Abstract
This study aims to discover the association between serum osteocalcin, the Chinese visceral adiposity index (CVAI), and atherosclerotic cardiovascular disease (ASCVD) risk, and their impact on arterial stiffness in T2DM patients. We included 639 T2DM patients aged 30 and older who received the assessment of ASCVD risk using the China-PAR equation, Osteocalcin and arterial stiffness in this cross-sectional study. We found that osteocalcin and CVAI as independent risk factors for both medium–high-risk ASCVD (osteocalcin: men, OR,0.96, 95% CI 0.92, 1.00; women, OR, 0.93, 95% CI 0.8, 1.08, respectively)(CVAI: men, OR,1.01,95% CI 1.00,1.02; women: OR, 1.08, 95% CI 1.02,1.14, respectively) and arterial stiffness (osteocalcin: men, OR, 0.98, 95% CI 0.94,1.01; women, OR, 0.98, 95% CI 0.90,1.06, respectively)(CVAI: men, OR,1.0, 95% CI 0.99,1.01; women, OR, 1.02, 95% CI 1.00,1.04, respectively) in both men and women patients with T2DM. Combining osteocalcin levels and CVAI improved the prediction accuracy of arterial stiffness in men patients with T2DM (difference of AUC(Model 4 vs. Model 1):1.5%, NRI: 0.06 [0.0,0.4]). All P-values were < 0.05. The results suggested that osteocalcin levels and CVAI are independent risk factors for ASCVD risk and arterial stiffness in T2DM. Combining osteocalcin and CVAI can enhance the early detection of atherosclerosis through male patients with T2DM.
Similar content being viewed by others
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of morbidity and mortality in patients with type 2 diabetes mellitus (T2DM), and diabetes increases the risk of ASCVD greatly1. Arterial stiffness serves as an early sign and “accelerator” of atherosclerosis, the most important lesion of ASCVD, reflects the dysfunction of arterial endothelium as a clinical index, and is closely related to adverse cardiovascular outcomes2. Research shows that cardiovascular risk assessments using traditional risk factors are inadequate3. Furthermore, most assessment models of ASCVD risk are based on the general population and focus on predicting coronary heart disease and stroke, whereas initial diabetic manifestations of cardiovascular disease (CVD) are more likely to be peripheral artery disease and heart failure3,4. What’s more, the high cost and lack of reproducibility of detecting arterial stiffness are one of the reasons limiting its wide clinical application. Identifying additional risk factors that are consistent with the representative characteristics of T2DM may facilitate the accurate evaluation of ASCVD risk and improve the early identification of atherosclerosis in T2DM.
Osteocalcin (OC) and visceral obesity have recently received much attention for their important effects on the development of ASCVD, involving the regulation of glycolipid metabolism. Osteocalcin is the most abundant non-collagen protein in the extracellular bone matrix synthesized by osteoblasts. Recently, an increasing number of studies have found that osteocalcin regulates glucose and lipid metabolism, vascular calcification, and atherosclerotic formation5, thereby affecting the rate of CVD events and mortality. Similar to its major active form undercarboxylated osteocalcin (ucOC), serum osteocalcin influences the frequency of CVD events and mortality6. However, owing to the limitations of the existing detection technology for ucOC, clinical studies usually detect serum total osteocalcin levels.Very recently, a study involving serum osteocalcin and ASCVD risk in men aged 40 and over revealed an inverse relationship between osteocalcin and ASCVD risk7.
The incidence of obesity in patients with type 2 diabetes increases annually, and the prevalence of abdominal obesity alone can reach 45.4%8. Visceral fat accumulation has been linked to the advancement of cardiovascular complications in T2DM, as demonstrated by recent studies9. Asians generally accumulate more visceral fat but have a lower body mass index (BMI) than their Western counterparts8. The Chinese visceral adiposity index (CVAI), a reliable parameter for visceral fat area (VFA) in Chinese individuals, is the most reliable indicator of increased ASCVD risk in adults among various cardiovascular and metabolic indicators10.
Studies have verified that there are age and gender differences in osteocalcin, VFA and the cardiometabolic risk profile. While the underlying mechanisms for these differences are currently unclear11, the distinctions in osteocalcin based on age and gender are believed to arise from variations in bone turnover rates, with menopausal status being pivotal in explaining this disparity12. The correlation between osteocalcin levels, VFA, ASCVD risk, and arterial stiffness should be interpreted according to sex and age.
