Abstract
Polymer composite scaffolds hold promise in bone tissue engineering due to their biocompatibility, mechanical properties, and reproducibility. Among these materials, polylactic acid (PLA), a biodegradable plastics has gained attention for its processability characteristics. However, a deeper understanding of how PLA scaffold surface properties influence cell behavior is enssential for advancing its applications. In this study, 3D-printed PLA scaffolds containing hydroxyapatite (HA) were analyzed using atomic force microscopy and nanomechanical mapping. The addition of HA significantly increased key surface properties compared to unmodified PLA scaffols. Notably, the HA-modified scaffold demonstrated Gaussian distribution of stiffness and adhesive forces, in contrast to the bimodal properties observed in the unmodified PLA scaffolds. Human adipose-derived mesenchymal stem cell (hADMSC) seeded on the 3D-printed PLA scaffolds blended with 10% HA (P10) exhibited strong attachment. After four weeks, osteogenic differentiation of hADMSCs was detected, with calcium deposition reaching 6.76% ± 0.12. These results suggest that specific ranges of stiffness and adhesive forces of the composite scaffold can support cell attachement, and mineralization. The study highlights that tailoring suface properties of composite scaffolds is crucial for modulating cellular interactions, thus advancing the development of effective bone replacement materials.
Similar content being viewed by others
Introduction
Critical-sized bone defects present significant clinical challenges, necessitating innovative solutions for effective bone regeneration1,2,3. While autografts and allografts are commonly used, they have limitations and potential complications4. This issue has aroused interest in artificial bone grafts due to their unlimited supply and the ability to customize their physical and biological properties5,6,7. Artificial grafts not only offer viable options for bone replacement but also serve as valuable tools for studying osteogenesis and bone formation, including bone models and scaffold-on-a-chip systems8,9.
Additive manufacturing (3D printing) becomes an attractive choice for bone graft fabrication as it effortlessly creates the porous structures necessary for nutrient exchange during cell proliferation and bone formation10,11. Among a wide range of material options, polylactic acid (PLA) is widely recognized for its versatility, durability, functionalization capabilities, biocompatibility, and biodegradability12,13. However, its relatively low toughness has led to efforts aimed at enhancing its ductility. A promising approach involves the rational design of polymer blends to improve properties of PLA14,15,16. In this context, hydroxyapatite (HA) has emerged as a valuable additive, particularly for reinforceing PLA mechanical strength. Incorporating HA into the scaffold introduces two distinct phases that mimic the composition of natural bone. The inorganic (ceramic) phase provides structural support and toughness, while the organic (polymeric) phase enhances integration with surrounding tissues and the vascular system13,16,17.
Despite these advancements, the development of PLA-HA biocomposite materials for promoting cell growth is still in its infancy and the correlation between material surface properties and cellular behavior remains largely uncharted18,19,20. For instance, HA has been reported to enhance cell attachment21,22, but conflicting evidence suggests it may reduce cell proliferation and increase apoptosis23,24. This discrepancy highlights the incomplete understanding of the material properties that are most conducive to cell growth within the scaffold's microenvironment. Moreover, while nanoscale material properties could provide more detailed insights, they are often overlooked due to their complexity and undetectability at the macroscale21,25,26. To comprehend cellular responses to their surrounding environment, pinpointing the material properties at the surface of a sample, cellular level is crucial27,28. Atomic force microscopy (AFM) has emerged as a powerful tool for nanoscale investigations29,30,31. AFM employs a nanometer-sized tip on a cantilever to scan the sample’s surface, measuring parameters like stiffness, adhesion, and phase difference. This technique provides high-spatial-resolution data, allowing precise analysis of both surface morphology and mechanical properties simultaneously32,33,34.
In this study, we investigated the surface nanomechanical properties of 3D-printed PLA-based scaffolds functionalized with hydroxyapatite (HA). We examined scaffolds with two levels of HA addition—10% (P10) and 20% (P20)—as well as a surface-treated sample with HA coating on PLA (PC). AFM-based nanoscale quantitative mapping revealed that the P10 scaffold surface homogeneity in terms of stiffness and adhesion.These unique properties of the P10 scaffold significantly enhanced cell attachment and osteogenic differentiation of human adipose-derived mesenchymal stem cells (hADMSCs). This nanomechanical data-driven approach demonstrates potential for engineering scaffolds that effectively guide hADMSCs towards osteoblasts differentiation, thereby facilitating bone tissue regeneration. The study’s findings pave the way for innovative scaffold designs with the potential to revolutionize artificial bone grafts.
Material and methods
Preparation of PLA and PLA-composite scaffolds
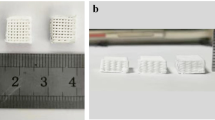
Hydroxyapatite (HA, Sigma-Aldrich, USA) and Poly(lactic acid) (PLA, grade 3051D, Natureworks, USA) pellets were dried at 60 °C for 4 h before mixing. The PLA-HA composites with varying compositions of HA (0, 10, 20%) were blended for 6 min in a laboratory internal mixer (Brabender®, Germany). The relative melting points of the blend were set at 180, 185, and 190 °C. Subsequently, the composites were ground into pellets using a high-speed pelletizer and extruded into filaments (diameter = 1.75 mm) at 160 °C and 40 RPM using a filament maker (Filabot, USA). Fused deposition modeling (FDM) was used to fabricate cylindrical scaffolds with gyroid geometry (D = 10 mm, h = 5 mm) on a Sermoon V1 3D printer (Creality 3D, China). The layer height was set to 0.2 mm. The scaffolds were labeled according to the HA content as PLA, P10, and P20, corresponding to 0, 10, and 20% HA, respectively.
