Abstract
Fall is common in the elderly, and chronic kidney disease is considered a major risk factor. Serum creatinine (Cre) and cystatin C (Cys C) are commonly used biomarkers for renal function, while the ratio of Cre to Cys C, known as the sarcopenia index (SI), provides insights into muscle health. This study investigates the relationships between Cre, Cys C, estimated glomerular filtration rates (eGFR), SI, and self-reported falls using National Health and Nutrition Examination Survey (NHANES) data. We included 4,272 older adults with eGFR > 30mL/min/1.73m2 from NHANES (1999 to 2004) and divided them into the fall and non-fall groups based on the questionnaires. Correlations were assessed using restricted cubic spline, weighted generalized linear regression models. Multi-factor logistic regression analysis identified serum Cys C as significantly associated with falls (all participants: OR 1.16, 95% CI: 1.09 to 1.23, p < 0.001; participants with eGFR > 75 mL/min/1.73m2: OR 1.17, 95% CI: 1.05 to 1.30, p < 0.001,). In contrast, Cre and eGFR were not significant after adjustments; SI showed marginal significance (p = 0.045). Cys C is significantly associated with fall risk in older adults, demonstrating a positive linear relationship with self-reported falls.
Similar content being viewed by others
Introduction
Falls pose a global public health challenge, emerging as a leading cause of death in developed countries1. Approximately one in three community-dwelling people aged over 65 years fall each year2, and the incidence of fall-related injuries escalates with advancing age3. For elderly people, falls can be devastating and fatal. Consequences of falls include fractures and head injuries4, resulting in fear of falling5, reduction in physical function6, social interactions, and deep venous thrombosis or pneumonia.
Chronic kidney disease is associated with an elevated risk of frailty, which further increases the likelihood of falls7. Cre and Cys C are markers routinely used to estimate glomerular filtration rate (eGFR)8. While serum Cre is primarily derived from muscle metabolism, leading to lower levels in individuals with reduced muscle mass, Cys C is produced at a constant rate by all nucleated cells and is less influenced by muscle mass9,10. Consequently, the ratio of Cre to Cys C has been identified as the sarcopenia index (SI), which provides a more nuanced evaluation of muscle health and has shown potential for screening sarcopenia in multiple populations11,12,13.
Previous studies have indicated a linear relationship between SI and self-reported falls in community-dwelling Caucasian women14. However, few studies have reported that creatinine and Cys C, when examined individually, may serve as risk factors for self-reported falls15,16,17. These studies predominantly focused on correlational analyses without investigating the nonlinear relationships that may exist between these biomarkers and fall risk. In another cohort study, researchers found that lower eGFR based on Cys C was associated with a higher risk of frailty, while eGFR based on Cre showed no such correlation18. Additionally, elevated levels of Cys C were linked to declines in physical function, including more rapid decreases in walking speed and grip strength19,20.
We propose that investigating the SI alongside serum Cys C and Cre will provide new insights into their differential associations with falls. Specifically, we hypothesized that serum Cys C levels are associated with an L-shaped relationship to falls, suggesting that higher levels correlate with an increased likelihood of falls. In contrast, both eGFR and serum Cre may exhibit J-shaped relationships with falls, albeit in opposing directions21. Furthermore, we postulate that the SI may demonstrate a skewed Z-shaped relationship with fall. Higher eGFR values or lower serum Cre levels, particularly when Cre is low relative to cystatin C, may indicate reduced muscle mass, which is anticipated to correspond with an increased risk of falls9,21,22. Therefore, we aim to explore the association between Cre and Cys C levels, as well as SI, with falls in the general elderly population of the United States (U.S.).
