Abstract
The Ames test is used worldwide to initially screen the mutagenic potential of new chemicals. In the standard Ames test, S. typhimurium strains (TA100, TA98, TA1535, and TA1537) and Escherichia coli (WP2uvrA) are treated with substances with/without cytochrome P450s (CYPs)-induced rat S9 fractions for identifying mutagens and pro-mutagens. However, many substances show completely different toxicity patterns depending on whether the liver S9 fraction belongs to rats or humans. The natural product Polygoni Multiflori Radix (PMR) can also show bacterial reverse mutation, followed by the rat or human liver S9 fraction. While PMR elicits reverse mutations in the TA1537 strain in rat liver S9 but not in human liver S9, this mechanism has not been verified yet. To explain this, the differences in metabolic enzymes compositions commonly observed between rats and humans have been implicated. This study aimed to explore the key factors that cause differences in the genotoxicity of PMR between rat and human liver S9 metabolic enzymes. The results of next-generation sequencing (NGS) analysis showed that both rat and human metabolic enzymes caused similar mutations in TA1537. However, when the metabolic enzymes in each S9 fraction were analyzed using ion mobility tandem mass spectrometry (IM-MS), rat- and human-specific enzymes were identified among the cytochrome (CYP) family, especially aryl hydrocarbon receptor (AHR)-related CYPs. These findings suggest that CYP1A1 isoforms contribute to the mechanism of PMR in the Ames test. Therefore, an in vitro Ames test might be more reliable in predicting genotoxicity for both rodents and humans. This will also help overcome the limitations of laboratory animal-based toxicity evaluations, which provide unreliable results due to interspecies differences between humans and rodents.
Similar content being viewed by others
Introduction
Ames test, which evaluates bacterial reverse mutation, is used worldwide as an initial screening method to determine the mutagenic potential of new chemicals1,2,3,4,5,6. In the standard Ames test, Salmonella Typhimurium (TA100, TA98, TA1535, and TA1537) and Escherichia coli (E. coli) (WP2uvrA) strains are used to identify potentially genotoxic substances7. Many carcinogens or mutagens remain inactive until they are enzymatically transformed into an electrophilic species that can covalently bind to DNA, causing mutations. Therefore, understanding metabolic activation is critical for investigating potential pro-mutagens. The Aroclor 1254-induced rat liver supernatant S9 fraction (Aroclor 1254-rat liver S9) is routinely used as an exogenous metabolic activation system for evaluating pro-mutagens1,4. As the responses obtained using rat liver S9 cannot be extrapolated in humans, human liver S9 fractions containing metabolic enzymes such as cytochrome P450s (CYPs), UDP glucuronyltransferases (UGTs), and other cytosolic enzymes have also been used for the Ames tests8. Nevertheless, the Aroclor 1254-rat liver S9 fraction is still commonly used for the Ames test.
As the type of S9 used is a critical factor in the Ames test4,5,9 S9-dependent Ames test results have been shown, which quantified several CYPs in each S9 fraction8,10. However, identifying the factor determining the genotoxicity is challenging due to the proteomic differences between rat and human liver metabolic enzymes, such as absolute quantity, species-specific isoforms, activity, and sensitivity, between rat and human liver metabolic enzymes8,10. Even in the case of chemical mixtures such as herbal medicines, dynamic interactions occur between chemicals and/or metabolic enzymes, such as similar actions (dose/concentration addition), dissimilar actions (independent action), and interactions11. Due to these limitations, the mechanism underlying toxicity in metabolic enzymes between different species is poorly understood.
Polygoni Multiflori Radix (PMR, Ha Su O in Korean, He Shou Wu in China) is a medicinal plant widely used in Korea, China, and Japan for treating conditions such as amnesia, insomnia, and heart palpitations. Traditionally, it has been reported to exhibit hair-darkening, liver and kidney-toning, anti-aging effects, and low toxicity12,13. PMR contains many chemical constituents, including flavones, quinones, emodin, chrysophanol, rhein, physcion, and stilbenes14. Among these, emodin (1,3,8-trihydroxy-6-methylanthraquinone) is well known for inducing hepatotoxicity, nephrotoxicity, genotoxicity, and reproductive toxicity15. Previously, we used quantitative analysis to show that PMR-water extracts (PMR-W) contain three standard components: 2,3,5,4'-tetrahydroxystilbene-2-O-β-D-glycoside (4.55% ± 0.10%), emodin (0.08% ± 0.01%), and physcion (0.02% ± 0.01%)14. When PMR-W was subjected to the Ames test, it showed different toxicity patterns and was then tested on rat and human liver S9 mix (Supplementary Figs. 1 and 2). In rat liver S9, PMR elicited reverse mutations in the TA100 and TA1537 strains but not in human liver S9. Although differences in the toxicity patterns between metabolic enzymes in rats and humans have been reported in several substances10,16,17, the underlying mechanism is unknown. Therefore, we aimed to explore the key factors underlying the differences in the genotoxicity exhibited by PMR in rat and human liver S9. To address this issue, we compared the mutation patterns of metabolic enzymes in Aroclor 1254-induced rat S9 and human S9 using next-generation sequencing (NGS) analysis. We identified the proteins in each S9 fraction using ion mobility tandem mass spectrometry (IM-MS) and then identified the major factors contributing to the species-specific response. We also discussed that the specific effects of CYP isoforms might be responsible for the Ames test results.