A 1:1 ethanol and 0.25 M NaOH aqueous solution was prepared for alkali treatment and HA coating. The scaffolds were submerged into the solution and subjected to magnetic stirring at 550 RPM for 1 h. Subsequently, the scaffolds were subjected to ultrasonic cleaning with 100% ethanol for 3 min. The 3D-printed PLA scaffolds were coated with the 3% (w/v) HA in 100% ethanol under magnetic stirring at 550 RPM for 2 h. The coated scaffolds were washed multiple times using deionized water until the pH of the solution reached 7.0. The scaffolds were further soaked in pure ethanol and air-dried at room temperature for additional characterization and cell culture experiments. These scaffolds were identified as PC.
Scanning electron microscopy (SEM) and energy dispersive X-ray spectrometry (EDS) analysis
For scaffold with cells, the scaffolds were immersed in 2.5% glutaraldehyde (Loba Chemie, India) and fixed overnight at 4 °C. The scaffolds underwent a 45 min dehydration process using a graded series of ethanol concentrations (30, 50, 70, 95, and 100%). Scaffolds without cells were prepared directly for coating. Then, the scaffolds were sputter-coated with gold using a sputter coater (BALZERS SCD 040, Balzers, Lichtenstein), and analyzed using a scanning electron microscope (JSM-IT300LV, Jeol, Japan) with an accelerating voltage of 10 kV. Furthermore, the chemical composition of the constructs was characterized using energy dispersive spectroscopy (EDS) with the assistance of computer-controlled software (Aztec EDS system, Oxford Instruments, Abingdon, UK).
AFM-based nanomechanical characterization
Nanomechanical properties were assessed using AFM. The scaffold was mounted on a glass slide with double-sided tape and examined on a JPK NanoWizard 3 AFM (Bruker, USA) in quantitative imaging (QI) mode, where the surface morphology and the nanomechanical data were retrieved simultaneously35. The cantilever was a non-contact probe with a spring constant of 37 N/m and a resonance frequency of 300 kHz (ACTA model, AppNano, USA). Force calibration with a thermal tune preceded data collection. Measurements covered ten randomly selected 20 µm × 20 µm surface areas (two areas per scaffold from five scaffolds) at a resolution of 256 × 256 pixels and a force threshold of 100 nN. Stiffness and adhesive force data were analyzed by plotting distribution histograms, with Gaussian or bimodal Gaussian functions used for fitting depending on the distribution. Peak center and standard deviation values were extracted from the fitting, and distribution plots were generated using the Matplotlib library in Python36.
Cultivation of human adipose-derived mesenchymal stem cells (hADMSCs)
Human adipose-derived mesenchymal stem cells (hADMSCs) at the fifth passage obtained from PromoCell (Germany) were used in this study. Briefly, 5 × 105 hADMSCs were seeded onto 3D-printed scaffolds, including PLA, P10, P20, and PC. The cells were cultured in an hMSC growth medium (alpha-MEM supplemented with 4% (v/v) FBS, 1% (v/v) antibiotic–antimycotic, 1% (v/v) HEPES buffer, 1% (v/v) GlutaMAX, and 1 ng/ml bFGF) for seven days and then shifted to an osteogenic medium (DMEM with 4% (v/v) FBS, 1% (v/v) antibiotic–antimycotic, 1% (v/v) HEPES buffer, 10 mM β-glycerolphosphate, 50 μM ascorbic acid, and 10 μM dexamethasone) for 21 days, with 3–4 days medium changes. Cell viability was quantified using PrestoBlue™ (Thermo Fisher Scientific, USA), and live/dead cells were visualized using the live/dead Cell Double Staining kit (Sigma-Aldrich, USA).
Cell viability assay
PrestoBlueTM (Thermo Fisher Scientific, USA) measured cell viability under the manufacturer's instructions. Briefly, the cell-seeded scaffolds were incubated in 1 ml of medium containing 10% (v/v) PrestoBlue™ in hMSC growth medium at 37 °C for an hour in the dark. The fluorescence intensity was measured using a microplate reader at λex 560 and λem 590 nm (Varioskan Flash Multimode, Thermo Scientific, USA).
For live/dead cell viability assay, the cells/scaffold constructs were incubated in live/dead Cell Double Staining kit (Sigma-Aldrich, USA) for 30 min in the dark. The constructs were observed and analyzed using an inverted fluorescence microscope (Nikon Eclipse Ti, USA) to determine live cells (green) and dead cells (red) after 1, 2, and 4 weeks of culture.
Assessment of calcium deposition by alizarin red staining
Alizarin Red S staining, the scaffolds were incubated in 2% (w/v) Alizarin Red S (pH 4.1–4.3) for 1 h, and repeatedly washed with DI water. The amount of Alizarin Red S bound to calcium was quantified by eluting the stain with a 10% (w/v) hexadecyltrimethylammonium chloride solution. The absorbance of the eluted solution was measured at 557 nm with a spectrophotometer (Multiskan Go, Thermo Fisher Scientific, USA).
Statistical analysis
Statistical analysis, employing analysis of variance (ANOVA) in GraphPad Prism version 9.0, revealed group differences. The data are presented as mean ± standard deviation (S.D.).
Results
3D-printed PLA and PLA-composite scaffolds
3D printing has gained significant popularity as a method for the design of customized scaffolds. Fused Deposition Modeling (FDM) has emerged as one of the most practical choices among various 3D printing techniques due to its versatility, environmental friendliness, and simplicity, making it ideal for printing a wide range of plastic materials37.
