Abstract
Peri-implant infection is a serious complication in orthopedic surgery. This study aimed to reduce the incidence of peri-implant infection by developing a durable and safe antibacterial silver coating. We compared the antibacterial properties and process controllability of various coating techniques to identify the most effective method for silver coating. We refined substrate treatment techniques and coating thicknesses through antibacterial and scratch tests. Scanning electron microscopy (SEM) and energy-dispersive X-ray spectroscopy (EDS) were used to analyze the coating’s morphology and composition. Micron-sized magnetron sputtering silver coating samples underwent in vitro antibacterial testing, cytotoxicity testing, silver ion release testing, and osteogenic testing using membrane contact culture, CCK-8 assay, inductively coupled plasma (ICP) detection, and alkaline phosphatase (ALP) activity/osteogenic gene PCR. Magnetron sputtering demonstrated superior antibacterial properties, uniformity, and process controllability compared to alternative techniques. The optimal adhesion strength was achieved with a 0.5 μm coating thickness and a 400 mesh sandpaper pretreatment process, without compromising antibacterial efficacy. The coating showed near-perfect antiseptic results in antibacterial and anti-biofilm tests. Fibroblasts cultured in silver ion precipitation medium exhibited growth rates of 89% on day 30 and 88% on day 90, compared to 95% in the control group. The osteogenic test indicated that the magnetron sputtering silver coating promotes osteogenesis effectively. Our study demonstrated that micron-sized magnetron sputtering silver coating has potential for clinical use to prevent peri-implant infections in the future.
Similar content being viewed by others
Introduction
Artificial joint replacement and orthopedic internal fixation procedures are increasing due to global population growth, advancements in medical technology, and longer life spans. These factors also contribute to a rise in implant-associated postoperative complications1. Such complications pose significant challenges for both physicians and patients. For example, complications following primary joint replacement occur in 2–10% of cases and are associated with increased financial burdens and annual mortality rates of 8–25%2. Periprosthetic joint infection (PJI) accounts for 15.3% of all complications following joint replacement surgery and is one of the most frequent and severe outcomes. PJI often requires at least one revision surgery. The incidence of PJI is notably higher in patients with diabetes, rheumatoid arthritis, and immunodeficiency compared to the average incidence rate of 1–4%3. PJI frequently develops at the implant-tissue interface, an immunocompromised area where the immune system is less effective, making it particularly vulnerable to bacterial colonization and biofilm formation. Once pathogenic biofilm establishes, the immune system and traditional antibiotic treatments become ineffective, potentially leading to secondary surgery4. Although pathogen identification is challenging, systemic antibiotics remain the primary clinical treatment for PJI. However, the overuse of antibiotics has led to the global spread of multidrug-resistant (MDR) bacteria5. Consequently, there is an urgent need for orthopedic implants to possess intrinsic and durable antibacterial properties. Current research primarily focuses on developing new implant materials with inherent antibacterial qualities that can actively kill bacteria and passively inhibit their attachment, or applying antibacterial coatings to implant surfaces.
Silver has long been recognized as a superior antiseptic metal with a well-established mechanism of action, commonly used topically to treat burns and prevent wound infections6.Recently, with advancements in nanotechnology, silver nanoparticles (AgNPs) have garnered significant attention, particularly in biomedicine. AgNPs are known for their broad-spectrum and highly effective antibacterial and anticancer activities. They also promote bone healing, wound repair, and enhance vaccine immunogenicity7,8. However, the use of silver as an implant material is limited due to concerns about biosafety, especially regarding silver nanoparticles. Their high surface area, which increases the release of silver ions8, and their ability to penetrate bacterial cell membranes and damage organelles such as mitochondria and ribosomes9, significantly enhance the antibacterial effect of silver. However, this increased antibacterial activity also corresponds to higher toxicity. Research indicates that high concentrations of released silver ions and the nano-effect are linked to the toxic effects of silver nanoparticles10. Recent in vivo studies have shown that silver nanoparticles can be harmful to the skin, eyes, kidneys, respiratory system, hepatobiliary system, and immune system8.
In contrast, silver ions, which differ from silver nanoparticles, have been found to exhibit less cytotoxicity while maintaining comparable antibacterial activity11. The antibacterial efficacy of silver ions is significantly influenced by their valence state12,13. Oxidized silver ions can produce antibacterial atomic oxygen in the surrounding environment14,15. The concentration of silver ions directly correlates with their antibacterial activity. According to affinity and electrostatic attraction theories, silver ions can adhere to bacterial membranes, increasing membrane permeability and leading to bacterial death16. Additionally, the absorption of free silver ions by bacteria can inhibit respiratory enzymes, produce reactive oxygen species (ROS), and disrupt ATP synthesis17. Silver ions can also degrade ribosomes and inhibit DNA replication, which may ultimately stop bacterial growth18. This complex mechanism reduces the likelihood of bacterial resistance compared to traditional antibiotics. However, high concentrations of silver ions can still be toxic in vivo, with serum concentrations as low as 0.3 mg/mL potentially causing damage to the kidneys, liver, and nerve tissues, and leading to leukopenia. Consequently, the use of silver ion-coated implants in clinical settings is becoming less feasible19,20.
Therefore, developing a unique silver coating with particles larger than nanoscale and reduced silver ion release could enhance silver’s biocompatibility. Research has shown that various preparation methods for the same materials can result in differing functions and biocompatibilities21. In this study, different silver coating techniques were compared to achieve this goal, and magnetron sputtering technology was selected to apply a micron-sized silver coating to the surface of titanium alloy. Subsequently, the antibacterial properties, biofilm resistance, osteogenic potential, and in vitro biocompatibility of the magnetron sputtering silver coating were evaluated.
Materials and methods
Screening of silver coating process
The research flow chart is presented in Fig. 1. Various antibacterial silver coatings were prepared on titanium alloy substrates using ion implantation, electroplating, and magnetron sputtering techniques. The effectiveness of these coatings was assessed based on antibacterial test results and process controllability. The titanium alloy samples had a diameter of 20 mm and a thickness of 1 mm.
