Abstract
Vaccination plays a crucial role in preventing and controlling SARS-CoV-2 infections as well as their associated adverse outcomes. But there is a notable lack of research on the effectiveness of COVID-19 vaccination in children, particularly those young preterm-born children, who are more vulnerable to severe outcomes from SARS-CoV-2 infection. We aimed to determine the effect of vaccination with inactivated vaccines BBIBP-CorV and CoronaVac on symptomatic COVID-19 infection and related symptoms in preterm-born children aged 3–7 years after relaxation of the COVID-19 prevention and control measures in December 2022 in China. We performed a retrospective cohort study involving 242 preterm-born children aged 3–7 years and the data were collected in March 2023. Logistic regression models and modified Poisson regression models combined with entropy balancing were used to explore the associations of vaccination against SARS-CoV-2 with symptomatic COVID-19, specific symptoms, and persistent symptoms one month after recovery from COVID-19. Of the 242 recruited preterm-born children, 156 (64.5%) were vaccinated with inactivated vaccines BBIBP‐CorV and CoronaVac. After entropy balancing, the covariates were balanced between the vaccinated and the unvaccinated groups, with standardized mean difference < 0.001. Vaccination with the said SARS-CoV-2 vaccines lowered the risk of developing symptomatic COVID-19 in preterm-born children (risk ratio [RR] = 0.783; 95% confidence interval [CI]: (0.711, 0.861). Likewise, COVID-19 vaccination was associated with a decline in the risk of pneumonia (odds ratio [OR] = 0.318; 95% CI 0.110, 0.913), fever (RR = 0.710; 95% CI 0.635, 0.794), high fever (RR = 0.542; 95% CI 0.297, 0.988), sore throat (OR = 0.304; 95% CI 0.139, 0.664), and persistent symptoms (RR = 0.425; 95% CI 0.182, 0.993). Immunization with inactivated vaccines BBIBP‐CorV and CoronaVac provides protection against symptomatic COVID-19 for preterm-born children 3–7 years.
Similar content being viewed by others
Introduction
COVID-19 remains a troublesome global issue and a threat to human health due to its constant prevalence and variation1. Vaccination is an important measure to prevent and control SARS-CoV-2 infection and the adverse outcomes of the infection2. Timely assessment of the effectiveness of vaccination would have significant implications for vaccine development and formulation of intervention measures against COVID-19. Although many studies have reported the effectiveness of SARS-CoV-2 vaccines in adults, children aged 5–11 years and adolescents, there is relatively little research on children, especially those younger than 5 years3,4,5,6,7.
Children born before 37 weeks’ gestational age are considered preterm, and they may exhibit varying levels of immaturity in their organ development and physiological functions. In China, there are about 1.2 million premature births annually, with a premature birth rate of about 7%8. Research shows that preterm-born children are more vulnerable to SARS-CoV-2 infection and have a higher risk of contracting severe COVID-199. Currently, there is a lack of real-world evidence on the protective effect of vaccination against the first SARS-CoV-2 infection among preterm-born children.
It was found in our previous research that adverse reactions related to COVID-19 vaccine administration were rare in preterm-born children aged 3–7 years and children with bronchopulmonary dysplasia (BPD); even though they occur, they are mostly mild10,11. However, the COVID-19 vaccination rate among preterm-born children is not very high in China compared with adults10. In addition to the potential adverse reactions after vaccination, the uncertain effect of COVID-19 vaccination is another concern among parents of preterm-born children. In China, children aged ≥ 3 years have been able to get a COVID-19 vaccine since October 202112,13,14. On December 7, 2022, the Chinese government made a decision about proposing a series of optimization measures, marking the beginning of the gradual relaxation of prevention and control policies against the COVID-19 pandemic15. Starting from January 8, 2023, China has fully lifted its control over COVID-19. In China, the age ranging from 3 to 7 years corresponds to the kindergarten stage, after which children enter primary school. In this study, we conducted a survey within three months after comprehensive lifting of the COVID-19 prevention and control policies in China, ensuring that the COVID-19 infection that all the premature children aged 3–7 years contracted was their first experience. The purpose of the study was to examine the effect of vaccination with inactivated vaccines BBIBP-CorV and CoronaVac on the first symptomatic COVID-19 infection, specific symptoms and persistent symptoms of COVID-19 in preterm-born children aged 3–7 years in China.
