Abstract
Left ventricular ejection fraction (LVEF) is the most ubiquitous parameter in cardiac imaging examinations, we aimed to investigate the associations between subtle changes of LVEF and risk of common cardiovascular diseases. This is a prospective cohort study based on UK Biobank. LVEF was obtained from cardiac magnetic resonance. Incident cardiovascular disease was the outcome, including heart failure, atrial fibrillation, ischemic heart disease, and myocardial infarction. Cox proportional hazard model was the main method. A U-shaped relationship was observed between quantified LVEF and cardiovascular events risk with the nadir at the LVEF of 55–64%. As compared to moderate LVEF (55–64%), both low (40–54%) and high LVEF ( ≥ 5%) were related to higher risk of cardiovascular diseases after adjusting for confounders (HRlow = 1.15, 95%CI = 1.02–1.30; HRhigh = 1.34, 95%CI = 1.05–1.72). Specifically, low LVEF was associated with increased risk of heart failure while high LVEF predominantly predicted elevated risk of ischemic heart diseases, both low and high LVEF were related to a borderline higher incidence of atrial fibrillation. Besides, associations with specific cardiovascular diseases varied by age, sex or comorbidities. There was a U-shaped relationship between LVEF and cardiovascular events risk with the nadir at the LVEF of 55–64%, while these associations were disease-specific and varied by age, sex or comorbidities.
Similar content being viewed by others
Introduction
Left ventricular ejection fraction (LVEF) is the most commonly-used measure for left ventricular systolic function assessment. The major strength of LVEF is universally known, broadly accepted, and easy to be obtained by using any cardiac imaging technique, such as echocardiography and cardiovascular magnetic resonance (CMR)1. The threshold of LVEF (< 40%) has been recognized to define heart failure with reduced ejection fraction, and studies of LVEF always focused on the outcome of heart failure1,2,3,4,5,6,7. Recently, some studies have investigated the association between quantified LVEF levels and survival in populations with cardiovascular disease8,9,10,11. For example, both clinical cohorts from US and New Zealand observed the lowest mortality in participants with LVEF of 60.0–65.0%, while another Australia register-based cohort found that the mortality was lowest among participants with LVEF of 65.0–69.9%8,9. Although LVEF has been linked to cardiovascular mortality, fewer studies focused on the role in the incidence of cardiovascular diseases (except for heart failure), even rarely studied among specific populations. A recent cohort study has explored the relationship between supranormal LVEF and risk of major adverse cardiovascular events12. In this study, we aimed to explore the association of LVEF with the risk of common cardiovascular diseases among population free of cardiovascular diseases at imaging in the UK Biobank cohort.
Methods
Study design and population
As reported previously, over 500 000 individuals with the age of 40–69 years were enrolled from the UK13. Baseline information were collected between March 2006 and July 2010 via online or/and verbal questionnaires, a series of physical measurements, and biological sample tests from 22 assessment centers. Individuals lack of baseline assessment were excluded.
In the present study, only individuals who attended imaging visit were included in analyses, and individuals were excluded if they:1 had a history of cardiovascular disease before imaging visit2, had a LVEF of < 40%, or3 were followed up for less than 180 days. Finally, a total of 35,277 individuals without cardiovascular disease and without recognized-reduced ejection fraction at baseline were included (Fig. 1).
Cardiac magnetic resonance
Cardiac magnetic resonance (CMR) was performed for participants during the imaging visit (instance 2) based on a pre-determined protocol. The details of the protocol have been described elsewhere14,15,16. Briefly, CMR imaging was performed on a clinical wide bore 1.5 Tesla scanner (MAGNETOM Aera, Syngo Platform VD13A, Siemens Healthcare, Erlangen, Germany) in Cheadle, United Kingdom. Three long axis cines (horizontal long axis, vertical long axis and left ventricular outflow tract cines including both sagittal and coronal) and a complete short axis stack of balanced steady state free precession (bSSFP) cines were acquired for the left ventricle at one slice per breath hold14,15,16. Fully automated quality-controlled image analysis pipeline was applied to obtain CMR indices, including LVEF, which was previously validated in the subpopulation of UK Biobank17,18,19.