Ion implantation
Ion implantation is a method for modifying surfaces by injecting high-energy ions into solid materials under vacuum conditions22. In this study, silver ions were implanted into the substrate at a concentration of 1 × 1017 ions/cm3, with a maximum dose of double the single dose. One-dose and double-dose silver ion implantation coatings were prepared, with a total of 10 samples for each condition. The uncoated control sample and the silver ion implantation coated samples are shown in Fig. 2A and B, respectively.
Electroplating method
Electroplating involves coating a substrate with silver through electrolysis23. The process was conducted potentiostatically at 40 °C, with an operating voltage of 0.5 V and a deposition time of 40 min. The electroplated silver coating sample is shown in Fig. 2C.
Magnetron sputtering method
Magnetron sputtering is a vacuum coating technique used to deposit metals, alloys, and compounds onto various materials, achieving thicknesses up to a millimeter. It offers advantages such as a high deposition rate, precise controllability, and excellent uniformity. The TRP450 vacuum magnetron sputtering equipment was used to create a microscale silver coating. In this method, the substrate acted as the target, and silver atoms were accelerated in a high vacuum environment (6.6 × 10−6Pa)24. The silver atoms were sputtered onto the substrate’s surface, with a sputtering rate set at 0.25 μm/h. The resulting magnetron sputtering silver-coated sample is shown in Fig. 2D.
Screening of coating process by antibacterial test
The various silver coating samples were cultured with Staphylococcus aureus (MTCC 737) bacterial suspension at a concentration of 1 × 104 CFU/ml for 24 h using the membrane contact culture method. This was done to identify the best antibacterial coating method with optimal process controllability. Three operators independently assessed the controllability of the coating process during the interim.
Optimizing and preparation of silver coating by magnetron sputtering
Following the screening of coating methods, parameters for the magnetron sputtering coating, including coating thickness, substrate treatment, sputtering time, and sputtering speed, were optimized. Titanium alloy plates (20 mm in diameter and 1 mm in thickness) were cleaned with acetone and alcohol, then allowed to dry. The sample surface was cleaned again with acetone and alcohol in preparation for the next step. The titanium alloy surface was polished using sandpaper with 200, 400, and 600 mesh or uniformly ion-polished. Sputtering times were set to 1, 2, and 3 h at a speed of 0.25 μm/h, producing coatings of 0.25 μm, 0.5 μm, and 0.75 μm thicknesses, respectively, using the TRP450 vacuum magnetron sputtering equipment. Coating thickness was measured with the Bruker DektakXT Stylus Profiler, which provides a more convenient and direct measurement compared to SEM.
To determine the optimal coating thickness and substrate treatment method, the bonding force of the magnetron sputtering silver coatings of varying thicknesses (0.25 μm, 0.5 μm, and 0.75 μm) and substrate treatment methods was tested using the nano-indentation instrument G200 (Physical Properties Division, Materials Center, Tsinghua University). The antibacterial properties of different coating groups were also evaluated using the membrane contact culture method to balance antibacterial features with adhesion strength.
SEM and EDS
The scanning electron microscope (SEM) is an electron microscope used to study the surfaces of solid objects. It employs a low-energy focused electron beam as a probe, which is scanned over the specimen. The surface morphology and uniformity of the magnetron sputtering coating were observed using a backscattering scanning electron microscope (SEM, JEM7500). Energy Dispersive Spectroscopy (EDS), also known as energy dispersive X-ray spectroscopy, is an analytical technique used to characterize materials chemically25. EDS was used to determine the apparent concentration percentage of elements in the antibacterial coating and analyze the coating’s composition. Ag antibacterial coatings were prepared using sputtering powers of 8 W, 10 W, and 12 W, and the Ag content in the coating layers was analyzed by EDS.
Antibacterial test in vitro
Microbial preparation
To prepare the bacterial suspension, colonies of standard Staphylococcus aureus strain were taken from an AGAR plate and directly injected into regular saline. The density of the bacterial suspension was adjusted to 1 × 106 CFU/mL for the co-culture method and 1 × 104 CFU/mL for the membrane contact culture method using an optical turbidimeter.
Bacterial culture
Co-culture method
Samples from the magnetron sputtering silver-coated group and the uncoated group were placed into 6-well culture plates. Following the addition of 2 mL of the prepared Staphylococcus aureus suspension (1 × 106 CFU/mL), the plates were incubated for 24 h at 35 °C. After 24 h, 100 µL of the bacterial suspension was inoculated onto a blood AGAR culture plate and incubated at a constant temperature of 35 °C for an additional 24 h before colony counting.
Membrane contact culture method
Twenty microliters of prepared Staphylococcus aureus suspension (1 × 104 CFU/mL) were applied to the surface of the samples. A sterile transparent plastic film (φ20 mm) was placed over the sample surface to ensure even distribution of the bacterial solution. The sample was then placed in a φ100 mm Petri dish surrounded by sterile cotton balls moistened with saline to create a humid environment. After incubating at 35 °C for 24 h, the samples and plastic films were gently washed three times with 2 mL of sterile PBS to remove loosely attached bacteria. Subsequently, an ultrasonic cleaning instrument (40 kHz, 5 min) was used to thoroughly elute bacteria and biofilm from the sample surface. One hundred microliters of each rinsed (antibacterial test) and ultrasonicated (anti-biofilm test) bacterial solution were inoculated onto blood AGAR culture plates and incubated at 35 °C for 24 h.
Biofilm detection by SEM
The bacterial suspension was discarded, and the samples were gently washed three times with PBS to avoid removing adherent bacteria. The samples were then fixed with 2.5% glutaraldehyde at 4 °C for 2 h, followed by two additional PBS washes. Gradient alcohol dehydration was performed (50%, 60%, 70%, 80%, 90%, 95%, 100%) for 15 min each. After air drying and gold coating, the biofilm was observed using a cold field emission scanning electron microscope.
Bacteria live and dead staining
The bacteria live and dead staining test was performed according to the manufacturer’s instructions. Briefly, SYTO 9 reagent and PI reagent were dissolved in 5 mL sterilized deionized water, with a 1:1 ratio of SYTO 9 and PI reagent forming the staining solution. An equal amount of the staining solution and bacterial suspension from either the co-culture or membrane contact culture was added to a 96-well culture plate. After a 15-minute staining period at room temperature, away from light, the suspensions were centrifuged and washed with PBS three times. The samples were then examined using green and red channels on an immunofluorescence microscope.
