Abstract
Male breast cancer (MBC) is a rare condition with unique characteristics compared to female breast cancer (FBC). Despite its scarceness, there is growing evidence that MBC should not be studied and treated as FBC due to factors like later diagnosis stage and distinct genetic makeup. Retrospective observational study in the EpiChron Cohort, selecting all the prevalent patients with breast cancer between 2010 and 2019. Logistic models were used to determine associated comorbidities. Between 2010 and 2019, 105 MBC and 11,657 FBC patients were found in the EpiChron Cohort. MBC patients had a high mean age at diagnosis and number of comorbidities. Paying attention to comorbidity prevalences in breast cancer patients, it was clear that MBC patients tended to be prone to cardio-metabolic coexisting diseases, while FBC patients were more prone to hormone-, bone- and mental diseases. There were nine chronic conditions associated to MBC patients, but after a year-by-birth matching only four associations remained. Two of them were associated previously [odds ratio (95% confidence interval)]: “Disorder of lipid metabolism” [1.65 (1.03–2.64)] and “Genitourinary symptoms and ill-defined conditions” [2.03 (1.07–3.87)]; and the other two were new, “Anxiety disorders” [2.05 (1.09–3.87)] and “Osteoporosis” [3.58 (1.26–10.14)]. After comparing associated comorbidities in FBC with those in MBC, it seems MBC patients share some of them, but they have their own particular set of coexisting diseases. In fact, once a year-by-birth matching was performed in MBC patient cohort, it was more obvious MBC comorbidities behave more similar to none-Breast-Cancer male population than to FBC patients. These findings highlight the distinct characteristics of the MBC patient population and the need for a tailored approach of managing MBC.
Similar content being viewed by others
Introduction
Male Breast cancer (MBC) is a rare condition, it accounts for less than 1% of all breast cancer in Spain and worldwide, as with Female Breast cancer (FBC) its incidence rate is steadily rising on an annual basis1,2,3. Due to its low prevalence, there is a lacking in prospective randomized clinical studies; historically male patients have been excluded from breast cancer clinical trials. Our current knowledge of MBC come from small retrospective studies, this is one of the reasons why MBC has been traditionally considered an analogous clinical entity to menopausal FBC4,5.
All the above has hampered to obtain useful and realistic knowledge regarding MBC characteristics and management, currently most treatment recommendations are extrapolated from FBC guidelines6. Nonetheless, there is an increasing evidence that MBC embodies its own distinct clinical identity, which requires its own particular considerations4,5,7. In fact, two specific histological subtypes have been described in MBC8, further supporting the aforementioned.
Most of the efforts for a better understanding of MBC have been focused to characterize sociodemographic, life-style and clinical differences between MBC and FBC patients and how those differences are associated to survivability and mortality. There are certain features of MBC well described in the literature. For instance, MBC patients tend to be diagnosed at older age, with a more advance tumour stage, with higher number of co-existing pathologies and with hormone-positive phenotype in comparison with their female counterparts. In reality, most of MBC patients are usually progesterone positive, estrogen positive and epidermal growth factor receptor negative. This hormone profile is associated with poorer prognosis2,3,9,10,11.
Breast cancer is a complex multifactorial disease, and as such, there seem to be genomic factors modulating its appearance and evolution. For instances, mutations in BRCA2 and BRCA1 are presented in around 16% of all MBC cases, increasing an 8% and a 2% respectively the risk of MBC development versus the general population with wild type genes with just 0.1%. There are other found genes that may influence appearance and evolution of breast cancer in a lighter way12. Other risk factor worthy to be mentioned are family history of breast cancer, strengthening the genomic background relevance; breast cancer in closed-degree relative has been associated with a high increased odds of MBC13.
Regarding treatment, MBC patients seem to mostly undergo mastectomy and they tend to be nonadherent to adjuvant endocrine therapy14,15. Nevertheless, it appears there are certain surgical treatments with better outcomes, but all of them have similar survival rates comparing with FBC once adjusted by treatment9,10,16,17.