However, the correlation between osteocalcin and ASCVD risk and arterial stiffness in participants with T2DM remains unclear, the association between the CVAI and ASCVD risk in patients with T2DM needs to be clarified, and the capacity of the CVAI combined with osteocalcin levels to pinpoint arterial stiffness in individuals with T2DM has not been established. In this study, we aim to examine the association between serum osteocalcin levels, CVAI, ASCVD risk, and arterial stiffness in men and women with T2DM. The predictive accuracy of serum osteocalcin and the CVAI for arterial stiffness are also discussed.
It is worth mentioning that, we utilized a 10-year atherosclerotic cardiovascular Risk Assessment Equation (China-PAR) to evaluate the risk of ASCVD13. Developed from four large cohort study( InterASIA, China MUCA (1998), China MUCA (1992–1994) and CIMIC), this equation has been endorsed by the American College of Cardiology/American Heart Association guidelines14. The Chinese guidelines recommend it as a practical tool for ASCVD risk prediction that deserves to be widely used15. More recently, its effectiveness has also been demonstrated in Chinese individuals with T2D16.
Methods
Subjects
In this study, we conducted a retrospective analysis of data from patients with T2DM over 30 years old who were admitted to the Endocrinology Department of the First Hospital of Lanzhou University between August 2021 and September 2022. The diagnosis of T2DM was based on the 1999 criteria set by the World Health Organization (WHO). The exclusion criteria were as follows: (1) age < 30 years; (2) patients with incomplete data on high-density lipoprotein cholesterol (HDL-C), osteocalcin, ASCVD family history, age, systolic blood pressure (SBP), fasting blood glucose (FBG), BMI, WC, triglycerides(TG), and brachial-ankle pulse wave velocity (ba PWV); (3) combined with any known disease that affects skeletal metabolism exogenously, including benign and malignant tumors of the pituitary, parathyroid, and adrenal glands, as well as traumatic fractures, bone tuberculosis, hyperthyroidism, and hypothyroidism; (4) take any drugs that are known to affect bone metabolism, including thiazolidinedione and hormonal drugs, within 3 months12; and (5) pregnant and lactating women17. Finally, 639 participants with complete data were included. Upon admission, trained professionals completed questionnaires, physical examination, examination of the abdominal fat region, and arteriosclerosis for all participants, and blood samples were collected the next morning. The questionnaire included: (1) basic information: sex, age, and course of diabetes; (2) previous history of ASCVD, hypertension, and other diseases, and family history of ASCVD; (3) lifestyle: current smoking and current alcohol consumption; and (4) medication history. This study was conducted in accordance with the World Medical Association Declaration of Helsinki and was approved by the Ethics Committee of the First Hospital of Lanzhou University. All participants provided written informed consent.
Biochemical parameters
The patient fasted for a minimum of 8 h before venous blood was obtained. All blood samples were centrifuged within 2 h of collection and frozen at -20 °C after serum extraction. All biochemical indices were tested at our hospital’s endocrine laboratory or transported to the biochemical laboratory on dry ice within 2–4 h of collection.
Leukocyte counts were analyzed using a fully automatic blood cell analyzer (XFA6000; Plant, China). An automatic biochemical analyzer (AU5831, Beckman Coulter, USA) was used to detect total cholesterol (TC), serum creatinine, blood calcium (Ca), TG, blood phosphorus (P), HDL-C, ferritin (FT), low-density lipoprotein cholesterol (LDL-C), FBG, and uric acid (UA) levels. High-performance liquid-phase analysis (Bole-D10, Bio-Rad, USA) was used to detect hemoglobin (HbA1c). Vitamin D (Vit D) levels were analyzed using an enzyme-linked immunoassay (AU5831, Beckman Coulter, USA). Fasting insulin (FINS), 2 h insulin (2 h INS), fasting C-peptide (FCP) and 2 h c-peptide (2 h CP) levels were measured using chemiluminescence (Centaur-XP, Siemens, Germany). The detection of osteocalcin was accomplished using the Elecsys N-MID osteocalcin kit, utilizing electrochemical luminescence technology from Roche Diagnostics in China; the coefficient of variation within and between the measurements was 1.2–4.0% and 1.7–6.5%, respectively.
