Abstract
The neutrophil-to-lymphocyte ratio (NLR), a simple marker of systemic inflammation, is crucial in the progression of cardiovascular diseases (CVD). Its predictive value for all-cause and cardiovascular mortality in CVD patients with diabetes or pre-diabetes remains unclear. We analyzed 3,780 CVD patients with diabetes or pre-diabetes from the National Health and Nutrition Examination Survey (2001–2018). Kaplan-Meier survival curves, weighted Cox proportional hazards models, and restricted cubic spline (RCS) analyses were used to assess the relationship between NLR and mortality risk. RCS revealed a U-shaped association between NLR and all-cause mortality, with an inflection point at 1.776. For NLR < 1.776, the risk of all-cause mortality decreased by 13% per unit increase in NLR (HR: 0.87, 95% CI: 0.76–0.98). For NLR ≥ 1.776, the risk increased by 15% per unit increase (HR: 1.15, 95% CI: 1.10–1.26). A positive linear association was found between NLR and cardiovascular mortality, with a 17% increase in risk per unit increase in NLR (HR: 1.17, 95% CI: 1.10–1.25). No significant interactions were observed in stratified analyses. Our study revealed the U-shaped relationship between NLR and all-cause mortality, and a positive linear relationship with cardiovascular mortality in CVD patients with diabetes or pre-diabetes.
Similar content being viewed by others
Cardiovascular disease (CVD) is a significant global public health issue, responsible for the majority of deaths and disabilities worldwide1. It imposes a substantial burden on both the health and economy of the world. CVD is commonly linked with metabolic disorders such as hyperglycemia, dyslipidemia, and hypertension, which increases its risk for cardiovascular problems2. Patients with diabetes or pre-diabetes are at even higher risk of cardiovascular morbidity and mortality3,4,5. The neutrophil-to-lymphocyte ratio (NLR), a simple and easily accessible indicator, is thought to reflect the state of systemic inflammation, which is crucial in the pathogenesis and progression of CVD6,7. Previous research has demonstrated that high NLR level was significantly associated with the occurrence of cardiovascular events and poor prognosis8,9,10. NLR is also a predictor of the occurrence of adverse cardiovascular events in diabetic patients11,12,13. However, the association between NLR levels and all-cause and cardiovascular mortality in CVD patients with diabetes or pre-diabetes has not been studied. Therefore, this study aims to investigate this association and gain a deeper understanding of the clinical significance of NLR in this high-risk population.
Materials and methods
Study population
The National Health and Nutrition Examination Survey (NHANES) is a program that aims to evaluate the health and nutritional status of people in the United States. This program is administered by the Centers for Disease Control and Prevention, and all NHANES study protocols has been formally approved by the Research Ethics Review Board of the National Center for Health Statistics (NCHS). Written informed consent was obtained from all participants in the study. Data for this study can be accessed on the NHANES website at https://www.cdc.gov/nchs/nhanes.
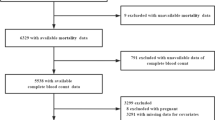
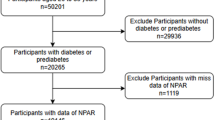
This national cohort study involved 3780 adults from the United States across nine NHANES survey cycles from 2001 to 2018 (Fig. 1). Participants with missing neutrophil counts, lymphocyte counts, and survival data were excluded. Diabetes was defined as meeting any of the following criteria: (1) fasting plasma glucose (FPG) ≥ 126 mg/dL; (2) 2-hour oral glucose tolerance test (OGTT) glucose ≥ 200 mg/dL; (3) hemoglobin A1c (HbA1c) ≥ 6.5%; (4) use of insulin or oral hypoglycemic medications; (5) self-reported physician-diagnosed diabetes. Pre-diabetes was defined as meeting any of the following criteria: (1) 100 mg/dL ≤ FPG < 126 mg/dL; (2) 140 mg/dL ≤ 2-hour OGTT glucose < 200 mg/dL; (3) 5.7% ≤ HbA1c < 6.5%; (4) self-reported physician-diagnosed pre-diabetes14. The diagnosis of CVD was confirmed by a quality-assured and controlled medical condition survey. Participants were asked if they had ever been told by a physician or other health professional that they had heart failure, coronary heart disease, angina, myocardial infarction, or stroke. If they answered “yes” to any of these questions, they were diagnosed with CVD15.