Silver ion release test
The samples (coated and uncoated groups) were maintained at 37 °C in a CO2 incubator after being submerged in 50 milliliters of normal saline to replicate the in vivo environment, in accordance with ISO 10993-12. Silver ion concentrations precipitated on the 7th, 30th, and 90th days were measured using inductively coupled plasma mass spectrometry (ICP-MS, Thermo, USA). For the subsequent cytotoxicity test, 2 milliliters of the precipitation solution were filtered and sterilized after 30 and 90 days of precipitation.
Cytotoxicity test
Human fibroblasts were purchased from BeNa Culture Collection. They were cultured in a DMEM cell medium containing 10% fetal bovine serum and 1% penicillin/streptomycin in a humid atmosphere of 5% CO2 at 37 °C. After the cells reached the logarithmic growth phase, cell suspension was prepared and adjusted to 1 × 105cells/mL for the following experiments. Then 100ul of cell suspension (cell amount: 10,000 cells) was added into the 96-well plate in an incubator for 4 h. After the cells were fully attached to the wall, 10µL of silver ion precipitation solution (30th and 90th day) prepared previously were added to the 96-well plates in incubator for 24 h. Then 10µL of CCK-8 solution was added to each well and the cells were incubated in an incubator for 4 h away from light. The optical density (OD) was detected at 450 nm by a microplate reader. The relative growth rate of cells (RGR) was calculated by the equation below. RGR above 75% is considered non-cytotoxic according to ISO 10993-5.
Osteogenic ability experiment
Cell culture
Human osteosarcoma cells (MG63) were purchased from BeNa Culture Collection. They were cultured in DMEM cell medium containing 15% fetal bovine serum and placed in a 100 mm sterile dish in a humid atmosphere of 5% CO2 at 37 °C. After the cells reached the logarithmic growth phase, cell suspension at concentration of 1 × 105cell / mL was prepared for the next experiment.
Quantitative determination of alkaline phosphatase
Human osteosarcoma cells (MG63) were co-cultured with the coated and uncoated samples. Cells were lysed with IP cell lysate (China Biyuntian Biotechnology Co., Ltd.) after 3 and 7 days. Enhanced BCA Protein Assay Kit (China Biyuntian Biotechnology Co., Ltd.) was used to detect the protein quantity and active unit of alkaline phosphatase. The concentration of alkaline phosphatase in unit mass of each group was calculated and compared to describe the osteogenic ability of the coating.
Osteogenic gene expression
Human osteosarcoma cells (MG63) were co-cultured with the coated samples. Cell RNAs were extracted after 3 and 7 days, then the RNAs were reverse transcripted into cDNA and PCR amplification was performed using ALPL and BMP2 primers (Table 1) to detect the expression levels of corresponding genes. At the same time, GAPDH was used as a reference gene.
Statistical analysis
All experimental data were processed by SPSS 23.0 (IBM SPSS, US) software. One-way ANOVA was used to compare the means of multiple copies. Independent-samples t-Test was used to compare the mean values of the two groups. The difference was considered to be statistically significant when P < 0.05.
Results
Magnetron sputtering coating possesses the best antibacterial ability, uniformity and process controllability among three coatings
Ion implantation prevented the negative effects typically associated with other coating techniques by injecting silver ions into the material’s inner surface without altering the substrate’s initial roughness. However, because silver atoms were implanted deeper into the substrate, ion implantation was less effective at releasing antibacterial components or providing a direct antibacterial effect. Although electroplating coatings have demonstrated excellent antibacterial properties in numerous studies, their lack of uniformity, poor adhesion strength, and uncontrollable coating thickness made them less suitable for antibacterial applications26,27. In contrast, magnetron sputtering produced a mirror-like silver coating with superior uniformity and adhesion strength. The process controllability of the coatings was rated as follows by the three independent operators: magnetron sputtering, ion implantation, and electroplating. Figure 2 shows representative images of the various silver-coated and uncoated samples.
The antibacterial properties of the various coating processes were assessed using a membrane contact method with 1 × 104 CFU/mL of Staphylococcus aureus. As shown in Fig. 2, the magnetron sputtering coating group exhibited no bacterial growth, the electroplating group had fewer bacterial colonies, while the ion implantation and uncoated groups had large numbers of bacterial colonies. Based on these results, the magnetron sputtering coating was selected for its superior antibacterial features, uniformity, and adhesion strength.
Optimization and characteristics of silver coating by magnetron sputtering
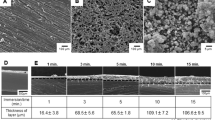
Magnetron sputtering silver-coated samples with various substrate treatments and coating thicknesses were compared to maximize coating adhesion strength. The coatings on substrates pretreated with 200 and 600 mesh sandpaper, as well as those on ion-polished substrates, partially detached after ultrasonic irrigation (40 kHz, 5 min). In contrast, the coating on substrates pretreated with 400 mesh sandpaper remained intact (Fig. 3A), indicating that the appropriate roughness of the substrate enhanced the bonding strength of the magnetron sputtering silver coating. As depicted in Fig. 3C; Table 2, the scratch load strength did not show a statistically significant difference between the 0.25 μm and 0.5 μm magnetron sputtering silver coatings (P > 0.05). However, the scratch load strength significantly decreased in the 0.75 μm coating group (P < 0.05). Furthermore, no bacterial growth was observed on the coated groups with varying thicknesses compared to the uncoated group (Fig. 3B), indicating that the antibacterial properties of the magnetron sputtering silver coating were unaffected by coating thickness. Therefore, the 400 mesh sandpaper-pretreated substrate with a 0.5 μm thickness of magnetron sputtering silver coating was selected for further experiments, as shown in Fig. 4A. The surface morphology of the magnetron sputtering silver coating was examined using SEM. As shown in Fig. 4B, the average size of the silver particles was approximately 0.1–0.5 μm, with larger island-shaped particles up to 1 μm in size. EDS component analysis revealed minimal variation in silver content across different coating sites on the sample surface (P > 0.05) (Fig. 4D; Table 3). The EDS surface scan in Fig. 4C indicated that the primary component of the film layer was Ag, with only a small amount of C impurities present. The component distribution was uniform, and base material composition was not detected in the surface scan results. The Ag content in the coating layers prepared using sputtering powers of 8 W, 10 W, and 12 W was analyzed by EDS, as shown in Fig. 5; Table 4.
