Abstract
Low serum albumin levels increase coronary morbidity, mortality, and postoperative cardiovascular risk. Therefore, this study investigated the relationship between these levels and the length of hospital stay in patients undergoing percutaneous coronary intervention (PCI) for acute coronary syndrome. A total of 350 patients were divided into quartiles according to serum albumin levels. Univariate and multivariate analyses were performed to identify factors associated with the length of hospital stay. A non-linear regression analysis of serum albumin and length of hospital stay was also performed. The results of the multifactorial analysis revealed low serum albumin levels as an independent predictor of longer hospital stay, even in the fully adjusted model. In the segmented linear regression model, serum albumin level showed a U-shaped relationship with the length of hospital stay. In conclusion, low serum albumin level was an independent predictor of longer hospital stay in patients undergoing PCI for acute coronary syndrome, with shorter stays observed for increasing serum albumin levels. Low serum albumin can be used to identify patients who require longer hospitalization and may need additional nutritional support or interventions to improve their prognosis.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the most common cause of mortality and morbidity worldwide, in which acute coronary syndrome (ACS) is a primary clinical manifestation of CVD1. ACS is a serious cardiac condition caused by unstable rupture or erosion of atherosclerotic plaques within the coronary arteries, followed by the formation of fresh blood clots leading to acute ischaemia of the myocardium. ACS includes ST-segment elevation myocardial infarction (STEMI), non-ST-segment elevation myocardial infarction (NSTEMI), and unstable angina (UA)1,2. Percutaneous coronary intervention (PCI) uses balloons and stents to dilate stenotic or obstructive sites in the coronary arteries, thereby restoring blood flow, alleviating myocardial ischemia, and improving patient clinical prognosis. No substitute for PCI exists in the treatment of ACS, especially in the management of STEMI1,2,3.
Serum albumin is the most abundant protein in human plasma and reflects not only nutritional status4,5but also plays important roles, such as in inflammation6,7, platelet aggregation8,9, and antioxidant regulation10,11. Albumin, as a negative acute phase protein, decreases in levels during inflammation. It possesses antioxidant properties, enabling it to scavenge free radicals and inhibit the expression of inflammatory mediators, thereby mitigating inflammatory damage. Additionally, it regulates the inflammatory response by binding and transporting these mediators12.Inflammation plays a crucial role in the pathogenesis of acute coronary syndrome (ACS). It not only promotes the development of atherosclerosis but also plays a key role in plaque rupture and thrombosis, which are the main pathological bases of ACS. In particular, the activation of inflammatory cells and mediators contributes to plaque instability and rupture, leading to acute occlusion of the coronary arteries13. The relative risks of coronary heart disease (CHD) morbidity and mortality14, cardiovascular disease mortality15, and all-cause mortality16,17are elevated in individuals with low serum albumin levels compared with those with high serum albumin levels. Hypoalbuminemia is also associated with poor reperfusion at the epicardial and tissue level after PCI18. Moreover, a decrease in albumin levels is associated with the occurrence of atrial fibrillation and the risk of mortality, especially in elderly patients with dual-chamber permanent pacemaker implantation19. In patients with ST-segment elevation myocardial infarction, newly developed atrial fibrillation is a common and serious complication closely linked to long-term mortality20. The uric acid/albumin ratio has been shown to have independent predictive value as a biomarker for predicting new-onset atrial fibrillation21. These findings further emphasize the important role of albumin in cardiovascular diseases and suggest its potential application value in disease management, risk assessment, and treatment. As low serum albumin levels increase coronary morbidity and mortality, poor reperfusion after PCI, and postoperative cardiovascular risk, we hypothesized that low serum albumin may be associated with a longer hospital stay in patients undergoing PCI for ACS. Therefore, the present study investigated this relationship.