On the other hand, available data of survivability in MBC patients suggest they have worse results than FBC in general, most likely due to the older age of diagnosis, the higher burden of multimorbidity and the advance tumour stage18,19,20. Remarkably, little is known about associated comorbidities to MBC, which may influence heavily survivability; and which ones differ from the general population or its female counterpart, information relevant enough to modulate the treatment itself of MBC patients. As far as we know up to the date, only Zoorob et al.(2019) have tried to elucidate this association and the differences between MBC and FBC patients in a set list of 20 chronic pathologies21. Other few studies have described the frequency of small fixed lists of chronic conditions without determining associations3,9,22, and lastly, in the vast majority of cases when talking about multimorbidity in MBC patients they choose some kind of index to assess disease number or multimorbidity burden without further disaggregation8,9,14,16,17,20,23,24,25,26. Despite the lack of knowledge in this matter, characterizing comorbidities associated to MBC patients is fundamental for a better management of their health and increasing chances of survival in their complex situation, as previous studies have widely seen that high multimorbidity burden leads to poorer cancer outcomes.
Bearing all above in mind, this study aimed to analyze the association of breast cancer with other comorbidities and to compare those associated comorbidities to those found in a general population of men without breast cancer and in a population of female breast cancer patients.
Methods
Study design and population
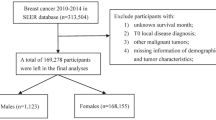
We conducted a retrospective, observational study in the EpiChron Cohort, which contains anonymized sociodemographic and clinical information of all users of the public health care system in the Spanish region of Aragon. Detailed description and data-linkage method of the EpiChron Cohort can be found elsewhere27. The total general population for this study comprised all individuals with at least one year of activity in the Health System and at least one chronic condition between 2010 and 2019 (1,136,624 individuals; 529,683 men and 606,941 women), almost 90% of the total population of Aragon region (1.3 M individuals).
For the breast cancer cohorts, all prevalent cases of breast cancer between 2010 and 2019 in men (105 men) and women (11,657 women) aged 18 years and older were selected. Patients with breast cancer were identified as those with an active diagnosis of breast cancer during the study period recorded in their primary or hospital electronic health records. All codes under the 24 code (Cancer of breast) of the Clinical Classification Software (CCS) were selected. Specifically, the following ICD9 diagnosis codes were considered by CCS: 174.0, 174.1, 174.2, 174.3, 174.4, 174.5, 174.6, 174.8, 174.9, 175.0, 175.9, 233.0 and V103. No other inclusion or exclusion criteria were applied.
Additionally, a small matched sample of male patients without breast cancer diagnosis (210 men) was selected to compare disease association.
Ethical considerations
The Clinical Research Ethics Committee of Aragón (CEICA) approved this study (PI17/0024). CEICA waived the need of obtaining the informed consent due to the use of anonymized data and the epidemiological approach used. This research was performed in accordance with the Declaration of Helsinki.
Study variables
For all MBC patients, we analysed age at breast cancer diagnosis, residency (urban/rural), all chronic diseases that the patient had registered in the studied period, number of chronic diseases at diagnosis and multimorbidity state (yes/no).
The diagnosis codes were originally coded according to the International Classification of Primary Care, 2nd edition (ICPC-2) or the International Classification of Diseases, 9th edition (ICD-9), depending on the source of the data (primary or hospital care). In order to reduce the number of different diagnosis codes, we transformed the ICPC-2 codes into ICD-9 codes using the conversion developed by the Navarra Institute of Public and Labour Health (8th edition)28, then we used the Agency for Healthcare Research and Quality’s Clinical Classification Software to group ICD-9 codes, particularly we used the single level category29. Then, we filtered out all non-chronic conditions using the Chronic Condition Indicator software tool, resulting in 161 chronic mutually exclusive categories30. Multimorbidity was defined as the presence of two or more chronic diseases after this reclassification process. For all populations, prevalence of the different CCS codes was analysed.