Optimization of magnetron sputtering silver coating according to adhesion strength and antibacterial ability. (A) Pictures of different substrate-pretreated magnetron sputtering silver coating samples after ultrasonic irrigation (40KHZ, 5 min), a: ion polishing, b:200 mesh sandpaper polishing, c:400 mesh sandpaper polishing, d:600 mesh sandpaper polishing. (B) The antibacterial features of magnetron sputtering silver coatings with different thicknesses. abc: coated group, def: uncoated group. The thicknesses of coatings were 0.25 μm(a),0.5 μm(b),0.75 μm(c) respectively. (C) Scratch test results of different coating thicknesses, (0.25 μm, 0.5 μm,0.75 μm). As shown, 400 mesh sandpaper pretreated magnetron sputtering silver coating with 0.5 μm thickness was the best from the perspectives of adhesion strength and antibacterial ability.
Surface morphology and component analysis of the silver coated samples under SEM and EDS. (A) General pictures of the magnetron sputtering silver coated samples. (B) Surface morphology of the coating observed by the SEM in varying magnifications. (a) 2,000 times magnification, (b) 10,000 times magnification, (c) 20,000 times magnification, (d) 50,000 times magnification. (C) Pictures of the silver-coated surfaces were scanned via EDS. D. Component analysis of silver coating at different sites under SEM-linked EDS.
Magnetron sputtering silver coating exerted excellent contact antibacterial and anti-biofilm features in vitro
In the Staphylococcus aureus co-culture antibacterial experiment, both the coated and uncoated groups showed exponential growth in bacterial colonies over 24 h, with no statistically significant difference between them (P > 0.05) (Fig. 6A and B). However, following a 24-hour membrane contact culture, no bacterial growth was observed on the coated group’s culture plate, whereas the uncoated group exhibited extensive colony formation (Fig. 6A). Additionally, the bacteria live and dead staining results for the co-culture group revealed that most bacteria in the coated group were stained red, indicating dead bacteria, while the majority of bacteria in the uncoated group were stained green (Fig. 6C). SEM imaging further confirmed the presence of a significant biofilm in the uncoated group, while no noticeable biofilm formation was observed on the magnetron sputtering silver-coated samples (Fig. 6D). These findings demonstrate the superior contact antibacterial and anti-biofilm properties of the magnetron sputtering silver coating.
Antibacterial and antibiofilm abilities of magnetron sputtering silver coating. (A) Colony count after incubation with Staphylococcus aureus for 24 h by co-culture method and membrane contact method. ab: magnetron sputtering silver coated titanium alloy group, cd: uncoated titanium alloy group, ac: co-culture method, bd: membrane contact method. (B) Time / CFU curve of the silver coated and uncoated groups after incubation with Staphylococcus aureus over time by co-culture method. (C) Bacteria live and dead staining of Staphylococcus aureus after cultured with silver coated titanium alloy for 24 h by co-cultured method or membrane contact method. As shown, there was almost no green stained live bacteria in the membrane contact method group while there were full of green stained live bacteria in the co-culture method group, which further supported the excellent contact antibacterial feature of the magnetron sputtering silver coating. (D) Representative SEM images of Magnetron sputtering silver coated titanium alloy (a) and uncoated titanium alloy (b). No obvious biofilm formation was observed on the surface of silver coated titanium alloy while there were large areas of biofilms on the surface of uncoated titanium alloy.
Silver ion release of magnetron sputtering silver coating was low and no obvious early-stage cytotoxicity in vitro
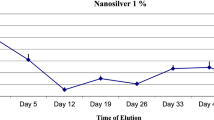
The average silver ion concentrations for the magnetron sputtering group were measured as 10 ± 1.5 ng/mL on day 7, 381 ± 17.8 ng/mL on day 30, and 421 ± 21.4 ng/mL on day 90, as determined by ICP-MS (Fig. 7A). For the cytotoxicity evaluation, fibroblasts were cultured with precipitation medium (day 30 and day 90) from magnetron sputtering silver-coated and uncoated samples for 24 h. The relative growth rates (RGR) were assessed using the CCK-8 test. On day 30, the RGRs were 89% for the coated group and 95% for the uncoated group; on day 90, the RGRs were 88% and 93%, respectively (Fig. 7B). All RGR values were above 75%, indicating that the coatings were non-toxic according to ISO 10993-5 standards.
Silver ion release and early-stage cytotoxicity of magnetron sputtering silver coating. (A) ICP detection of silver ion precipitation concentration in magnetron sputtering coating group with time. (B) Relative growth rate (RGR) of the silver coated and uncoated group fibroblasts in silver precipitation (30 day and 90 day) culture medium.
Magnetron sputtering silver coating showed good osteogenic ability in vitro
The alkaline phosphatase (ALP) activity in the magnetron sputtering silver-coated group was significantly higher than that in the uncoated group on both the 3rd and 7th days of the ALP activity experiment (P < 0.05) (Fig. 8A). Additionally, the mRNA levels of osteogenic markers, such as ALPL and BMP-2, were significantly elevated in the coated group on day 7 compared to day 3 (P < 0.05) (Fig. 8B and C). These results indicate that the magnetron sputtering silver coating promotes osteogenic activity over time.