Assessment of outcomes
The primary outcome was incident cardiovascular disease, defined as any investigational cardiovascular event in this study, including heart failure, atrial fibrillation and flutter, ischemic heart diseases and myocardial infarction. The secondary outcome was incident specific cardiovascular disease. Heart failure, atrial fibrillation and flutter, and ischemic heart diseases were identified from fields of “First occurrence (Category ID: 1712)” by using the International Classification of Disease 10 (ICD-10) I50 (Field ID:131355), I48 (Field ID:131351), I20-I25 (Field ID:131297, 131299, 131301, 131303, 131305 and 131307), respectively. Myocardial infarction were identified from fields of “Algorithmically-defined outcomes (Category ID: 42)” by using Field ID of 42,001, details of ICD codes are described elsewhere20. Both fields of “First occurrence” and “Algorithmically-defined outcomes” were derived from self-reported medical conditions, primary health care, hospital admission data and death registry data for the entire cohort.
Assessment of covariates
Age was calculated by using difference between birth year and year of imaging. Sex, ethnic and educational background were recorded from self-reported at baseline of UK Biobank. Ethnic background was dichotomized as British or not. Education was recorded as seven categories (i.e., College or University degree, Advanced [A] levels/Advanced Subsidiary [AS] levels or equivalent, Ordinary [O] levels/General Certificate of Secondary Education [GCSE] or equivalent, Certificate of Secondary Education [CSE] or equivalent, National Vocational Qualification [NVQ] or Higher National Diploma [HND] or Higher National Certificate [HNC] or equivalent, other professional qualifications, and unknown qualifications). Socioeconomic status was recorded as the Townsend deprivation index at baseline, which is calculated based on the preceding national census output areas21. Smoking status was obtained from self-report at imaging visit and recorded as never, former, current and unknown. Alcohol intake frequency was obtained from self-report at imaging visit and categorized into daily, often (i.e., one to four times a week), seldom (i.e., one to three times a month or special occasions only), never and unknown. Body mass index (BMI) was measured at imaging visit. Physical activity was assessed as a continuous variable of summed metabolic equivalent (MET) minutes per week for all activity22,23. Average heart rate was obtained during CMR. Comorbidities (i.e., diabetes, high cholesterol or hypertension) were defined by combining self-report medical conditions, self-report medications and biochemistry data at imaging visit (Glycosylated haemoglobin > 48 mmol/mol, total cholesterol > 7 mmol/L, and systolic blood pressure > 140 mmHg or diastolic blood pressure > 90 mmHg, respectively).
Statistical analysis
Participants were followed up from the date of imaging to the date of any cardiovascular event, date of death, date of loss-to-follow, or the censoring date (May 20, 2022), whichever came first. Cox proportional hazard model with categorized LVEF (per 5-unit increment) or with restricted cubic spline (three knots) were first used to assess the association between LVEF and risk of cardiovascular events. Adjustments were made for age at imaging, sex, ethnic background, education, townsend deprivation index, BMI, heart rate, physical activity, smoking, alcohol intake and comorbidities. Based on results from Cox proportional hazard model with categorized LVEF (per 5-unit increment) or with restricted cubic spline mentioned above, participants were divided into three groups based on LVEF (Low: 40–55%; Moderate: 55–64%; High: ≥ 65%) for descriptive analyses and incidence rate calculations. Continuous variables are described as mean and SD, and categorical variables described as the frequencies and percentages. Cox proportional hazard models were further conducted by using the group with moderate LVEF as the reference group, and stratified analyses were performed by sex, age and comorbidities. And proportional hazard assumption was tested by Schoenfeld residuals test (Supplementary Fig. 1). All analyses were conducted in SAS 9.4 or R 4.1.2 and P-value of < 0.05 was considered as statistical significance.