Anthropometric measurements and examination parameters
Participants’ height and weight were measured while they stood shoeless and wore light clothing. Waist circumference was measured at the mid-axillary line and midpoint between the lowest rib and the highest level of the ilium with a precision of 0.1. Automatic electronic equipment (HEM-752 FUZZY, Omron, China) was used to measure blood pressure in the non-dominant arm (units: mmHg). Participants were instructed to rest for 5 min prior to the blood pressure measurement. This procedure was repeated three times, with one-minute intervals between each reading, and the average of the three readings was calculated. The DUCALSCAN Bioimpedance technique (HDS-2000, Omron, China) measured the subcutaneous fat area (SFA) and visceral fat area (VFA). A color ultrasound diagnostic instrument (IU22; Philips, Holland) was used to detect fatty liver disease. Screening for diabetic retinopathy (DR) was performed using an aphakia binocular indirect ophthalmoscope (TRC-NW 400, Topcon, Japan).
Definition
Current smoking was defined as having smoked at least 100 cigarettes in the past and continuing to smoke currently. Current alcohol consumption was defined as the intake of more than 20 g per day for more than 3 months. Hypertension was defined as an SBP ≥ 140 mmHg, DBP ≥ 90 mmHg, or a self-reported diagnosis. TC ≥ 5.7 mmol/L, TG ≥ 1.8 mmol/L, LDL ≥ 3.7 mmol/L or HDL < 0.8 mmol/L was considered as dyslipidemia. The deficiency of diabetic retinopathy was indicated by fundus photographs without abnormalities. In contrast, the presence of diabetic retinopathy was determined by findings under a fundus microscope that displayed characteristics such as inner retinal microaneurysms, hemorrhages, venous beading, noticeable abnormal microvessels, neovascular formation, and changes like retinal hemorrhage or detachment. Diabetic kidney disease (DKD) was diagnosed as an urinary albumin/creatinine ratio > 30 mg/g or a glomerular filtration rate (eGFR) < 60 mL/min / 1.73 m2, excluding other causes other than diabetes. ASCVD includes acute coronary syndrome, myocardial infarction, stable or unstable angina pectoris, arterial revascularization, stroke, transient ischemic attack, and atherosclerotic peripheral vascular disease. Insulin resistance (HOME-IR) and insulin sensitivity (HOMA-β) according to homeostasis models were determined using the following formula: HOME-IR = FPG × FINS/22.5, HOMA-β = 20 × FINS/(FBG-3.5). The glomerular filtration rate was calculated according to the CG-GFR formula: eGFR = (140- age) × Body weight (kg) × 1.23/ serum creatinine (umol/L) (male), eGFR = (140- age) × Body weight (kg) × 1.08/ serum creatinine (umol/L) (female). BMI was calculated by the formula: weight/height2(kg/m2). The CVAI, triglyceride-glucose (TyG) index, and waist-height ratio (WHR) were calculated as follows:
CVAI
ASCVD risk
According to precedent18, individuals were categorized into a low ASCVD risk group based on a 10-year ASCVD risk of less than 5%, and into a medium–high risk group based on a 10-year ASCVD risk of 5% or greater.
Detection and evaluation criteria for arterial stiffness indicators
For the ba PWV measurement, subjects were required to rest for 5 min in the supine position. Cuff straps were placed around the subject’s arms and ankles, and both left and right brachial and ankle blood pressures were recorded. A volumetric splenogram (BP-203RPE II; Colin, Komaki, Japan) was used to record the pressure waves in the brachial artery.
Arterial stiffness was considered as baPWV ≥ 1600 cm/s. All the surgeries were performed by trained professionals. The measurements were repeated 3 times, and the average double-sided ba PWV values were recorded, and the ba PWV value was the upper value from the double side.