Discussion
As the population ages, an increasing number of patients with osteoarthritis or fractures require internal fixation with orthopedic implants or joint replacement surgery. A significant complication associated with these procedures is periprosthetic or peri-implant joint infection (PJI). Despite advancements in orthopedic surgery, 1–4% of implants still experience infections28. One of the major challenges for orthopedic surgeons is preventing and managing infections related to implants. Inhibiting biofilm formation and bacterial colonization is crucial for infection prevention. Creating antimicrobial surfaces is a key strategy to address bacterial colonization and biofilm development. Titanium alloys are widely used for orthopedic implants due to their excellent mechanical properties, fatigue resistance, wear resistance, and biocompatibility, although they lack inherent antibacterial qualities29. While silver (Ag) and its ions have known potent antibacterial properties, including a broad spectrum of activity and durability, high concentrations of silver ions or nanoscale silver can be harmful to human health30. Finding the optimal balance between silver’s antibacterial efficacy and biocompatibility remains challenging, with concerns particularly surrounding the biocompatibility of nano-silver. Combining the advantages of titanium alloys with silver to create biomaterials that offer both strong antibacterial properties and good biocompatibility is a promising approach. Wan et al. demonstrated the antibacterial enhancement of titanium alloy surfaces through silver coating but did not address the biocompatibility of the materials31. This study utilizes magnetron sputtering to apply a silver coating to titanium alloy surfaces. The resulting micron-size silver coating, which exhibits excellent antibacterial properties, osteogenic effects, and low silver ion release without significant early-stage cytotoxicity, appears to be a safer alternative to controversial silver nanoparticles.
In the 1970s, a high-speed, low-temperature deposition technique known as magnetron sputtering was developed32. Chang and colleagues used this method to produce a silver coating on tantalum oxide surfaces33. Their study demonstrated that the silver coating enhanced the hydrophobicity and water contact angle of tantalum oxide and exhibited effective antibacterial activity against Staphylococcus aureus. Similarly, Gao et al. applied magnetron sputtering to create a silver coating on titanium implant surfaces, showing sustained antibacterial activity against Escherichia coli and Staphylococcus aureus. However, they did not evaluate the biocompatibility of the silver coating34. In our study, we applied silver coatings to titanium alloy surfaces using magnetron sputtering, electroplating, and ion implantation techniques. The results indicated that magnetron sputtering yielded coatings with superior uniformity, antibacterial properties, and process controllability. Further investigation into the adhesion strength of the magnetron sputtering coatings revealed that it depended on the coating’s thickness and the substrate’s roughness. The optimal adhesion strength and antibacterial performance were achieved with a 0.5 μm thick silver coating on a substrate pre-treated with 400 mesh sandpaper. We hypothesize that this pre-treatment created a uniformly distributed surface with irregular micro-pits, which disrupted internal shrinkage stress during deposition and reduced residual stress in the coating. Additionally, the micro-pits enhanced the nucleation density of the silver coating on the substrate surface and facilitated nucleation. The interlocking laminated structures formed by silver atoms depositing in the pits improved the mechanical adhesion between the substrate and the coating. However, the increased binding force between the substrate and the silver coating also reduced the release of silver ions, further decreasing the biological toxicity of the silver ions. Moreover, the increase in substrate area resulting from the enhanced surface roughness improved the formation of diverse physical and chemical adsorption. Concurrently, as substrate roughness increased, the coating-cell surface area also increased, which often led to improved fibroblast adhesion and growth in cytotoxicity tests35,36. The advantages of our coating method and parameters suggested that this silver coating might possess exceptional antibacterial properties and biocompatibility. To confirm the antibacterial performance and biocompatibility of the magnetron sputtering silver coating, titanium alloys coated with silver to a thickness of 0.5 μm and pretreated with 400 mesh sandpaper were selected for further in vitro experiments.
The Ag content is crucial to the antibacterial performance, and the apparent concentration percentage of Ag ions provides insights into the uniformity and antibacterial properties of the coating layer. As shown in Fig. 5; Table 4, when the sputtering power is 8 W, the EDS results indicate that the Ag content is around 70%. The EDS surface scan also detects some of the substrate composition, suggesting insufficient film thickness and uniformity, which results in poor antibacterial performance. However, increasing the power to 10 W or above raises the Ag content to approximately 85%, with Ag being the dominant element in the film layer and exhibiting minimal variations in relative content. This leads to improved antibacterial effectiveness of the film layer. The Ag target power is also crucial for the coating’s properties; higher power accelerates the Ag ion deposition rate. However, excessively high power can cause the energy of sputtered Ag ions to be too high, making deposition on the substrate difficult. Additionally, high power can reduce the coating’s uniformity and compactness, affecting its overall quality. Finally, target power influences the coating’s morphology and structure. As power increases, Ag particles on the coating surface become smaller and more uniform, and the coating structure becomes more compact. This is due to the higher energy of atoms or ions sputtered at high power, which form a more compact packing structure on the substrate37,38. With high Ag relative content, the difference in Ag content is minimal when the sputtering power increases from 10 W to 12 W. To avoid the negative effects associated with high power, we ultimately selected 10 W for sputtering the coating. The EDS composition analysis and surface scanning results indicated that our film layers exhibited good uniformity and compactness. This finding aligns with previous studies. Chen et al39. employed radio frequency magnetron sputtering technology to apply a hydroxyapatite coating containing silver to the surface of pure titanium substrates. The XRD pattern obtained with an Ag target power of 10 W and a HA target power of 300 W revealed that compared to the original pure Ti substrate, the contact angle of the Ag-HA co-deposited coating was significantly reduced, enhancing both hydrophilicity and antibacterial properties. Wu et al38. used RF magnetron sputtering to prepare Ag and Ta co-doped ACP-coated films on Ti substrates, with targets of varying Ta concentrations (0, 0.9, and 9.0 mol%) and a constant Ag concentration (10.0 mol%). The sintered dense bodies were labeled as Ag-TCP, (Ag + L-Ta)-TCP, and (Ag + HTa)-TCP, respectively. The Ag concentration in the coatings prepared with (Ag + L-Ta)-TCP and (Ag + H-Ta)-TCP decreased from 9.6 mol% to 3.7 mol% and from 12.8 mol% to 3.8 mol%, respectively, as RF power increased from 8 W to 50 W. Ivanova et al40. utilized a 220 mm diameter Ag-Hap target and prepared Ag-Hap coating films using RF magnetron sputtering at an RF power of 500 W. They reported that the Ag concentration in the coating film (1.5 mol%) was significantly lower than that in the target material (9.8 mol%).