Materials and methods
Study population
The NHANES is a comprehensive epidemiological program that has systematically evaluated the health and dietary patterns of the U.S. population since the early 1960s. Utilizing a stratified, multistage probability design, NHANES recruits a nationally representative cohort. Each year, approximately 5,000 individuals are selected from various counties nationwide, with data collection occurring in two-year cycles since 199923. The NHANES data from 1999 to 2004 were included in this study. The total sample in NHANES consisted of 31,126 participants. Of these participants, we excluded individuals based on the following criteria: (1) those under 60 years old (n = 25,519), (2) those missing self-reported prevalence of falls data (n = 19), (3) those missing serum creatinine information (n = 1,040), (4) those missing serum Cystatin C information (n = 190), and (5) those with an eGFR < 30 mL/min/1.73 m2n = 86). Finally, a total of 4,272 participants (2,135 men and 2,137 women) were included in this analysis (Supplementary Fig. 1).
Exposure variables
In the NHANES database, biochemistry indicators were analyzed using a Hitachi Model 704 multichannel analyzer (Boehringer Mannheim Diagnostics, Indianapolis, IN). Serum creatinine was measured using the Jaffe kinetic alkaline picrate method. Specimens of serum creatinine from NHANES were evaluated to determine whether adjustments were necessary when compared to a method traceable to a gold standard reference. According to NHANES guidelines, correction for serum creatinine in the 1999–2000 dataset is highly recommended; therefore, we employed regression analysis to convert NHANES 1999–2000 serum creatinine values to standardized creatinine. For the 2001–2002 and 2003–2004 datasets, no correction was deemed necessary. Cystatin C was measured in serum using a Cystatin C immunoassay (Siemens Healthcare Diagnostics) on an automated multi-channel analyzer, Siemens Dimension Vista 1500 (Siemens Healthcare Diagnostics). eGFR was calculated using the CKD-EPI Creatinine Eq. (2021)24. SI was defined as the ratio of serum creatinine (mg/mL) to cystatin C (mg/L): SI = (creatinine/ cystatin C) × 100. Detailed measurements can be found at: https://wwwn.cdc.gov/Nchs/Nhanes/1999-2000/LAB18.htm.
Identifying fall and non-fall groups
To categorize participants into fall and non-fall groups, individuals who responded “yes” to the question “Have you had difficulty with falling in the past 12 months?” were classified into the fall group. For the non-fall group, participants who answered “no” to the initial question about difficulty with falling were included. Additionally, individuals who, when asked, " During the past 12 months, have you had dizziness, difficulty with balance, or difficulty with falling? " answered “no” were also considered part of the non-fall group.
Covariates
Demographic characteristics such as age, gender, and ethnicity were confounding factors between exposure and the primary outcome. The socioeconomic covariates comprise education level, smoking status, alcohol consumption status, and mean energy intake. Similarly, medical comorbidity variables were also acquired, including body mass index (BMI) and comorbidities such as hypertension, diabetes, and cancer. We provide an overview of the diagnostic methods utilized, as informed by NHANES, in Supplementary Table 2. A comprehensive explanation of the variables utilized in this study is available at https://www.cdc.gov/nchs/nhanes/.
Statistical analysis
All analyses were conducted using R.4.3.1 (http://www.R-project.org). For most covariates, less than 5.0% of the data were missing. However, there was a lack of data in 4.6% of the study participants for body mass index (BMI), 4.3% for drinking status, and 3.8% for total calorie intake. The missing data were multiply imputed for the covariates by the “jomo” package, which implements a multilevel approach designed for survey data25. A Gibbs sampling procedure was used to generate 3 imputed data sets after a burn-in of 1000 iterations and 1000 updates to ensure stochastic independence between imputed data26. When calculating all estimates, we took into account the NHANES sample weights. Results for continuous variables were reported as mean (Interquartile Range, IQR), and categorical variables were expressed as numbers and numbers (%). The significance of differences was determined via weighted wilcoxon rank-sum test for the continuous variables and weighted chi-square tests for the categorical variables. Weighted generalized linear regression models were used to examine the relationship between exposure variables and the risk of fall. Model 1 was adjusted for age, gender, BMI, and race. Model 2 adjusted for Model 1 variables and educational level, smoking, alcohol drinking, and calorie intake. Finally, model 3 was adjusted to model 2 variables, supplemented by stroke, diabetes, arthritis, chronic bronchitis, congestive heart failure, heart attack, liver condition, and hypertension as the final model. Receiver operating characteristic (ROC) curves with area under curves (AUC) metrics were utilized to assess the ability of exposure variables to screen for fall. A bootstrap resampling method with 2000 iterations was employed to compute 95% confidence intervals for the AUCs using the ci.auc() function from the pROC package in R27. Additionally, we used the roc.test() function from the same package to compare the AUCs of any two metrics. In the restricted cubic spline (RCS) analysis, a restricted cubic spline transformation with four knots was utilized. Generally, using five or fewer knots was often sufficient and specifying knot locations could potentially lead to loss of information28. Consequently, the specific locations of these knots were not explicitly defined or specified in the analysis. A two-tailed p < 0.05 was considered statistically significant.