Results
Comparative analysis of Ames test results for uninduced, Aroclor 1254-induced rat liver S9, and human liver S9-induced bacterial reverse mutations following PMR-W treatment
The mutagenic potential of PMR-W was tested using the Ames test with TA100, TA1535, TA98, TA1537, and WP2uvrA in the presence and absence of the Aroclor 1254-induced rat liver S9 system (Supplementary Figs. 1 and 2). In the PMR-W-treated TA100 and TA1537 strains, the number of revertant colonies increased in a concentration-dependent manner, showing a 2.7- and 9.9-fold increase over the previously reported data at the maximum concentration (5000 μg/plate).
Unlike Aroclor 1254-induced rat liver S9, when uninduced rat liver S9 or human liver S9 were used, PMR-W did not increase the number of revertant colonies in the TA1537 strain at concentrations up to 5000 μg/plate (Fig. 1). These results suggested that Aroclor 1254 possibly altered the factor that is responsible for the increase in revertant colonies.
In vitro bacterial reverse mutation test of the PMR-W-treated TA1537 strain in the absence and presence of metabolic activation (S9 mix). The mean number of revertant colonies in the absence or presence of uninduced is 5% Aroclor 1254-induced rat or 5% human liver S9 mix. Regardless of whether the S9 metabolic activation system was used, no turbidity, precipitation, or antibacterial toxicity, such as the formation of a background lawn, micro-colonies, or a decrease in the number of reverted colonies by more than 50%, was observed in all strains. The data represent the averages from triplicate plates per dose.
Comparative analysis of mutation patterns induced by Aroclor 1254-induced rat S9 and human S9 metabolic enzymes using next-generation sequencing analysis
In TA1537 strains, a frameshift mutation in the histidinol-phosphate aminotransferase 3076 (HisC3076) gene region caused revertant colonies1. We selected each revertant colony from Aroclor 1254-induced rat S9 or human S9 used at a concentration (3000 μg/plate) and compared the PMR-W-induced mutation pattern (Fig. 2, Table 1, Supplementary Table 1). The results showed that a similar number of single nucleotide polymorphisms (SNPs), insertions, or deletions occurred between the S9 types used. Both rat and human liver S9-treated TA1537 colony revertants had the same mutated gene regions without any PMR-specific SNPs. The total SNP number was not different.
The number of variants from the genome sequences of TA1537 or revertant colonies compared with the reference genome based on NCBI. Each bar represents three revertants treated by vehicle (distilled water) or PMR-W (3000 μg/plate). Reference genome: Salmonella enterica subsp. enterica serovar Typhimurium LT2 (AE006468.2); SNP single nucleotide polymorphism.
Comparative analysis of metabolizing enzymes identified in Aroclor 1254-induced rat S9 and human S9 using ion mobility tandem mass spectrometry
The proteins in each S9 fraction were identified using IM-MS, which revealed 2960 and 3166 proteins in human (pooled 50 donors) and rat liver S9 metabolic enzymes, respectively. Among these, 1040 and 1246 proteins were identified exclusively in human and rat liver S9 fractions, respectively. Whereas 1920 proteins were in common between these two fractions. Among human- and rat-specific proteins, 17 CYP isoforms, 8 UDP-glucuronosyltransferases (UGTs), 38 CYP isoforms, and 5 UGTs might contribute to the different toxicity patterns. Further, 1019 and 1171 human and rat liver metabolizing-specific enzymes were identified (Fig. 3). Comparison of the metabolic enzyme profiles of cytochrome P450 (CYPs) isoforms and UDP-glucuronosyltransferases (UGTs) revealed that 6 CYPs and 4 UGTs isoforms were commonly expressed, while 21 CYPs and 5 UGTs isoforms are expressed in humans. The specific activation and expression of 40 CYP and 5 UGT isoforms were confirmed (Table 2). As the actual expression levels of the CYP isoforms were compared (Fig. 4), the expression level of these isoforms, including CYP1A1, CYP1B1, CYP2B1/2B2, and CYP2D1 could be confirmed only in rat livers. While similar expression levels were seen for CYP1A2 and CYP3A4 in both rats and humans, it was confirmed that the levels were higher in rats.