Statistical analysis
For the descriptive analysis, we presented continuous data by their mean and standard deviation and categorical data by their frequency and proportion.
For the characterization of comorbidities, firstly no matching by age was performed in the comparison with the FBC population, so odds ratios (OR) were calculated by using the whole population without breast cancer for their respective sex, the comorbidity results were compared between MBC and FBC. For the second comparison, a matching procedure was performed in a ratio 1:2, using birth year as matching variable, MBC patients were matched with male patients without breast cancer, a small population of 315 individuals in total. Conditional logistic regression models were used to calculate OR and their confidence interval of prevalence for each comorbidity according to the presence or absence of breast cancer in each population. OR were adjusted by age. All p-values were two-sided and adjusted by age, results with adjusted p-values < 0.05 were considered statistically significant. All the analysis was made in STATA 12.0.
Data visualization was performed using Microsoft Excel version 1808; for the frequency tables and using ggplot2 v3.4.2 in R v4.3.0; for the bar plots.
Results
Characteristics of male breast cancer patients
Between 2010 and 2019, 105 MBC patients were identified in EpiChron Cohort, their mean age at diagnosis was 65.62 ± 12.02 years [Mean ± Standard deviation]. Half of all MBC patients had died during the study period and 60 of them (57.14%) lived in an urban area. Almost all of them (more than 90%) were over 45 years old and with multimorbidity. Notoriously, more than half of all MBC patients (52.38%) had six or more chronic conditions at breast cancer diagnosis time and, in general, the mean number of chronic diseases presented in the population was 5.7 ± 3.17, without considering breast cancer diagnosis (Table 1).
Most frequent comorbidities in breast cancer patients
The most frequent comorbidities for breast cancer patients are shown in Fig. 1. “Hypertension”, “Genitourinary symptoms and ill-defined conditions” and “Delirium, dementia, and amnestic and other cognitive disorders” were shared similarly in proportion between male and female breast cancer populations. Nevertheless, in MBC patients there were some pathologies more frequently presented, such as “Disorders of lipid metabolism”, “Other nutritional, endocrine, and metabolic disorders”, “Diabetes Mellitus”, “Cardiac dysrhythmia”, “Other ear and sense organ disorders”, “Coagulation and haemorrhagic disorders” and “Acute myocardial infraction”. On the other hand, FBC patients tended to suffer more “Anxiety disorders”, “Osteoarthritis”, “Thyroid disorders”, “Depression and mood disorders”, “Osteoporosis”, “Headache; including migraine”, “Spondylosis; intervertebral disc disorders; other back problems” and “Menopausal disorders”. Around 15% of MBC cases suffered from “Hyperplasia of prostate” (all prevalences can be found in Table 2).
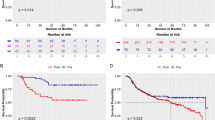
In Tables 3 and 4 the results for men and women of the conditional logistic model after adjusting by age can be checked, nine pathologies showed modified risk chances in MBC patients in comparison to the general male population. MBC patients had less risk of “Hypertension” [0.62 (0.41–0.93)] [OR (95% CI)]. In contrast, these patients had more risk than male population of “Anxiety disorders” [1.65 (1.03–2.65)], “Asthma” [2.66 (1.23–5.77)], “Heart valve disorders” [2.99 (1.31–6.85)], “Aortic; peripheral; and visceral artery aneurysms” [3.39 (1.24–9.28)], “Epilepsy; convulsions” [3.43 (1.26–9.31)], “Osteoporosis” [4.26 (2.2–8.24)], “Other endocrine disorders” [7.77 (2.46–24.58)] and “Other diseases of veins and lymphatics” [23.12 (8.45–63.25)] (Tables 3 and 4). Women with FBC also had less risk of “Hypertension”, but this risk also decreased with other comorbidities like “Genitourinary symptoms and ill-defined conditions”, “Headache; including migraine” or “Congestive heart failure; nonhypertensive”.