Ethics statement
The NHANES protocols adhere to the Declaration of Helsinki and have been approved by the NCHS Research Ethics Review Board (Protocol #98 − 12), with all participants providing written informed consent29. We confirm that all methods were performed according to the relevant guidelines and regulations and followed the Strengthening the Reporting of Observational Studies for Epidemiology (STROBE) guidelines for cross-sectional studies30.
Results
Baseline characteristics
Weighted socio-demographic and medical characteristics are described in Table 1. Data of 4,272 participants were extracted from the NHANES database, 376 (8.8%) had falling problems in the past years and 3,896 (91.2%) reported no falls. Fallers exhibited a higher mean age when compared to non-fallers (p < 0.001) and were more frequently female (63.43% vs. 55.94%, p = 0.031). Participants in the fallers group exhibited elevated levels of Cys C (p < 0.001) and reduced levels of eGFR (p < 0.001) compared to those in the non-fallers group. In terms of social factors, the fallers group body had a lower proportion of people with a high school education than the non-fallers group (61.81% vs. 70.88%, p < 0.001). Compared with the non-fallers group, the fallers group exhibited a significantly higher prevalence of comorbidities. The fallers group had a higher prevalence of conditions such as diabetes mellitus (28.27% vs. 19.78%), hypertension (75.83% vs. 68.02%), stroke (23.74% vs. 5.33%), arthritis (69.58% vs. 48.52%), among others. All comparisons showed a statistically significant difference with p < 0.05. Following the exclusion of all missing data, subsequent analysis revealed that the estimated effects of directly deleting missing values and using multiple interpolation methods were comparable.
Associations of Cys C, Cre, eGFR, and SI with fall
The Table 2 displays the odds ratios (ORs) of Cys C, Cre, eGFR, and SI for the presence of falls. After adjusting for covariates, Cys C (OR 1.16, 95% CI: 1.09 to 1.23, p < 0.001) and Cre (OR 1.07, 95% CI: 1.01 to 1.13, p = 0.024) demonstrated significant associations with falls. Interestingly, eGFR (OR 1.00, 95% CI: 1.00 to 1.00, p = 0.015) and SI (OR 1.00, 95% CI: 1.00 to 1.00, p = 0.048) also showed statistically significant associations with falls, despite their confidence intervals including 1.00. These findings suggest that eGFR and SI are associated with the reports of falls, although with varying effect sizes.
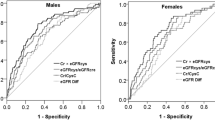
The Fig. 1 illustrates the relationship between Cys C, Cre, eGFR, and SI with falls using a RCS model analysis. After adjustment for various covariates, including age, gender, race, educational level, BMI, smoking quantity, alcohol consumption, calorie intake, stroke, diabetes, arthritis, chronic bronchitis, congestive heart failure, heart attack, liver condition, and hypertension, we found the Cys C were positively associated with falls risk (p < 0.001), and the nonlinear tests were not significant. Meanwhile, the RCS plot showed that the ORs gradually decreased with the increase in SI (Fig. 1).