The printed scaffold surface was analyzed using SEM (Fig. 1). High-magnification images provided a close look at the surface morphology of the scaffolds. The surface of the PLA group appeared smooth, whereas the P10 and P20 groups exhibited a rough surface due to HA particles mixed with PLA13. Additionally, scratch marks and micropores were observed on the surface of the PC scaffold following alkali treatment and HA coating. It is possible that carbon chain cleavage resulted in the release of carbon radicals, which could bind with hydroxyl groups from the alkali solution, thus creating an ideal surface for the absorption of HA particles38. The Ca distribution images, as revealed by EDS mapping, indicate the presence of Ca in the P10, P20, and PC scaffolds. While P10 and P20 show localized variations in calcium density, PC demonstrates a more uniform calcium distribution across its surface. The calcium content in P10, P20, and PC was measured at 6.76% ± 0.12, 12.37% ± 0.12, and 3.76% ± 0.08, respectively.
AFM-based nanomechanical mapping
The hADMSCs are responsive to the microenvironments in which they reside39,40,41. It has been shown that even nanoscale alteration can impact cell viability and fate42,43. Therefore, we investigated the surface properties of the scaffolds at the nanometer resolution. The AFM-based quantitative imaging (QI) mode simultaneously collected the height, stiffness, and adhesive force maps. The exemplary data maps for the PLA and PLA/HA composite scaffolds (P10, P20, and PC) were displayed (Fig. 2). The data showed that the PLA and PC scaffolds had a relatively smooth surface. On the other hand, the P10 and P20 scaffolds possessed sharp and rough surfaces. The rough appearance observed from the AFM measurement agreed well with the SEM micrographs (Fig. 1 1000x–5000x). The QI mode allowed simultaneous extraction of the height, stiffness, and adhesive force of the interfaces. The QI mapping data were collected for the PLA, P10, P20, and PC scaffolds. For the PLA scaffolds, the height of the PLA surface fluctuated within a 400-nm range (Fig. 2a). The stiffness, the slope of the approaching force-distance curve, of the PLA surface was about 0.5–1.5 N/m (Fig. 2b). Lastly, the adhesive force, which is the attraction between the AFM tip and the PLA surface, varied within the 40-nN range (Fig. 2c). By comparing three QI maps of the PLA surface, it appeared that the rough regions (Fig. 2a) have high stiffness (Fig. 2b) and high adhesive force (Fig. 2c). The result agrees with previous studies that indicate that the stiffness depends on surface roughness44.
Exemplary AFM micrographs of (a, d, g, j) topography or height, (b, e, h, k) stiffness, and (c, f, i, l) adhesive force of the (a-c) PLA, (d-f) P10, (g-i) P20, and (j-l) PC scaffold surfaces. The scale bars (5 µm) on the right bottom corner showed the lateral (XY) dimensions. The color gradient bars on the right showed the values of height, stiffness, and adhesive force.
Stiffness and adhesion distributions
We analyzed the height, stiffness, and adhesive force distributions across different scaffold types. Height, stiffness, and adhesive forces were extracted and plotted as distributions, revealing distinct patterns (Fig. 3). PLA and PC scaffolds displayed bimodal Gaussian distributions for height, stiffness, and adhesive forces. P20 scaffolds displayed a Gaussian distribution of height but bimodal distributions of stiffness and adhesive forces. In contrast, the P10 scaffold exhibited Gaussian distributions of all three parameters, indicating surface homogeneity. For height (Fig. 3a–d), the PLA scaffolds showed an average height of 1.01 µm, with a small part having an average height of 1.24 µm. The P20 scaffolds had an average of 1.92 µm, with a small portion having an average of 2.42 µm. The surfaces of the P10 and PC scaffolds exhibited average heights of 6.56 and 0.26 µm, respectively. For stiffness (Fig. 3e–h), the PLA scaffolds predominantly showed an average stiffness of 1.20 N/m, with a small portion having an average stiffness of 2.56 N/m. In contrast, the P20 scaffolds featured a majority with an average stiffness of 4.54 N/m, and a small portion had an average stiffness of 1.65 N/m. The PC scaffolds had a dominant stiffness of 1.75 N/m, with a small portion having an average stiffness of 3.71 N/m. Notably, the P10 scaffolds displayed the most uniform stiffness, averaging 1.69 N/m. These variations in stiffness are attributed to the presence of hydroxyapatite (HA) particles in P10 (1.69 N/m), P20 (4.54 N/m), and PC (1.75 N/m) scaffolds, resulting in higher stiffness compared to PLA (1.20 N/m) presumably due to the addition of the HA particles45. The surfaces of the PC scaffolds also had higher stiffness than the PLA scaffolds, possibly due to an HA layer. Some studies also suggest that the HA presence contributes to the reinforcement of the scaffold, which may be associated with the increasing stiffness in our case26.