Methods
This retrospective cohort study included non-selective consecutive patients diagnosed with ACS, including UA, STEMI, and NSTEMI, who underwent PCI in the Department of Cardiovascular Medicine of the Second People’s Hospital of Shenzhen, China. To protect patient privacy, these data did not include identifiable participants. The data were obtained from the hospital’s electronic medical record system. The Ethics Committee of the Affiliated Hospital of Shenzhen University approved this study (ethics number: 2024-021-02PJ), which was conducted in accordance with the principles of the Declaration of Helsinki. All patients participating in the study provided written informed consent.
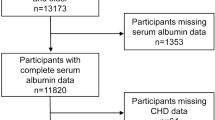
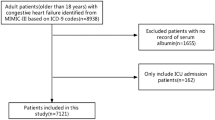
Data were collected on a total of 2490 patients undergoing catheterization laboratory procedures between 1 January 2021 and 31 December 2023. The inclusion criteria were patients diagnosed with ACS who underwent PCI. The exclusion criteria were no baseline serum albumin data, postoperative request for transfer or abandonment of treatment to home, and intraoperative or preoperative death of patients who did not complete the procedure. Based on the inclusion/exclusion criteria, 1,493 patients without ACS, 586 patients who did not undergo PCI, and 66 patients without pre-count serum albumin data were excluded. Finally, this study included 345 cases.
Data collection
The primary study outcome was the patient’s length of stay, which was calculated as the number of days between the date of discharge and the date of admission. The clinical and demographic characteristics of patients were obtained from hospital files and computerized records. The covariates included demographic data, variables affecting the severity of coronary artery disease and length of hospital stay reported in previous studies22,23,24, and clinical data. A fully adjusted model was constructed using continuous variables (age, white blood cell [WBC] count, platelet count [PLT], hemoglobin (HGB) level, ultrasensitive C-reactive protein [Hs-CRP] level, potassium ion (K+) level, cardiac troponin I [cTnI] level, high-density lipoprotein cholesterol [HDL-C] level, low-density lipoprotein cholesterol [LDL-C] level, and ejection fraction [EF] obtained at baseline); and categorical variables (sex, chronic heart failure [CHF], chronic renal insufficiency [CRF], history of PCI, old myocardial infarction [OMI], stroke, hypertension, diabetes mellitus, smoking, intravascular ultrasound [IVUS], and aortic balloon counterpulsation pump [IABP]).
Statistical methods
Patients were categorized into four groups (Q1–4) based on the quartiles of their serum albumin levels measured prior to percutaneous coronary intervention (PCI). The specific ranges of serum albumin levels for each group were determined by the distribution of data collected from all participants, which were as follows: ≤32.9 g/L, 32.9–37.9 g/L, 37.9–42.9 g/L, and > 42.9 g/L. Normally distributed continuous variables are expressed as means ± standard deviation (SD). Continuous variables with a skewed distribution are expressed as medians [interquartile range]. Categorical variables are expressed as numbers (n) and percentages (%). The characteristics of the study population were compared according to serum albumin levels.
We assessed the relationship between serum albumin levels and the length of hospital stay. One-way analyses were first performed to compare the differences between different albumin quartiles using the chi-squared test (for categorical variables), one-way analysis of variance (ANOVA) (for normal distribution), or the Kruskal–Wallis H test (for skewed distribution). Multivariate linear regression analyses were performed to control for potential confounding factors. Model 1 was unadjusted, while Models 2 and 3 were adjusted. In addition, segmented linear regression was used to explore the threshold effect of serum albumin levels on the length of hospital stay according to the smoothing plots.
P < 0.05 was considered to be statistically significant. Data analyses were performed using the Empower Stats statistical package (http://www.empowerstats.com; X&Y Solutions, Inc., Boston, MA, USA).
Results
Baseline participant characteristics
Among 2490 patients initially assessed, 345 were finally included in this study after applying the inclusion and exclusion criteria. Table 1 demonstrates the baseline characteristics of the patients who participated in the study. Participants with lower serum albumin levels had older ages, lower platelet and haemoglobin levels, more right coronary artery lesions, and more frequent use of IABP during surgery, while anterior descending branch lesions were more likely to be observed in participants with higher serum albumin levels.
