Abstract
Nutritional status assessment has been deemed essential in treating elderly cancer patients. This study aims to investigate and compare the prognostic value and clinical utility of pre-treatment nutritional indicators in elderly rectal cancer (RC) patients. We retrospectively collected data from 361 elderly rectal cancer patients. The optimal cut-off values for pre-treatment nutritional indicators were calculated using ROC curve analysis. Univariate and multivariate Cox analyses were conducted to identify independent prognostic nutritional indicators. The predictive performance and clinical utility of these independent nutritional indicators was evaluated using time-dependent ROC. Multivariate analyses showed that body mass index (BMI), prognostic nutritional index (PNI), geriatric nutrition risk index (GNRI), and platelet-albumin ratio (PAR) independently predicted overall survival and progression-free survival in elderly RC patients (all p < 0.05), except for advanced lung cancer inflammation index (ALI). According to the nomogram model, the pre-treatment nutritional prognosis score was calculated and the patients were risk stratified. The KM curve showed that the survival of the high-risk group was significantly worse than that of the low-moderate risk group. Time-dependent ROC indicated that novel nutritional prognostic indicator (NNPI) had the best predictive ability compared with the independent prognostic nutritional indicator. Subgroup analysis also showed that NNPI had prognostic value across different clinical factors and had significant clinical utility. In elderly RC patients, BMI, PNI, GNRI, PAR, and NNPI serve as objective assessment tools for nutrition-related mortality risk. Identifying elderly patients at higher nutritional risk can guide early clinical nutritional interventions and improve patient outcomes.
Similar content being viewed by others
Introduction
Rectal cancer (RC) is one of the most common malignant tumors globally, with its incidence showing an increasing trend1. With the improvement of living standards and medical levels, the proportion of elderly patients with RC is gradually increasing. According to statistics, the median age at diagnosis of RC is around 63 years, with elderly RC patients accounting for 44%2. Despite significant advancements in treatment modalities3, the mortality rate remains relatively high among elderly RC patients. Part of the reason is that elderly patients often have poor nutritional status, which significantly increases the risk of complications in surgical procedures, chemotherapy, and other treatment regimens, reduces treatment tolerance, and thereby impacts the smooth progress of treatment4. 10–20% of cancer patients die as a result of malnutrition rather than the tumor itself, as malnutrition can impact the progression of cancer and treatment response5,6. However, in clinical practice, its significance is often underestimated due to a lack of effective nutritional risk screening tools7.
Numerous studies have shown that cancer progression and metastasis depend not only on factors such as tumor type, differentiation status, treatment approaches, and staging8 but also significantly on the nutritional status of patients9,10,11. Various nutrition-related indicators, including body mass index (BMI), platelet-albumin ratio (PAR), the prognostic nutritional index (PNI), the geriatric nutrition risk index (GNRI), and the advanced lung cancer inflammation index (ALI) have emerged as valuable predictors of prognosis in RC. While serum albumin and BMI have traditionally been used to assess nutritional status in cancer patients, including RC12,13. Recent studies have highlighted the significance of a low PNI and a high PAR, incorporating serum albumin with lymphocytes or platelets, as prognostic markers for RC14,15. Similarly, Research indicates that a low GNRI is associated with poorer overall and cancer-specific survival across multiple human cancers16,17. ALI has also been shown to be associated with poor prognosis in patients with colorectal cancer18. Notably, these nutrition-related indicators can be accurately assessed using objective clinical data such as weight, height, albumin levels, lymphocyte counts, platelets counts, and more. This simple and objective approach to monitoring the nutritional status of elderly individuals should be widely implemented in clinical practice.
Elderly individuals constitute a fragile and diverse patient cohort, with a heightened risk of malnutrition, particularly among those with malignant tumors. Therefore, it is imperative to assess the nutritional risk of elderly RC patients before treatment to provide appropriate nutritional support, reduce malnutrition-associated mortality, and prolong survival. This study aimed to investigate the relationship between pre-treatment nutrition-related parameters and the prognosis of elderly RC patients undergoing comprehensive treatment. Additionally, we developed a novel nutritional prognostic index (NNPI) and constructed a nomogram model. We also compared the prognostic abilities of different nutritional prognostic indicators and the NNPI. Lastly, based on the nomogram score of independent nutritional risk factors, we calculated the pre-treatment nutritional prognostic score (PNPS) and stratified the patients according to their nutritional risk levels.
Materials and methods
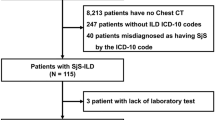
Patients
From 2014 to 2020, a total of 361 elderly patients with RC who received treatment at our institution were included in this study. We define elderly patients as those aged 60 years and older for several reasons. Firstly, according to statistics, the median age of RC diagnosis is approximately 63 years2. Secondly, research has shown a trend toward younger age at diagnosis for RC19,20. Thirdly, the World Health Organization (WHO) defines the elderly as those aged 60 years and above21. Additionally, a review of the relevant literature suggests that 60 years is a commonly used age threshold in studies22,23. Therefore, we believe that using age 60 as the cutoff would better encompass this high-risk population. The inclusion criteria were as follows: (i) aged 60 years or older; (ii) histologically confirmed as RC; (iii) TNM stages I-III; (iv) no distant metastasis or other primary tumors; (v) karnofsky performance status points ≥ 70 points. Exclusion criteria were: (i) severe hematologic disorders or hepatic/renal dysfunction; (ii) incomplete clinical and pathological data; (iii) loss to follow-up. Ultimately, 361 elderly RC patients met the aforementioned criteria. In this study, we used the eighth edition of the TNM staging system published by the American Joint Committee on Cancer (AJCC) to evaluate the staging of patients24,25. This study adhered to the Helsinki Declaration and was approved by the Ethics Committee of the Fujian Cancer Hospital.