RCS curve for the association between Cys C, Cre, eGFR, or SI with the risk of fall. (a) the association between Cys C and fall; (b) the association between Cre and fall; (c) the association between eGFR and fall; (d) the association between SI and fall. Adjustment factors included age, gender, race, educational level, BMI, smoking quantity, alcohol consumption, calorie intake, stroke, diabetes, arthritis, chronic bronchitis, congestive heart failure, heart attack, liver condition, and hypertension. Abbreviations: RCS, restricted cubic spline; Cys C, cystatin C; Cre, creatinine; eGFR: estimated glomerular filtration rates; SI: sarcopenia index; BMI: body mass index.
Subgroup analyse
Subanalyses of participants eGFR ≥ 75mL/min/1.73m2 were also performed. Cys C (OR 1.17, 95% CI: 1.05, 1.30, p = 0.006) continued to demonstrate a robust association with falls, whereas Cre (0.96, 95% CI: 0.86, 1.08, p = 0.5) was not, after adjusting for covariates (Table 2).
Comparison of Cys C and Cre, eGFR, and SI
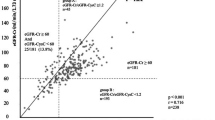
Further analyses were conducted to compare the predictive value of Cys C and other indicators. In the analysis of all participants, the AUC of Cys C (0.67,95%CI:0.64 to 0.70), indicating a moderate predictive ability for falls. In comparison, the AUC for Cre was 0.56 (95% CI: 0.52 to 0.59), the AUC for the SI was 0.62 (95% CI: 0.59 to 0.65), and the AUC for eGFR was 0.60 (95% CI: 0.57 to 0.63). Statistical comparisons revealed significant differences in predictive ability. The AUC for Cys C was significantly higher than that for Cre (p < 0.001), eGFR (p < 0.001), and SI (p = 0.005). In the subanalyses (participants with eGFR ≥ 75mL/min/1.73m2), Cys C (AUC: 0.64, 95% CI: 0.59 to 0.68) demonstrated a significantly better predictive ability for falls compared to Cre (AUC: 0.54, 95% CI: 0.49 to 0.58, p = 0.006) and eGFR (AUC: 0.53, 95% CI: 0.48 to 0.57, p < 0.001). However, the difference in AUC between Cystatin C and SI was not statistically significant (AUC for SI: 0.63, 95% CI: 0.59 to 0.67, p = 0.856), suggesting comparable predictive abilities for falls in this subgroup (Fig. 2).
ROC curve and AUC of Cys C, Cre, eGFR, or SI for fall. (a) All participants. Red line represents Cys C (AUC 0.67, 95% CI 0.64 to 0.70), green line represents SI (AUC 0.62,95%CI:0.59 to 0.65), blue line represents Cre (AUC 0.56,95%CI:0.53 to 0.59), and purple line represents eGFR (AUC 0.60,95%CI:0.57 to 0.63). (b) Participants eGFR ≥ 75mL/min/1.73m2. Red line represents Cys C (AUC 0.64,95%CI:0.59 to 0.68), green line represents SI (AUC 0.63,95%CI:0.59 to 0.67), blue line represents Cre (AUC 0.54, 95% CI 0.50 to 0.58), and purple line represents eGFR (AUC 0.53, 95% CI 0.48 to 0.57). Abbreviations: Cys C, cystatin C; Cre, creatinine; eGFR: estimated glomerular filtration rates; SI: sarcopenia index.