Univariate and multivariate analyses
The results of the univariate analysis showed that WBC count, Hr-CRP, BG, LVEF, IVUS, and IABP were strongly associated with the length of hospital stay (Table 2). The results of the multivariate analysis indicated that lower serum albumin levels were significantly associated with longer hospital stays (Table 3). In Model 1 (unadjusted), the length of stay first decreased and then increased with increasing serum albumin levels (Q2 vs. Q1, odds ratio [OR] -1.00, 95% confidence interval [CI] -1.80, -0.20, P = 0.015; Q3 vs. Q1, OR -1.56, 95%CI -2.35, -0.76, P < 0.001; Q4 vs. Q1, OR -1.26, 95%CI -2.06, -0.46, P < 0.001). In Model 2 after adjusting for sex, age, hypertension, diabetes mellitus, hyperlipidaemia, smoking, OMI, PCI, shock, CKD, CHF, HGB, Hs-CRP, BG, LVEF, IVUS, IABP, PLT, K+, cTnI, LDL-C, and HDL-C. The relationship between serum albumin levels and length of stay remained consistent with Model 1 (categorical variables: Q2 vs. Q1, OR -0.99, 95%CI -1.89, -0.09, P = 0.032; Q3 vs. Q1, OR -1.02, 95%CI -1.97, -0.07, P = 0.036; Q4 vs. Q1, OR -0.62, 95%CI-1.66, 0.43, P = 0.248). After further smoothing for age, HGB, Hs-CRP, BG, LVEF, PLT, K+, cTnI, LDL-C, and HDL-C in Model 3, the relationship between serum albumin levels and length of hospital stay remained significant (categorical variables: Q2 vs. Q1, OR -0.92, 95%CI -1.79, -0.05, P = 0.040; Q3 vs. Q1, OR -1.08, 95%CI -2.00, -0.16, P = 0.022; Q4 vs. Q1, OR -0.70, 95%CI -1.71, 0.30, P = 0.173).
Non-linear regression of serum albumin and length of hospital stay
Analysis of the relationship between serum albumin levels and length of hospital stay, after adjusting for sex, leukocytes, HBG, Hs-CRP, BG, LVEF, IVUS, and offender vascularity, showed a U-shaped relationship between serum albumin level and length of hospital stay (Fig. 1).
We also performed a threshold effect analysis and calculated an inflection point of 39.9. When serum albumin levels were < 39.9 g/L, the length of hospital stay decreased with increasing serum albumin level (OR -0.29, 95% CI -0.43, -0.16 P < 0.001). When serum albumin levels were > 39.9, the length of hospital stay increased with increased serum albumin level (OR 0.09, 95% CI -0.09, -0.36 P = 0.331).
Discussion
This retrospective study analysed the relationship between serum albumin levels and length of hospital stay in 345 patients with ACS treated with PCI. We observed a U-shaped relationship between serum albumin level and length of hospital stay. The inflection point in threshold effect analysis was 39.9; thus, among patients with serum albumin levels < 39.9 g/L, the length of hospital stay decreased with increasing serum albumin (OR -0.29, 95% CI -0.43, -0.16 P < 0.001). In contrast, the effect of serum albumin > 39.9 g/L on the length of hospital stay was not significant (P = 0.331).
Our study findings are consistent those of Hideki Wada et al. and Oduncu et al. who demonstrated that low serum albumin concentrations are linked to poor outcome in patients with CAD and PCI16,25,26. The present study confirmed the association between serum albumin levels and hospital length of stay in patients diagnosed with ACS who underwent PCI. After adjusting for several potential confounders, we found that patients with serum albumin levels < 39.9 g/L experienced decreasing length of stay with increasing serum albumin levels, suggesting that, below a certain threshold, improved clinical recovery and shorter hospital stays are achieved by increasing serum albumin levels.