Treatment
According to guidelines, the main treatment for stage I-II patients is surgical intervention, followed by adjuvant therapy based on postoperative pathological findings. For stage III patients, the predominant treatment approach is a combination of neoadjuvant therapy, surgery, and postoperative adjuvant therapy. The adjuvant chemotherapy regimens utilized include FOLFOX/mFOLFOX (oxaliplatin + fluorouracil + leucovorin) and CAPEOX/XELOX (oxaliplatin + capecitabine). Patients are monitored for complete blood count and biochemical parameters before and after treatment, with chemotherapy doses adjusted according to the patient’s side effects and tolerance. Neoadjuvant radiotherapy consists of either long-course radiotherapy (45–50.4 Gy/25–28 fractions) or short-course radiotherapy (25 Gy/5 fractions). Postoperative radiotherapy is tailored based on each patient’s pathological findings after surgery.
Data collection
Patient age, sex, TNM staging, carcinoembryonic antigen (CEA) levels, mesorectal fascia involvement (MRF), extramural vascular invasion (EMVI), perineural invasion, tumor deposits, tumor size, pre-treatment complete blood count, and comprehensive biochemical data were retrospectively collected from the medical records system of our center. The above data were all for patients before treatment.
Calculation of nutritional indicators before treatment
Nutritional indicators were calculated based on the acquired clinical data using the following formula: BMI = weight (kg)/height2 (m); PNI = 5*lymphocyte count + albumin level; GNRI = 1.489 × albumin + 41.7 × present body weight (PBW)/ideal body weight (IBW) [(IBW was determined using the formula: height (m2) * 22 (kg/m2). When PBW exceeded IBW, the ratio of PBW/IBW was set to 1); PAR = absolute platelet count/albumin level; ALI = BMI* albumin/NLR; NLR = absolute neutrophil count/absolute lymphocyte count.
Endpoints and follow-up
The primary endpoint of the study is overall survival (OS). OS is defined as the duration from diagnosis to death or the last visit. Because of the value of progression-free survival (PFS) in assessing treatment effect and patient prognosis, we also analyzed PFS as a secondary end point in this study. PFS is defined as the duration from diagnosis to disease progression, death, or the last visit. Disease progression was assessed based on clinical imaging, tumor markers, and clinical symptoms. Disease progression included locoregional recurrence and distant metastasis. Generally, the follow-up strategy for patients with RC after treatment is as follows: within the first year post-treatment, appointments are typically scheduled every 3 months; in the second and third years, the frequency reduces to every 6 months; in the subsequent years, it becomes annually. The last follow-up for this study was conducted in June 2023.
Statistical analysis
All analyses were performed using IBM SPSS software (version 26.0), R software (version4.1.0). A double-tailed p value < 0.05 was considered statistically significant. Optimal cutoff values for age, tumor size, BMI, PNI, GNRI, PAR, and ALI were estimated using the X-tile software. Kaplan–Meier curve was used to draw OS and PFS, and log-rank test was used for comparison. Univariate and multivariate Cox analysis was used to evaluate the relationship between pre-treatment nutrition-related indicators and prognosis in elderly patients with RC. Construct a nomogram prognostic model and evaluate its efficacy with calibration curve and decision curve. Then, time-dependent ROC (time-ROC) was used to evaluate the predictive power of nutrition-related prognostic indicators. Finally, restricted cubic splines (RCS) were used to assess the relationship between nutrition-related indicators and survival outcomes.
Results
Clinical characteristics
We ultimately enrolled 361 elderly patients with rectal cancer, whose baseline clinical characteristics are shown in Table 1. In the entire cohort, there were 257 elderly patients under the age of 71 (71.2%), 222 males (61.5%), TNM stage II 158 cases (43.8%), 142 cases with elevated CEA levels (39.3%), 89 cases with positive MRF (24.7%), 54 cases with positive EMVI (15.0%), 77 cases with perineural invasion (21.3%), and 40 cases with tumor deposits (11.1%). The optimal cutoff values for age, tumor size, BMI, PNI, GNRI, PAR, and ALI were 71, 3.5, 26.49, 52.5, 108.58, 6.38 cm, and 229.07, respectively. The median follow-up time was 43.4 months.