Comparison with age-matched population
The aforementioned relationships were checked in a case-control sample to confirm their validity and reduce biases. For that purpose, a matched-by-birth-year population of male breast patients without breast cancer diagnoses were selected. Only four diseases remained associated in this scenario, two of them not previously associated, “Disorder of lipid metabolism” [1.65 (1.03–2.64)] and “Genitourinary symptoms and ill-defined conditions” [2.03 (1.07–3.87)]; and the other two had been already associated, “Anxiety disorders” [2.05 (1.09–3.87)] and “Osteoporosis” [3.58 (1.26–10.14)] (Table 5).
Discussion
Our MBC population is mostly old with high number of chronic conditions, which is in accordance with previously seen in the literature, independently if we are referring to a Western or Eastern country3,5,10,11,14,18,20,21,23,26,31. The fact that they have a greater number of comorbidities is a factor to be taken into account, since a greater number of comorbidities has been related to a worse prognosis14, along with other factors like poor access to health care, older age and black race11,18,19.
The difference in the prevalence of comorbidities between MBC and FBC was observed previously3,11,22. Men are described to have more comorbidities than women3,11,21, and some diseases like diabetes, chronic obstructive pulmonary disease (COPD), chronic kidney disease and liver cirrhosis are more frequent in men, whereas female patients are more likely to suffer from autoimmune diseases22. The higher rate of comorbidities in MBC cases may be associated to the higher median age of MBC cases comparing with FBC3.
Between 2010 and 2019, the five most prevalent comorbidities in men in our cohort were “Disorders of lipid metabolism”, “Hypertension”, “Other nutritional; endocrine; and metabolic disorders”, “Depression and mood disorders”, “Diabetes Mellitus” and “Anxiety disorders”, Shimomura et al. observed similar results to us, with more prevalence of diabetes and cardiovascular disease3. Furthermore, our results seem to be in accordance with those from Zoorob et al. Despite using only a set of 20 chronic conditions; their top five most prevalent comorbidities were the same as ours, except for the presence of “Arrythmia” instead of “Other nutritional disorders”21.
From this descriptive analysis, there seem to be a difference at least in the nature of the most frequent diseases between MBC and FBC; MBC patients tend to suffer more of cardiometabolic diseases in contrast with FBC patients who presented more hormone-, bone- and mental comorbidities. It might be useful for a proper management of their diseases to act in tailored manner regarding the most common MBC patient’s comorbidities, as they are thought to impact the overall risk of developing second primary cancer22.
Regarding the association analysis, initially nine diseases were linked to MBC. Nevertheless, most of them are presented in a very low number of MBC patients. “Hypertension”, “Anxiety disorder” and “Osteoporosis” account for 58, 22 and 10 cases respectively, greater MBC cohort numbers are needed to confirm these findings. Furthermore, after matching by year of birth, only four of those associations remained. “Disorder of lipid metabolism” and “Genitourinary symptoms and ill-defined conditions” were added to the before mentioned associations.
Firstly, “Hypertension” [0.62 (0.41–0.93)] was the only disease to have a negative association, this finding should be taken with special care, as to the low quantity of cases, lack of specific MBC literature and mix results of this association in FBC patients3,21,32 increases its uncertainty of an actual association. In fact, in our case once we matched by age, this association disappeared. The mechanisms proposed for the relationship between hypertension and breast cancer risk are the common pathophysiological pathway mediated by adipose tissue, which could cause chronic inflammation, the modification in the apoptosis caused by hypertension, and the use of calcium channel blockers32.