Discussion
In this study, we identified elevated levels of Cys C, increased levels of Cre, and reduced SI as independent factors for falls in an American population. This study highlights that the difference in Cys C and Cre levels can offer valuable clinical information regarding the risk of falls. Serum creatinine and cystatin C were commonly utilized to assess renal function. Our finding was in accordance with an earlier study by Dukas et al. who found that a reduced creatinine clearance associated risk for falls and risk of becoming a faller31. Patients with chronic renal failure typically exhibit low serum 1,25(OH)2D3 concentrations due to impaired kidney synthesis, resulting in muscle weakness, atrophy, and an elevated risk of falls in the elderly17,32. Dukas et al. found a significant reduction in the risk of falls with alfacalcidol supplementation in individuals with creatinine clearance below 65 ml/min, while this effect was not evident in those with creatinine clearance up 65 ml/min31. In the studies by Zhao et al.33 and Gallagher et al.32 do not support the routine use of vitamin D in community-dwelling older people.
Non-linear analyses indicated an L-shaped association between fall risk and eGFR, with eGFR levels at approximately 75 mL/min/1.73 m² demonstrating a plateau lower risk. Moreover, further subanalyses did not find a significant association between Cre or eGFR and reported falls in individuals with eGFR greater than 75 mL/min/1.73m2. However, higher Cys C levels was strongly associated with higher odds of falls independent of age, disease status, and stage of kidney disease, suggested that cystatin C may impact fall risk through non-kidney function pathways34. The ROC analysis demonstrated that the AUC for Cys C was significantly higher than that for Cre, eGFR, and SI, underscoring the importance of Cys C as a more reliable biomarker for assessing the likelihood of falls among older adults. Notably, the difference in predictive ability between Cys C and SI was not statistically significant in our subanalysis, suggesting that while SI may provide some insights into fall-related factors, it does not enhance the accuracy of assessment beyond what is offered by Cys C alone. Consistently with our finding, Potok et al.22 indicated that in the hypertensive population, higher levels of cystatin C relative to creatinine are associated with an increased risk of incident frailty and mortality. Li et al.35 constructed the mHAI scores based Cys C levels and suggested association with objective mobility limitations in the individuals aged 80 years or older. Previous researchers proposed that inflammation was linked to increased serum Cys C levels34,36, which might correlate with decreased muscle mass and increased risk of falls. Petermann-Rocha37 showed its potential to screen sarcopenia both in men and women. A previous study has shown that baseline levels of cystatin C are associated with gait, balance, and strength in the Health ABC cohort38. Sarcopenia has been found to be positively correlated with SI, and lower SI levels have been identified as independent risk factors for cardiovascular events and poor prognosis37,39. We noted a lower intake of calories and a higher prevalence of stroke, heart failure, and arthritis in participants with lower SI and higher Cys C. Gielen et al.40 suggested an increase in the number of muscle mass among frail elderly patients following nutritional supplementation. In the sensitivity analysis, excluding patients with self-reported stroke and heart failure, and controlling for renal function, a significant association was observed with Cystatin C (OR: 1.17, 95% CI: 1.05, 1.31), whereas SI did not reach statistical significance (Table S1). Instead, we propose a readily available and time-effective laboratory test that may not only capture sarcopenia but also estimate the risk of falls. To our knowledge, this is the first study to analyze the association of cystatin C with falls using data from a large cross-sectional study based on NHANES.
However, there are some potential limitations to this study. First, self-reported recall bias for stroke and chronic heart failure diagnoses may exist, given that falls were asked to be recalled for the past year and might have been underestimated. Second, the cross-sectional design of the NHANES study limits our ability to establish causality between exposures and falls. The data were collected at a single time point, preventing us from determining whether changes in biomarkers such as Cys C and Cre precede or result from fall incidents. Third, despite adjusting for multiple potential confounders in our analyses, residual confounding from unmeasured covariates may still bias our results. Additionally, our analysis was based on biomarkers recorded only once, underscoring the need for longitudinal studies to explore how these biomarkers fluctuate over time. Understanding the trajectories of Cys C and Cre could provide valuable insights into their roles in fall risk and overall health. Moreover, conducting nutrition research would be beneficial to gain insight into the factors influencing the progression of these biomarkers and their implications for health41. Finally, it is essential to explore whether our present findings could be generalized to other populations besides the US population.