Independent prognostic risk factors for elderly RC
Through univariate cox analysis, we found that T stage (P = 0.001), tumor size (P = 0.003), BMI (P = 0.003), PNI (P < 0.001), GNRI (P = 0.001), PAR (P < 0.001), MRF (P < 0.001), EMVI (P < 0.001), perineural invasion (P = 0.004), and tumor deposits (P = 0.002) are potential prognostic factors for OS deterioration (Table 2). In multivariate analysis, BMI [Hazard Ratio (HR) = 0.464, 95% confidence interval (CI): 0.154–0.674, P = 0.003), PNI (HR = 0.258, 95% CI: 0.089–0.743, P = 0.012), GNRI (HR = 0.258, 95% CI: 0.101–0.660, P = 0.005), PAR (HR = 0.446, 95% CI: 0.256–0.777, P = 0.004), perineural invasion (HR = 2.823, 95% CI: 1.699–4.692, P < 0.001), and tumor deposits (HR = 2.208, 95% CI: 1.177–4.140, P = 0.014) were identified as independent risk factors for OS.
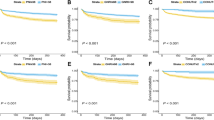
Similarly, univariate analysis revealed that sex (P = 0.020), T stage (P < 0.001), tumor size (P = 0.001), BMI (P = 0.002), PNI (P < 0.001), GNRI (P < 0.001), PAR (P < 0.001), ALI (P = 0.031), CEA (P = 0.020), MRF (P < 0.001), EMVI (P = 0.002), perineural invasion (P < 0.001), and tumor deposits (P < 0.001) are potential prognostic factors for PFS (Table 3). In multivariate analysis, sex (HR = 1.299, 95% CI: 1.006–1.677, P = 0.045), BMI (HR = 0.503, 95% CI: 0.274–0.925, P = 0.027), PNI (HR = 0.456, 95% CI: 0.223–0.931, P = 0.031), GNRI (HR = 0.346, 95% CI: 0.168–0.712, P = 0.004), PAR (HR = 0.520, 95% CI: 0.324–0.836, P = 0.007), perineural invasion (HR = 3.082, 95% CI: 1.965–4.836, P < 0.001), and tumor deposits (HR = 1.837, 95% CI: 1.036–3.255, P = 0.037) were identified as independent risk factors for PFS. The Kaplan–Meier curve demonstrates that elderly patients with high BMI, PNI, GNRI, and low PAR values have a better clinical prognosis compared to malnourished individuals (Fig. 1A–H). Figure S1 depicts the survival differences based on perineural invasion and tumor deposits. Figure S2 showed that elderly patients with low BMI, low PNI, low GNRI, and high PAR had higher cumulative risks of OS and PFS.
Kaplan–Meier curves for OS and PFS by pre-therapeutic nutritional indicators in elderly RC patients. BMI survival curves of OS (A) and PFS (B); PNI survival curves of OS (C) and PFS (D); GNRI survival curves of OS (E) and PFS (F); PAR survival curves of OS (G) and PFS (H). OS overall survival; PFS progression-free survival; BMI body mass index; PNI the prognostic nutritional index, GNRI the geriatric nutrition risk index; PAR platelet-albumin ratio.
Build a nomogram model to predict OS and PFS based on the independent prognostic factors mentioned above (Figs. 2A, 3A). The calibration curve demonstrates good consistency between actual observed outcomes and predicted survival probabilities (Figs. 2B–D, 3B–D). Lastly, the decision curve indicates a positive net benefit of the nomogram model at threshold probabilities, suggesting satisfactory clinical utility (Figs. 2E–G, 3E–G).
Predictive nomogram prognosis model for 1-year, 3-year, and 5-year OS in elderly RC patients, integrating BMI, PNI, GNRI, PAR, perineural invasion, and tumor deposit (A). Calibration curves for 1-year, 3-year, and 5-year OS (B–D). Decision curves for 1-year, 3-year, and 5-year OS (E–G). Complex is composed of independent nutritional prognostic indicators (PNI, BMI, GNRI, and PAR). OS overall survival; RC rectal cancer; BMI body mass index; PNI the prognostic nutritional index, GNRI the geriatric nutrition risk index; PAR platelet-albumin ratio.
Predictive nomogram prognosis model for 1-year, 3-year, and 5-year PFS in elderly RC patients, integrating BMI, PNI, GNRI, PAR, perineural invasion, and tumor deposit (A). Calibration curves for 1-year, 3-year, and 5-year PFS (B–D). Decision curves for 1-year, 3-year, and 5-year PFS (E–G). Complex is composed of independent nutritional prognostic indicators (PNI, BMI, GNRI, and PAR). PFS progression-free survival; RC rectal cancer; BMI body mass index; PNI the prognostic nutritional index, GNRI the geriatric nutrition risk index; PAR platelet-albumin ratio.
Novel nutritional prognostic index and pre-treatment nutritional prognostic score
We have developed a novel Nutritional Prognostic Index (NNPI). The NNPI is calculated by multiplying each independent nutritional prognostic factor by its corresponding beta coefficient and summing the results (zero indicates absence, one indicates presence). The NNPI calculation formula is 0.464*BMI + 0.258*PNI + 0.258*GNRI + 0.446*PAR. The study population is divided into two groups based on NNPI at 0.26. Kaplan–Meier curves illustrate that elderly RC patients with NNPI ≥ 0.26 exhibit significantly better survival compared to those with NNPI < 0.26 (Fig. 4A–B). Subsequently, we utilized RCS curves to assess the relationship between NNPI and survival. The results indicated a non-linear relationship between NNPI and OS as well as PFS among elderly patients with RC. The risk of death sharply increased when NNPI was less than 0.464 (p < 0.05, Fig. 4C–D).
