.org/10.1007/s12178-017-9398-3 (2017).
Wang, L. et al. Does the sizing of current cervical disc arthroplasty systems match Chinese cervical anatomic dimensions?. Front. Bioeng. Biotechnol. 10, 1036223. https://doi.org/10.3389/fbioe.2022.1036223 (2022).
Smith, L. J., Nerurkar, N. L., Choi, K. S., Harfe, B. D. & Elliott, D. M. Degeneration and regeneration of the intervertebral disc: Lessons from development. Dis. Models Mech. 4, 31–41. https://doi.org/10.1242/dmm.006403 (2011).
Thaler, M. et al. Footprint mismatch in total cervical disc arthroplasty. Eur. Spine J. 22, 759–765. https://doi.org/10.1007/s00586-012-2594-3 (2013).
Ezra, D. et al. Demographic aspects in cervical vertebral bodies’ size and shape (C3–C7): A skeletal study. Spine J. 17, 135–142. https://doi.org/10.1016/j.spinee.2016.08.022 (2017).
Ezra, D. et al. Morphologic aspects of the cervical (C3–C7) annular epiphysis: A skeletal study. Spine J. https://doi.org/10.1016/j.spinee.2023.04.006 (2023).
Decker, S. J., Foley, R., Hazelton, J. M. & Ford, J. M. 3D analysis of computed tomography (CT)-derived lumbar spine models for the estimation of sex. Int. J. Legal Med. 133, 1497–1506. https://doi.org/10.1007/s00414-019-02001-8 (2019).
Kim, M. K. et al. Quantitative anatomy of the endplate of the middle and lower cervical vertebrae in Koreans. Spine 32, E376-381. https://doi.org/10.1097/BRS.0b013e318067e384 (2007).
Chen, H., Zhong, J., Tan, J., Wu, D. & Jiang, D. Sagittal geometry of the middle and lower cervical endplates. Eur. Spine J. 22, 1570–1575. https://doi.org/10.1007/s00586-013-2791-8 (2013).
Lou, J. et al. Geometry of inferior endplates of the cervical spine. Clin. Neurol. Neurosurg. 142, 132–136. https://doi.org/10.1016/j.clineuro.2016.01.027 (2016).
Zhu, Y. H., Cheng, K. L., Zhong, Z., Li, Y. Q. & Zhu, Q. S. Morphologic evaluation of Chinese cervical endplate and uncinate process by three-dimensional computed tomography reconstructions for helping design cervical disc prosthesis. J. Chin. Med. Assoc. 79, 500–506. https://doi.org/10.1016/j.jcma.2016.04.003 (2016).
Feng, H. et al. Quantitative morphometric study of the subaxial cervical vertebrae end plate. Spine J. 17, 269–276. https://doi.org/10.1016/j.spinee.2016.09.019 (2017).
Shin, J. J. et al. Cervical disc arthroplasty: What we know in 2020 and a literature review. J. Orthop. Surg. 29, 23094990211006936. https://doi.org/10.1177/23094990211006934 (2021).
Yao, Q. et al. Differences of the morphology of subaxial cervical spine endplates between Chinese and white men and women. Biomed. Res. Int. 2018, 2854175. https://doi.org/10.1155/2018/2854175 (2018).
Chen, D. et al. Three-dimensional reconstructions in spine and screw trajectory simulation on 3D digital images: A step by step approach by using Mimics software. J. Spine Surg. 3, 650–656. https://doi.org/10.21037/jss.2017.10.09 (2017).
O’Rourke, J. Finding minimal enclosing boxes. Int. J. Comput. Inf. Sci. 14, 183–199. https://doi.org/10.1007/BF00991005 (1985).
Schneider, C. A., Rasband, W. S. & Eliceiri, K. W. NIH Image to ImageJ: 25 years of image analysis. Nat. Methods 9, 671–675. https://doi.org/10.1038/nmeth.2089 (2012).
Ofiram, E. et al. Cervical degenerative index: A new quantitative radiographic scoring system for cervical spondylosis with interobserver and intraobserver reliability testing. J. Orthop. Traumatol. 10, 21–26. https://doi.org/10.1007/s10195-008-0041-3 (2009).