Secondly, breast cancer is well documented to generate psychological distress to female patients, depending on several factors, such as prognosis, tumour state, patient’s personal circumstance; their mental health might worsen in a lighter or heavier manner. A positive association of MBC with “Anxiety disorder” seems more than plausible and clear33. In addition, a study in the United States observed that the prevalence of depression was higher in MBC and FBC patients than in the general population, with a greater gradient between number of comorbidities and the odds of depression21. Nevertheless, FBC and MBC patients might react different to the psychological distress, as FBC patients appear to suffer less from “Anxiety disorders” and more from “Depression and mood disorders” than MBC patients, further concise research is needed.
Thirdly, bone health has been described to be negatively affected by endocrine therapy and adjuvant settings in certain cases in FBC and male prostate cancer patients with similar treatments, it is plausible that these increased chances of “Osteoporosis” in our MBC and FBC cohorts are cancer treatment-related comorbidity34, thus, actually associated, even though there is no possibility to determine if it is due to the disease or the treatment effect.
Fourthly, dyslipidaemia was more frequent in MBC patients, and it is important to control this disease properly because deregulation of lipid metabolism has been seen to increase proliferation, chemoresistance and invasiveness of breast cancer, leading to worsen outcomes and complications35,36,37. In addition, this deregulation generates an enhancing microenvironment for BC tumours proliferation and selection of chemoresistant cells35,37.
Lastly, “Genitourinary symptoms and ill-defined conditions” refers to a broad group of events related to the urinary tract, as with the case of “Osteoporosis” it might be related to BC medication and the older age of this kind of patients. The higher risk of genitourinary symptoms and MBC may be related to the associated risk between cancers of the breast and prostate, because BCRA2 mutations and estrogen treatment used in the prostate cancer38. Also, it has been showed that the incidence of urinary symptoms, like urinary incontinence, in patients with early-stage breast cancer may be higher than in the general population related to endocrine adjuvant therapy, and is questioned if the risk factors of developing urinary incontinence and breast cancer overlap39.
When compared to the age-matched population, the MBC cohort exhibited a similar pattern of comorbidities. This finding suggests that, from a comorbidity perspective, MBC patients may resemble to their non-cancerous counterparts of a similar age group. However, the presence of breast cancer itself may interact with these pre-existing conditions, potentially influencing treatment decisions and overall prognosis. Regarding prognosis, it is well-known that MBC patients have higher risk of cancer recurrence and similar overall survival than FBC patients, at least in later tumour stages40,41. Nevertheless, once comorbidities are taken into account, the recurrence, overall survival and breast-cancer specific mortality seems to worsen in FBC patients with high comorbidity burden, it is plausible this issue affect similarly to MBC patients42. Furthermore, it appears that specific comorbidities, such as anxiety and depression, are associated with poorer prognosis in all aspects (recurrence, overall survival and cancer-specific mortality)43. In regards of treatment, FBC patients with high comorbidity were associated with reduced usage of different treatments (mastectomy, lumpectomy + radiation, and chemotherapy) in regards of their tumour stage44. Additionally, pre-existing conditions not only might affect breast cancer treatment decision, but also the concomitant medication of those comorbidities might influence positively or negatively the prognosis of breast cancer45.
All these findings highlight the distinct characteristics of the MBC patient population, particularly regarding their high burden of comorbidities. The traditional approach of extrapolating treatment guidelines from FBC to MBC may not be optimal, given the differences in the associated comorbidity profiles. Our study underscores the need for a more tailored approach to managing MBC, considering the unique challenges posed by co-existing chronic conditions. Future research should focus on developing evidence-based treatment strategies that address the specific needs of the MBC population while accounting for their complex comorbidity landscape.
Data availability
The data used in this study cannot be publicly shared because of restrictions imposed by the data owner (i.e., Aragon Health Sciences Institute—IACS) due to the existence of potentially identifying patient information. This restriction has been asserted by the Clinical Research Ethics Committee of Aragón (CEICA). The authors who accessed the data belong to the EpiChron Research Group of IACS and received permission from IACS to utilise the data for this specific study. The EpiChron Group can establish future collaborations with other groups based on the same data. However, each new project based on these data must be previously submitted to the CEICA to obtain the respective mandatory approval. Potential collaborations should be addressed to the Principal Investigator of the EpiChron Research Group at [email protected].