NNPI survival curves of OS (A) and PFS (B); RCS curves indicate a non-linear relationship between NNPI and survival in elderly RC patients (C–D). risk stratification for PNPS on OS and PFS (E–F). NNPI novel nutritional prognostic index; OS overall survival; PFS progression-free survival; RCS restricted cubic splines; PNPS pre-treatment nutritional prognostic score.
Furthermore, based on the nomogram model, we calculated the risk scores for each independent nutritional indicator in the model and summarized them to obtain the total risk score for each independent sample in the study cohort. The median total risk score was 250 (range 0–321). Patients were stratified into low-risk group (≤ 106), moderate-risk group (106 < score ≤ 214), and high-risk group (214 < score ≤ 321) based on the range of total risk scores. Survival curves demonstrate statistically significant differences in OS and PFS among patients in different risk groups (P < 0.05) (Fig. 4E–F).
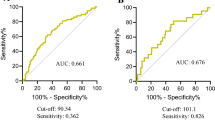
To evaluate the prognostic power of nutritional indicators
Comparing the ROC curves of different nutritional indicators and NNPI helps to evaluate and compare their prognostic value in a specific clinical context. Our findings indicate that the area under the curve (AUC) of the ROC curve for NNPI is greater than that of other nutritional indicators, suggesting that NNPI possesses excellent prognostic predictive capability and may serve as a novel indicator for assessing nutritional risk in clinical practices (Fig. 5A–J). Figure S3 illustrates the 1-year, 3-year, and 5-year time-dependent ROC curves for perineural invasion and tumor deposit.
The time-ROC of nutritional indicators in elderly RC patients. (A, B) the time-ROC of BMI on OS and PFS (1 year, 3-year, and 5-year); (C, D) the time-ROC of PNI on OS and PFS (1 year, 3-year, and 5-year); (E, F) the time-ROC of GNRI on OS and PFS (1 year, 3-year, and 5-year); (G, H) the time-ROC of PAR on OS and PFS (1 year, 3-year, and 5-year); (I, J) the time-ROC of NNPI on OS and PFS (1 year, 3-year, and 5-year). time-ROC the time-dependent receiver operating curve; RC rectal cancer; OS overall survival; PFS progression-free survival; BMI body mass index; PNI the prognostic nutritional index, GNRI the geriatric nutrition risk index; PAR platelet-albumin ratio.
To explore the prognostic value of nutritional indexes and NNPI in different clinicopathological factors
To better understand the impact of nutritional indicators and NNPI on prognosis across different clinical and pathological characteristics, we conducted subgroup analyses on elderly RC patients, stratifying them by age, gender, CEA levels, tumor stage, T stage, N stage, tumor size, MRF, EMVI, neural invasion, and tumor deposits. The forest plot illustrates detailed results of the subgroup analyses for BMI, PNI, GNRI, PAR, and NNPI (Fig. 6A–E). The results indicate that high NNPI is a significant protective factor for survival in elderly RC patients across the aforementioned clinical and pathological factors. However, high BMI, high PNI, high GNRI, and low PAR only serve as protective factors for prognosis in specific clinical and pathological scenarios. In summary, NNPI demonstrates superior clinical applicability.
The sub-group analysis of BMI, PNI, GNRI, PAR, and NNPI in elderly RC patients (A–E). The adjusted factors include age, sex, CEA, tumor stage, T stage, N stage, tumor size, perineural invasion, and tumor deposit. BMI body mass index; PNI the prognostic nutritional index, GNRI the geriatric nutrition risk index; PAR platelet-albumin ratio; NNPI novel nutritional prognostic index; RC rectal cancer; HR hazard ratio; 95% CI 95% confidence interval.
Discussion
With the aging population, there is an increasing number of elderly cancer patients who require comprehensive and complex care to achieve optimal treatment outcomes, where the assessment of nutritional status is crucial26. The occurrence of malnutrition among cancer patients is estimated to be between 20 and 70%6,27, particularly in those with colorectal cancer, often due to inadequate food intake, poor absorption, and increased metabolic demands. Malnutrition has been proven to have adverse effects on treatment outcomes28,29. Previous studies have compared different screening tools for malnutrition risk, such as NRS-2002, MNA-SF, MUST, PG-SGA, and the GLIM criteria, but these tools are complex and subject to individual and cultural influences30,31. Therefore, there is an urgent need for quantitative and objective nutritional screening tools to simplify the assessment and dynamic monitoring of the nutritional status of cancer patients.
Fortunately, some nutritional indicators have overcome the aforementioned issues and can be derived through routine blood tests and biochemical calculations, such as BMI, PAR, PNI, GNRI, and ALI, which possess objective, simple, and practical characteristics. To my knowledge, this study is the first to simultaneously analyze the prognostic value of five nutritional indicators in elderly patients with RC. We observed that (i) low BMI, low PNI, low GNRI, and high PAR were independent risk factors for poor prognosis in elderly RC patients; (ii) compared with other independent nutritional prognostic factors, NNPI had the largest AUC value and was statistically significant in subgroup analyses of different clinicopathological factors, indicating that NNPI had stronger predictive ability and clinical utility; and (iii) by constructing a nomogram model to calculate the PNPS, elderly RC patients were stratified based on risk, with survival curves demonstrating that the OS and PFS of high-risk elderly patients were lower than those of low- or moderate-risk groups.