Assessment of NLR
Blood samples were collected at the Mobile Examination Center (MEC), and laboratory tests were performed under standardized conditions. Neutrophil and lymphocyte counts were measured by a Beckman Coulter DxH 800 instrument. NLR was calculated by dividing the neutrophil count by the lymphocyte count.
Assessment of covariates
Demographic characteristics and covariates including age, sex, race, education level, household income, hypertension, and cancer were obtained through household interviews or questionnaires. Body mass index (BMI) was calculated by dividing weight (in kilograms) by the square of height (in meters) and categorized as underweight (< 18.5), normal (18.5 to < 25), overweight (25 to < 30), and obese (30 or greater). Race was classified as Non-Hispanic White, Non-Hispanic Black, Mexican American, Other Hispanic, and Other/multiracial. Education level was classified as “some college or above”, “below high school”, and “high school graduate or equivalent”. Smoking status was classified as current smoker (reported smoking recently and smoked over 100 cigarettes in their lifetime), former smoker (smoked over 100 cigarettes but not currently smoking), and never smoker (smoked fewer than 100 cigarettes in their lifetime). Hypertension was defined as a self-reported history of physician-diagnosed hypertension. Cancer was defined as a self-reported history of physician-diagnosed cancer. High-density lipoprotein cholesterol (HDL), low-density lipoprotein cholesterol (LDL), total cholesterol (TC), triglycerides (TG), serum creatinine (SCR), HbA1c, FPG, albumin (ALB), alanine transaminase (ALT), alanine transaminase (AST), and blood urea nitrogen (BUN) were obtained from laboratory data. Estimated glomerular filtration rate (eGFR) was calculated according to the CKD-EPI Eq. (2021).
Ascertainment of mortality
The mortality details for the follow-up population were obtained from the NCHS-linked National Death Index mortality file (last updated December 31, 2019), available at https://www.cdc.gov/nchs/data-linkage/mortality-public.htm. The follow-up period started on the day of the interview and concluded on either the day of death or December 31, 2019. Cardiovascular deaths were identified by codes I00-I09, I11, I13, and I20-I51 using the International Statistical Classification of Diseases, 10th revision (ICD-10).
Statistical analysis
Sample weights, clustering, and stratification were incorporated into the analysis of this study in compliance with NHANES data analysis requirements due to its complex sample design16. Sample weights used for this study were calculated as Full sample 2-year MEC exam weight divided by 9.
Participants were divided into four groups (Q1-Q4) based on quartiles of the NLR. Continuous variables were presented as weighted mean and standard deviation (SD), and categorical variables were presented as unweighted frequencies and weighted percentages. The Kruskal-Wallis rank sum test or ANOVA was used for continuous variables, and chi-square tests were used for categorical variables to analyze group differences. Kaplan-Meier curves were plotted to assess the association of NLR with all-cause and cardiovascular mortality, and weighted Cox proportional regression models were constructed. Model 1 was unadjusted. Age, sex, and race were adjusted in Model 2. Age, sex, race, BMI, LDL, HDL, TC, TG, eGFR, education, smoking status, hypertension, and cancer were adjusted in Model 3. The final multivariate Cox models included covariates that were both clinically meaningful and statistically significant in the univariate analyses. Restricted cubic spline (RCS) was used to explore the potential non-linear relationship between NLR and all-cause mortality and cardiovascular mortality in CVD patients with diabetes or pre-diabetes. Two-piecewise Cox proportional hazard model was constructed on both sides of the inflection point to investigate the non-linear relationship between NLR and all-cause mortality. Finally, stratified analyses were performed according to age, sex, BMI, smoking status, hypertension, and glucose metabolism disorders, and P for interaction was calculated.