Network analysis using STRING. Identified CYP- and UGT-metabolism-related enzymes from (A) human S9 (40 CYPs and UGT in total) and (B) Aroclor 1254-induced rat S9 (55 CYPs and UGT in total) were analyzed for each protein–protein interaction network. Metabolism-related enzymes, specifically CYP and UGT, were identified from (A) human S9 (comprising a total of 40 CYPs and UGTs) and (B) Aroclor 1254-induced rat S9 (with a total of 55 CYPs and UGTs). Each enzyme was analyzed within the protein–protein interaction network.
Protein–protein interaction networks and functional enrichment analyses
The differences in the composition between rat and human S9 metabolic enzymes were investigated using functional protein–protein interaction (PPI) network analysis with the STRING database (https://string-db.org/). Drug metabolism-related proteins were sorted according to the method by Wang et al.,21. A total of 127 human and 164 rat proteins, including phase I, phase II, and transporter proteins, were analyzed (Supplementary Table 2 and Supplementary Fig. 3). Functional enrichment analysis in biological processes showed the top five different KEGG (Kyoto Encyclopedia of Genes and Genomes) pathways (Supplementary Tables 3 and 4)18. They only considered phase I metabolic enzymes, rat liver S9 related in the steroid hormone biosynthesis KEGG pathway 46% among 55 CYPs and UGTs than human liver S9 40 CYPs and UGTs (Fig. 5 and Table 3).
In this study, we investigated the differential composition for rat and human metabolic enzymes through a comprehensive functional protein–protein interaction (PPI) network analysis, utilizing the STRING database. The categorization of drug metabolism-related proteins followed the methodology proposed by Wang et al.,21. Our analysis encompassed a total of 291 proteins, including 127 human and 164 rat proteins, which span phase I and II metabolic enzymes, in addition to transporter proteins (Supplementary Table 2 and Supplementary Fig. 3). Subsequent functional enrichment analysis focused on biological processes, highlighting the top five different KEGG pathways between the species-specific enzyme compositions (Supplementary Tables 3 and 4). Notably, when considering solely phase I metabolic enzymes, our findings revealed a pronounced discrepancy in the steroid hormone biosynthesis pathway within the rat liver S9, where 46% of the analyzed CYPs and UGTs (55 in total) were implicated, in constrast to the human liver S9, which involved 40 CYPs and UGTs. This disparity underscores potential variations in drug metabolism and hormonal regulation between rats and humans (Table 3).
Expression profile of CYPs in rat and human liver S9 fractions
Expression profile of CYPs in rat and human liver S9 fractions The expression levels of cytochrome P450 isoenzymes were investigated in uninduced rat liver S9 (lane 1), Aroclor-1254-induced rat liver S9 (lane 2), human liver S9 (lane 3), and human non-alcoholic steatohepatitis (NASH) liver S9 (lane 4). The western blot was probed with antibodies against CYP1A1, CYP1A2, CYP1B1, CYP2B1/2B2, CYP2D1, CYP2D6, and CYP3A4 for assessing the induction and expression profiles of these enzymes; β-actin serving as the loading control (Fig. 5). Lane 1 demonstrates CYPs’ baseline expression levels in uninduced rat liver S9 fractions. Lane 2 shows enhanced expression of CYP1A1, CYP1A2, and CYP2B1/2B2, indicating induction by Aroclor 1254 in rat liver S9 fractions. Lane 3 exhibits a distinct expression pattern in human liver S9 fractions with notable expression of CYP2D6 and CYP3A4, reflecting the metabolic profile typically observed in human liver. Lane 4 represents human NASH liver S9 fractions revealing marked alteration in the expression of CYPs, particularly with reduced expression of CYP2D6 and CYP3A4, which may imply altered drug metabolism in NASH-affected livers (Fig. 5). These findings suggest species-specific differences in the expression of CYPs and the potential impact of liver conditions, such as NASH, on the metabolic capacity of the liver.
In vitro Ames test results utilizing the BaP-induced rat liver S9 fraction
The differences in the induction of CYPs might be responsible for the differences in the mutagenic response induced in rat liver S9 by several reagents. Based on the omics-based data obtained from human and rat liver (Table 2), aryl hydrocarbon receptor (AHR)-derived downstream genes such as CYP1a1, CYP1a2, CYP1b1 was selected as the key candidate for metabolic enzymes responsible for mutagenicity. Interestingly, when the representative genes induced by the positive control benzo[a]pyrene (BaP) in the Ames test results were compared (Fig. 6), some enzymes were considered prime candidates. As a positive reagent to TA1537, the effects of BaP on PMR-W were similar in Aroclor 1254-induced rat and human S9 fractions. The efficacy of CYP1A1, induced by BaP19,20, was confirmed by introducing it into the Ames test using the BaP-induced rat liver S9 fraction. BaP-treated Sprague–Dawley rats showed a BaP dose-dependent increase in CYP1A1.