It is well known that BMI calculated based on height and weight is associated with the risk of colorectal cancer32. Yuko et al. found that compared to low BMI patients, high BMI patients with colorectal cancer have a lower risk of all-cause and disease-specific mortality33. Studies have also identified high BMI as a high-risk factor for recurrence and poorer survival rates in colorectal cancer patients34,35. However, the impact of BMI on the prognosis of colorectal cancer patients may vary between elderly and young patients. To investigate this further, Tomohiro et al. retrospectively collected data on preoperative BMI from 1613 elderly colorectal cancer patients. The study confirmed that lower BMI is associated with an increased risk of mortality in elderly colorectal cancer patients36. Similarly, we have also observed that in elderly RC patients, those with low BMI exhibit significantly poorer OS and PFS compared to patients with high BMI. One possible reason for this is that low BMI may lead to poorer physical condition and weakened immune function in patients, ultimately affecting treatment outcomes and survival rates. Further prospective studies with larger sample sizes are needed to further validate the impact of BMI on the prognosis of elderly patients with RC.
In clinical practice, serum albumin is a widely utilized indicator of nutritional status; its levels can plummet sharply due to malnutrition. Preliminary studies suggest that albumin can be used to assess disease progression and prognosis37,38. The systemic inflammatory response of tumors synergistically inhibits albumin synthesis39. Lymphocytes play a crucial role in the host’s cytotoxic immune response against tumors and can also be used to assess nutritional status40. Platelets have also been observed to be associated with systemic inflammation and the immune system41. Based on this evidence, low PNI reflects hypoalbuminemia and low lymphocyte count, suggesting impaired immune response and/or poor nutritional status. Similarly, a high PAR is indicative of high platelet count and hypoalbuminemia, which can also be used to assess the inflammatory-nutritional status. Okugawa et al. found that a low pre-treatment PNI in RC patients is associated with shorter OS, disease-free survival (DFS), and early recurrence, serving as a significant clinical prognostic factor42. Wang et al. also discovered that a low pre-treatment PNI can be an independent predictor of DFS and OS in locally advanced RC patients9. Some studies have reported that PAR can serve as an independent prognostic marker for certain types of cancers, including esophageal cancer43, pancreatic cancer44, hepatocellular carcinoma45, and cholangiocarcinoma46. However, the relationship between pre-treatment PAR and survival in RC patients remains uncertain. This study for the first time confirms that a high PAR is an independent adverse prognostic factor for OS and PFS in elderly RC patients. These early studies, combined with our current data, suggest that pre-treatment PNI and PAR can serve as nutritional assessment and prognostic indicators for elderly RC patients.
The GNRI was first proposed by Bouillanne et al. as a tool for assessing malnutrition risk and related mortality in elderly medical patients47. GNRI can be computed using routine hematological parameters (such as weight, height, and albumin levels) and can help save time for physicians during pre-treatment evaluations. Numerous studies have demonstrated that GNRI is not only an effective nutritional assessment tool for chronic illnesses but also can be used to predict clinical outcomes in malignant tumors48,49,50. In our study, a low GNRI was associated with poorer OS and PFS in elderly RC patients. Research by Chen et al. also indicates that GNRI can serve as a nutritional tool and an independent predictor of OS17. Zhang et al. have further confirmed this view, showing that GNRI is an effective and simple tool for predicting the risk of major postoperative complications and long-term prognosis in elderly RC patients receiving neoadjuvant therapy16.
Our study highlights the importance of combining these independent nutritional prognostic indicators to improve the accuracy of nutritional assessments and prognostic predictions. The newly developed composite nutritional prognostic index, incorporating BMI, PNI, PAR, and GNRI, shows superior predictive power and practical relevance. Subsequently, we stratified elderly RC patients, enabling medical workers to gain a better understanding of the patients’ overall nutritional status and prognostic risk. This stratification serves as a crucial reference point for devising personalized treatment plans.
Our study has several limitations. Firstly, it is a retrospective single-center study, which may introduce selection bias. Larger prospective multicenter studies are needed to further validate the predictive value of pre-treatment nutritional indicators in elderly RC patients. Secondly, there are currently no standardized cutoff values for each nutritional indicator, posing challenges for nutritional assessment. It is hoped that universally accepted cutoff values can be established in the future, turning these nutritional indicators into early screening tools for nutritional risk. Thirdly, nutritional indicators may be influenced by systemic inflammatory responses and are assessed only once before treatment. The impact of dynamic changes in nutritional indicators needs further evaluation. Fourth, the clinical value of NNPI needs to be compared with traditional nutritional assessment methods such as MNA-SF, MUST, PG-SGA, and GLIM to further validate its clinical significance. Despite these limitations, our study can serve as a crucial reference for assessing the nutritional status and predicting survival in elderly RC patients.