Using the membrane contact method, in vitro antibacterial experiments revealed that the silver-coated group exhibited excellent antibacterial activity against Staphylococcus aureus, while the co-culture method showed no discernible antibacterial activity. The antibacterial test confirmed the biosafety of the coating by demonstrating minimal release of silver ions from the silver coating. After culturing Staphylococcus aureus on the surfaces of both groups for 24 h, SEM analysis showed massive bacterial attachment and biofilm formation on the uncoated group, whereas no such formation was observed in the silver-coated group. Since PJI typically originates at the bone-implant interface and the initial bacterial concentration causing PJI is usually very low, the results indicated that the magnetron sputtering silver coating exhibited excellent contact antibacterial properties rather than a releasing antibacterial property, which was sufficient to prevent PJI. We speculate on the possible mechanisms involved: (1) Magnetron sputtering technology offers advantages such as controllable film thickness, high purity, low temperature, high speed, and good adhesion. These factors contribute to a firm bond between the coating and the substrate, enhancing the coating’s service life and improving its antibacterial and osteogenic properties. (2) The micro-pits created by sandpaper provide ideal sites for protein adsorption41, facilitating the binding of adsorbed proteins to cell membrane receptors like ligands42,43. This process may inhibit bacterial adhesion and biofilm formation. Even if bacteria contact the coating initially, they are rapidly inactivated by the silver coating, preventing extracellular matrix secretion and inhibiting biofilm formation, thereby avoiding irreversible bacterial adhesion and proliferation. (3) During the preparation of antibacterial films via magnetron sputtering of silver ions, small particles within the film layer aggregate to form larger, island-shaped particles. Compared to smaller particles, these larger particles: (i) increase the likelihood of contact between the silver ion film and bacteria, thereby enhancing antibacterial effectiveness; (ii) improve the stability of the film layer, reducing damage due to external forces; and (iii) act as reservoirs for silver ions, allowing for sustained release and improving the sustained-release effect in antibacterial performance.
The killing effect of silver ions is non-selective, and their strong antibacterial properties can be a double-edged sword. While inhibiting bacteria, silver ions can also damage normal cells. Our results demonstrated that the group with silver coatings produced via magnetron sputtering had extremely low free silver ion release, below the safe threshold for silver ion concentration in drinking water as defined by the WHO’s Fourth Edition of “Guidelines for Drinking Water Quality” and GB5749-2006. Since silver nanoparticles can be directly toxic to cells due to the nano-effect and/or high concentrations of released silver ions, this micron-sized silver coating offers advantages over silver nanoparticles44. In addition to the negative nano-effect, the large surface area of nanoparticles accelerates the release of silver ions. Research has shown that the bacteriostatic ring test of nano-silver coatings produced clear antibacterial rings, indicating high concentrations of free silver ion precipitation45. The high concentration of silver ions released from conventional silver coatings can cause toxicity to the human body, potentially due to the aggregation of silver ions in cells and tissues. The relatively small amount of free silver ions released from this novel magnetron sputtering silver coating is significant in vitro46. Silver ions, due to their size similarity to certain biomolecules, including DNA and proteins, can directly damage DNA and denature proteins, resulting in cell death through mitochondrial membrane destruction, free oxygen radical production, and apoptotic pathway activation13,47. Our early-stage cytotoxicity test on human fibroblasts showed that the RGR of the coating group was 89% (day 30) and 88% (day 90), significantly higher than the International Standards Organization’s safety standard of 75%. We used MG63 cells for their ease of culture, low heterogeneity, and robust nature compared to hMSC48. These results suggest that the silver coating prepared by magnetron sputtering has good biosafety.
A significant contributing factor to implant failure, aside from infection, is implant loosening49. Osteolysis caused by wear from metal and polyethylene is a common cause of implant loosening50,51, making the biotribological aspect of metal wear a primary focus for prevention. Research revealed that silver-coated implants experience less wear compared to titanium alloys52. Effective strategies to prevent implant loosening include promoting bone formation and stimulating osteogenic differentiation53. In this study, we assessed ALP activity and the expression of osteogenic genes using the MG63 cell line to investigate the impact of magnetron sputtering silver coating on osteogenic activity. ALP, a glycoprotein present on cell surfaces that plays a role in mineralization, is a significant early indicator of osteogenic differentiation and is frequently used to evaluate osteogenic capacity54. The ALP activity of the silver coating group was higher than that of the uncoated group on the third and seventh days of the experiment. ALPL and BMP-2 are key osteogenic genes55, and their expression was significantly higher in the silver-coated group on the seventh day compared to the third day, indicating an increasing osteogenic potential of the silver coating over time. These findings suggest that the osteogenic ability was enhanced by this micron-sized silver coating prepared by magnetron sputtering, both at functional and genetic levels.
Nevertheless, this study has certain limitations. We investigated the antibacterial activity of magnetron sputtering silver coating only against Staphylococcus aureus; the antibacterial effects on other bacteria such as Staphylococcus epidermidis and Escherichia coli remain to be determined. Additionally, in silico, in vivo, and antibacterial mechanism studies are required for clinical application. In silico studies are especially recommended for the next steps due to their lower cost and faster results56. Although we observed that magnetron sputtering silver coating could enhance osteogenic ability, further research is necessary to fully understand the osteogenic mechanism. The roughness, long-term stability, and performance of the coating have not yet been studied, which are also limitations of this study. We will address these aspects in subsequent experiments. Currently, our animal experiments, including assessments of in vivo antibacterial properties and biosafety, have been completed, and the article will be published soon.
Conclusions
The magnetron sputtered silver coating with a sputtering power of 10 W, a coating thickness of 0.5 μm, and ground with 400 mesh sandpaper demonstrated excellent surface contact antibacterial activity, anti-biofilm properties, osteogenesis, and no significant biological toxicity in vitro. This provides a theoretical basis for the future clinical application of silver-coated orthopedic implants.
Clinical perspectives
As orthopedic surgery is currently unavoidable, periprosthetic joint infection (PJI) is a catastrophic consequence. The implant-tissue interface is a common site for PJI, as it is an area where the immune system is less effective, making the implant-tissue surface particularly susceptible to bacterial colonization and biofilm formation. Therefore, there is an urgent need for orthopedic implants to possess intrinsic and durable antibacterial properties. This study aims to reduce the incidence of peri-implant infection by developing a long-lasting, safe antibacterial silver coating. The magnetron sputtering silver coating demonstrated excellent surface contact antibacterial and anti-biofilm properties, good osteogenic ability, and minimal silver ion release with no significant biological toxicity. The selected magnetron sputtering process and coating parameters improved the biological safety of silver to some extent and provided a theoretical basis for the future clinical application of silver-coated orthopedic implants.