The mechanism underlying the U-shaped relationship between serum albumin and length of hospital stay is unclear. Low serum albumin levels are associated with higher SYNTAX score27, which is an independent predictor of freedom from regurgitation and in-stent restenosis after primary PCI28, as well as increased risks of several PCI complications, including contrast-induced acute renal failure29and new-onset cardiac insufficiency25,30. Serum albumin is not only a biomarker of nutritional status but is also involved in a variety of physiological processes, including the maintenance of colloid osmotic pressure, transport of a variety of compounds, modulation of inflammatory responses, and antioxidant activity4,5,6,7,8,9,10,11,31. The possible mechanisms linking low serum albumin levels to longer hospital stays include reduced albumin levels leading to a weakening of its antioxidant effect, causing increased oxidative stress, vascular endothelial cell damage32, and atherosclerosis promotion, thereby increasing the risk of cardiovascular events. Albumin helps prevent endothelial dysfunction by maintaining the integrity and function of the vascular endothelium. In an inflammatory state, the synthesis of acute phase proteins such as C-reactive protein and fibrinogen is increased in the liver, whereas albumin synthesis may be inhibited33, leading to a decrease in serum albumin levels, while the ACS counters the hyperinflammatory state34. Inflammation induces increased vascular permeability and impaired endothelium-dependent vasodilatation, which exacerbates cardiac insufficiency and may also directly impair cardiac function, leading to heart failure35. Finally, albumin has anticoagulant properties and is a potent inhibitor of platelet aggregation. As a result, platelets are activated when albumin levels decrease, leading to an increased risk of cardiovascular events36,37,38,39.
Serum albumin level has long been considered the primary indicator of malnutrition. However, the role of nutritional support in patients undergoing PCI for ACS is unclear: the results of the PICNIC study showed that nutritional intervention improved the prognosis of malnourished patients with acute heart failure40, while in patients with acute heart failure, the effect of nutritional intervention was consistent in hypoalbuminemic and normoalbuminemic patients compared with conventional treatment41. The significant protective effect of serum albumin observed in the present study further confirms its role in nutritional support. However, empirical support for the role of nutritional support such as albumin supplementation in patients with ACS is lacking; therefore. further research and evaluation are required.
This study has several limitations. First, as a retrospective observational study, this study has design limitations. Second, the study was performed in a single centre, and the population studied was mainly post-PCI patients with ACSs; hence, the findings are not applicable to the entire population. The research findings should take into account the potential impact of conditions such as acute infections and chronic inflammation on serum albumin levels, which were not excluded from our patient cohort. Although we aimed to include a representative sample of ACS patients without excluding these conditions, we acknowledge that this approach may introduce variability in the data. Finally, although we adjusted for confounders that may have been associated with the results, some unrecorded confounders may have affected the results. Therefore, a larger population and higher-level clinical trials are required.
Conclusions
Low serum albumin level was an independent predictor of longer hospital stays in patients undergoing PCI for ACS. Serum albumin levels showed a U-shaped relationship with the length of hospital stay, with an inflection point of 39.9 g/L. Low serum albumin may be used as a tool to identify patients who require longer hospitalization and may need additional nutritional support or interventions to improve their prognosis. Further evaluation and higher-level clinical trials are necessary to confirm and extend our findings.
Data availability
The data sets used and/or analysed in this study are available on request from the corresponding author.
References
Byrne, R. A. et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur. Heart J. 44, 3720–3826 (2023).
Kimura, K. et al. JCS 2018 guideline on diagnosis and treatment of acute coronary syndrome. Circ. J. 83, 1085–1196 (2019).
Chinese Society of Cardiology of Chinese Medical Association & Editorial Board of Chinese Journal of Cardiology. 2019 Chinese Society of Cardiology (CSC) guidelines for the diagnosis and management of patients with ST-segment elevation myocardial infarction. Zhonghua Xin Xue Guan Bing Za Zhi 47, 766–783 (2019).
Phillips, A., Shaper, A. G. & Whincup, P. H. Association between serum albumin and mortality from cardiovascular disease, cancer, and other causes. Lancet. 2, 1434–1436 (1989).