Patwardhan, A. G. & Havey, R. M. Biomechanics of cervical disc arthroplasty: A review of concepts and current technology. Int. J. Spine Surg. 14, 14–28. https://doi.org/10.14444/7087 (2020).
Moore, R. J. The vertebral end-plate: What do we know?. Eur. Spine J. 9, 92–96. https://doi.org/10.1007/s005860050217 (2000).
Liu, W. J. P., Parr, W. C. H., Walsh, W. R. & Mobbs, R. J. Three-dimensional morphometric analysis of cervical vertebral endplate anatomy: A systematic literature review. Interdiscipl. Neurosurg. 27, 101388. https://doi.org/10.1016/j.inat.2021.101388 (2022).
Tan, S. H., Teo, E. C. & Chua, H. C. Quantitative three-dimensional anatomy of cervical, thoracic and lumbar vertebrae of Chinese Singaporeans. Eur. Spine J. 13, 137–146. https://doi.org/10.1007/s00586-003-0586-z (2004).
Tao, Y. et al. Radiographic cervical spine degenerative findings: A study on a large population from age 18 to 97 years. Eur. Spine J. 30, 431–443. https://doi.org/10.1007/s00586-020-06615-0 (2021).
de Assis, R. R., Barbosa, M. N. & Defino, H. L. A. Sagittal plane geometry of cervical, thoracic, and lumbar endplates. Int. J. Spine Surg. 16, 792–799. https://doi.org/10.14444/8336 (2022).
Kettler, A. et al. Validity and interobserver agreement of a new radiographic grading system for intervertebral disc degeneration: Part II. Cervical spine. Eur. Spine J. 15, 732–741. https://doi.org/10.1007/s00586-005-1037-9 (2006).
Wing-Yuk Chan, R., Chiang, Y. H., Yang, Y. A., Chen, Y. Y. & Tsou, Y. S. One-year follow-up study on assessing the range of segmental motion and clinical outcomes following cervical disc arthroplasty for treatment of severe cervical disc degeneration. World Neurosurg. 183, e276–e281. https://doi.org/10.1016/j.wneu.2023.12.079 (2024).
Patel, N. et al. Should patient eligibility criteria for cervical disc arthroplasty (CDA) be expanded? A retrospective cohort analysis of relatively contraindicated patients undergoing CDA. Spine J. 24, 210–218. https://doi.org/10.1016/j.spinee.2023.09.017 (2024).
Luo, C. A. et al. The surgical outcome of multilevel anterior cervical discectomy and fusion in myelopathic elderly and younger patients. Sci. Rep. 12, 4495. https://doi.org/10.1038/s41598-022-08243-8 (2022).
Reinas, R., Kitumba, D., Pereira, L., Baptista, A. M. & Alves, Ó. L. Multilevel cervical arthroplasty—Clinical and radiological outcomes. J. Spine Surg. 6, 233–242 (2020).
Acknowledgements
We thank support by our hospital (Grant CRRPVVM0011 and CRRPVVM0012). The funding body did not have any role in the design of the study, data collection, analysis and interpretation, or in writing the manuscript. We also thank Bone and Joint Research Center of our hospital for devotion to our project and providing statistical consultation.
Author information
Authors and Affiliations
Contributions
C.C.N. did conception and study design. C.A.L. and C.J.F. did acquisition of subjects and/or data. M.Y.L. and C.W.T did analysis and interpretation of data. M.Y.L did drafting and C.A.L did critical revision of the manuscript. T.T.T and C.C.N. had administrative, technical or material support.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study (Ref. No. 202101795B0) was approved by the institutional review board of Chang Gung Medical Foundation, Taiwan and the IRB approved the waiver of the participants' consent.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, MY., Tsai, CW., Niu, CC. et al. The footprint mismatch of cervical disc arthroplasty comes from degenerative factor besides ethnic factor. Sci Rep 14, 20673 (2024). https://doi.org/10.1038/s41598-024-71786-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71786-5