Similarly, adhesive force distributions showed bimodal Gaussian patterns in PLA, P20, and PC scaffolds, while P10 exhibited a Gaussian distribution (Fig. 3i–l). Most PLA scaffolds displayed an average adhesive force of 57.3 nN, with a small portion having an average adhesive force of 23.9 nN. For P20, the dominant adhesive force was 166.3 nN, while a small portion had an average adhesive force of 114.7 nN. PC scaffolds mainly exhibited an average adhesive force of 38.3 nN, with a small portion having an average adhesive force of 26.2 nN. Lastly, the P10 scaffolds demonstrated uniform adhesive force distribution, averaging 58.8 nN. We found that both P10 and P20 scaffolds exhibited high adhesive forces. Our result suggests that HA incorporation enhances surface stickiness, agreeing with other studies that adding reinforcing filler can increase adhesion interfaces and, thus, create adhesive force between the surface and the AFM tip46. However, despite having HA as a top layer, the PC scaffolds showed a lower average adhesion force than PLA. The result implies that the HA corporation method with PLA can affect the nanomechanical properties of the scaffold. The presence of the HA layer in the PC scaffolds did not increase the surface adhesion, but mixing the HA as reinforcing filler allows the co-existence of two phases—HA and PLA, which, in turn, increase the surface adhesion. These nanomechanical characterizations provide critical insights into scaffold surface properties. Next, we explore how these properties influence the behavior of hADMSCs, which have clinical relevance and are instrumental in in vitro bone formation studies.
Cell attachment and metabolic activity
AFM results indicated that HA addition or coating altered the nanoscale surface properties of PLA scaffolds. To understand their impact on cellular behavior, hADMSCs were seeded and differentiated into osteoblasts, serving as a proof of concept of bone tissue engineering. Fluorescence of PrestoBlue™ assay results (Fig. 4a) reflected cellular metabolic activity. After three days, hADMSCs showed robust attachment to all scaffolds, as indicated by strong fluorescence signals. However, by day seven, the PC scaffold group exhibited significantly lower metabolic activity compared to the other groups. These findings suggest that PLA, P10, and P20 scaffolds support cell attachment and viability. SEM analysis (Fig. 4b) after seven days revealed spread-out cell morphologies on PLA, P10, and P20 scaffolds, indicating favorable cell adhesion and proliferation. In contrast, cells appeared rounded on the PC scaffold, correlating with reduced viability. These observations suggest that the surface properties of scaffolds play a crucial role in influencing cell adhesion and viability. PLA/HA composite materials have shown promise for bone scaffolds with osteogenic and osteoconductive potential12,40. Based on cell attachment and viability results, we selected P10 and P20 scaffolds to investigate long-term hADMSCs osteogenic differentiation. Both scaffolds exhibited sustained cell viability and even distribution on the scaffold surface for up to 4 weeks (Fig. 4c).
The hADMSCs (a) viability cultured on the PLA, P10, P20, and PC scaffolds for three days and seven days. All data are expressed as mean ± SD (n = 3) and *indicates a statistically significant difference with p-value < 0.05, (b) morphology by SEM micrographs cultured in the PLA, P10, P20, and PC scaffolds for seven days at different magnifications. The scale bars are 200 µm for 200x, 50 µm for 1000x, and 10 µm for 5000x, (c) images of live/dead staining of P10 and P20 scaffolds for 1, 2, and 4 weeks (green: live cells, red: dead cells). The white scale bars are 100 µm.
The mineralization and calcium deposition in the cell/scaffold constructs were visualized using Alizarin Red S staining (Fig. 5a,b), which has a high affinity for calcium ions. This staining method is commonly used to assess calcium deposition during osteogenic differentiation. The non-cell seeded scaffolds were initially stained with Alizarin Red S, and the resulting staining intensity reflected the baseline levels of hydroxyapatite incorporated in the scaffolds. Alizarin Red staining of the P10 scaffold significantly increased after 2 weeks of osteogenic differentiation, and the staining reached its peak at week 4. The staining intensity of the P20 scaffold gradually increased until week 4. We found that osteogenic differentiation at 4 weeks in the P10 group was significantly higher than in the P20 group. This is related to the quantitative analysis of the cell viability test at 4 weeks, where P10 showed higher cell viability than P20, as shown in (Figure S1). Together, the results suggest that the P10 scaffold appeared to be the most suitable for hADMSCs culture and osteoblast differentiation.
Evaluation of osteogenic differentiation of hADMSCs in P10 and P20 scaffolds. (a) Alizarin Red S staining detected calcium deposition in scaffolds at 2 and 4 weeks. A non-seeded scaffold was a control group without cells. The white scale bars are 1 cm. (b) The corresponding quantitative analysis of Alizarin red S staining for calcium deposition. The data are shown as mean ± SD. ** and *** indicate a statistically significant difference with p-value < 0.01 and 0.0001.
Discussion
The surface properties where cells reside can influence cell functions, including attachment, proliferation, and differentiation47,48,49,50. Eukaryotic cells respond to their surroundings through mechanosensing signals that trigger metabolic pathways regulating cell behavior and fate51,52. For example, cells tend to become neurons on soft surfaces and transform into muscle and bone cells at intermediate and high stiffness ranges, respectively50. To investigate the effect of surface properties on cell behavior, we analyzed the nanomechanical properties of 3D-printed scaffold surfaces. Nanomechanical mapping revealed that the PLA, P20, and PC scaffolds displayed bimodal distributions of stiffness and adhesive forces, while the P10 scaffold exhibited homogeneous surface properties, characterized by a Gaussian distribution of both stiffness and adhesion. Previous studies showed that the bimodal distributions normally reflect two composition phases26,34,44. In this study, the presence of a sufficient amount of HA and PLA in P20 and PC scaffolds seems to give rise to the bimodal stiffness and adhesion distributions, agreeing with the previous work. The bimodal distributions of PLA scaffold may be caused by printing traits, which may occur for pure PLA. Since HA has a much higher modulus than PLA, adding 10% of HA as a reinforcing filler may help obscure such traits, resulting in a Gaussian distribution of the stiffness and adhesion in the P10 scaffold. Adding more HA (i.e., 20%) could cause HA agglomeration within the PLA matrix, thus displaying the two-phase behavior and the bimodal distributions46. Lastly, the coating of HA in the PC scaffold directly introduces a separated phase of the HA, resulting in bimodal distributions.