Comparison of metabolic activation systems in the PMR-W-treated TA1537 strain in the Ames test. The mean of the number of revertant colonies in the absence and presence of the 5% Aroclor1254-induced rat S9, 5% human liver S9, 5% and 10% CYP1A1 bactosome (instead of liver s9); combination of 5% human liver S9 and 5% CYP1A1 bactosome; and 10%, 20%, and 40% in vivo BaP-treated rat liver S9 are shown in (A). The BaP responses are shown in (B). 2AA 0.5 μg/plate (S9 positive control), 9AA 50 μg/plate (positive control), and BaP (Aroclor 1254-induced rat S9 positive control) were treated with positive control.
Inter-species variation in metabolic enzyme disparities
Comparison of the proteomic profiles of the AHR-related and rat and human metabolic enzymes were shown to be potent inducers of mutagenicity. BaP is a representative benign substance that exhibits carcinogenicity in the Ames test. It is used as a positive substance of TA1537 for rat metabolic enzymes, while 2-amino anthracene (2-AA) is used for humans. A comparison of the results obtained using these positive controls (Fig. 6) revealed that the mutagenicity of the TA1537 strain was increased by 2-AA and BaP when using the rat metabolic activation system. In the human metabolic activation system, revertant colony increased from 5 to 10% in a dose-dependent manner. However, concentration-dependent positive reactions could not be confirmed for various concentrations of BaP. Therefore, confirming the mutagenic response of CYP1a1 using the human metabolic activation system is impossible.
In addition, 5% and 10% of human CYP1a1 (Bactosome, Cypex) only were added to the human S9 mix and compared for reactivity. To confirm the effect of CYP1a1 alone, a three-day oral dose of BaP was prepared using a female rat liver S9 mix and subjected to the Ames test. The results were compared with those from the Aroclor 1254-induced rat S9 system (Fig. 6).
Western blotting was performed to confirm the relative amount of CYP1A1 expression (Fig. 7). As the amount of CYP1a1 was evaluated by loading 30 μg of protein, it was possible to confirm the concentration-dependent expression of CYP1a1 in rats orally administered with BaP. The amount of overexpressed CYP1a1 in the bactosome was similar to that of the Aroclor 1254-induced rat liver metabolic enzymes.
CYP1A1 expression levels from BaP-orally treated rat liver S9 faction. CYP1A1 gene expression level in BaP-treated or control corn oil-treated SD rats compared with the Aroclor 1254-induced Rat S9, HEK 293T cell lysate, Human S9, and ezCYP1A1 bactosome (A), and CYP1A1/GAPDH ratio (B). GAPDH was normalized as an internal control.
Analysis of the changes in the Ames test results after CYP1a1 was added with PMR-W (Fig. 6) revealed that the degree of EROD and MROD activity, which indicates the metabolic activity due to CYP1a1/1a2 isoforms, was reported to be 1/10 of ezCYP1A1 bactosome. These findings showed that the number of reverse mutations increased with an increase in the concentration of the product (5%–10%). The highest number of reverse mutations was observed in the human metabolic activation system, confirming an increase. This suggests that metabolic activators other than CYP1a1 might be required.
As Aroclor 1254 utilizes the liver metabolic enzymes of rats, which involves the induction of various metabolic activation systems, BaP, a representative inducer of CYP1a1, was orally administered to produce PMR directly from the liver metabolic enzymes of rats to confirm the effect of CYP1a1 only. The results were compared using the Ames test. Considering the relative expression levels illustrated in Fig. 7, we utilized proportions of 5, 10, 20, and 40% of BaP-induced rat S9 due to the observed variations in the expression level of CYP1a1 alone. We confirmed that the number of reverse mutations of TA1537 increased with an increase in the percentage of BaP-induced rat S9.
Discussion
In this study, the differences in rat and human liver S9 levels were explained based on rat- and human-specific metabolic enzymes, especially AHR-related CYPs. Adding CYP1A1 bactosomes or using BaP-induced rat liver S9 could contribute to increased TA1537 revertant colony numbers in human liver S9. Our findings suggest that CYP1a1 might be a major factor in genotoxicity testing.
Generally, induction of the metabolic activation system in the liver might enhance sensitivity toward chemicals, increasing the chances of false positive results. In particular, in the herbal extracts, induced CYP1a1 might contribute to the false positive Ames test results. Moreover, rodent data are needed to estimate the genotoxicity risk toward humans.