Conclusion
In conclusion, among a nationwide sampling of the older adults, we found that serum Cys C was strongly associated with self-reported and previous falls. In participants with eGFR > 75 mL/min/1.73m2, as cystatin C levels increase, the risk of falls also increases. This suggests that clinicians can gather information about patients’ overall health status solely by this marker which usually used to assess kidney function using.
Data availability
All data are publicly available and can be accessed at the NHANES website (https://wwwn.cdc.gov/nchs/nhanes/default.aspx). Relevant R code is available upon request to the corresponding author.
Change history
26 November 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41598-024-79849-3
References
Chen, X. et al. Age-stratified modifiable fall risk factors in Chinese community-dwelling older adults. Arch. Gerontol. Geriatr. 108https://doi.org/10.1016/j.archger.2023.104922 (2023).
Bergen, G., Stevens, M. R. & Burns, E. R. Falls and fall injuries among adults aged ≥ 65 years - United States, 2014. MMWR Morb Mortal. Wkly. Rep. 65, 993–998. https://doi.org/10.15585/mmwr.mm6537a2 (2016).
Ganz, D. A. & Latham, N. K. Prevention of falls in community-dwelling older adults. N Engl. J. Med. 382, 734–743. https://doi.org/10.1056/NEJMcp1903252 (2020).
Peel, N. M., Kassulke, D. J. & McClure, R. J. Population based study of hospitalised fall related injuries in older people. Inj Prev. 8, 280–283. https://doi.org/10.1136/ip.8.4.280 (2002).
Oh, J. et al. Association of falls and fear of falling with mortality in Korean adults: The Dong-gu Study. Chonnam Med. J. 55, 104–108. https://doi.org/10.4068/cmj.2019.55.2.104 (2019).
Sri-On, J. et al. Subsequent hospitalization, recurrent fall, and death within 6 months after a fall among elderly emergency department patients. Ann. Emerg. Med. 70, 516–521e512. https://doi.org/10.1016/j.annemergmed.2017.05.023 (2017).
Chowdhury, R., Peel, N. M., Krosch, M. & Hubbard, R. E. Frailty and chronic kidney disease: A systematic review. Arch. Gerontol. Geriatr. 68, 135–142. https://doi.org/10.1016/j.archger.2016.10.007 (2017).
Stevens, P. E. & Levin, A. Evaluation and management of chronic kidney disease: Synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann. Intern. Med. 158, 825–830. https://doi.org/10.7326/0003-4819-158-11-201306040-00007 (2013).
Beddhu, S. et al. Creatinine production, nutrition, and glomerular filtration rate estimation. J. Am. Soc. Nephrol. 14, 1000–1005. https://doi.org/10.1097/01.asn.0000057856.88335.dd (2003).
Ferguson, M. A. & Waikar, S. S. Established and emerging markers of kidney function. Clin. Chem. 58, 680–689. https://doi.org/10.1373/clinchem.2011.167494 (2012).
Kashani, K. B. et al. Evaluating muscle mass by using markers of kidney function: Development of the sarcopenia index. Crit. Care Med. 45, e23–e29. https://doi.org/10.1097/ccm.0000000000002013 (2017).
Zheng, C. et al. Serum creatinine/cystatin C ratio as a screening tool for sarcopenia and prognostic indicator for patients with esophageal cancer. BMC Geriatr. 22, 207. https://doi.org/10.1186/s12877-022-02925-8 (2022).
Shin, J. Y. Low serum creatinine to cystatin C ratio is independently associated with sarcopenia and high carotid plaque score in patients with type 2 diabetes. Nutr. Metab. Cardiovasc. Dis. 32, 1454–1462. https://doi.org/10.1016/j.numecd.2022.02.005 (2022).
Sim, M. et al. Creatinine to cystatin C ratio, a biomarker of sarcopenia measures and falls risk in community-dwelling older women. J. Gerontol. Biol. Sci. Med. Sci. 77, 1389–1397. https://doi.org/10.1093/gerona/glab369 (2022).