Materials and methods
Study population
A retrospective cohort study was conducted. This survey was conducted in March 2023 among preterm-born children aged 0–7 years who contracted the first episode of COVID-19 infection three months after comprehensive lifting of the COVID-19 defense measures in China.
After multiple discussions and revisions by senior neonatologists of the said hospital, a standardized questionnaire form was designed. Then it underwent repeated testing by neonatologists and parents of preterm infants before it was finally utilized to keep the consistency and reliability. The questionnaire was developed by the online survey platform “Wenjuanxing” and distributed in WeChat groups of neonatology directors in China. Subsequently, the questionnaire was forwarded to parents of preterm-born children aged 0–7 years.
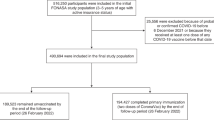
Inclusion criteria were (1) children aged 3–7 years; (2) children with a gestational age of less than 37 weeks. Children with incomplete information and the ones who were vaccinated with recombinant vaccines were excluded. A total of 242 preterm-born children were included in this study (Fig. 1; details on how to calculate the minimum sample size was provided in Supplementary File S1 and the results of minimum sample size required in different scenarios can be found in Supplementary Table S1).
This study was approved by the Ethics Committee of the Seventh Medical Center of the PLA General Hospital. All research was performed in accordance with relevant guidelines/regulations. Informed consent was obtained from all subjects involved in the study. All procedures were performed in accordance with the Helsinki Declaration.
Data collection
Patient data were collected, including demographic characteristics, gestational age ([24.9, 28) weeks, [28, 32) weeks, and [32, 37) weeks), underlying health conditions, COVID-19 vaccination status, and whether having COVID-19-related outcomes (for the vaccinated children, we documented whether they had COVID-19-related outcomes 14 days after vaccination against SARS-CoV-2). Demographic characteristics included age, sex, ethnicity, the living environment (urban or rural), educational background, and place of residence (i.e., eastern, central or western China) (Supplementary Table S2). Underlying health conditions included atrial septal defect (ASD), ventricular septal defect (VSD), BPD, asthma, hypersensitive disease, hereditary disease, metabolic disease, and immune deficiency. Diagnosis of COVID-19 was made through antigen testing, nucleic acid testing, and confirmation of infection in cohabiting individuals during the same period.
COVID-19-related outcomes included symptomatic COVID-19, pneumonia, some COVID-19-related symptoms (including fever, high fever [i.e., the highest body temperature during the course of COVID-19 of ≥ 39 °C], poor mental response, fatigue, muscle pain, sore throat, hyposmia, hypogeusia, cough, stuffy nose, and runny nose), persistent symptoms one month after recovery from COVID-19 (including easy fatigue, dizziness, headache, muscle aches, joint pains, dry throat, sore throat, hoarseness, chest tightness, breathlessness, cough, nasal congestion, runny nose, reduced sense of smell, reduced sense of taste, sleep disorders, and mood swings), myocardial damage, multisystem inflammatory syndrome in children (MIS-C), hospitalization, and the requirement of respiratory support.
Statistical analysis
Preterm-born children were divided into two groups: the vaccinated and the unvaccinated children according to their COVID-19 vaccination status. Continuous variables were summarized using means and standard deviations. Categorical variables were expressed as counts and proportions. In the main analysis, we considered age, sex, ethnicity, whether living in an urban area, educational background, place of residence, and underlying health conditions as covariates.
Entropy balancing (EB) was employed to balance the covariates of the vaccinated and the unvaccinated children, aiming to infer the effect of vaccination against SARS-CoV-2 on symptomatic COVID-19 and related symptoms appropriately16. Standardized mean difference (SMD) was calculated to evaluate the level of covariate balance between the vaccinated and the unvaccinated children. SMD < 0.1 indicated a proper balance17. Weights were derived based on the covariates through EB.