Gillum, R. F., Ingram, D. D. & Makuc, D. M. Relation between serum albumin concentration and stroke incidence and death: the NHANES I epidemiologic follow-up study. Am. J. Epidemiol. 140, 876–888 (1994).
Andus, T., Geiger, T., Hirano, T., Kishimoto, T. & Heinrich, P. C. Action of recombinant human interleukin 6, interleukin 1 beta and tumor necrosis factor alpha on the mRNA induction of acute-phase proteins. Eur. J. Immunol. 18, 739–746 (1988).
Grimble, R. Serum albumin and mortality (letter). Lancet. 335, 350 (1990).
Goodman, D. S. The interaction of human serum albumin with long-chain fatty acid anions. J. Am. Chem. Soc. 80, 3892–3898 (1958).
Doweiko, J. P. & Bistrian, B. R. The effect of glycosylated albumin on platelet aggregation. JPEN J. Parenter. Enter. Nutr. 18, 516–520 (1994).
Halliwell, B. Albumin—an important extracellular antioxidant? Biochem. Pharmacol. 37, 569–571 (1988).
Cross, C. E. et al. Oxygen radicals and human disease. Ann. Intern. Med. 107, 526–545 (1987).
Sheinenzon, A. et al. Serum albumin levels and inflammation. Int. J. Biol. Macromol. 184, 857–862 (2021).
Cimmino, G. et al. Pathophysiology and mechanisms of Acute Coronary syndromes: atherothrombosis, immune-inflammation, and beyond. Expert Rev. Cardiovasc. Ther. 20, 351–362 (2022).
Nelson, J. J. et al. Serum albumin level as a predictor of incident coronary heart disease: the atherosclerosis risk in communities (ARIC) study. Am. J. Epidemiol. 151, 468–477 (2000).
Plakht, Y., Gilutz, H. & Shiyovich, A. Decreased admission serum albumin level is an independent predictor of long-term mortality in hospital survivors of acute myocardial infarction. Soroka acute myocardial infarction II (SAMI-II) project. Int. J. Cardiol. 219, 20–24 (2016).
Wada, H. et al. Impact of serum albumin levels on long-term outcomes in patients undergoing percutaneous coronary intervention. Heart Vessels. 32, 1085–1092 (2017).
Chien, S. C. et al. Association of low serum albumin concentration and adverse cardiovascular events in stable coronary heart disease. Int. J. Cardiol. 241, 1–5 (2017).
Rezkalla, S. H. & Kloner, R. A. Coronary no-reflow phenomenon: from the experimental laboratory to the cardiac catheterization laboratory. Catheter Cardiovasc. Interv. 72, 950–957 (2008).
Hayıroğlu, M. İ. et al. Prognostic value of serum albumin for long-term mortality in patients with dual-chamber permanent pacemakers. Biomark. Med. 16, 341–348 (2022).
Hayıroğlu, M. İ. et al. Cardiac variables associated with atrial fibrillation occurrence and mortality in octogenarians implanted with dual chamber permanent pacemakers. Aging Clin. Exp. Res. 34, 2533–2539 (2022).
Selçuk, M. et al. Predictive value of uric acid/albumin ratio for the prediction of new-onset atrial fibrillation in patients with ST-Elevation myocardial infarction. Rev. Invest. Clin. 74, 156–164 (2022).
Miyazaki, D., Tarasawa, K., Fushimi, K. & Fujimori, K. Risk factors with 30-day readmission and the impact of length of hospital stay on it in patients with heart failure: a retrospective observational study using a Japanese National database. Tohoku J. Exp. Med. 259, 151–162 (2023).
Hassen, C. B. et al. Change in lipids before onset of dementia, coronary heart disease, and mortality: a 28-year follow-up Whitehall II prospective cohort study. Alzheimers Dement. 19, 5518–5530 (2023).
Houghton, D. E. et al. Hemoglobin levels and coronary heart disease risk by age, race, and sex in the reasons for geographic and racial differences in stroke study (REGARDS). Am. J. Hematol. 95, 258–266 (2020).