Desmet, C., Beguin, C., Swine, C. & Jadoul, M. Falls in hemodialysis patients: prospective study of incidence, risk factors, and complications. Am. J. Kidney Dis. 45, 148–153. https://doi.org/10.1053/j.ajkd.2004.09.027 (2005).
Heybeli, C., Kazancioglu, R., Smith, L., Veronese, N. & Soysal, P. Risk factors for high fall risk in elderly patients with chronic kidney disease. Int. Urol. Nephrol. 54, 349–356. https://doi.org/10.1007/s11255-021-02884-w (2022).
Peláez, V. C., Ausín, L., Mambrilla, M. R., Gonzalez-Sagrado, M. & Pérez Castrillón, J. L. Prospective observational study to evaluate risk factors for falls in institutionalized elderly people: the role of cystatin C. Aging Clin. Exp. Res. 27, 419–424. https://doi.org/10.1007/s40520-014-0304-1 (2015).
Dalrymple, L. S. et al. Kidney function and prevalent and incident frailty. Clin. J. Am. Soc. Nephrol. 8, 2091–2099. https://doi.org/10.2215/cjn.02870313 (2013).
Newman, A. B. et al. Trajectories of function and biomarkers with age: the CHS All Stars Study. Int. J. Epidemiol. 45, 1135–1145 (2016).
Li, C. et al. Association of cystatin C kidney function measures with long-term deficit-accumulation frailty trajectories and physical function decline. JAMA Netw. Open. 5, e2234208. https://doi.org/10.1001/jamanetworkopen.2022.34208 (2022).
Shlipak, M. G. et al. Cystatin C versus creatinine in determining risk based on kidney function. N Engl. J. Med. 369, 932–943. https://doi.org/10.1056/NEJMoa1214234 (2013).
Potok, O. A. et al. The difference between cystatin C- and creatinine-based estimated GFR and associations with frailty and adverse outcomes: A cohort analysis of the systolic blood pressure intervention trial (SPRINT). Am. J. Kidney Dis. 76, 765–774. https://doi.org/10.1053/j.ajkd.2020.05.017 (2020).
Curtin, L. R. et al. The National Health and Nutrition Examination Survey: Sample Design, 1999–2006. Vital Health Stat. 2 (2012).
Inker, L. A. et al. New creatinine- and cystatin C-based equations to estimate GFR without race. N Engl. J. Med. 385, 1737–1749. https://doi.org/10.1056/NEJMoa2102953 (2021).
Quartagno, M., Grund, S., Carpenter, J. R. & Jomo A flexible package for two-level joint modelling multiple imputation. R J. 11, 205 (2019).
Muntner, P. et al. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA. 324, 1190–1200. https://doi.org/10.1001/jama.2020.14545 (2020).
Robin, X. et al. pROC: an open-source package for R and S + to analyze and compare ROC curves. BMC Bioinform. 12, 77. https://doi.org/10.1186/1471-2105-12-77 (2011).
Gauthier, J., Wu, Q. V. & Gooley, T. A. Cubic splines to model relationships between continuous variables and outcomes: a guide for clinicians. Bone Marrow Transpl. 55, 675–680. https://doi.org/10.1038/s41409-019-0679-x (2020).
National Center for Health Statistics (US). National Health and Nutrition Examination Survey. NCHS Ethics Review Board (ERB) Approval, (2024). https://www.cdc.gov/nchs/nhanes/irba98.htm
Vandenbroucke, J. P. et al. Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. (London England). 12, 1500–1524. https://doi.org/10.1016/j.ijsu.2014.07.014 (2014).
Dukas, L., Schacht, E., Mazor, Z. & Stähelin, H. B. Treatment with alfacalcidol in elderly people significantly decreases the high risk of falls associated with a low creatinine clearance of < 65 ml/min. Osteoporos. Int. 16, 198–203. https://doi.org/10.1007/s00198-004-1671-9 (2005).