All analyses were conducted using R software version 4.3.1, P < 0.05 was considered statistically significant.
Results
Baseline characteristics of study participants
Participants were divided into groups based on their NLR quartiles to compare their baseline characteristics. Participants in the high NLR group, as compared to those in the low NLR group, were older, had a higher proportion of males, a higher proportion of whites, and a higher prevalence of cancer. There were also differences in biochemical markers such as HDL, LDL, TC, TG, HbA1c, FPG, ALB, ALT, AST, BUN, SCR, and eGFR between the groups. The all-cause mortality of participants in the four groups (Q1-Q4) was 28.77%, 33.10%, 36.58%, and 50.98%, respectively. The cardiovascular mortality was 8.74%, 11.41%, 12.87%, and 18.28%, respectively. Both all-cause and cardiovascular mortality showed an increase with increasing NLR. Detailed information is shown in Table 1.
Kaplan–Meier survival analysis curves for all-cause and cardiovascular mortality
Kaplan-Meier survival analysis curves showed that the group with higher NLR level had a significantly lower probability of survival for both all-cause mortality and cardiovascular mortality (P for log-rank test < 0.001) (Fig. 2).
Associations between NLR and mortality
A total of 1588 all-cause deaths and 543 cardiovascular deaths were recorded during a median follow-up time of 72 months. Weighted cox proportional hazard models were constructed to explore the association between NLR and mortality risk (Table 2). After adjusting for age, sex, race, BMI, LDL, HDL, TC, TG, eGFR, education, smoke status, hypertension, and cancer in model 3, the all-cause mortality hazard ratios (HRs) and 95% confidence intervals (CIs) for Q2, Q3, and Q4, using Q1 as the reference, were 1.06 (0.87, 1.29), 1.09 (0.89, 1.33), 1.71 (1.41, 2.06), respectively. For cardiovascular mortality, the HR and 95% CI were 1.21 (0.80, 1.83), 1.25 (0.87, 1.81), and 1.97 (1.33, 2.94), respectively. Hazards of all-cause and cardiovascular mortality tended to increase as NLR quartiles increased in all three models (P for trend < 0.001).
In order to investigate the relationship between NLR and all-cause mortality and cardiovascular mortality, RCS analysis was conducted to determine any potential non-linear relationships (Fig. 3). The adjusted RCS curve revealed a U-shaped association between NLR and all-cause mortality (P-non-linear = 0.005), with an inflection point of 1.776. However, there appeared to be no significant nonlinear relationship between NLR and cardiovascular mortality (P-non-linear = 0.644).
Restricted cubic spline for the association of NLR with all-cause (a) and cardiovascular mortality (b) in CVD patients with diabetes or pre-diabetes. Adjusted for age, sex, race, BMI, LDL, HDL, TC, TG, eGFR, education, smoke status, hypertension, and cancer. The NLR has an inflection point of 1.776 for all-cause mortality restricted cubic spline curve. The solid red line and the light red area represent the estimated hazard ratios and their corresponding 95% confidence intervals. The horizontal dashed line identifies the hazard ratio of 1. CI confidence interval, NLR neutrophil-to-lymphocyte ratio.
A two-piecewise Cox proportional hazard model was constructed to further analyze the threshold effect of the U-shaped relationship between NLR and all-cause mortality (Table 3). When the NLR was less than 1.776, the risk of all-cause mortality decreased by 13% for every unit increase in NLR (HR (95% CI) 0.87 (0.76, 0.98), P = 0.004). However, when NLR was equal to or greater than 1.776, the risk of all-cause mortality increased by 15% for every unit increase in NLR (HR (95% CI) 1.15 (1.10, 1.26), P < 0.001). In the continuous model, the risk of all-cause mortality increased by 14% for every unit increase in NLR (HR (95% CI) 1.14 (1.10, 1.19), P < 0.001). The association between NLR and cardiovascular mortality was roughly linear, with an increase in the risk of cardiovascular mortality of 19% for every unit increase in NLR (HR (95% CI) 1.17 (1.10, 1.25), P < 0.001).