Emodin is also positive for TA1537 results, and emodin-induced hepatotoxicity is enhanced by 3-methylcholanthrene through activation of the AHR and induction of CYP1a1 in vitro and in vivo20 (Supplementary Fig. 4). Certain substances can exhibit positive reactions under specific metabolic activation systems. For nitrosamine impurities in medications, an enhanced Ames test is recommended22.
The data indicated that the mutagenicity of chemicals in the rat and human liver S9 fractions varied considerably, depending on the chemicals. In addition, a large interindividual diversity in the mutagenic response was seen using two selected human S9 fractions, which depended on the chemical structures of the mutagens16.
The differences in the responses toward specific chemicals might be an underlying cause. Emodin, a constituent of PMR, has known genotoxicity and has been tested using TA1537 with Aroclor 1254-induced rat or human liver S9 systems (Supplementary Fig. 4). As PMR-W contains 0.08% of emodin14, its concentration in a plate containing 5000 μg PMR-W is 4 μg/plate. The lowest concentration of emodin required to induce TA1537 revertants in both rat and human S9 system was determined to be 4.2 μg/plate. This suggested that emodin is genotoxic to rats and humans but might not cause the S9-dependent response.
Increased CYP1A1 levels can increase the risk of carcinogenesis. People with increased CYP1A1 expression have been shown to have a higher risk of developing cancer as carcinogens, such as polycyclic aromatic hydrocarbons (PAHs), are bioactivated in the human body, which increases their toxicity23. In addition to CYP1A1, other CYP isoforms are also increased by Aroclor 1254, and other cofactors, such as reductase, might be involved in these changes.
The metabolic enzyme profiles in rats and humans showed differences in the content of AHR-induced CYPs, including CYP1A1, CYP1B1, and CYP2D1. Previously, the increase in the metabolic activity of liver S9 fraction of a carcass by Aroclor 1254 was found to be associated with changes in the expression of CYP2E1, CYP3A4/5, CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, and CYP2C1924. When the effect of PMR extract was evaluated on the liver metabolites (hNASH liver S9) from non-alcoholic fatty liver (NASH) patients, the Ames test result was negative, and there was no change.
In conclusion, ingredients that bind to AHR might be present in the PMR extract. Further, AHR-related metabolic enzymes, such as CYP1A1, CYP1B1, and CYP2D1, in the liver metabolite are potent metabolic enzymes of mutagenicity. In the case of natural extracts, the expression level of metabolic enzymes is considered a major factor in genotoxicity testing.
Materials and methods
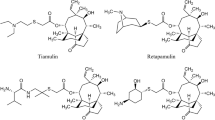
Chemicals and reagents
The PMR-W was prepared using the standard decoction preparation method (Ministry of Food and Drug Safety Notification 2003–17, Safety and Effectiveness Review Regulations Standard decoction manufacturing method according to the standard)14 and freeze-dried after concentration. Distilled water (DW) (Gibco, USA) was used as the negative control.
For the bacterial reverse mutation test, the following stock solutions were prepared: 5 μg/plate sodium azide (SA) in DW; 20 μg/plate 2-nitrofluorene (2-NF), 500 μg/plate 9-aminoacridine (9-AA), 10 μg/plate 4-nitroquinoline N-oxide (4NQO), 20 μg/plate and 40 μg/plate 2-aminoanthracene (2-AA) and 20 μg/plate benzo[a]pyrene (BaP) stock solution in DMSO (Dimethyl sulfoxide, Sigma-Aldrich, USA). These were kept at − 20 °C until use. For the BP stock solution, 5.8 μg/plate (final concentration to the plate 1 mM) was diluted to 2.9 and 1.45 μg/plate with DMSO.
Metabolic activation system (liver S9 fractions)
Liver S9 fractions were included in the tests because many substances only show mutagenic activity in the presence of enzymatic activation. To prepare the S9 mix, the Aroclor 1254-induced Sprague–Dawley rat liver S9 metabolic system (Molecular Toxicology Inc., USA) was mixed with the cofactor (Wako Pure Chemical Industries, Ltd., Japan).
In our human enzyme studies, we utilized human CYP1A1LR EasyCYP Bactosome enzymes, specifically designed to co-express with human NADPH CYP low reductase (#CYP/EZ018, Cypex Ltd, UK), along with a mixed-gender pool of 50 human liver S9 fractions and a mixed-gender pool of 5 human liver S9 fractions from individuals with non-alcoholic steatohepatitis (NASH), both provided by SEKISUI XenoTech, LLC, USA.