Gallagher, J. C., Rosen, C. J. & Vitamin, D. 100 years of discoveries, yet controversy continues. Lancet Diabetes Endocrinol. 11, 362–374. https://doi.org/10.1016/s2213-8587(23)00060-8 (2023).
Zhao, J. G., Zeng, X. T., Wang, J. & Liu, L. Association between calcium or vitamin D supplementation and fracture incidence in community-dwelling older adults: A systematic review and meta-analysis. Jama. 318, 2466–2482. https://doi.org/10.1001/jama.2017.19344 (2017).
Ivey-Miranda, J. B. et al. Cystatin C and muscle mass in patients with heart failure. J. Card Fail. 27, 48–56. https://doi.org/10.1016/j.cardfail.2020.07.013 (2021).
Li, K. et al. The modified Healthy Aging Index is associated with mobility limitations and falls in a community-based sample of oldest old. Aging Clin. Exp. Res. 33, 555–562. https://doi.org/10.1007/s40520-020-01560-w (2021).
Svensson, A. S., Kvitting, J. P., Kovesdy, C. P., Cederholm, I. & Szabó, Z. Changes in serum cystatin C, creatinine, and C-reactive protein after cardiopulmonary bypass in patients with normal preoperative kidney function. Nephrol. (Carlton). 21, 519–525. https://doi.org/10.1111/nep.12630 (2016).
Petermann-Rocha, F., Gray, S. R., Pell, J. P., Celis-Morales, C. & Ho, F. K. Biomarkers profile of people with sarcopenia: A cross-sectional analysis from UK Biobank. J. Am. Med. Dir. Assoc. 21https://doi.org/10.1016/j.jamda.2020.05.005 (2020). 2017.e2011-2017.e2019.
Odden, M. C. et al. Cystatin C and measures of physical function in elderly adults: the Health, Aging, and Body Composition (HABC) Study. Am. J. Epidemiol. 164, 1180–1189. https://doi.org/10.1093/aje/kwj333 (2006).
Lu, Y. W. et al. Serum creatinine to cystatin C ratio is associated with major adverse cardiovascular events in patients with obstructive coronary artery disease. Nutr. Metab. Cardiovasc. Dis. 31, 1509–1515. https://doi.org/10.1016/j.numecd.2021.01.024 (2021).
Gielen, E. et al. Nutritional interventions to improve muscle mass, muscle strength, and physical performance in older people: An umbrella review of systematic reviews and meta-analyses. Nutr. Rev. 79, 121–147. https://doi.org/10.1093/nutrit/nuaa011 (2021).
Juraschek, S. P. et al. Effect of glycemic index and carbohydrate intake on kidney function in healthy adults. BMC Nephrol. 17 https://doi.org/10.1186/s12882-016-0288-5 (2016).
Acknowledgements
The authors thank the staff and the participants of NHANES study for their valuable contributions.
Funding
The study was supported by the National Natural Science Foundation of China (Grant No.81571373, No.81601217, No.82001491), Natural Science Foundation of Hubei Province of China (Grant No. 2017CFB627), Health Commission of Hubei Province scientific research project (Grant No. WJ2021M247) and Scientific Research Fund of Wuhan Union Hospital (Grant No.2019).
Author information
Authors and Affiliations
Contributions
HJ: Conceptualization, Methodology, Formal analysis, Writing – original draft, VisualizationWRY: Conceptualization, Methodology, Writing – review & editing, VisualizationBLJ: Formal analysis, Data curation, ValidationLY: Formal analysis, Writing – review & editing.LM: Data curation, Writing – review & editing.ZLT: Data curationLLH: Methodology, Project administration, Writing – review & editing, SupervisionQBL: Conceptualization, Methodology, Project administration, Writing – review & editing, Supervision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Han, J., Wang, R., Bai, L. et al. Associations between serum cystatin C and fall reports in an Elderly population. Sci Rep 14, 26054 (2024). https://doi.org/10.1038/s41598-024-77138-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-77138-7