Stratified analyses
Stratified analyses were performed according to age, sex, BMI, smoking status, hypertension, and glucose metabolism disorders (Fig. 4). Among CVD patients with diabetes or pre-diabetes, low NLR (< 1.776) had a lower hazard of all-cause mortality relative to high NLR (≥ 1.776) (Fig. 4a), and low levels of NLR were also associated with a lower hazard of cardiovascular mortality (Fig. 4b). There were no significant interactions in all subgroups (P for interaction > 0.05).
Stratified analyses of the associations between NLR and all-cause (a) and cardiovascular mortality (b) among CVD patients with diabetes or pre-diabetes. The survival advantage of lower NLR (< 1.776) relative to higher NLR (≥ 1.776) was compared in a stratified analysis of all-cause mortality (a). Adjusted for age, sex, race, BMI, LDL, HDL, TC, TG, eGFR, education, smoke status, hypertension, and cancer. CI confidence interval, HR hazard ratio, NLR neutrophil-to-lymphocyte ratio.
Predictive capacity of NLR for mortality outcomes
The predictive ability of NLR for mortality outcomes was analyzed using time-dependent receiver operating characteristic (ROC) analysis (Fig. 5). The area under the curve (AUC) values for all-cause mortality at 36, 60, and 120 months were 0.650, 0.649, and 0.639, respectively. Similarly, for cardiovascular mortality, the AUC values at 36, 60, and 120 months were 0.649, 0.649, and 0.653, respectively. These results indicate that the predictive ability of NLR remained consistent over time. Additionally, we analyzed the predictive performance of neutrophil and lymphocyte counts individually and found that their predictive abilities were inferior to NLR across all time points (Supplementary Fig. S1).
Discussion
The results of our study revealed an association between NLR and mortality in the population of CVD patients with diabetes or pre-diabetes. We found that there is a U-shaped relationship between NLR and all-cause mortality, with NLR being positively associated with all-cause mortality risk when it is above a threshold of 1.776. Moreover, there is a positive linear correlation between NLR and cardiovascular mortality. While the AUC values from our time-dependent ROC analysis indicate that NLR has moderate predictive capacity for both all-cause and cardiovascular mortality, it remains a valuable marker due to its simplicity and accessibility. This can be useful for risk stratification of patients as well as adjustment of treatment strategies.
In recent years, several studies have been conducted to investigate the predictive value of NLR in CVD.NLR was significantly associated with cardiovascular diseases such as coronary heart disease, stroke and heart failure8,17. High NLR level in coronary artery disease patients with diabetes increased the risk of poor prognosis after undergoing coronary intervention9. On the other hand, NLR has been demonstrated to be an important prognostic indicator in diabetic patients. NLR level was elevated in diabetic patients and was independently associated with the prevalence and severity of coronary artery disease12. And NLR served as a risk factor for all-cause and cardiovascular mortality in diabetic patients18. In patients with diabetic kidney disease the predictive value of NLR has also been validated19. The significance of NLR in both CVD and diabetes is likely due to the inextricable role of inflammation in the two diseases20, and this is the reason why we chose CVD patients with diabetes or pre-diabetes as our high-risk study population. And our research included CVD individuals with pre-diabetes, who are often neglected in studies that primarily focus on diabetic populations.
Since inflammation is a central player in the development of CVD as well as complications, monitoring of inflammatory markers is necessary7,21,22. The accessibility and affordability of blood count testing are advantages of the NLR as an indicator of inflammation. The NLR is also appealing because it is easy to interpret in both clinical and research settings. In contrast, composite indices such as systemic immune-inflammation index and systemic inflammation response index, although valuable, incorporate multiple parameters, which may complicate their clinical application10. In addition, NLR is an integrating variable of leukocyte data, providing more comprehensive information on inflammation and prognostic value than separate indicators6. Neutrophil counts are a marker of nonspecific inflammation, whereas low lymphocyte counts indicate a relative deficiency in immunoregulatory pathways18. Our study did not suggest a specific biological mechanism by which NLR predicts mortality risk, but it has been proposed that Neutrophil counts are associated with the severity of a variety of cardiovascular diseases, with possible mechanisms being the release of cytoplasmic granules from neutrophils and the formation of neutrophil extracellular traps23,24. Different types of lymphocytes have different roles in CVD. CD4+ T lymphocytes play a protective role in both atherosclerosis and myocardial infarction, and low lymphocyte counts are associated with a poorer prognosis and increased mortality after acute myocardial infarction25,26. Diabetes is accompanied by increased oxidative stress and necrosis of neutrophils, triggering an inflammatory response that impairs endothelial function27. Chronic inflammation driven by neutrophil extracellular traps affected wound healing in diabetic patients and may also contribute to increased mortality28.