References
Zheng, G. et al. Familial associations of male breast cancer with other cancers. Breast Cancer Res. Treat.166, 897–902 (2017).
Yao, N. et al. Clinicopathologic characteristics and prognosis for male breast cancer compared to female breast cancer. Sci. Rep. [Internet] (2022). https://doi.org/10.1038/s41598-021-04342-0
Shimomura, A. et al. Clinicopathological features of male patients with breast cancer based on a nationwide registry database in Japan. Breast Cancer29, 985–992 (2022).
Zheng, G. & Leone, J. P. Male breast cancer: An updated review of epidemiology, clinicopathology, and treatment. Breast Cancer [Internet] (2022). https://doi.org/10.1155/2022/1734049
Longo, D. L. & Giordano, S. H. Breast Cancer in Men. N. Engl. J. Med.378, 2311–2320 (2018).
Hassett, M. J. et al. Management of male breast cancer: ASCO guideline. J. Clin. Oncol.38, 1849–1863 (2020).
Leon-Ferre, R. A. et al. A contemporary review of male breast cancer: Current evidence and unanswered questions. Cancer Metastas. Rev.37, 4 (2018).
Johansson, I. et al. Gene expression profiling of primary male breast cancers reveals two unique subgroups and identifies N-acetyltransferase-1 (NAT1) as a novel prognostic biomarker. Breast Cancer Res. BCR [Internet] (2012).
Bender, P. F. M. et al. Men and women show similar survival rates after breast cancer. J. Cancer Res. Clin. Oncol.143, 563–571 (2017).
Konishi, T. et al. Comparison of short-term surgical outcomes between men and women with breast cancer: A retrospective study using nationwide inpatient data in Japan. Breast Cancer Res. Treat.186, 731–739 (2021).
Elimimian, E. B. et al. Male breast cancer: A comparative analysis from the national cancer database. World J. Men’s Health [Internet] (2021).
McClurg, D. P. et al. Analysis of the clinical advancements for BRCA-related malignancies highlights the lack of treatment evidence for BRCA-positive male breast cancer. Cancers (Basel). 14, 3175 (2022).
Calip, G. S. et al. Family history of breast cancer in men with non-BRCA male breast cancer: Implications for cancer risk counseling. Breast Cancer Res. Treat.185, 195–204 (2021).
Yadav, S. et al. Male breast cancer in the United States: Treatment patterns and prognostic factors in the 21st century. Cancer. 126, 26–36 (2020).
Oke, O., Niu, J., Chavez-MacGregor, M., Zhao, H. & Giordano, S. H. Adjuvant tamoxifen adherence in men with early-stage breast cancer. Cancer. 128, 59–64 (2022).
Konduri, S., Singh, M., Bobustuc, G., Rovin, R. & Kassam, A. Epidemiology of male breast cancer. Breast. 54, 8–14 (2020).
Lin, A. P., Huang, T. W. & Tam, K. W. Treatment of male breast cancer: Meta-analysis of real-world evidence. Br. J. Surg.108, 1034–1042 (2021).
Parise, C. A. & Caggiano, V. The association of race/ethnicity in male breast cancer survival within similar comorbidity cohorts. Cancer. 129, 750–763 (2023).
Ellington, T. D., Henley, S. J., Wilson, R. J. & Miller, J. W. Breast cancer survival among males by race, ethnicity, age, geographic region, and stage—United States, 2007–2016. MMWR Morb. Mortal. Wkly. Rep.69, 1481–1484 (2020).
Sarmiento, S. et al. Male breast cancer: A closer look at patient and tumor characteristics and factors that affect survival using the National Cancer Database. Breast Cancer Res. Treat.180, 471–479 (2020).