Conclusion
In conclusion, the assessment of nutritional status plays a crucial role in the comprehensive care of elderly RC patients, as malnutrition can significantly impact treatment outcomes. Our study revealed that BMI, PNI, GNRI, and PAR can serve as simple and objective assessment tools for evaluating the nutritional-related mortality risk in elderly RC patients. Among these indicators, NNPI demonstrated the strongest predictive ability and clinical utility in forecasting nutritional-related mortality risk in elderly RC patients. Lastly, constructing a nomogram model based on independent prognostic nutritional indicators enables risk stratification of elderly RC patients, facilitating the development of personalized treatment plans.
Data availability
The data supporting the results of this study can be provided by the corresponding author upon reasonable request.
Abbreviations
- RC:
-
Rectal cancer
- BMI:
-
Body mass index
- PNI:
-
Prognostic nutritional index
- PAR:
-
Platelet-albumin ratio
- GNRI:
-
The geriatric nutrition risk index
- ALI:
-
The advanced lung cancer inflammation index
- NNPI:
-
Novel nutritional prognostic index
- PTNS:
-
Pre-treatment nutritional prognostic score
- WHO:
-
World Health Organization
- TNM:
-
Tumor, node, metastasis
- AJCC:
-
American Joint Committee on Cancer
- CEA:
-
Carcinoembryonic antigen
- MRF:
-
Mesorectal fascia invasion
- EMVI:
-
Extramural vascular invasion
- IBW:
-
Ideal body weight
- PBW:
-
Present body weight
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- time ROC:
-
Time-dependent receiver operating characteristic curve
- RCS:
-
Restricted cubic splines
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
References
Siegel, R. L., Giaquinto, A. N. & Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin.74, 12–49. https://doi.org/10.3322/caac.21820 (2024).
Siegel, R. L. et al. Colorectal cancer statistics, 2020. CA Cancer J. Clin.70, 145–164. https://doi.org/10.3322/caac.21601 (2020).
Keller, D. S., Berho, M., Perez, R. O., Wexner, S. D. & Chand, M. The multidisciplinary management of rectal cancer. Nat. Rev. Gastroenterol. Hepatol.17, 414–429. https://doi.org/10.1038/s41575-020-0275-y (2020).
Lee, D. U. et al. The clinical impact of malnutrition on the postoperative outcomes of patients undergoing colorectal resection surgery for colon or rectal cancer: Propensity score matched analysis of 2011–2017 US hospitals. Surg. Oncol.38, 101587. https://doi.org/10.1016/j.suronc.2021.101587 (2021).
Arends, J. et al. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr.36, 11–48. https://doi.org/10.1016/j.clnu.2016.07.015 (2017).
Muscaritoli, M. et al. ESPEN practical guideline: Clinical Nutrition in cancer. Clin. Nutr.40, 2898–2913. https://doi.org/10.1016/j.clnu.2021.02.005 (2021).
Barker, L. A., Gout, B. S. & Crowe, T. C. Hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. Int. J. Environ. Res. Public Health8, 514–527. https://doi.org/10.3390/ijerph8020514 (2011).
Bjerkeset, T., Morild, I., Mork, S. & Soreide, O. Tumor characteristics in colorectal cancer and their relationship to treatment and prognosis. Dis. Colon Rectum30, 934–938. https://doi.org/10.1007/BF02554279 (1987).
Wang, Y. et al. Pretreatment inflammatory-nutritional biomarkers predict responses to neoadjuvant chemoradiotherapy and survival in locally advanced rectal cancer. Front Oncol.11, 639909. https://doi.org/10.3389/fonc.2021.639909 (2021).
Zhou, C. J. et al. Malnutrition and visceral obesity predicted adverse short-term and long-term outcomes in patients undergoing proctectomy for rectal cancer. BMC Cancer23, 576. https://doi.org/10.1186/s12885-023-11083-y (2023).
Mayne, S. T., Playdon, M. C. & Rock, C. L. Diet, nutrition, and cancer: past, present and future. Nat. Rev. Clin. Oncol.13, 504–515. https://doi.org/10.1038/nrclinonc.2016.24 (2016).
Liu, H. et al. BMI may be a prognostic factor for local advanced rectal cancer patients treated with long-term neoadjuvant chemoradiotherapy. Cancer Manag. Res.12, 10321–10332. https://doi.org/10.2147/CMAR.S268928 (2020).
Yamano, T. et al. Influence of chemoradiotherapy on nutritional status in locally advanced rectal cancer: Prospective multicenter study. Nutrition77, 110807. https://doi.org/10.1016/j.nut.2020.110807 (2020).
Kocak, M. Z., Coban, S., Araz, M., Eryilmaz, M. K. & Artac, M. Prognostic biomarkers in metastatic colorectal cancer: delta prognostic nutritional index, delta neutrophil to lymphocyte ratio, and delta platelet to lymphocyte ratio. Support Care Cancer31, 357. https://doi.org/10.1007/s00520-023-07829-w (2023).
Xia, L. J. et al. Significance of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, lymphocyte-to-monocyte ratio and prognostic nutritional index for predicting clinical outcomes in T1–2 rectal cancer. BMC Cancer20, 208. https://doi.org/10.1186/s12885-020-6698-6 (2020).