Results
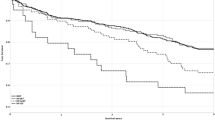
As shown in Table 1, a total of 35,277 participants were included in the study, consisting of 16,011 males (45.4%) and 19,266 females (54.6%). Most participants had a LVEF of 55–59% (n = 12,811, 36.32%), followed by 50–54% (n = 8,717, 24.71%) and 60–64% (n = 7,893, 22.37%) (Supplementary Table 1). Overall, the mean age was 63.67 years, after a mean follow-up of 4.5 years, there were 1229 (3.5%) participants diagnosed with one or more investigational cardiovascular events, 129 (0.4%) with heart failure, 446(1.3%) with atrial fibrillation or flutter, 610 (1.7%) with ischemic heart diseases, and 229 (0.7%) with myocardial infarction. Figure 2A presents results from multivariable restricted cubic spline regressions, in which participants with a LVEF of 55–59% had the lowest risk of overall cardiovascular events. Figure 2B showed the results from multivariable Cox proportional hazard models with categorized LVEF (per 5-unit increment) by using the group with a LVEF of 55–59% as reference, in which similar risk was observed between the reference group and those with a LVEF of 50–54% or 60–64%. Overall, both analyses indicated a U-shaped relationship between LVEF and cardiovascular events risk with the nadir at the LVEF of 55–64%.
Association between quantified LVEF and risk of cardiovascular outcomes. (A) Restricted cubic spline; (B) Categorized LVEF (per 5-unit increment). *Adjusted for age, sex, ethnic background, education, townsend deprivation index, BMI, heart rate, physical activity, smoking, alcohol intake and comorbidities.
Based on results above, LVEF was further categorized into three groups: low (< 55%), moderate (55–64%) and high (≥ 65%). Table 1 presented the details of descriptive analyses between three groups. Table 2 presents results from multivariable Cox proportional hazard models by using the group with moderate LVEF as the reference group. As compared to the group with moderate LVEF, after adjusted for potential confounders in model 2, groups with low or high LVEF was significantly related to a higher risk of overall cardiovascular events (HRlow=1.15,95%CI = 1.02–1.30; HRhigh=1.34,95%CI = 1.05–1.72). Low LVEF was associated with increased risk of heart failure (HR = 1.69,95%CI = 1.17–2.43) while high LVEF was related to higher risk of ischemic heart disease (HR = 1.56,95%CI = 1.13–2.15), including myocardial infarction (HR = 1.70,95%CI = 1.00-2.88); both high and low LVEF were associated with a borderline higher risk of atrial fibrillation (HRlow=1.21,95%CI = 1.00-1.48; HRhigh=1.46,95%CI = 0.98–2.17).
Stratified analyses suggested that the role of LVEF varied by age, sex and comorbidities. As shown in Table 3, there was significant sex-based differences in the observed associations, in which a low LVEF was mainly related to a higher risk of cardiovascular events in females (HR = 1.16,95%CI = 1.00-1.33), specifically heart failure and atrial fibrillation; while high LVEF predominantly predicted an increased risk of cardiovascular events in males (HR = 1.41,95%CI = 1.02–1.95), specifically ischemic heart disease, myocardial infarction and atrial fibrillation. In Table 4, stratified analyses by age found that low LVEF played a more important role in younger population (< 65 years old), specifically associated with 2.46 times higher risk of heart failure; high LVEF seemed to have similar associations between young and older population with cardiovascular diseases, for example, with similar increased incidence of ischemic heart disease (HR< 65yrs = 1.66 vs. HR≥ 65yrs = 1.52). In Table 5, stratified analyses by comorbidities indicated interactions between LVEF and comorbidities. Both low and high LVEF was significantly associated with higher risk of overall cardiovascular events among participants with overweight/obesity or hypertension. Although stratified analyses by high cholesterol observed a significant positive association between high LVEF and overall cardiovascular events risk among participants without high cholesterol rather than those with, further analyses showed that the association of LVEF with ischemic heart disease and myocardial infarction was stronger among participants with high cholesterol (Supplementary Table 4). A stronger but without significant association between high LVEF and overall cardiovascular events risk among participants with diabetes was probably related to the relative smaller sample size. Details of stratified analyses for specific cardiovascular disease are presented in Supplementary Tables 2–5.