In vitro bacterial reverse mutation test (Ames test)
Ames test was performed according to the OECD test guidelines 4716, based on the method of Maron and Ames with minor modifications4. Briefly, S. typhimurium strains TA98, TA100, TA1535, and TA1537 and E. coli WP2uvrA (Molecular Toxicology Inc., USA) were used as the test strains in the presence or absence of 5% v/v Aroclor 1254-induced rat liver S9 metabolic system (S9 mix). Either 500 μL PBS (NaCl 0.135 M, KCL 2.7 mM, Na2HPO4 4.3 mM, KH2PO4 1.4 mM, pH 7.4) or S9 cofactor mixed with 2 mL of top agar supplemented with histidine-biotin or tryptophan solution was added to minimal glucose agar plates. 30,000 or 50,000 μg/mL of PMR-W were made as a highest concentration and diluted to each concentration with DW. Each bacterium (100 μL) was inoculated on the agar, followed by the appropriate test substance (100 μL volume) or vehicle/positive control. Therefore, 3000 or 5000 μg/plate was treated for the Ames test for PMR-W as a highest concentration. Following the maximum concentration, six dilutions (98.75, 187.5, 375, 750, 1500, and 5000 μg/plate) or four (111.11, 333.33, 1000, and 3000 μg/plate) and positive reagent (SA, 2-NF, 9-AA, 4NQO, 2-AA, BaP) were tested for each bacterial strain and incubated at 37 °C for 48 h. The experiments were performed using at least three replicates for each dose.
Whole genome resequencing
Each TA1537 colony treated with PMR-W (3000 μg/plate) without S9, Aroclor-1254-induced S9, or human S9 was incubated for 24 h in nutrient broth media. After library construction using the TruSeq Nano DNA kit, whole genome resequencing (WGS) was performed at the commercial sequence service of Macrogen Inc., Korea.
To map the sequenced reads, Salmonella enterica subsp. enterica serovar Typhi LT2 (NC_003197.2) was used as a reference genome. Based on this reference genome, the genes of the histidine operon 1 and 4 of TA1537 were mutated. Somatic mutations, including single nucleotide variants (SNVs), small insertions and deletions (Indels), and gene rearrangements and copy number variations (CNVs), were also identified.
Identification of S9 metabolic enzyme fraction using an ion mobility tandem mass spectrometer (IM-MS)
The trypsin-digested samples were subjected to LC–MS/MS sequencing and data analysis at the Korea Basic Science Institute. The detailed NanoElute settings, timsTOF Pro settings, and mass spectrometry data analysis are described25,26,27.
Protein–protein interaction networks functional enrichment analysis
Using identified metabolism-related proteins from each Aroclor 1254-induced rat or human S9, the STRING database (https://string-db.org/, version: 12.0) was employed to seek different protein–protein network compositions using the databases for Rattus norvegicus or Homo sapiens for the rat and human S9, respectively. Probes for which there was no information in the database were excluded. The most significant gene ontology and KEGG pathways18 enriched in the substantial terms and pathways were selected with the adjusted p-value threshold < 0.05, and the top five were sorted.
Preparation of the BaP-induced rat liver S9 fraction
All animal experiments were conducted by the Regulations Guide for the Care and Use of Laboratory Animals (published by the Institute for Laboratory Animal Research) and are reported in accordance with ARRIVE guidelines for the reporting of animal experiments. Ten-week-old specific pathogen-free female Sprague–Dawley (SD)/Crl: CD rats were purchased from Orient Bio Co., Korea. The animals were housed together in polycarbonate cages at room temperature (22 ± 3 °C) with a 12-h light/dark period. Gamma-ray-irradiated food and filtered water were provided ad libitum (#5053, LabDiet, USA). For treatment, the rats were randomly assigned five groups (n = 1/group) and administered corn oil-dissolved BaP via oral gavage at doses 20, 10, 5, 1, and 0 mg/kg body weight (bw) directly into the stomach. All animals were euthanized with CO2 overdose on day 4, and again 24 h after receiving treatment on day 3. About 3–4 g of left liver was collected and used to make an S9 fraction. Collected livers were washed in 1 mL/g 0.15 M KCL (pH 7.4) once and homogenized in 3 mL/g with a 100 μm mesh in 0.15 M KCL (pH 7.4). The homogenate obtained was centrifuged at 9000×g for 10 min. The prepared S9 fractions were aliquoted and stored at − 80 °C until use.
Animal welfare and regulatory compliance
The animal study was independently approved by the appropriate Institutional Animal Care and Use Committees (IACUC) and the Association for Assessment and Accreditation of Laboratory Animal Care International (AAALAC) at each participating institute and was conducted by the most recent version of the Korean Association of Laboratory Animal Science. Experimental animals were handled under a protocol approved by the Institutional Animal Care and Use Committee of the Korea Institute of Toxicology (IACUC No. 2105-0021).