Zoorob, R. J., Salemi, J. L., Mejia de Grubb, M. C., Modak, S. & Levine, R. S. A nationwide study of breast cancer, depression, and multimorbidity among hospitalized women and men in the United States. Breast Cancer Res. Treat.174, 237–248 (2019).
Hung, M. H. et al. Risk of second non-breast primary cancer in male and female breast cancer patients: A population-based cohort study. PLoS ONE. 11, 1–12 (2016).
Linehan, E. S., Samant, N. D. & Rabbani, J. W. Examining racial disparities in male breast cancer. J. Clin. Oncol.39, 6555–6555 (2021).
Liu, F. C. et al. Epidemiology and survival outcome of breast cancer in a nationwide study. Oncotarget. 8, 16939–16950 (2017).
Reiner, A. S., Navi, B. B., DeAngelis, L. M. & Panageas, K. S. Increased risk of arterial thromboembolism in older men with breast cancer. Breast Cancer Res. Treat.166, 903–910 (2017).
Sun, H. F. et al. Clinicopathological characteristics and survival outcomes of male breast cancer according to race: A SEER population-based study. Oncotarget. 8, 69680 (2017).
Prados-Torres, A. et al. Cohort profile: The epidemiology of chronic diseases and multimorbidity. The EpiChron Cohort Study. Int. J. Epidemiol.47, 382e–4e (2018).
Ancín Ducay, J. M., Erce Lopez, S., Extramiana Cameno, E. & Izcue Argandoña, A. Correlación de códigos CIE-9-MC (8a edic)—CIAP-2 para la gestión de Incapacidad Temporal [Internet]. Instituto de Salud Pública y Laboral de Navarra; 2014 [cited 2023 Oct 14]. https://www.navarra.es/NR/rdonlyres/E520399C-0612-4C75-A912-B16295014FC3/281429/codigosCIE_9_MC.pdf
Agency for Healthcare Research and Quality. Clinical Classifications Software (CCS) for ICD-9-CM [Internet]. Healthcare Cost and Utilization Project (HCUP). 2015 [cited 2023 Aug 1]. www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp
Chronic Condition. Indicator (CCI) for ICD-9-CM [Internet]. [cited 2023 Aug 24]. https://hcup-us.ahrq.gov/toolssoftware/chronic/chronic.jsp
Thuler, L. C. S. & Bergmann, A. Male breast cancer: Clinical-epidemiological characteristics of 1189 Brazilian patients. Aging Male. 18, 118–123 (2015).
Han, H. et al. Hypertension and breast cancer risk: A systematic review and meta-analysis. Sci. Rep.7, 44877 (2017).
Dinapoli, L., Colloca, G., Di Capua, B. & Valentini, V. Psychological aspects to consider in breast cancer diagnosis and treatment. Curr. Oncol. Rep.23, 38 (2021).
Rachner, T. D., Coleman, R., Hadji, P. & Hofbauer, L. C. Bone health during endocrine therapy for cancer. Lancet Diabetes Endocrinol.6, 901–910 (2018).
Liu, W. et al. Dysregulated cholesterol homeostasis results in resistance to ferroptosis increasing tumorigenicity and metastasis in cancer. Nat. Commun.12, 5103 (2021).
González-Ortiz, A., Galindo-Hernández, O., Hernández-Acevedo, G. N., Hurtado-Ureta, G. & García-González, V. Impact of cholesterol-pathways on breast cancer development, a metabolic landscape. J. Cancer. 12, 4307–4321 (2021).
Zipinotti dos Santos, D. et al. The impact of lipid metabolism on breast cancer: A review about its role in tumorigenesis and immune escape. Cell. Commun. Signal.21, 161 (2023).
Karlsson, C. T., Malmer, B., Wiklund, F. & Grönberg H. Breast cancer as a second primary in patients with prostate cancer—estrogen treatment or association with family history of cancer? J. Urol.176, 538–543 (2006).