Discussion
Despite widespread use of LVEF in clinical practice, the role of LVEF in the risk of cardiovascular events has rarely been investigated. This study evaluated the associations between LVEF and risk of cardiovascular events in general population from UK Biobank cohort. Analyses from both Cox proportional hazard model with restricted cubic spline and categorized LVEF (per 5-unit increment) indicated a U-shaped relationship between quantified LVEF and risk of cardiovascular diseases with the nadir at the LVEF of 55–64%. We then performed analyses by using moderate LVEF (55–64%) as reference group. Interestingly, these observed associations were disease-specific, low LVEF (40-54%) was mainly associated with increased risk of heart failure while high LVEF (≥ 6%) predominantly predicted elevated risk of ischemic heart diseases, both low and high LVEF was related to higher incidence of atrial fibrillation. Besides, associations with specific cardiovascular diseases varied by age, sex or comorbidities. As compared to the group with moderate LVEF, for females, low LVEF was specifically associated with an increased risk of heart failure and atrial fibrillation, while no association was found between high LVEF and any cardiovascular disease. For males, in contrast, high LVEF but not low LVEF was associated with an elevated risk of cardiovascular diseases, specifically with the risk of myocardial infarction, ischemic heart disease and atrial fibrillation. The deviation of LVEF showed a stronger association with some specific cardiovascular disease among younger participants and participants with comorbidities.
Left ventricle is the main chamber of heart, we thus hypothesized that LV function impairment was related to the risk of cardiovascular diseases. LVEF is the most ubiquitous parameter to assess the systolic function of left ventricle, and LVEF < 40% is recognized as the threshold of heart failure with reduced EF. Some studies have investigated the relationships between LVEF and the prognosis of cardiovascular diseases8,9,10,11. For example, a cohort study with 203,135 patients from US regional healthcare system showed a U-shaped relationship between LVEF and all-cause mortality, with the lowest mortality at a LVEF of 60–65%9, besides patients with LVEF ≥ 70% had similar mortality risk as those with LVEF of 35–40%9. Similar U-shaped relationships were observed in a validation cohort with 35, 976 patients from New Zealand9. Another Australia cohort study with the largest-scale population also showed a U-shaped relationship between LVEF and mortality, while the lowest mortality was observed at LVEF of 65.0–69.9%8. However, the role of LVEF subtle changes in the incidence of cardiovascular diseases was less studied. A recent pooled cohort study in US, including 6990 individuals with LVEF above 57%, suggested that supranormal LVEF was associated with increased risk of major adverse cardiovascular events, while the sample size is too small to investigate the relation with specific cardiovascular disease12.
The present study observed a similar U-shaped relationship between LVEF and the risk of incident cardiovascular diseases with the nadir at LVEF of 55–64%, but the pattern was different across different cardiovascular diseases. Previous study has suggested that subtle changes of LV systolic function independently predicted an increased risk of heart failure in late life24. Consistently, despite the LVEF was over 40%, a relatively lower LVEF (40-54%) also predicted a significantly increased risk of heart failure in the future in this study. Consistent with the US cohort study mentioned above, we also found a significant relationship between supra-normal LVEF ( > = 65%) and increased incidence of cardiovascular diseases, but specifically related to higher risk of ischemic heart diseases, including myocardial infarction. Both low and high LVEF were related to borderline higher risk of atrial fibrillation, it seemed plausible as both heart failure and ischemic heart disease were positively associated with atrial fibrillation25. Although the underlying mechanism is unclear for the observed increased risk of mortality or incidence of cardiovascular diseases in participants with supra-normal LVEF, several recent cohort studies showed similar U-shaped relationships between LVEF and cardiovascular-related outcomes, thus largely precluding false positive results. The US cohort found a significant effect modification in the association between supra-normal LVEF and cardiovascular diseases by LV stroke volume, indicating that impaired diastolic function might play a role in the observed association12. Our study provided the evidence of disease-specific associations, which might reflect the patholophysiological mechanism of these diseases and provide some clues to explore the underlying mechanisms.