The primary outcome of interest was symptomatic COVID-19. The effect of vaccination with SARS-CoV-2 on symptomatic COVID-19 was explored by constructing a modified Poisson regression model combined with EB using the weight derived from EB to each observation18,19. In addition, other COVID-19-related outcomes with at least ten cases were used as the secondary outcomes. The effect of COVID-19 vaccination on these outcomes was explored by using a modified Poisson regression model or logistic regression combined with EB when appropriate. The logistic regression model is a commonly used approach for the assessment of the influential factors of a binary outcome which is rare (typically < 10%). For the rare outcome, the odds ratio (OR) estimated from the logistic regression model approaches the risk ratio (RR). However, for the outcome that is not rare, the value of OR can be different from that of RR. In this case, the modified Poisson regression model is a better alternative to estimate RR18,19. Therefore, the RR and the OR of the outcomes comparing the vaccinated with the unvaccinated children were estimated by using the modified Poison regression model and binary logistic regression model, respectively in this study. />
To test the robustness of the results, we conducted a sensitivity analysis by excluding the covariate of children’s educational background. All analyses were performed using R (version 4.3.1). Two-sided P < 0.05 was considered statistically significant.
Results
Of the 242 preterm-born children, 156 (64.5%) received inactivated vaccines BBIBP-CorV and CoronaVac. Preterm-born children who received COVID-19 vaccine were on average older than the unvaccinated children (5.65 vs. 4.13 years) (Table 1). Most vaccinated children (98.1%) were kindergarteners or primary school students versus 77.9% in the unvaccinated children. The proportion of children with a gestational age of less than 28 weeks among the vaccinated was lower than that among the unvaccinated (7.1% vs. 17.4%). Regarding the regional difference, these respondents all from different hospitals and geographical area and 62.8% of the vaccinated children lived in central areas of China versus 48.8% for the unvaccinated children. The fraction of children residing in eastern China in the vaccinated group was lower than that in the unvaccinated group (25.6% vs. 43.0%). In vaccinated children, there were two cases of ASD (1.3%), while unvaccinated children had five cases (5.8%). More children were diagnosed with BPD in the vaccinated group than in the unvaccinated group (35.3% vs. 26.7%). Asthma, hereditary disease, and metabolic disease were not reported among the participants at the time of survey. There was only one case of immune deficiency among the vaccinated children (0.6%), while two were reported among the unvaccinated (2.3%). Figure 2 shows the standardized mean differences of the covariates before and after implementing entropy balancing. It was observed that the covariates were balanced between the children with and without COVID-19 vaccination after entropy balancing (SMD < 0.001).
Absolute values of the standardized mean differences (SMDs) before and after the adjustment of covariates with entropy balancing (EB). SMD measures the difference in the means (scaled by standard deviation) between the vaccinated and the unvaccinated groups. Blue and red dots indicate the SMDs of the covariates before and after the EB, respectively. The value of SMD less than 0.1 (shown as the dashed line) indicates that a covariate is well balanced between the vaccinated and the unvaccinated children. ASD atrial septal defect, BPD bronchopulmonary dysplasia, VSD ventricular septal defect.
Among the 242 included children, 182 (75.2%) displayed clinical manifestations and 13 (5.4%) had pneumonia (Table 2). Nearly 70% of the children had fever, more than 30% had high fever, 8.3% experienced sore throat, and 16.5% had persistent symptoms one month after recovering from COVID-19 infection. Myocardial damage, MIS-C, hospitalization, and requirement of respiratory support rarely occurred among the children.
Table 3 shows the results of logistic regression models and modified Poisson regression models which were applied to evaluate the association of vaccination against SARS-CoV-2 with COVID-19-related outcomes. It was found that receiving inactivated vaccines reduced the risk of symptomatic COVID-19 among preterm-born children (RR = 0.783; 95% CI 0.711, 0.861). Likewise, COVID-19 vaccination was associated with a decline in the risk of pneumonia (OR = 0.318; 95% CI 0.110, 0.913), fever (RR = 0.710; 95% CI 0.635, 0.794), high fever (RR = 0.542; 95% CI 0.297, 0.988), sore throat (OR = 0.304; 95% CI 0.139, 0.664), and persistent symptoms (RR = 0.425; 95% CI 0.182, 0.993).
In the sensitivity analyses, the relationship between vaccination and asymptomatic COVID-19 was also statistically significant (Supplementary Table S3) when adjusting the absolute value of the SMDs before and after the adjustment of covariates with EB (Supplementary Fig. S1).