Chung, C. P., Behrendt, C., Wong, L., Flores, S. & Mortimer, J. E. Serial Assessment of urinary incontinence in breast Cancer survivors undergoing (neo)adjuvant therapy. J. Natl. Compr. Canc. Netw.18, 712–716 (2020).
Greif, J. M., Pezzi, C. M., Klimberg, V. S., Bailey, L. & Zuraek, M. Gender differences in breast cancer: Analysis of 13,000 breast cancers in men from the National Cancer Data Base. Ann. Surg. Oncol.19, 3199–3204 (2012).
Scomersi, S. et al. Comparison between male and female breast cancer survival using propensity score matching analysis. Sci. Rep.11, 11639 (2021).
Land, L. H., Dalton, S. O., Jensen, M-B. & Ewertz, M. Impact of comorbidity on mortality: A cohort study of 62,591 Danish women diagnosed with early breast cancer, 1990–2008. Breast Cancer Res. Treat.131, 1013–1020 (2012).
Wang, X. et al. Prognostic value of depression and anxiety on breast cancer recurrence and mortality: A systematic review and meta-analysis of 282,203 patients. Mol. Psychiatry. 25, 3186–3197 (2020).
Parise, C. A. & Caggiano, V. The influence of comorbidity on treatment and survival of triple-negative breast cancer. Breast J.26, 1729–1735 (2020).
Dumas, E. et al. Concomitant medication, comorbidity and survival in patients with breast cancer. Nat. Commun.15, 2966 (2024).
Acknowledgements
This research was funded by the Carlos III Institute of Health, Ministry of Science and Innovation (Spain), through the Network for Research on Chronicity, Primary Care, and Health Promotion (RICAPPS), awarded for the call for the creation of Health Outcomes-Oriented Cooperative Research Networks (grant number RD21/0016/0019). This research was also funded by Gobierno de Aragón (grant number B01_23R) and funded by European Union’s Next Generation EU funds.
Limitations
As with the majority of secondary-use clinical real-world-data based studies, our results are subjected to several limitations. The data used are extracted from the daily clinical practice, some level of inconsistency and low reliability in the diagnosis may be possible. The small sample size of male breast cancer patients, due to its rareness, may decrease the observed differences, but show the differences between patient profiles. In addition, there is a lack of potential explanatory variables not considered by this research, like lifestyle habits that could influence in the prevalence of some comorbidities or cancer prognosis that is related to mental health disorders. Lastly, the gap in knowledge of the literature hinders comparability with previous studies. Studies with bigger sample sizes of male patients with breast cancer are needed to strengthen our knowledge in this matter. These studies should also take into account and analyse the role of potential influencing and confounding socio-demographic and clinical factors such as socioeconomic status, lifestyle habits, environmental factors, tumour characteristics, or genetic factors. Future studies analysing the differences in the comorbidity profile and survival between MBC and FBC are encouraged to improve our knowledge about this clinical entity and to identify potential differences between men and women that could justify the revision and adaptation of the clinical practice guidelines currently available for this condition. The ultimate goal of all this would be to adopt a person-centred care approach to improve the treatment, care, prognosis and quality of life of these patients.
Author information
Authors and Affiliations
Contributions
Conceptualization: A.S.M. , D.A.L., M.C.C.F., R.I.C.; Data curation and Formal Analysis: C.L.B; Methodology: B.P.P., C.L.B; Project Administration: A.G.M.; Visualization: A.S.M.; Writing – original draft: A.S.M.; Writing – review & editing: A.S.M., A.M.J., C.L.B., D.A.L., M.C.C.F., R.I.C.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Santos-Mejías, A., Moreno-Juste, A., Laguna-Berna, C. et al. Unveiling the comorbidity burden of male breast cancer. Sci Rep 14, 22977 (2024). https://doi.org/10.1038/s41598-024-73032-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-73032-4