This study further found significant sex-based differences in these observed associations, in which low LVEF had a greater impact for females with an increased risk of heart failure and atrial fibrillation, while males tended to be affected by high LVEF with an increased risk of atherosclerotic diseases and atrial fibrillation. Australia cohort study of cardiovascular mortality mentioned above also found sex-specific associations between LVEF and cardiovascular-related mortality, in which the increased incidence in females with low LVEF were relatively greater than that in males almost across the board, indicating a stronger impact of low LVEF for females8. A retrospective study also reported HFpEF pathophysiologic differences between males and females26. These findings indicated that females might be more sensitive to subtle LVEF reduction. Besides, the role of LVEF seemed to be strengthened in young population or those with comorbidities.
There are some strengths of this study. Firstly, this study covered 35,277 participants, which allowed us to explore disease-specific association. Secondly, cardiac parameters were measured by CMR in UK Biobank cohort, which is recognized as the gold standard to obtain the value of LVEF. Thirdly, information of cardiovascular outcomes were collected from several sources by combining self-report data, health record data and death registry data, minimizing misclassification of outcome. Fourthly, detailed baseline information allowed us to account for potential confounders in the analyses. However, several limitations should be noted. The sample size for investigation of specific cardiovascular disease is still relatively small, especially when analyses were performed using LVEF categorized by per 5-unit increment. Thus, false negative results cannot be ruled out, but the observed significant associations are more notable. Next, reverse causation or residual confounding cannot be eliminated completely. However, we have excluded participants with less than 180 days of follow-up, which we believe could contribute to reducing the probability of reverse causation. At last, most population were European in UK biobank, therefore these findings should be interpreted with caution in other populations and further studies in different populations are needed for validation.
In conclusion, this cohort study showed a U-shaped relationship between LVEF and risk of cardiovascular diseases, and these associations were disease-specific and varied by sex, age and comorbidities.
Data availability
Data described in the manuscript, code book, and analytic code will be made available upon a data access application to UK Biobank and reasonable request to the corresponding authors.
References
Ponikowski, P. et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 18, 891–975 (2016).
Mele, D., Nardozza, M. & Ferrari, R. Left ventricular ejection fraction and heart failure: An indissoluble marriage? Eur. J. Heart Fail. 20, 427–430 (2018).
Curtis, J. P. et al. The association of left ventricular ejection fraction, mortality, and cause of death in stable outpatients with heart failure. J. Am. Coll. Cardiol. 42, 736–742 (2003).
Hall, T. S. et al. Left ventricular ejection fraction and adjudicated, cause-specific hospitalizations after myocardial infarction complicated by heart failure or left ventricular dysfunction. Am. Heart J. 215, 83–90 (2019).
Solomon, S. D. et al. Influence of ejection fraction on cardiovascular outcomes in a broad spectrum of heart failure patients. Circulation 112, 3738–3744 (2005).
Toma, M. et al. The relationship between left ventricular ejection fraction and mortality in patients with acute heart failure: Insights from the ASCEND-HF Trial. Eur. J. Heart Fail. 16, 334–341 (2014).
Tsao, C. W. et al. Prognosis of adults with borderline left ventricular ejection fraction. JACC Heart Fail. 4, 502–510 (2016).
Stewart, S. et al. Ejection fraction and mortality: A nationwide register-based cohort study of 499 153 women and men. Eur. J. Heart Fail. 23, 406–416 (2021).
Wehner, G. J. et al. Routinely reported ejection fraction and mortality in clinical practice: Where does the nadir of risk lie? Eur. Heart J. 41, 1249–1257 (2020).
Angaran, P. et al. Association of Left Ventricular Ejection Fraction with mortality and hospitalizations. J. Am. Soc. Echocardiogr. 33, 802–811 (2020).
Strange, G. et al. Change in ejection fraction and long-term mortality in adults referred for echocardiography. Eur. J. Heart Fail. 23, 555–563 (2021).