Discussion
To our best knowledge, this is the first study to evaluate the effect of vaccination with inactivated vaccines BBIBP-CorV and CoronaVac on symptomatic COVID-19 and related symptoms among preterm-born children aged 3–7 years in China in a real-world setting. The differences between the vaccinated and unvaccinated groups are similar with the findings in our previous study about preterm-born children10,11, showing that these differences are mainly related to the age20, region21, and health status22, leading to a low vaccination rate in these children as compared with normal children23,24. However, the majority of the factors are not contraindications25. Therefore, in the future, we can start from more detailed aspects to improve the vaccination rate.
In our study, we found that the risk of symptomatic COVID-19 was lower among the vaccinated compared to the unvaccinated. According to the studies published in the PubMed database on the COVID-19 pandemic in Asian populations up to November 2022, only a few studies (5.1%) have considered the impact of vaccination among children26. Research has found that COVID-19 vaccines can optimize protective immunity in the upper respiratory tract, reducing infections, viral transmission, and severe disease by inhibiting the progression to the lower respiratory tract27. These vaccines provide good protection against severe disease for children28 and adults29, and also protect children from MIS-C30,31 and long COVID syndrome32,33. Meanwhile, inactivated COVID-19 vaccines have been proven effective and safe in reducing disease severity, hospitalization, MIS-C, and death among infants and children over six months old34,35. Nonetheless, due to the emergence of variants, the real-world effectiveness of these vaccines in preventing infection is often lower than the efficacy observed in clinical trials. Different from previous studies which mainly focused on the efficacy of the vaccine against severe disease36, our study, however, focused on the protection of preterm-born children in the real world after receiving the COVID-19 vaccine. We found that COVID-19 vaccination had a protective effect on preterm-born children against symptomatic COVID-19. It is encouraged for preterm-born children to receive the COVID-19 vaccine.
Previous studies have found that preterm-born children under the age of 2 are more susceptible to COVID-19 and are more likely to develop severe illness after infection. Considering that susceptibility to COVID-19 is usually associated with high levels of oxidative stress, an imbalance in redox balance may lead to increased susceptibility to the virus. Due to changes in oxidative stress status related to prematurity, the clinical condition of preterm-born children infected with COVID-19 may worsen. Although the above situation may have a smaller impact on preterm-born children aged 2–17 years, the specific extent of the impact is unknown37,38. COVID-19 vaccines primarily reduce the risk of infection by activating the immune system, producing antibodies, and forming memory cells39. Previous studies have found that regardless of the type of vaccine used, preterm-born children developed adequate antibody responses to all vaccine antigens after initial and booster vaccinations40,41. The immunogenicity and safety observed in preterm-born children after vaccination are generally not inferior to those in full-term infants in some special vaccination42. However, these studies mainly focus on the early reactivity of preterm-born children to the vaccine and lack relevant research on the response of preterm-born children aged 3–7 years after vaccination. Therefore, our study provides evidence for the current situation of COVID-19 infection and the protective effects of the vaccine in preterm-born children aged 3–7 years.
Vaccination against COVID-19 can alleviate symptoms such as fever, high fever, and sore throat. Previous studies have found that vaccines provide protection for both children and adults39,43,44. showing that even if vaccinated individuals contract COVID-19, their viral load is lower. This means there is less virus in the body, which may help reduce the severity and duration of symptoms. Previous studies have found that vaccinated children have a lower incidence of fever45. Fever is the most common symptom in children. However, In the real world, the protective effects of COVID-19 vaccines on children are mostly evaluated based on whether they contract COVID-19 and COVID-19-related hospital admissions, with mainly focus on adolescents and less on specific symptoms46,47. Therefore, our research is particularly valuable. Families with preterm-born children are usually more anxious48, and when children show symptoms, this anxiety increases. The more symptoms the child has, the more anxious the family becomes49,50, and the child may become irritable, cry more, or exhibit poor spirits. This creates a vicious cycle, leading families to frequent hospital visits, which may result in cross-infection and increased economic burden. Vaccination reduces symptoms, possibly alleviating family anxiety, reducing the child’s discomfort, and decreasing the number of hospital visits and associated costs and time. Thus, vaccination can prevent this vicious cycle from occurring to some extent.
In addition, we have also found that vaccination can reduce the risk of pneumonia and persistent symptoms in preterm-born children. The study on the reduction of pneumonia through vaccination has already been confirmed in normal children51, and our research fills the gap in preterm-born children. Persistent symptoms have been less studied in children; previous findings have suggested that vaccination may reduce the syndrome of long COVID32,52, and our research has similarly confirmed this in preterm-born children.