Oduncu, V. et al. The prognostic value of serum albumin levels on admission in patients with acute ST-segment elevation myocardial infarction undergoing a primary percutaneous coronary intervention. Coron. Artery Dis. 24, 88–94 (2013).
Hartopo, A. B., Gharini, P. P. R. & Setianto, B. Y. Low serum albumin levels and in-hospital adverse outcomes in acute coronary syndrome. Int. Heart J. 51, 221–226 (2010).
Kurtul, A. et al. Usefulness of serum albumin concentration to predict high coronary SYNTAX score and in-hospital mortality in patients with acute coronary syndrome. Angiology. 67, 34–40 (2016).
Kurtul, A. et al. Serum albumin levels on admission are associated with angiographic no-reflow after primary percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction. Angiology. 66, 278–285 (2015).
Murat, S. N., Kurtul, A. & Yarlioglues, M. Impact of serum albumin levels on contrast-induced acute kidney injury in patients with acute coronary syndromes treated with percutaneous coronary intervention. Angiology. 66, 732–737 (2015).
Gopal, D. M. et al. Serum albumin concentration and heart failure risk the health, aging, and body composition study. Am. Heart J. 160, 279–285 (2010).
Li, X. et al. J-shaped association between serum albumin levels and long-term mortality of cardiovascular disease: experience in National Health and Nutrition Examination Survey (2011–2014). Front. Cardiovasc. Med. 9, 1073120 (2022).
Lang, J. D. Jr et al. Albumin and hydroxyethyl starch modulate oxidative inflammatory injury to vascular endothelium. Anesthesiology. 100, 51–58 (2004).
Moshage, H. J., Janssen, J. A., Franssen, J. H., Hafkenscheid, J. C. & Yap, S. H. Study of the molecular mechanism of decreased liver synthesis of albumin in inflammation. J. Clin. Invest. 79, 1635–1641 (1987).
Elhajj, I. I., Haydar, A. A., Hujairi, N. M. & Goldsmith, D. J. The role of inflammation in acute coronary syndromes: review of the literature. J. Med. Liban. 52, 96–102 (2004).
Cheng, T. et al. The relationship between a series of inflammatory markers on the risk of heart failure in different gender groups: analysis from NHANES 2015–2018. PLOS ONE. 19, e0296936 (2024).
Gresele, P., Deckmyn, H., Huybrechts, E. & Vermylen, J. Serum albumin enhances the impairment of platelet aggregation with thromboxane synthase inhibition by increasing the formation of prostaglandin D2. Biochem. Pharmacol. 33, 2083–2088 (1984).
Mikhailidis, D. P. & Ganotakis, E. S. Plasma albumin and platelet function: relevance to atherogenesis and thrombosis. Platelets. 7, 125–137 (1996).
Linden, M. D., Jackson, D. E. & Platelets Pleiotropic roles in atherogenesis and atherothrombosis. Int. J. Biochem. Cell. Biol. 42, 1762–1766 (2010).
Gawaz, M., Langer, H. & May, A. E. Platelets in inflammation and atherogenesis. J. Clin. Invest. 115, 3378–3384 (2005).
Bonilla-Palomas, J. L. et al. Nutritional intervention in malnourished hospitalized patients with heart failure. Arch. Med. Res. 47, 535–540 (2016).
Ramiro-Ortega, E. et al. Nutritional intervention in acute heart failure patients with undernutrition and normal buminemia: a subgroup analysis of PICNIC study. Clin. Nutr. 37, 1762–1764 (2018).
Acknowledgements
All authors declare that there exist no acknowledgments.
Author information
Authors and Affiliations
Contributions
HB.C: Conceptualisation, formal analysis, investigation, methodology, project management, writing - review and editing. D.P: Investigation, data organisation, methodology, writing - original manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pan, D., Chen, H. Relationship between serum albumin level and hospitalization duration following percutaneous coronary intervention for acute coronary syndrome. Sci Rep 14, 23883 (2024). https://doi.org/10.1038/s41598-024-74955-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-74955-8