It is noteworthy that in our RCS results NLR was negatively associated with all-cause mortality at less than the threshold. This U-shaped association is consistent with some studies of NLR13,29.A possible explanation is that this group of patients includes patients with neutropenia or hematopoietic dysfunction who may suffer more adverse events13. Due to the limited relevant information provided by the NHANES database, more other cohort studies are needed to validate this. The non-significant HRs for Q2 and Q3 in some models may indicate a threshold effect or dose-response relationships, where only individuals in the highest quartile of NLR (Q4) are at significantly elevated risk for mortality. This observation highlights that while NLR is associated with mortality, the increased risk may become more apparent at higher levels of inflammation, as reflected by Q4. However, the P for trend (< 0.001) suggests a significant overall trend across the quartiles, despite the non-significance of individual quartiles in some models. Our findings seemed to confirm an independent association between NLR and mortality. However, whether the NLR directly contributes to the pathogenesis of poor outcomes or is merely a manifestation of the disease process remains to be determined. This question is important in terms of whether treatments targeting the NLR affect clinical outcomes. Some commonly used drugs such as clopidogrel30and colchicine31 have been demonstrated to have effects on lowering neutrophil counts. It is also worth exploring whether repeated measurements of complete blood counts and utilizing the mean NLR may result in better prognostic outcomes.
Our study examined NLR and risk of mortality in the population of CVD patients with diabetes or pre-diabetes. The large sample size and long follow-up period increased the reliability of the statistical findings. The NHANES sampling weight design also helped to reduce selection bias in the study population to some extent. However, it is important to note that our study has some limitations. Firstly, the study only examined the baseline NLR levels. Further research is needed to investigate the impact of dynamic changes in NLR over time on all-cause and cardiovascular mortality. Secondly, the study data was limited to the US population, and its applicability to other populations needs further examination. Thirdly, we did not assess the potential overlap of the NLR with other identified inflammatory markers. It will be interesting to study and understand the role of different inflammatory markers in predicting mortality outcomes in the future. Lastly, despite our statistical approach to controlling for confounders, they could not be completely eliminated.
Conclusions
The findings of our study revealed a U-shaped association between NLR and all-cause mortality with an inflection point of 1.776, as well as a positive linear association between NLR and cardiovascular mortality in CVD patients with diabetes or pre-diabetes. This suggested that NLR can be used as a biomarker to identify high-risk patients, which potentially provides clinical guidance and management strategies to improve prognosis in CVD patients with diabetes or pre-diabetes.
Data availability
The data used for this study are publicly available at https://www.cdc.gov/nchs/nhanes/index.htm.
Abbreviations
- ALB:
-
Albumin
- ALT:
-
Alanine transaminase
- AST:
-
Alanine transaminase
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- BUN:
-
Blood urea nitrogen
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular diseases
- eGFR:
-
Estimated glomerular filtration rate
- FPG:
-
Fasting plasma glucose
- HbA1c:
-
Hemoglobin A1c
- HDL:
-
High-density lipoprotein cholesterol
- HR:
-
Hazard ratio
- LDL:
-
Low-density lipoprotein cholesterol
- MEC:
-
Mobile Examination Center
- NHANES:
-
National Health and Nutrition Examination Survey
- NCHS:
-
National Center for Health Statistics
- NLR:
-
Neutrophil-to-lymphocyte ratio
- OGTT:
-
Oral glucose tolerance test
- RCS:
-
Restricted cubic spline
- ROC:
-
Receiver operating characteristic
- SCR:
-
Serum creatinine
- SD:
-
Standard deviation
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
References
Roth, G. A. et al. Global Burden of Cardiovascular diseases and Risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 76(25), 2982–3021 (2020).