Zhang, L. et al. The clinical predictive value of geriatric nutritional risk index in elderly rectal cancer patients received surgical treatment after neoadjuvant therapy. Front. Nutr.10, 1237047. https://doi.org/10.3389/fnut.2023.1237047 (2023).
Chen, X. Y. et al. The geriatric nutritional risk index is an effective tool to detect GLIM-defined malnutrition in rectal cancer patients. Front. Nutr.9, 1061944. https://doi.org/10.3389/fnut.2022.1061944 (2022).
Kusunoki, K. et al. advanced lung cancer inflammation index predicts outcomes of patients with colorectal cancer after surgical resection. Dis. Colon Rectum63, 1242–1250. https://doi.org/10.1097/DCR.0000000000001658 (2020).
Skalitzky, M. K. et al. Characteristics and symptomatology of colorectal cancer in the young. Surgery173, 1137–1143. https://doi.org/10.1016/j.surg.2023.01.018 (2023).
Stoffel, E. M. & Murphy, C. C. Epidemiology and mechanisms of the increasing incidence of colon and rectal cancers in young adults. Gastroenterology158, 341–353. https://doi.org/10.1053/j.gastro.2019.07.055 (2020).
Mathers, C. D., Stevens, G. A., Boerma, T., White, R. A. & Tobias, M. I. Causes of international increases in older age life expectancy. Lancet385, 540–548. https://doi.org/10.1016/S0140-6736(14)60569-9 (2015).
Li, Q. et al. Secular trends and attributable risk factors of esophageal cancer deaths among non-elderly adults based on Global Burden of Disease Study. J. Cancer Res. Clin. Oncol.149, 16417–16427. https://doi.org/10.1007/s00432-023-05380-z (2023).
Jiang, K. T. & Huang, D. Z. The risks and trends of cardiac-specific mortality associated with chemotherapy or radiotherapy in a large cohort of non-elderly patients with non-small cell lung cancer. Transl. Cancer Res.10, 842–853. https://doi.org/10.21037/tcr-20-2981 (2021).
Weiser, M. R. AJCC 8th edition: colorectal cancer. Ann. Surg Oncol.25, 1454–1455. https://doi.org/10.1245/s10434-018-6462-1 (2018).
Nicholls, R. J., Zinicola, R. & Haboubi, N. Extramural spread of rectal cancer and the AJCC Cancer Staging Manual 8th edition, 2017. Ann. Oncol.30, 1394–1395. https://doi.org/10.1093/annonc/mdz147 (2019).
Faivre, J., Lemmens, V. E., Quipourt, V. & Bouvier, A. M. Management and survival of colorectal cancer in the elderly in population-based studies. Eur. J. Cancer43, 2279–2284. https://doi.org/10.1016/j.ejca.2007.08.008 (2007).
Marshall, K. M., Loeliger, J., Nolte, L., Kelaart, A. & Kiss, N. K. Prevalence of malnutrition and impact on clinical outcomes in cancer services: A comparison of two time points. Clin. Nutr.38, 644–651. https://doi.org/10.1016/j.clnu.2018.04.007 (2019).
van den Berg, M. G. et al. Comparison of the effect of individual dietary counselling and of standard nutritional care on weight loss in patients with head and neck cancer undergoing radiotherapy. Br. J. Nutr.104, 872–877. https://doi.org/10.1017/S0007114510001315 (2010).
Chandra, R. K. Nutrition and the immune system: an introduction. Am J Clin Nutr66, 460S-463S. https://doi.org/10.1093/ajcn/66.2.460S (1997).
Zhang, Z. et al. Prevalence of malnutrition comparing NRS2002, MUST, and PG-SGA with the GLIM criteria in adults with cancer: A multi-center study. Nutrition83, 111072. https://doi.org/10.1016/j.nut.2020.111072 (2021).
Huang, Y., Chen, Y., Wei, L., Hu, Y. & Huang, L. Comparison of three malnutrition risk screening tools in identifying malnutrition according to Global Leadership Initiative on Malnutrition criteria in gastrointestinal cancer. Front. Nutr.9, 959038. https://doi.org/10.3389/fnut.2022.959038 (2022).
Keum, N. & Giovannucci, E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat. Rev. Gastroenterol. Hepatol.16, 713–732. https://doi.org/10.1038/s41575-019-0189-8 (2019).
Minami, Y. et al. Associations of cigarette smoking, alcohol drinking and body mass index with survival after colorectal cancer diagnosis by anatomic subsite: a prospective patient cohort study in Japan. Jpn. J. Clin. Oncol.52, 1375–1388. https://doi.org/10.1093/jjco/hyac140 (2022).
Campbell, P. T. et al. Impact of body mass index on survival after colorectal cancer diagnosis: the Cancer Prevention Study-II Nutrition Cohort. J. Clin. Oncol.30, 42–52. https://doi.org/10.1200/JCO.2011.38.0287 (2012).
Fedirko, V. et al. Pre-diagnostic anthropometry and survival after colorectal cancer diagnosis in Western European populations. Int. J. Cancer135, 1949–1960. https://doi.org/10.1002/ijc.28841 (2014).