The scaffold surface properties, such as roughness, wettability, and surface energy, have been demonstrated to be crucial for cell attachment, growth, and differentiation53,54. Several studies showed that high surface roughness increased space for cells residing13 and thus promoted cell attachment during the initial stage of the cells55,56,57. Regarding MSC differentiation, Adipocytes, in contrast to osteoblasts, are highly sensitive to topographical features58. High surface wettability is also shown to control the adhesion of cellular proteins and modulate cell adhesion59.
In this study, hADMSCs exhibited better attachment to P10 and P20 scaffolds than PLA and PC scaffolds. Higher surface roughness of P10 and P20 scaffolds, providing more contact points for cell anchoring58,60. Mineralization analysis revealed higher calcium deposition on the P10 scaffold than on the P20 scaffold. Since calcium mineralization is linked to cell differentiation, the result indicates that hADMSCs can differentiate into bone cells on the P10 scaffold better than on the P20 scaffold. The hADMSCs cell differentiation result suggests that the P10 scaffold provides a more conducive mechanical environment for cellular function61,62.
While the scaffold properties are extensively studied, surface homogeneity at the nanoscale is rarely investigated and discussed. The single distributions of the stiffness and the adhesive force of the P10 scaffold indicate a high degree of surface homogeneity compared to the PLA and PLA-composite materials. Our result suggests that homogenous surface properties of the P10 scaffold promote cell attachment and differentiation. The finding agrees with the previous study showing that a uniform β-phase poly(vinylidene fluoride) (PVDF) surface promotes uniform distribution of the fibroblast cells on the surface63. A study by Beijer et al. also showed that non-uniform surface topography caused hMSC cells to create an adapted cellular state where the shrinkage of cell and nucleus, protein condensation, and mitochondria reduction can be observed60. Furthermore, Chun Yang and colleagues confirmed that hMSC osteogenesis is influenced by surface pattern regularity. Cells on regularly patterned scaffolds were more spread, larger in area, and exhibited darker staining with alkaline phosphatase (ALP), indicating higher expression of the osteogenic marker ALP, like hMSCs cultured on uniformly stiff gels. In contrast, minimal staining was observed in hMSCs cultured on randomly patterned and uniformly soft surfaces, suggesting significantly lower osteogenesis64. Therefore, it is evident that the hADMSCs cells prefer the P10 scaffold due to its surface homogeneity properties.
The P10 scaffold also has unique properties. Its stiffness (1.69 N/m) and adhesive force (58.8 nN) were relatively in the middle range of the stiffness (1.20–4.54 N/m) and adhesive force values (23.9–116.3 nN). Surface stiffness in this work is essentially the surface energy, which has been shown to promote cell retention and adhesion53. Adhesive force in this work is directly proportional to wettability and surface charge, which help with cell attachment. Our results imply that hADMSCs favor distinct stiffness (surface energy) and adhesion force (surface charge) for the best growth condition. Such specific surface characteristics may differ for different cell types. Studies showed that different parts of the neuron cells favor different surface stiffness65,66. Fibroblasts prefer soft over hard surfaces54. The surface energy can influence the interactions between cells and the extracellular matrix, broadly impacting cell adhesion responses. Our work emphasizes the need to understand cell-surface interaction and cellular response to microenvironments to improve the design and engineering of bone-replacement material synthesis67.
Furthermore, the preparation method may affect the material properties. In this case, we employed two methods of incorporating HA into PLA, blending and surface coating. Despite the PC scaffold having HA content on the surface, hADMSCs exhibited poor cell viability when cultured on the PC scaffold, suggesting that contact with HA from surface modification may have a toxic effect on hADMSCs68,69. This outcome may be due to HA particle agglomeration38 and residual alkali or other chemicals70,71. HA agglomeration creates stress points for cells, adversely affecting their morphology and potentially leading to cell death. Residual alkali from surface treatment can increase local pH, producing cell toxicity. These changes in surface chemistry may render the material less conducive to cell attachment and proliferation72. Therefore, it is crucial to thoroughly evaluate the preparation method of these scaffolds before considering their in vivo usage.
Conclusion
The present study investigated the nanomechanical mapping of HA-composite PLA scaffolds and the potential association with in vitro cellular responses. The P10 scaffold modified by adding 10% of HA showed the highest cell attachment, viability, and mineralization among the four scaffold types. The AFM-based nanomechanical mapping provided high-spatial-resolution interface data of the PLA-composite scaffolds. Notably, the P10 scaffold exhibited uniform distributions of stiffness and adhesive force within an intermediate range. The result suggests an association between optimal conditions for cell growth and homogeneity of the surface properties. The study highlights the importance of understanding the material properties at a nanoscale resolution to reveal distinct properties that may not be evident in low-resolution data. The surface homogeneity is critical for interactions between cells and the scaffold interface. It must be further investigated for its potential correlation with other osteogenesis properties, such as osteoinductivity, osteointegrity, and osteoconductivity16. The insight into these correlations used as a design guideline will allow us to synthesize, functionalize, and tailor the scaffolds with specific requirements to maximize cell growth and enhance scaffold in vivo performance. Furthermore, the high-spatial-resolution data from AFM opens up the potential for future application of machine-learning analysis approaches73,74.
Data availability
The raw data required to reproduce these findings cannot be shared at this time as it is also part of an ongoing study. However, the processed data required to reproduce these findings are available in the manuscript and the supporting information section.