This study has some limitations. First, it only focused on COVID-19 infections in preterm-born children aged 3–7 years. Further efforts are warranted to reveal the effect of COVID-19 vaccination for other age groups. Second, the sample size of this study is relatively small, which may be insufficient for the inference for the effect of vaccination on some outcomes. Third, the representativeness of the sample could be improved if the subjects were selected from more diverse sources. Finally, we missed some important data such as the dosage and administration of the COVID-19 vaccine. This may underestimate the effect of full vaccination.
In conclusion, vaccination with inactivated vaccines BBIBP-CorV and CoronaVac reduces the risk of symptomatic COVID-19 in preterm-born children aged 3–7 years. Therefore, we advise that preterm infants aged 3 to 7 years receive the inactivated vaccines in order to alleviate symptoms following COVID-19 infection.
Data availability
The dataset analyzed during the current study is available from the corresponding authors on reasonable request.
References
Biancolella, M. et al. COVID-19 annual update: a narrative review [J]. Hum. Genomics. 17 (1), 68 (2023).
Sharma, K. & Li-Kim-Moy J. COVID-19 vaccines in 2023 [J]. Aust Prescr. 46 (3), 60–63 (2023).
Gao, P. et al. Effectiveness and safety of SARS-CoV-2 vaccines among children and adolescents: a systematic review and Meta-analysis [J]. Vaccines (Basel), 10(3) (2022).
Pinto Pereira, S. M. et al. Post-COVID-19 condition at 6 months and COVID-19 vaccination in non-hospitalised children and young people [J]. Arch. Dis. Child. 108 (4), 289–295 (2023).
Feldstein, L. R. et al. Effectiveness of Bivalent mRNA COVID-19 vaccines in preventing SARS-CoV-2 infection in children and adolescents aged 5 to 17 years [J]. Jama. 331 (5), 408–416 (2024).
Piechotta, V. et al. Safety and effectiveness of vaccines against COVID-19 in children aged 5–11 years: a systematic review and meta-analysis[J].The Lancet. Child. Adolesc. Health. 7 (6), 379–391 (2024).
Lan, Z. et al. Effectiveness of COVID-19 vaccines among children and adolescents against SARS-CoV-2 variants: a meta-analysis. Eur. J. Pediatr. 182 (12), 5235–5244 (2023).
Hangzhou Center for Disease Control and Prevention SCfDCaP. One of expert consensus on immunization in children with special state-prematurity and vaccination [J]. Chin. J. Appl. Clin. Pediatr. 33 (10), 737–738 (2018).
Choi, J. H., Choi, S. H. & Yun, K. W. Risk factors for severe COVID-19 in children: a systematic review and Meta-analysis [J]. J. Korean Med. Sci. 37 (5), e35 (2022).
Wang, D. et al. Receipt of COVID-19 vaccine in preterm-born children aged 3–7 in China [J]. Front. Public. Health. 11, 1191941 (2023).
Wang, D. et al. Acceptability of COVID-19 vaccination in Chinese children aged 3–7 years with bronchopulmonary dysplasia [J]. Pediatr. Pulmonol. 58 (5), 1417–1426 (2023).
Han, B. et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine (CoronaVac) in healthy children and adolescents: a double-blind, randomised, controlled, phase 1/2 clinical trial [J]. Lancet Infect. Dis. 21 (12), 1645–1653 (2021).
Innovation NCfST. China’s inactivated COVID-19 vaccine has been officially approved for use in people aged 3–17 years. Preprint at (2021). http://www.ncsti.gov.cn/kjdt/ztbd/zyq/zxxx/202107/t20210718_36885.html.
CK, G. Chinese government: striving to complete the full vaccination of non-contraindication population aged 3 to 11 years by the end of December. Preprint at https://baijiahao.baidu.com/s?id=1715043532185356789&wfr=spider&for=pc (2021).
website, H. C. Notice on Further Optimizing and Implementing COVID-19 Prevention and Control Measures. https://www.gov.cn/xinwen/2022-12/07/content_5730443.htm (2022).
J H. Entropy balancing for causal effects: a multivariate reweighing method to produce balanced samples in observational studies [J]. Political Anal. 20(1), 25–46 (2012).
Austin, P. C. S. E. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies [J]. Stat. Med. 34 (28), 3661–3679 (2015).