Data availability
All the raw data are available upon request to the corresponding author.
References
Jamari, J. et al. The Effect of Bottom Profile Dimples on the Femoral Head on Wear in Metal-on-Metal Total Hip Arthroplasty. J. Funct. Biomater. 12(2), (2021).
Otto-Lambertz, C. et al. Periprosthetic infection in joint replacement. Dtsch. Arztebl Int. 114 (20), 347–353 (2017).
Glyn-Jones, S. et al. Osteoarthritis. Lancet 386(9991), 376–387 (2015).
Orapiriyakul, W. et al. Antibacterial surface modification of titanium implants in orthopaedics. J. Tissue Eng. 9, 2041731418789838 (2018).
Høiby, N. et al. Antibiotic resistance of bacterial biofilms. Int. J. Antimicrob. Agents. 35 (4), 322–332 (2010).
Hussain, A. & Choukairi, F. To cool or not to cool: evolution of the treatment of burns in the 18th century. Int. J. Surg. 11 (7), 503–506 (2013).
Brennan, S. A. et al. Silver nanoparticles and their orthopaedic applications. Bone Joint J. 97-b (5), p582–p589 (2015).
Xu, L. et al. Silver nanoparticles: synthesis, medical applications and biosafety. Theranostics. 10 (20), 8996–9031 (2020).
Liu, X. et al. Antibacterial properties of nano-silver coated PEEK prepared through magnetron sputtering. Dent. Mater. 33 (9), e348–e360 (2017).
Pauksch, L. et al. Biocompatibility of silver nanoparticles and silver ions in primary human mesenchymal stem cells and osteoblasts. Acta Biomater. 10 (1), 439–449 (2014).
Li, W. R. et al. A comparative analysis of antibacterial activity, dynamics, and effects of silver ions and silver nanoparticles against four bacterial strains. Int. Biodeterior. Biodegrad. 123, 304–310 (2017).
Melaiye, A. et al. Silver(I)-imidazole cyclophane gem-diol complexes encapsulated by electrospun tecophilic nanofibers: formation of nanosilver particles and antimicrobial activity. J. Am. Chem. Soc. 127 (7), 2285–2291 (2005).
Pal, S. et al. Synthesis of highly antibacterial nanocrystalline trivalent silver polydiguanide. J. Am. Chem. Soc. 131 (44), 16147–16155 (2009).
Atiyeh, B. S. et al. Effect of silver on burn wound infection control and healing: review of the literature. Burns. 33 (2), 139–148 (2007).
Dellasega, D. et al. Nanostructured Ag(4)O(4) films with enhanced antibacterial activity. Nanotechnology. 19 (47), 475602 (2008).
Khorrami, S. et al. Selective cytotoxicity of green synthesized silver nanoparticles against the MCF-7 tumor cell line and their enhanced antioxidant and antimicrobial properties. Int. J. Nanomed. 13, 8013–8024 (2018).
Ramkumar, V. S. et al. Biofabrication and characterization of silver nanoparticles using aqueous extract of seaweed Enteromorpha compressa and its biomedical properties. Biotechnol. Rep. (Amst). 14, 1–7 (2017).
Durán, N., Nakazato, G. & Seabra, A. B. Antimicrobial activity of biogenic silver nanoparticles, and silver chloride nanoparticles: an overview and comments. Appl. Microbiol. Biotechnol. 100 (15), 6555–6570 (2016).
Donati, F. et al. Silver-coated hip megaprosthesis in oncological limb savage surgery. Biomed. Res. Int. 2016, p9079041 (2016).
Denes, E., Balkhi, S. E. & Fiorenza, F. Local Argyria due to Silver-Coated Megaprosthesis. Am. J. Med. 135 (6), e116 (2022).
Ibrahim, A. A. et al. Synthesis of 12-tungestophosphoric acid supported on Zr/MCM-41 composite with excellent heterogeneous catalyst and promising adsorbent of methylene blue. Colloids Surf., a. 631, 127753 (2021).
Feng, Z. C. et al. Synthesis, Structural and Magnetic Properties of Cobalt-Doped GaN Nanowires on Si by Atmospheric Pressure Chemical Vapor Deposition. Mater. (Basel) 16(1),97 (2022).
Kao, Y. J. et al. Significant Hall-Petch effect in micro-nanocrystalline electroplated copper controlled by SPS concentration. Sci. Rep. 13 (1), 428 (2023).
Smolik, J. et al. Evaluation of the Fracture Toughness K(Ic) for Selected Magnetron Sputtering Coatings by Using the Laugier Model. Mater. (Basel) 15(24), 9061(2022).
Wu, Y. et al. High-voltage energy dispersive x-ray spectrometry using a low-energy primary beam. J. Vacuum Sci. Technol. B 32(6), 06FC05 (2014).
Han, X. et al. Surface modification techniques of titanium and titanium alloys for biomedical orthopaedics applications: a review. Colloids Surf., B. 227, 113339 (2023).
Jing, Z. et al. Functionalization of 3D-printed titanium alloy orthopedic implants: a literature review. Biomed. Mater. 15 (5), 052003 (2020).
Kose, N. et al. A silver ion-doped calcium phosphate-based ceramic nanopowder-coated prosthesis increased infection resistance. Clin. Orthop. Relat. Res. 471 (8), 2532–2539 (2013).
Kaur, M. & Singh, K. Review on titanium and titanium based alloys as biomaterials for orthopaedic applications. Mater. Sci. Eng. C Mater. Biol. Appl. 102, 844–862 (2019).
Rai, M., Yadav, A. & Gade, A. Silver nanoparticles as a new generation of antimicrobials. Biotechnol. Adv. 27 (1), 76–83 (2009).
Wan, Y. Z. et al. Surface modification of medical metals by ion implantation of silver and copper. Vacuum. 81 (9), 1114–1118 (2007).