References
Mirkhalaf, M., Men, Y., Wang, R., No, Y. & Zreiqat, H. Personalized 3D printed bone scaffolds: A review. Acta Biomater. 156, 110–124 (2023).
Koons, G. L., Diba, M. & Mikos, A. G. Materials design for bone-tissue engineering. Nat. Rev. Mater. 5, 584–603 (2020).
Roddy, E., DeBaun, M. R., Daoud-Gray, A., Yang, Y. P. & Gardner, M. J. Treatment of critical-sized bone defects: Clinical and tissue engineering perspectives. Eur. J. Orthop. Surg. Traumatol. 28, 351–362 (2018).
Campana, V. et al. Bone substitutes in orthopaedic surgery: From basic science to clinical practice. J. Mater. Sci. Mater. Med. 25, 2445 (2014).
Gaharwar, A. K., Singh, I. & Khademhosseini, A. Engineered biomaterials for in situ tissue regeneration. Nat. Rev. Mater. 5, 686–705 (2020).
Vidal, L. et al. In situ production of pre-vascularized synthetic bone grafts for regenerating critical-sized defects in rabbits. Acta Biomater. 114, 384–394 (2020).
Bohner, M., Loosli, Y., Baroud, G. & Lacroix, D. Commentary: Deciphering the link between architecture and biological response of a bone graft substitute. Acta Biomater. 7, 478–484 (2011).
Han, J. et al. Development of a scaffold-on-a-chip platform to evaluate cell infiltration and osteogenesis on the 3D-printed scaffold for bone regeneration. ACS Biomater. Sci. Eng. 9, 968–977 (2023).
Ilhan, E. et al. Fabrication of tissue-engineered tympanic membrane patches using 3D-printing technology. J. Mech. Behav. Biomed. Mater. 114, 104219 (2021).
Zhang, L., Yang, G., Johnson, B. N. & Jia, X. Three-dimensional (3D) printed scaffold and material selection for bone repair. Acta Biomater. 84, 16–33 (2019).
Bose, S., Vahabzadeh, S. & Bandyopadhyay, A. Bone tissue engineering using 3D printing. Mater. Today 16, 496–504 (2013).
Wang, W. et al. 3D printing of PLA/n-HA composite scaffolds with customized mechanical properties and biological functions for bone tissue engineering. Compos. B Eng. 224, 109192 (2021).
Hao, S. et al. Modulatory effects of the composition and structure on the osteogenic enhancement for superparamagnetic scaffolds. Eng. Sci. 4, 100–110 (2018).
Hou, X., Lu, X. & He, C. Strong interface via weak interactions: Ultratough and malleable polylactic acid/polyhydroxybutyrate biocomposites. Macromol. Rapid Commun. 43, 2100619 (2022).
Hou, X. et al. Entropy-driven ultratough blends from brittle polymers. ACS Macro Lett. 10, 406–411 (2021).
Donate, R., Monzón, M. & Alemán-Domínguez, M. E. Additive manufacturing of PLA-based scaffolds intended for bone regeneration and strategies to improve their biological properties. E-Polymers 20, 571–599 (2020).
Hou, X. et al. Entropically toughened robust biodegradable polymer blends and composites for bone tissue engineering. ACS Appl. Mater. Interfaces 16, 2912–2920 (2024).
Patil, S., Dhyani, V., Kaur, T. & Singh, N. Spatiotemporal control over cell proliferation and differentiation for tissue engineering and regenerative medicine applications using silk fibroin scaffolds. ACS Appl. Bio. Mater. 3, 3476–3493 (2020).
Zheng, S., Guan, Y., Yu, H., Huang, G. & Zheng, C. Poly-L-lysine-coated PLGA/poly(amino acid)-modified hydroxyapatite porous scaffolds as efficient tissue engineering scaffolds for cell adhesion, proliferation, and differentiation. New J. Chem. 43, 9989–10002 (2019).
Liedert, A., Kaspar, D., Augat, P., Ignatius, A. & Claes, L. Mechanobiology of bone tissue and bone cells. In Mechanosensitivity in Cells and Tissues (eds Liedert, A. et al.) (Academia, 2005).
Mondal, S. et al. Hydroxyapatite nano bioceramics optimized 3D printed poly lactic acid scaffold for bone tissue engineering application. Ceram. Int. 46, 3443–3455 (2020).
Diao, H., Si, Y., Zhu, A., Ji, L. & Shi, H. Surface modified nano-hydroxyapatite/poly(lactide acid) composite and its osteocyte compatibility. Mater. Sci. Eng. C 32, 1796–1801 (2012).
Jin, Y. et al. Oxidative stress-induced apoptosis of osteoblastic MC3T3-E1 cells by hydroxyapatite nanoparticles through lysosomal and mitochondrial pathways. RSC Adv. 7, 13010–13018 (2017).
Shi, Z., Huang, X., Cai, Y., Tang, R. & Yang, D. Size effect of hydroxyapatite nanoparticles on proliferation and apoptosis of osteoblast-like cells. Acta Biomater. 5, 338–345 (2009).
Ji, S. & Guvendiren, M. 3D printed wavy scaffolds enhance mesenchymal stem cell osteogenesis. Micromachines 11, 31 (2019).
Martínez-Tong, D. E. et al. Quantitative mapping of mechanical properties in polylactic acid/natural rubber/organoclay bionanocomposites as revealed by nanoindentation with atomic force microscopy. Compos. Sci. Technol. 104, 34–39 (2014).
Mandriota, N. et al. Cellular nanoscale stiffness patterns governed by intracellular forces. Nat. Mater. 18, 1071–1077 (2019).