Chen, W. et al. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification [J]. BMC Med. Res. Methodol. 18 (1), 63 (2018).
Zou, G. A modified poisson regression approach to prospective studies with binary data [J]. Am. J. Epidemiol. 159 (7), 702–706 (2004).
ifeng.com. 95% of people aged 3–17 have been fully vaccinated against COVID-19 in China. Preprint at (2022). https://finance.ifeng.com/c/8H22My8CI2S.
Tian, C. et al. Influenza vaccination coverage among US children from 2004/2005 to 2015/2016 [J]. J. Public. Health (Oxf). 41 (1), e62–e69 (2019).
Soans, S. et al. Vaccination in preterm and low birth weight infants in India [J]. Hum. Vaccin Immunother. 18 (1), 1–12 (2022).
China, N. H. C. P. R. Transcript of the press conference of the Joint Prevention and Control Mechanism of the State Council on January 15, Preprint at (2022). http://www.nhc.gov.cn/xcs/yqfkdt/202201/956b9a4d566546d7966d5cf93641bd2a.shtml (2022).
Province TPsGoH. The cumulative coverage rate of the first dose of COVID-19 vaccine among people aged 3 to 11 years in our province has reached 97.76%. Preprint at (2022). https://www.hainan.gov.cn/hainan/yqfkzzzzxxx/202202/7394493b54aa4800826fc8e459a0633c.shtml.
Zheng, Y. J. et al. Expert’s consensus on severe acute respiratory syndrome coronavirus-2 vaccination of children [J]. Chin. J. Appl. Clin. Pediatr. 36 (18), 1361–1367 (2021).
Thakkar, K. et al. Impact of vaccination and non-pharmacological interventions on COVID-19: a review of simulation modeling studies in Asia [J]. Front. Public. Health. 11, 1252719 (2023).
Ramasamy, R. COVID-19 vaccines for optimizing immunity in the Upper respiratory tract [J]. Viruses. 15(11) (2023).
Frenck, R. W. et al. Safety, Immunogenicity, and efficacy of the BNT162b2 Covid-19 vaccine in adolescents [J]. N Engl. J. Med. 385 (3), 239–250 (2021).
Skowronski, D. M. & De Serres, G. Safety and Efficacy of the BNT162b2 mRNA Covid-19 vaccine [J]. N Engl. J. Med. 384 (16), 1576–1577 (2021).
Levy, M. et al. Multisystem inflammatory syndrome in children by COVID-19 vaccination status of adolescents in France [J]. Jama. 327 (3), 281–283 (2022).
Liu, T. H. et al. Effectiveness of COVID-19 vaccination against multisystem inflammatory syndrome in children: a systematic review and meta-analysis [J]. J. Microbiol. Immunol. Infect.56 (6), 1299–1300 (2023).
Boufidou, F. et al. SARS-CoV-2 reinfections and Long COVID in the Post-omicron phase of the pandemic [J]. Int. J. Mol. Sci. 24(16). (2023).
Català, M. et al. The effectiveness of COVID-19 vaccines to prevent long COVID symptoms: staggered cohort study of data from the UK, Spain, and Estonia [J]. Lancet Respir Med. 12 (3), 225–236 (2024).
Jantarabenjakul, W. et al. Global COVID-19 vaccination in infants and children: effectiveness, Safety, and challenges [J]. Asian Pac. J. Allergy Immunol. 41 (4), 292–303 (2023).
Powell, A. A. et al. Current state of COVID-19 in children: 4 years on [J]. J. Infect. 88 (5), 106134 (2024).
Mastrolia, M. V. et al. Clinical syndromes related to SARS-CoV-2 infection and vaccination in Pediatric Age: a narrative review [J]. Med. (Kaunas), 59(11) (2023).
Kompaniyets, L. et al. Underlying Medical conditions Associated with severe COVID-19 illness among children [J]. JAMA Netw. Open. 4 (6), e2111182 (2021).
Shi, T. et al. Risk of COVID-19 hospital admission among children aged 5–17 years with asthma in Scotland: a national incident cohort study [J]. Lancet Respir Med. 10 (2), 191–198 (2022).
Akahata, W. et al. Safety and immunogenicity of SARS-CoV-2 self-amplifying RNA vaccine expressing an anchored RBD: a randomized, observer-blind phase 1 study [J]. Cell. Rep. Med. 4 (8), 101134 (2023).