Martin, S. S. et al. 2024 heart disease and stroke statistics: A report of US and global data from the American Heart Association. Circulation 149(8), e347–e913 (2024).
Echouffo-Tcheugui, J. B., Perreault, L., Ji, L. & Dagogo-Jack, S. Diagnosis and management of prediabetes: A review. Jama 329(14), 1206–1216 (2023).
Rentsch, C. T. et al. Sex-specific risks for cardiovascular disease across the glycaemic spectrum: A population-based cohort study using the UK Biobank. Lancet Reg. Health Eur. 32, 100693 (2023).
Wong, N. D. & Sattar, N. Cardiovascular risk in diabetes mellitus: Epidemiology, assessment and prevention. Nat. Rev. Cardiol. 20(10), 685–695 (2023).
Horne, B. D. et al. Which white blood cell subtypes predict increased cardiovascular risk? J. Am. Coll. Cardiol. 45(10), 1638–1643 (2005).
Ruparelia, N., Chai, J. T., Fisher, E. A. & Choudhury, R. P. Inflammatory processes in cardiovascular disease: A route to targeted therapies. Nat. Rev. Cardiol. 14(3), 133–144 (2017).
Kim, S., Eliot, M., Koestler, D. C., Wu, W. C. & Kelsey, K. T. Association of neutrophil-to-lymphocyte ratio with mortality and cardiovascular disease in the Jackson Heart Study and modification by the Duffy antigen variant. JAMA Cardiol. 3(6), 455–462 (2018).
He, J. et al. High neutrophil to lymphocyte ratio with type 2 diabetes mellitus predicts poor prognosis in patients undergoing percutaneous coronary intervention: A large-scale cohort study. Cardiovasc. Diabetol. 21(1), 156 (2022).
Ferro, D. et al. Neutrophil-to-lymphocyte ratio predicts cerebral edema and clinical worsening early after reperfusion therapy in stroke. Stroke 52(3), 859–867 (2021).
Verma, S. et al. Neutrophil to lymphocyte ratio predicts cardiovascular events in people with type 2 diabetes: Post hoc analysis of the SUSTAIN 6 and PIONEER 6 cardiovascular outcomes trials. Diabetes Obes. Metab. 25(8), 2398–2401 (2023).
Verdoia, M. et al. Impact of diabetes on neutrophil-to-lymphocyte ratio and its relationship to coronary artery disease. Diabetes Metab. 41(4), 304–311 (2015).
Lee, G. K. et al. The long-term predictive value of the neutrophil-to-lymphocyte ratio in type 2 diabetic patients presenting with acute myocardial infarction. QJM 105(11), 1075–1082 (2012).
2. Diagnosis and classification of diabetes: Standards of Care in Diabetes-2024. Diabetes Care 47(Suppl 1), S20–S42 (2024).
Zhang, Q., Xiao, S., Jiao, X. & Shen, Y. The triglyceride-glucose index is a predictor for cardiovascular and all-cause mortality in CVD patients with diabetes or pre-diabetes: Evidence from NHANES 2001–2018. Cardiovasc. Diabetol. 22(1), 279 (2023).
Johnson, C. L. et al. National health and nutrition examination survey: Analytic guidelines, 1999–2010. Vital Health Stat. 2(161), 1–24 (2013).
Bhat, T. et al. Neutrophil to lymphocyte ratio and cardiovascular diseases: A review. Expert Rev. Cardiovasc. Ther. 11(1), 55–59 (2013).
Dong, G. et al. The neutrophil-lymphocyte ratio as a risk factor for all-cause and cardiovascular mortality among individuals with diabetes: Evidence from the NHANES 2003–2016. Cardiovasc. Diabetol. 22(1), 267 (2023).