Western blotting
Lysates from rat and human S9, each containing 30 μg protein, were resolved using an 8–16% precast polyacrylamide gel (Bio-Rad #BR4568104, USA) and subsequently transferred onto a 0.2 μm PVDF membrane (Bio-Rad #1704157, USA). After blocking with 5% non-fat dry milk in Tris-buffered saline with 0.1% Tween 20 (TBS-T, Tris 24.7 mM, NaCl 0.137 M, KCL 2.7 mM, pH 7.4, 0.1% Tween 20), the membranes were first incubated with the primary antibodies (CYP1a1; ab126887, CYP1a2; ab22717, CYP2b1 + 2b2; ab22719, CYP1b1; ab185954, CYP2d1; ab22590, CYP2e1; ab28146, CYP2d6; ab230472, CYP3a4; ab3572, Abcam biotechnology, UK) overnight at 4 °C and then incubated with a horse radish peroxidase (HRP)-labeled secondary antibody (anti-Goat IgG H&L; ab205723, anti-Rabbit IgG H&L; ab97051, Abcam, UK) at room temperature for 1 h. Finally, the signal bands were visualized and normalized using enhanced chemiluminescence. GAPDH was chosen as the protein loading control.
Statistical analysis
All values were expressed as mean ± standard deviations (SD) using GraphPad Prism 8.4.3. (GraphPad Software, Inc., USA) or Microsoft Excel 2016. No statistical analysis was conducted on the bacterial reverse mutation test results. The results were judged to be positive when the mean number of revertants in each concentration dose-dependently increased two-fold over the vehicle control for TA98 and TA100 or three-fold for TA1535, TA1537, and WP2uvrA.
Data availability
Proteomics data is provided within the supplementary information files.
References
Ames, B. N., Lee, F. D. & Durston, W. E. An improved bacterial test system for the detection and classification of mutagens and carcinogens. Proc. Natl. Acad. Sci. USA 70, 782–786. https://doi.org/10.1073/pnas.70.3.782 (1973).
Ames, B. N., McCann, J. & Yamasaki, E. Methods for detecting carcinogens and mutagens with the Salmonella/mammalian-microsome mutagenicity test. Mutat. Res. 31, 347–364. https://doi.org/10.1016/0165-1161(75)90046-1 (1975).
Gatehouse, D. et al. Recommendations for the performance of bacterial mutation assays. Mutat. Res. 312, 217–233. https://doi.org/10.1016/0165-1161(94)90037-x (1994).
Maron, D. M. & Ames, B. N. Revised methods for the Salmonella mutagenicity test. Mutat. Res. 113, 173–215. https://doi.org/10.1016/0165-1161(83)90010-9 (1983).
Mortelmans, K. & Zeiger, E. The Ames Salmonella/microsome mutagenicity assay. Mutat. Res. 455, 29–60. https://doi.org/10.1016/s0027-5107(00)00064-6 (2000).
OECD. Test No. 471: Bacterial Reverse Mutation Test (OECD iLibrary, 2020).
Bak, S. M. et al. Genotoxicity assessment of root extracts of Paeonia lactiflora Pall. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 886, 503579. https://doi.org/10.1016/j.mrgentox.2022.503579 (2023).
Escobar-Garcia, D. et al. S9 induction by the combined treatment with cyclohexanol and albendazole. Mutagenesis 16, 523–528. https://doi.org/10.1093/mutage/16.6.523 (2001).
Callander, R. D., Mackay, J. M., Clay, P., Elcombe, C. R. & Elliott, B. M. Evaluation of phenobarbital/beta-naphthoflavone as an alternative S9-induction regime to Aroclor 1254 in the rat for use in in vitro genotoxicity assays. Mutagenesis 10, 517–522. https://doi.org/10.1093/mutage/10.6.517 (1995).
Cox, J. A., Fellows, M. D., Hashizume, T. & White, P. A. The utility of metabolic activation mixtures containing human hepatic post-mitochondrial supernatant (S9) for in vitro genetic toxicity assessment. Mutagenesis 31, 117–130. https://doi.org/10.1093/mutage/gev082 (2016).
Bopp, S. K. et al. Regulatory assessment and risk management of chemical mixtures: Challenges and ways forward. Crit. Rev. Toxicol. 49, 174–189. https://doi.org/10.1080/10408444.2019.1579169 (2019).
Lei, X. et al. Liver damage associated with Polygonum multiflorum Thunb.: A systematic review of case reports and case series. Evid. Based Complement. Altern. Med. 2015, 459749. https://doi.org/10.1155/2015/459749 (2015).
Xia, X. H., Yuan, Y. Y. & Liu, M. The assessment of the chronic hepatotoxicity induced by Polygoni Multiflori Radix in rats: A pilot study by using untargeted metabolomics method. J. Ethnopharmacol. 203, 182–190. https://doi.org/10.1016/j.jep.2017.03.046 (2017).