Ingber, D. E. Mechanobiology and diseases of mechanotransduction. Ann. Med. 35, 564–577 (2009).
Kwon, J. & Cho, H. Nanomechanical characterization of bone quality depending on tissue age via bimodal atomic force microscopy. Nanomanuf. Metrol. 6, 1–11 (2023).
Collinson, D. W., Sheridan, R. J., Palmeri, M. J. & Brinson, L. C. Best practices and recommendations for accurate nanomechanical characterization of heterogeneous polymer systems with atomic force microscopy. Prog. Polym. Sci. 119, 101420 (2021).
Alsteens, D. et al. Atomic force microscopy-based characterization and design of biointerfaces. Nat. Rev. Mater. 2, 1–16 (2017).
Garcia, R. Nanomechanical mapping of soft materials with the atomic force microscope: Methods, theory and applications. Chem. Soc. Rev. 49, 5850–5884 (2020).
Hu, J. et al. Global mapping of live cell mechanical features using peakforce QNM AFM. Biophys. Rep. 6, 9–18 (2020).
Zhang, S. et al. Quantitative nanomechanical mapping on poly(lactic acid)/poly(ε-caprolactone)/carbon nanotubes bionanocomposites using atomic force microscopy. Polym Test 77, 105904 (2019).
JPK Instruments. QI mode-Quantitative Imaging with the Nanowizard 3 AFM. https://www.jpk.com/app-technotes-img/AFM/pdf/jpk-tech-quantitative-imaging.14-1.pdf (2014).
Matplotlib: Python plotting—Matplotlib 3.4.1 documentation. https://matplotlib.org/.
Wickramasinghe, S., Do, T. & Tran, P. FDM-based 3D printing of polymer and associated composite: A review on mechanical properties, defects treatments. Polymers 12, 1529 (2020).
Chen, W. et al. Alkali treatment facilitates functional nano-hydroxyapatite coating of 3D printed polylactic acid scaffolds. Mater. Sci. Eng. C 120, 111686 (2021).
Abdallah, B. M. & Kassem, M. Human mesenchymal stem cells: From basic biology to clinical applications. Gene Ther. 15, 109–116 (2007).
Docheva, D., Popov, C., Mutschler, W. & Schieker, M. Human mesenchymal stem cells in contact with their environment: Surface characteristics and the integrin system. J. Cell. Mol. Med. 11, 21–38 (2007).
Pittenger, M. F. et al. Multilineage potential of adult human mesenchymal stem cells. Science 1979(284), 143–147 (1999).
Rothdiener, M. et al. Stretching human mesenchymal stromal cells on stiffness-customized collagen type I generates a smooth muscle marker profile without growth factor addition. Sci. Rep. 6, 1–15 (2016).
Danti, S., D’Acunto, M., Trombi, L., Berrettini, S. & Pietrabissa, A. A micro/nanoscale surface mechanical study on morpho-functional changes in multilineage-differentiated human mesenchymal stem cells. Macromol. Biosci. 7, 589–598 (2007).
Serra, T., Ortiz-Hernandez, M., Engel, E., Planell, J. A. & Navarro, M. Relevance of PEG in PLA-based blends for tissue engineering 3D-printed scaffolds. Mater. Sci. Eng. C 38, 55–62 (2014).
Zheng, L. et al. 3D-printed scaffolds based on PLA/HA nanocomposites for trabecular bone reconstruction. J. Phys. Conf. Ser. 741, 012068 (2016).
Akindoyo, J. O., Beg, M. D. H., Ghazali, S., Heim, H. P. & Feldmann, M. Effects of surface modification on dispersion, mechanical, thermal and dynamic mechanical properties of injection molded PLA-hydroxyapatite composites. Compos. Part A Appl. Sci. Manuf. 103, 96–105 (2017).
Bobbert, F. S. L. & Zadpoor, A. A. Effects of bone substitute architecture and surface properties on cell response, angiogenesis, and structure of new bone. J. Mater. Chem. B 5, 6175–6192 (2017).
Monchaux, E. & Vermette, P. Effects of surface properties and bioactivation of biomaterials on endothelial cells. Front. Biosci. (Schol. Ed.) 2, 239–255 (2010).
Wells, R. G. The role of matrix stiffness in regulating cell behavior. Hepatology 47, 1394–1400 (2008).
Cheng, X. et al. Enhanced biocompatibility of polyurethane-type shape memory polymers modified by plasma immersion ion implantation treatment and collagen coating: An in vivo study. Mater. Sci. Eng. C 99, 863–874 (2019).
Chen, S. et al. Tuning surface properties of bone biomaterials to manipulate osteoblastic cell adhesion and the signaling pathways for the enhancement of early osseointegration. Coll. Surf. B Biointerfaces 164, 58–69 (2018).
Lee, M. H., Ducheyne, P., Lynch, L., Boettiger, D. & Composto, R. J. Effect of biomaterial surface properties on fibronectin–α5β1 integrin interaction and cellular attachment. Biomaterials 27, 1907–1916 (2006).
Idaszek, J., Kijeńska, E., Łojkowski, M. & Swieszkowski, W. How important are scaffolds and their surface properties in regenerative medicine. Appl. Surf. Sci. 388, 762–774 (2016).
Chang, H. I., Wang, Y., Chang, H. I. & Wang, Y. Cell responses to surface and architecture of tissue engineering scaffolds. In Regenerative Medicine and Tissue Engineering-Cells and Biomaterials (ed. Daniel, E.) (IntechOpen, 2011).
Tong, C. Y. & Derek, C. J. C. Membrane surface roughness promotes rapid initial cell adhesion and long term microalgal biofilm stability. Environ. Res. 206, 112602 (2022).