Zeng, G. et al. Relationship of the neutrophil-lymphocyte ratio with all-cause and Cardiovascular Mortality in patients with Diabetic kidney disease: A prospective cohort study of NHANES Study. J. Multidiscip Healthc. 17, 2461–2473 (2024).
Sharif, S. et al. Low-grade inflammation as a risk factor for cardiovascular events and all-cause mortality in patients with type 2 diabetes. Cardiovasc. Diabetol. 20(1), 220 (2021).
Hansson, G. K. Inflammation, atherosclerosis, and coronary artery disease. N. Engl. J. Med. 352(16), 1685–1695 (2005).
Libby, P. Inflammation and cardiovascular disease mechanisms. Am. J. Clin. Nutr. 83(2), 456s–60s (2006).
Gaul, D. S., Stein, S. & Matter, C. M. Neutrophils in cardiovascular disease. Eur. Heart J. 38(22), 1702–1704 (2017).
Luo, J., Thomassen, J. Q., Nordestgaard, B. G., Tybjærg-Hansen, A. & Frikke-Schmidt, R. Neutrophil counts and cardiovascular disease. Eur. Heart J. 44(47), 4953–4964 (2023).
Hofmann, U. et al. Activation of CD4+ T lymphocytes improves wound healing and survival after experimental myocardial infarction in mice. Circulation 125(13), 1652–1663 (2012).
Sager, H. B. & Koenig, W. Immune cell-based cardiovascular risk assessment: Spotlight on the neutrophil-lymphocyte ratio. Eur. Heart J. 42(9), 904–906 (2021).
Shurtz-Swirski, R. et al. Involvement of peripheral polymorphonuclear leukocytes in oxidative stress and inflammation in type 2 diabetic patients. Diabetes Care 24(1), 104–110 (2001).
Wong, S. L. et al. Diabetes primes neutrophils to undergo NETosis, which impairs wound healing. Nat. Med. 21(7), 815–819 (2015).
Zhang, X. et al. The neutrophil-to-lymphocyte ratio is associated with all-cause and cardiovascular mortality among individuals with hypertension. Cardiovasc. Diabetol. 23(1), 117 (2024).
De Servi, S., Landi, A. & Savonitto, S. Clopidogrel induced reduction in neutrophil count: An overlooked beneficial effect? Eur. J. Intern. Med. (2024).
Sethuramalingam, S., Maiti, R., Hota, D. & Srinivasan, A. Effect of colchicine in reducing inflammatory biomarkers and cardiovascular risk in coronary artery disease: A meta-analysis of clinical trials. Am. J. Ther. 30(3), e197–e208 (2023).
Acknowledgements
We greatly appreciated the contributions of NHANES participants and staff.
Funding
This work is supported by the National Natural Science Foundation of China (No. 81870336, No. 82300530); Natural Science Foundation of Changsha, China (No. kq2208307); Natural Science Foundation of Hunan Province, China (No. 2023JJ40843).
Author information
Authors and Affiliations
Contributions
B.Z. and W.L. conceived and designed the study. B.Z., Yu.L. organized and analyzed the data wrote the manuscript. B.Z., Yu.L., S.W. and C.C. prepared the figures. Y.C., Yo.L., X.G. and Y.Y. edited the manuscript. D.P. proofread the manuscript. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The NHANES study was formally approved by the National Center for Health Statistics Research Ethics Review Board. All participants signed a written informed consent form.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhu, B., Liu, Y., Liu, W. et al. Association of neutrophil-to-lymphocyte ratio with all-cause and cardiovascular mortality in CVD patients with diabetes or pre-diabetes. Sci Rep 14, 24324 (2024). https://doi.org/10.1038/s41598-024-74642-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-74642-8
Keywords
This article is cited by
-
Interpretable machine learning method to predict the risk of pre-diabetes using a national-wide cross-sectional data: evidence from CHNS
BMC Public Health (2025)
-
Neutrophil percentage to albumin ratio predicts cardiovascular and all-cause mortality in diabetes and pre diabetes patients
Scientific Reports (2025)