Shah, S. et al. Supranormal left ventricular ejection fraction, stroke volume, and cardiovascular risk: Findings from population-based cohort studies. JACC Heart Fail. 10, 583–594 (2022).
Palmer, L. J. UK Biobank: Bank on it. Lancet 369, 1980–1982 (2007).
Petersen, S. E. et al. Imaging in population science: Cardiovascular magnetic resonance in 100,000 participants of UK Biobank—rationale, challenges and approaches. J. Cardiovasc. Magn. Reson. 15, 46 (2013).
Petersen, S. E. et al. UK Biobank’s cardiovascular magnetic resonance protocol. J. Cardiovasc. Magn. Reson. 18, 8 (2016).
Raisi-Estabragh, Z., Harvey, N. C., Neubauer, S. & Petersen, S. E. Cardiovascular magnetic resonance imaging in the UK Biobank: A major international health research resource. Eur. Heart. J. Cardiovasc. Imaging 22, 251–258 (2021).
Olsen, F. J. et al. Left atrial structure and function among different subtypes of atrial fibrillation: An echocardiographic substudy of the AMIO-CAT trial. Eur. Heart. J. Cardiovasc. Imaging 21, 1386–1394 (2020).
Bai, W. et al. Automated cardiovascular magnetic resonance image analysis with fully convolutional networks. J. Cardiovasc. Magn. Reson. 20, 65 (2018).
Petersen, S. E. et al. Reference ranges for cardiac structure and function using cardiovascular magnetic resonance (CMR) in caucasians from the UK Biobank population cohort. J. Cardiovasc. Magn. Reson. 19, 18 (2017).
John Danesh, N. A. et al. UK Biobank Follow-Up and Outcomes Working Group. Algorithmicallydefined outcomes(ADOs). Version 2.0. https://biobank.ndph.ox.ac.uk/ukb/ukb/docs/alg_outcome_main.pdf (2022).
Jarman, B., Townsend, P. & Carstairs, V. Deprivation indices. BMJ Br. Med. J. 303, 523 (1991).
The IPAQ Group. IPAQ scoring protocol—International Physical Activity Questionnaire. https://sites.google.com/site/theipaq/scoring-protocol.
Ainsworth, B. E. et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports. Exerc. 32, S498–S504 (2000).
Reimer Jensen, A. M. et al. Association of left ventricular systolic function with incident heart failure in late life. JAMA Cardiol. 6, 509–520 (2021).
Nattel, S., Maguy, A., Le Bouter, S. & Yeh, Y. H. Arrhythmogenic ion-channel remodeling in the heart: Heart failure, myocardial infarction, and atrial fibrillation. Physiol. Rev. 87, 425–456 (2007).
Beale, A. L. et al. Sex differences in heart failure with preserved ejection fraction pathophysiology: A detailed invasive hemodynamic and echocardiographic analysis. JACC Heart Fail. 7, 239–249 (2019).
Acknowledgements
This study has been performed using the UK Biobank Resource under Application Number 84352. We thank the patients and investigators who contributed to the UK Biobank.
Funding
This work was supported by Major Scientific Research Program for Young and Middle-aged Health Professionals of Fujian Province, China (2023ZQNZD01020044), Natural Science Foundation of Fujian Province (2022J01706), National Natural Science Foundation of China (82304213) and the Start-up Fund for high-level talents of Fujian Medical University (XRCZX2021026) to Dr. Wuqing Huang. The funder had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Author information
Authors and Affiliations
Contributions
All authors were responsible for the study concept and design. W.H. obtained funding. J.X. did the statistical analysis. J.X. and W.H. drafted the manuscript, and all authors revised it for important intellectual content.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The North West Multi-Centre Research Ethics Committee has approved UK Biobank study (REC reference: 21/NW/0157), and written informed consent was obtained from all participants. This study have been performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xiao, J., Wu, H., Gao, Z. et al. Association of left ventricular ejection fraction with risk of cardiovascular diseases: a prospective cohort study. Sci Rep 14, 25233 (2024). https://doi.org/10.1038/s41598-024-76462-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-76462-2