Chiappini, E. et al. Hexavalent vaccines in preterm infants: an update by Italian Society of Pediatric Allergy and Immunology jointly with the Italian society of neonatology [J]. Ital. J. Pediatr. 45 (1), 145 (2019).
Omeñaca, F. et al. Combined Haemophilus Influenzae type B-Neisseria meningitidis serogroup C vaccine is immunogenic and well tolerated in preterm infants when coadministered with other routinely recommended vaccines [J]. Pediatr. Infect. Dis. J. 30 (11), e216–e224 (2011).
Knuf, M. et al. Penta- and hexavalent vaccination of extremely and very-to-moderate preterm infants born at less than 34 weeks and/or under 1500 g: a systematic literature review [J]. Hum. Vaccin Immunother. 19 (1), 2191575 (2023).
Katoto, P. D. et al. Effectiveness of COVID-19 Pfizer-BioNTech (BNT162b2) mRNA vaccination in adolescents aged 12–17 years: a systematic review and meta-analysis [J]. Hum. Vaccin Immunother. 19 (1), 2214495 (2023).
Hamad, S. M. et al. The protective effect of COVID-19 vaccines on developing multisystem inflammatory syndrome in children (MIS-C): a systematic literature review and meta-analysis [J]. Pediatr. Rheumatol. Online J. 21 (1), 80 (2023).
Wei, F. et al. Clinical characteristics of severe acute respiratory syndrome coronavirus 2 vaccine breakthrough infections in children [J]. Chin. J. Infect. Dis. 41 (01), 58–63 (2023).
Lan, Z. et al. Effectiveness of COVID-19 vaccines among children and adolescents against SARS-CoV-2 variants: a meta-analysis [J]. Eur. J. Pediatr. 182 (12), 5235–5244 (2023).
Tartof, S. Y. et al. Effectiveness of mRNA BNT162b2 COVID-19 vaccine up to 6 months in a large integrated health system in the USA: a retrospective cohort study [J]. Lancet. 398(10309), 1407–1416 (2021).
Sandnes, R. et al. Parental stress and mental health outcomes following very preterm birth: a systematic review of recent findings [J]. J. Affect. Disord. 355, 513–525 (2024).
Staver, M. A., Moore, T. A. & Hanna, K. M. An integrative review of maternal distress during neonatal intensive care hospitalization [J]. Arch. Womens Ment Health. 24 (2), 217–229 (2021).
Guittard, C. et al. Effect of tactile and/or kinesthetic stimulation therapy of preterm infants on their parents’ anxiety and depressive symptoms: a systematic review [J]. BMC Psychol. 12 (1), 3 (2024).
Brodin, P. Immune responses to SARS-CoV-2 infection and vaccination in children [J]. Semin Immunol. 69, 101794 (2023).
Esposito, S. et al. True prevalence of long COVID in children: a narrative review [J]. Front. Microbiol. 14, 1225952 (2023).
Acknowledgements
We thank all directors of the neonatology departments who helped implement this survey, and the parents who helped complete the questionnaires.
Funding
This study was supported by the National Key R&D Program of China (2021YFC2701702 to Q.L.), Guangdong Basic and Applied Basic Research Foundation (2024A1515011957 to L.L.), Scientific Research Project of Hunan Provincial Health Commission (20232084 to D.W.) and Hunan Province Natural Science Foundation Youth Project (2022JJ40202 to D.W.). The study sponsor had no role in study design, collection, analysis and interpretation of data, the writing of the report, and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Dan Wang conceptualized and designed the study, collected data, interpreted the data, and drafted the manuscript. Li Li and Jia-Dong Ning analyzed and interpreted the data, and drafted the manuscript. Qiuping Li, Li Li, and Tao Han critically conceptualized, designed the study, revised the manuscript for important intellectual content. Changgen Liu, Shanghong Tang, Jingke Cao, and Zhichun Feng collected data, revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional Review Board Statement
This study was approved by the research ethics board of the Seventh Medical Center of PLA General Hospital (Beijing, China).
Informed consent
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, D., Ning, JD., Cao, J. et al. The effect of COVID-19 vaccination on symptomatic infection and related symptoms among preterm-born children aged 3–7 years in China. Sci Rep 14, 25384 (2024). https://doi.org/10.1038/s41598-024-76609-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-76609-1