Kang, S., Hoek, E. M. V., Choi, H. & Shin, H. Effect of membrane surface properties during the fast evaluation of cell attachment. Sep. Sci. Technol. 41, 1475–1487 (2007).
Huang, H. H. et al. Effect of surface roughness of ground titanium on initial cell adhesion. Biomol. Eng. 21, 93–97 (2004).
Ortiz, R. et al. Laser surface microstructuring of a bio-resorbable polymer to anchor stem cells, control adipocyte morphology, and promote osteogenesis. Polymers (Basel) 10, 1337 (2018).
Al-Azzam, N. & Alazzam, A. Micropatterning of cells via adjusting surface wettability using plasma treatment and graphene oxide deposition. PLoS ONE 17, e0269914 (2022).
Beijer, N. R. M. et al. Dynamic adaptation of mesenchymal stem cell physiology upon exposure to surface micropatterns. Sci. Rep. https://doi.org/10.1038/s41598-019-45284-y (2019).
Maazouz, Y., Chizzola, G., Döbelin, N. & Bohner, M. Cell-free, quantitative mineralization measurements as a proxy to identify osteoinductive bone graft substitutes. Biomaterials 275, 120912 (2021).
González-Vázquez, A., Planell, J. A. & Engel, E. Extracellular calcium and CaSR drive osteoinduction in mesenchymal stromal cells. Acta Biomater. 10, 2824–2833 (2014).
Low, Y. K. A. et al. β-Phase poly(vinylidene fluoride) films encouraged more homogeneous cell distribution and more significant deposition of fibronectin towards the cell–material interface compared to α-phase poly(vinylidene fluoride) films. Mater. Sci. Eng. C 34, 345–353 (2014).
Yang, C. et al. Spatially patterned matrix elasticity directs stem cell fate. Proc. Natl. Acad. Sci. USA 113, E4439–E4445 (2016).
Zhang, Q. Y. et al. Stiff substrates enhance cultured neuronal network activity. Sci. Rep. https://doi.org/10.1038/srep06215 (2014).
Yi, B., Xu, Q. & Liu, W. An overview of substrate stiffness guided cellular response and its applications in tissue regeneration. Bioact. Mater. 15, 82 (2022).
Song, Y. et al. Micromechanical compatibility between cells and scaffolds directs the phenotypic transition of stem cells. ACS Appl. Mater. Interfaces 13, 58152–58161 (2021).
Coelho, C. C., Grenho, L., Gomes, P. S., Quadros, P. A. & Fernandes, M. H. Nano-hydroxyapatite in oral care cosmetics: Characterization and cytotoxicity assessment. Sci. Rep. 9, 1–10 (2019).
Zhao, X. et al. Cytotoxicity of hydroxyapatite nanoparticles is shape and cell dependent. Arch. Toxicol. 87, 1037–1052 (2013).
Gomes, H. I., Mayes, W. M., Rogerson, M., Stewart, D. I. & Burked, I. T. Alkaline residues and the environment: A review of impacts, management practices and opportunities. J. Clean. Prod. 112, 3571–3582 (2016).
Yang, J. et al. Enhancing the cell affinity of macroporous poly(L-lactide) cell scaffold by a convenient surface modification method. Polym. Int. 52, 1892–1899 (2003).
Tan, J. et al. Effect of local alkaline microenvironment on the behaviors of bacteria and osteogenic cells. ACS Appl. Mater. Interfaces 10, 42018–42029 (2018).
Sokolov, I. et al. Noninvasive diagnostic imaging using machine-learning analysis of nanoresolution images of cell surfaces: Detection of bladder cancer. Proc. Natl. Acad. Sci. USA 115, 12920–12925 (2018).
Kalinin, S. V. et al. Big, deep, and smart data in scanning probe microscopy. ACS Nano 10, 9068–9086 (2016).
Acknowledgements
US acknowledges funding support from the NSRF via the Program Management Unit for Human Resources & Institutional Development, Research, and Innovation (grant number B16F640116) and the National Center for Genetic Engineering and Biotechnology (BIOTEC), National Science and Technology Development Agency (NSTDA), Thailand (Project Number P21-51892). SS is funded by a Postdoctoral Fellowship, Ratchadapisek Somphot Fund, Chulalongkorn University. SY received research funds from Fundamental Fund 2567, grant number: HEAF67300042. XH and CH acknowledge the financial support from the Ministry of Education (MoE) in Singapore, grant number T2EP50222-0001. The funding sources had no role in study design, data collection, data analysis, data interpretation, manuscript writing, manuscript editing, and manuscript submission.
Author information
Authors and Affiliations
Contributions
SS, US, and SY: Conceptualization, Methodology, Formal analysis, Investigation, Resources, Writing—original draft, Writing—review & editing, Funding acquisition. XH, AT, XX, CH, and WL: Methodology, Investigation, Resources, Writing—review & editing. All authors approved the manuscript submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sitthisang, S., Hou, X., Treetong, A. et al. Nanomechanical mapping of PLA hydroxyapatite composite scaffolds links surface homogeneity to stem cell differentiation. Sci Rep 14, 21097 (2024). https://doi.org/10.1038/s41598-024-72073-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-72073-z
Keywords
This article is cited by
-
Structural, morphological and biological assessment of magnetic hydroxyapatite with superior hyperthermia potential for orthopedic applications
Scientific Reports (2025)
-
Enzymatic etching of PLA/hydroxyapatite scaffolds for improved cell adhesion: surface modification and homogeneity
Emergent Materials (2025)