Swann, S. Magnetron sputtering. Phys. Technol. 19 (2), 67 (1988).
Huang, H. L. et al. Antibacterial properties and cytocompatibility of tantalum oxide coatings with different silver content. J. Vacuum Sci. Technol. A 32(2), 02B117(2014).
Gao, A. et al. The effects of titania nanotubes with embedded silver oxide nanoparticles on bacteria and osteoblasts. Biomaterials. 35 (13), 4223–4235 (2014).
Yamashita, D. et al. Effect of surface roughness on initial responses of osteoblast-like cells on two types of zirconia. Dent. Mater. J. 28 (4), 461–470 (2009).
Hou, Y. et al. Surface roughness gradients reveal topography-specific mechanosensitive responses in human mesenchymal stem cells. Small. 16 (10), e1905422 (2020).
Shi, J. Z. et al. The effect of process conditions on the properties of bioactive films prepared by magnetron sputtering. Vacuum. 83 (2), 249–256 (2008).
Wu, J., Ueda, K. & Narushima, T. Fabrication of Ag and Ta co-doped amorphous calcium phosphate coating films by radiofrequency magnetron sputtering and their antibacterial activity. Mater. Sci. Engineering: C. 109, 110599 (2020).
Chen, W. et al. In vitro anti-bacterial and biological properties of magnetron co-sputtered silver-containing hydroxyapatite coating. Biomaterials. 27 (32), 5512–5517 (2006).
Ivanova, A. A. et al. Fabrication and physico-mechanical properties of thin magnetron sputter deposited silver-containing hydroxyapatite films. Appl. Surf. Sci. 360, 929–935 (2016).
Firkowska-Boden, I., Zhang, X. & Jandt, K. D. Controlling Protein Adsorption through Nanostructured Polymeric Surfaces. Adv. Healthc. Mater. 7(1), 1700995(2018).
Luo, N. et al. PEGylated graphene oxide elicits strong immunological responses despite surface passivation. Nat. Commun. 8, 14537 (2017).
Zhu, Y. et al. Bacterial and mammalian cells adhesion to tantalum-decorated micro-/nano-structured titanium. J. Biomed. Mater. Res. A. 105 (3), 871–878 (2017).
Choi, Y. et al. Comparative toxicity of silver nanoparticles and silver ions to Escherichia coli. J. Environ. Sci. (China). 66, 50–60 (2018).
Shukla, S. P. et al. Size selective green synthesis of silver and gold nanoparticles: enhanced Antibacterial efficacy of Resveratrol Capped Silver Sol. J. Nanosci. Nanotechnol. 16 (3), 2453–2463 (2016).
Kunrath, M. F. & Campos, M. M. Metallic-nanoparticle release systems for biomedical implant surfaces: effectiveness and safety. Nanotoxicology. 15 (6), 721–739 (2021).
Locht, L. J. et al. Uptake of silver from metallic silver surfaces induces cell death and a pro-inflammatory response in cultured J774 macrophages. Histol. Histopathol. 26 (6), 689–697 (2011).
Kühl, J. et al. Extrusion-based 3D printing of osteoinductive scaffolds with a spongiosa-inspired structure. Front. Bioeng. Biotechnol. 11, 1268049 (2023).
Hodges, N. A., Sussman, E. M. & Stegemann, J. P. Aseptic and septic prosthetic joint loosening: impact of biomaterial wear on immune cell function, inflammation, and infection. Biomaterials. 278, 121127 (2021).
Jamari, J. et al. Computational Contact Pressure Prediction of CoCrMo, SS 316L and Ti6Al4V Femoral Head against UHMWPE Acetabular Cup under Gait Cycle. J. Funct. Biomater. 13(2), 64 (2022).
Ammarullah, M. I. et al. Tresca Stress Simulation of Metal-on-Metal Total Hip Arthroplasty during Normal Walking Activity. Mater. (Basel) 14(24), 7554(2021).
P Sullivan, M. et al. Nanotechnology: current concepts in orthopaedic surgery and future directions. Bone Joint J. 96-b (5), 569–573 (2014).
Lu, X. et al. Multifunctional Coatings of Titanium implants toward promoting osseointegration and preventing infection: recent developments. Front. Bioeng. Biotechnol. 9, 783816 (2021).
Stucki, U. et al. Temporal and local appearance of alkaline phosphatase activity in early stages of guided bone regeneration. A descriptive histochemical study in humans. Clin. Oral Implants Res. 12 (2), 121–127 (2001).
Frank, O. et al. Real-time quantitative RT-PCR analysis of human bone marrow stromal cells during osteogenic differentiation in vitro. J. Cell. Biochem. 85 (4), 737–746 (2002).
Jamari, J. et al. In Silico Contact Pressure of Metal-on-Metal Total Hip Implant with Different Materials Subjected to Gait Loading. 12 (8),1241. (2022).
Acknowledgements
We gratefully acknowledge Jia-Lin Wang at Beijing National Innovation Institute of Lightweight LTD for supplying compounds and testing plates.
Funding
This research was funded by Beijing Science and Technology Planning Project (Grant No. Z181100001918028), the Jiangsu Province Science and technology Project (Grant No. BE2022760), and Peking University First Hospital Research Seed Fund (Grant No. 4805299).
Author information
Authors and Affiliations
Contributions
Conceptualization, Y-P.C. and W-J.R.; methodology, Y-P.C. and J.T.; software, H-B.W. and X-Y.C.; validation, Y-P.C., J.T. and Q-W.W.; formal analysis, J.T. and H-B.W.; investigation, H-B.W. and H.W.; resources, X-Y.C. and H.T.; data curation, Q-W.W. and B-X.Y.; writing—original draft preparation, J.T. and H-B.W.; writing—review and editing, Y-P.C. and X-T.B.; visualization, W-J.R. and H.W.; supervision, Y-P.C. and R-W.J.; project administration, Y-P.C., W-J.R. and H.T.; funding acquisition, Y-P.C. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Juma, T., Wang, H., Cao, X. et al. Novel biocompatible magnetron-sputtered silver coating for enhanced antibacterial properties and osteogenesis in vitro. Sci Rep 14, 28599 (2024). https://doi.org/10.1038/s41598-024-77270-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-77270-4