Tran, H. N. K. et al. Analysis and stability test of the water extract and powder from Polygoni Multiflori Radix for toxicity study. Korean J. Pharmacogn. 51, 86–91 (2020).
Morooka, N., Nakano, S., Itoi, N. & Ueno, Y. The chemical structure and the mutagenicity of emodin metabolites. Agric. Biol. Chem. 54, 1247–1252. https://doi.org/10.1271/bbb1961.54.1247 (1990).
Hakura, A. et al. Salmonella/human S9 mutagenicity test: A collaborative study with 58 compounds. Mutagenesis 20, 217–228. https://doi.org/10.1093/mutage/gei029 (2005).
Kawaguchi, S., Nakamura, T., Tsuda, S., Murashige, R. & Sasaki, Y. Detection of in vitro genotoxicity of pro-mutagens using the comet assay under human and rat liver S9 fractions. MOJ Toxicol. 4, 255–261 (2018).
Kanehisa, M., Furumichi, M., Sato, Y., Kawashima, M. & Ishiguro-Watanabe, M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 51, D587–D592. https://doi.org/10.1093/nar/gkac963 (2023).
Schrenk, D. Impact of dioxin-type induction of drug-metabolizing enzymes on the metabolism of endo- and xenobiotics. Biochem. Pharmacol. 55, 1155–1162. https://doi.org/10.1016/s0006-2952(97)00591-1 (1998).
Kim, S. J. et al. Network-based toxicogenomic approach to explore oral benzo(a)pyrene exposure effect on respiratory system. Mol. Cell. Toxicol. 18, 521–529. https://doi.org/10.1007/s13273-022-00223-3 (2022).
Wang, M. et al. Emodin-induced hepatotoxicity is enhanced by 3-methylcholanthrene through activating aryl hydrocarbon receptor and inducing CYP1A1 in vitro and in vivo. Chemico-Biol. Interact. 365, 110089 (2022).
Li, X. et al. Revisiting the mutagenicity and genotoxicity of N-nitroso propranolol in bacterial and human in vitro assays. Regul. Toxicol. Pharmacol. 141, 105410. https://doi.org/10.1016/j.yrtph.2023.105410 (2023).
Androutsopoulos, V. P., Tsatsakis, A. M. & Spandidos, D. A. Cytochrome P450 CYP1A1: Wider roles in cancer progression and prevention. BMC Cancer 9, 187. https://doi.org/10.1186/1471-2407-9-187 (2009).
Jamwal, R. & Barlock, B. J. Nonalcoholic fatty liver disease (NAFLD) and hepatic cytochrome P450 (CYP) enzymes. Pharmaceuticals 13, 222. https://doi.org/10.3390/ph13090222 (2020).
Milev, M. P., Ravichandran, M., Khan, M. F., Schriemer, D. C. & Mouland, A. J. Characterization of staufen1 ribonucleoproteins by mass spectrometry and biochemical analyses reveal the presence of diverse host proteins associated with human immunodeficiency virus type 1. Front. Microbiol. 3, 367. https://doi.org/10.3389/fmicb.2012.00367 (2012).
Sandow, J. J., Infusini, G., Dagley, L. F., Larsen, R. & Webb, A. I. Simplified high-throughput methods for deep proteome analysis on the timsTOF Pro. bioRxiv https://doi.org/10.1101/657908 (2021).
Wan, X. et al. The MHC-II peptidome of pancreatic islets identifies key features of autoimmune peptides. Nat. Immunol. 21, 455–463. https://doi.org/10.1038/s41590-020-0623-7 (2020).
Acknowledgements
The authors would like to thank Prof. Byung Sun Min (Daegu Catholic University, Korea) for their help in PMR analyses and scientific comments.
Funding
This work was funded by the Korea Institute of Toxicology (NTIS No., 1711195885) and National Research Council of Science & Technology (NST) by the Korea government (MSIT) (No. CAP-21023-000).
Author information
Authors and Affiliations
Contributions
S.M.B. and S.M.B.: Methodology, Investigation, Data curation, Visualization, Writing-original draft. D.Y.K., S.J., N.Y.J., N.Y.K: Investigation, Data curation, Visualization. K.H.H., Y.B.K., B.S.L., J.H.P., H.J.C., H.G.L.: Project administration, Funding acquisition, Writing-review. O.O., S.K.K.: Project administration, Writing-review & editing. S.H.P.: Conceptualization, Writing, Writing-review & editing, Funding acquisition, Supervision. All authors commented on the manuscript and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bak, SM., Back, SM., Kim, D.Y. et al. Differential genotoxicity of Polygoni Multiflori in rat and human: insights from Ames test and S9 metabolic activation system. Sci Rep 14, 21433 (2024). https://doi.org/10.1038/s41598-024-72283-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-72283-5