Adachi, T. et al. Lower body mass index predicts worse cancer-specific prognosis in octogenarians with colorectal cancer. J. Gastroenterol.51, 779–787. https://doi.org/10.1007/s00535-015-1147-z (2016).
Noble, F. et al. The role of systemic inflammatory and nutritional blood-borne markers in predicting response to neoadjuvant chemotherapy and survival in oesophagogastric cancer. Med. Oncol.30, 596. https://doi.org/10.1007/s12032-013-0596-6 (2013).
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell144, 646–674. https://doi.org/10.1016/j.cell.2011.02.013 (2011).
Yeun, J. Y. & Kaysen, G. A. Factors influencing serum albumin in dialysis patients. Am. J. Kidney Dis.32, S118-125. https://doi.org/10.1016/s0272-6386(98)70174-x (1998).
Schmidt, M. A. et al. Circulating regulatory T cells of cancer patients receiving radiochemotherapy may be useful to individualize cancer treatment. Radiother. Oncol.104, 131–138. https://doi.org/10.1016/j.radonc.2012.05.003 (2012).
Thomas, M. R. & Storey, R. F. The role of platelets in inflammation. Thromb. Haemost.114, 449–458. https://doi.org/10.1160/TH14-12-1067 (2015).
Okugawa, Y. et al. Feasibility of assessing prognostic nutrition index in patients with rectal cancer who receive preoperative chemoradiotherapy. J. Parenter. Enteral Nutr.42, 998–1007. https://doi.org/10.1002/jpen.1041 (2018).
Huang, Z. et al. Prognostic significance of platelet-to-albumin ratio in patients with esophageal squamous cell carcinoma receiving definitive radiotherapy. Sci. Rep.12, 3535. https://doi.org/10.1038/s41598-022-07546-0 (2022).
Shirai, Y. et al. Preoperative platelet-to-albumin ratio predicts prognosis of patients with pancreatic ductal adenocarcinoma after pancreatic resection. Anticancer Res.37, 787–793. https://doi.org/10.21873/anticanres.11378 (2017).
Li, C., Peng, W., Zhang, X. Y., Wen, T. F. & Chen, L. P. The preoperative platelet to albumin ratio predicts the prognosis of hepatocellular carcinoma patients without portal hypertension after liver resection. Medicine (Baltimore)98, e17920. https://doi.org/10.1097/MD.0000000000017920 (2019).
Saito, N. et al. Preoperative platelet to albumin ratio predicts outcome of patients with cholangiocarcinoma. Anticancer Res.38, 987–992. https://doi.org/10.21873/anticanres.12313 (2018).
Bouillanne, O. et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am. J. Clin. Nutr.82, 777–783. https://doi.org/10.1093/ajcn/82.4.777 (2005).
Taniguchi, E. et al. Nutritional assessments for ordinary medical care in patients with chronic liver disease. Hepatol. Res.43, 192–199. https://doi.org/10.1111/j.1872-034X.2012.01055.x (2013).
Hino, H., Saito, T., Matsui, H., Taniguchi, Y. & Murakawa, T. Utility of Geriatric Nutritional Risk Index in patients with lung cancer undergoing surgery. Eur. J. Cardiothorac. Surg.58, 775–782. https://doi.org/10.1093/ejcts/ezaa066 (2020).
Kushiyama, S. et al. The preoperative geriatric nutritional risk index predicts postoperative complications in elderly patients with gastric cancer undergoing gastrectomy. In Vivo32, 1667–1672. https://doi.org/10.21873/invivo.11430 (2018).
Acknowledgements
We thank all the investigators and patients who participated in the present study.
Funding
This work was supported by the Joint Funds for the National Clinical Key Specialty Construction Program (Grant No. 2021), the Fujian Provincial Clinical Research Center for Cancer Radiotherapy and Immunotherapy (Grant No. 2020Y2012), and Fujian Clinical Research Center for Radiation and Therapy of Digestive, Respiratory and Genitourinary Malignancies (Grant No. 2021Y2014).
Author information
Authors and Affiliations
Contributions
Conceptualization, Jianjian Qiu, Yilin Yu, and Zhiping Wang; Data curation, Lingdong Shao, and Liang Hong; Formal analysis, Jianjian Qiu, Yilin Yu, Zhiping Wang, Lingdong Shao, and Liang Hong; Funding acquisition, Junxin Wu; Methodology, Jianjian Qiu, Yilin Yu, Zhiping Wang, Lingdong Shao, and Liang Hong; Supervision, Lingdong Shao, Liang Hong, and Junxin Wu; Writing – original draft, Jianjian Qiu, Yilin Yu, and Zhiping Wang, Lingdong Shao, and Liang Hong; Writing – review & editing, Jianjian Qiu, Yilin Yu, and Junxin Wu.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was sanctioned by Fujian Cancer Hospital’s Ethics Committee. All patients provided written informed consent.
Consent for publication
The manuscript has been approved by all authors for publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qiu, J., Yu, Y., Wang, Z. et al. Comprehensive analysis of the prognostic value of pre-treatment nutritional indicators in elderly rectal cancer patients. Sci Rep 14, 22078 (2024). https://doi.org/10.1038/s41598-024-73123-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-73123-2