Statistical analysis
All steps are analyzed separately for women and men. Continuous variables with a normal distribution are presented as mean ± standard deviation, while those with skewed distributions are represented by the median and interquartile ranges. The t-test or Mann–Whitney U test was employed for group comparisons. Categorical variables are described using frequency and percentage, with chi-square tests used for between-group comparisons. Before linear regression analysis, the existence of a linear relationship was confirmed using a scatterplot of the two variables to be tested. The tolerance or variance inflation factor was used to diagnose collinearity. Tolerance ≥ 0.1 or variance inflation factor < 10 indicates no collinearity. Simple linear regression analysis was conducted using osteocalcin and CVAI as dependent variables to examine the correlation between general features, osteocalcin, and CVAI. Statistically significant variables were included in the multiple linear regression analysis. For the binary logistic regression analysis, the included variables were decided carefully according to clinical importance and multifactorial stepwise logistic regression. By building various models, the recognition ability of the variables was assessed using the receiver operating characteristic (ROC) curve and area under the curve (AUC). The differential recognition performances of the models were compared with those of the Delong test. When examining the correlation between different variables and 10-year ASCVD risk, the Crude Model only controls for the female menopausal status; Model 1 included traditional atherosclerosis risk factors: current smoking (male), menopausal status (female), hypertension, antihypertensive therapy, history of ASCVD, HDL, and osteocalcin or CVAI; Model 2 added osteocalcin and CVAI to the traditional atherosclerosis risk factors in Model 1; Model 3 added statin therapy, Ca, and HOMA-β to Model 1; Model 4 adds statin therapy, Ca, and HOMA-β to Model 2. SPSS software (version 26.0) was used for the statistical analysis. Differences were considered statistically significant when all P-values were double-tailed (P < 0.05).
Results
General characteristics of the participants
In total, 639 patients with T2DM were included in this study. The group consisted of 427 men and 212 women, with a mean age of 59.1 ± 9.5 years (ranging from 30 to 85 years old). Compared to the low-risk of ASCVD group, men with T2DM in the medium–high-risk of ASCVD group had higher age, diabetes duration, SBP, DBP level, hypertension, antihypertensive treatment, DR, and arterial stiffness incidence, lower weight, height, ferritin, TG, TyG index, Ca, eGFR, osteocalcin levels, and fatty liver incidence, as shown in Table 1. Meanwhile, women with T2DM in the medium–high-risk of ASCVD group had higher age, WC, BMI, FCP, CP-2, SFA, VFA, SBP, DBP, CVAI level, menopausal status, hypertension, antihypertensive therapy, and DR incidence, as shown in Table 2.
Furthermore, postmenopausal women exhibited higher levels of SBP, CP-2, Vitamin D, and CVAI, as well as incidence of a 10-year medium–high risk of ASCVD, statin use, DR, and arterial stiffness. In contrast, they showed lower estimated eGFR levels and incidence of fatty liver compared to premenopausal women, as indicated in Supplementary Table 1. Among women with T2DM at medium–high risk for ASCVD, the postmenopausal group had elevated levels of Vitamin D, creatinine, 10-year ASCVD risk, and incidence of arterial stiffness, while exhibiting lower BMI, SFA, and eGFR levels compared to the premenopausal group, as shown in Supplementary Table 2. All P values < 0.05.
Association between general characteristics and osteocalcin and CVAI
For men with T2DM, as shown in Tables 3 and 4, history of ASCVD, FIN, HOMA-β, and creatinine were positively associated with osteocalcin (standardized β, 0.1; standardized β, 1.1; standardized β, 0.3; standardized β, 0.2, respectively); HOME-IR, and CVAI were negatively associated with osteocalcin (standardized β, -0.8; standardized β, -0.1, respectively); WC, SBP, HOME-IR, CP-2, FIN, VFA, and TyG index were positively related to CVAI (standardized β, 1.3; standardized β, 0.04; standardized β, 0.08; standardized β, 0.04; standardized β, 0.09; standardized β, 0.02; standardized β, 0.1, respectively); DBP, FCP, HDL, uric acid, eGFR, and osteocalcin were negatively related to CVAI (standardized β, -0.04; standardized β, -0.04; standardized β, -0.1; standardized β, -0.02; standardized β, -0.09; standardized β, -0.02, respectively). For women with T2DM, creatinine had a positive correlation with osteocalcin (standardized β, 0.5), age were positively linked to CVAI (standardized β, 0.9). All P values < 0.05.
Association between osteocalcin and CVAI with ASCVD risk
Table 5 shows osteocalcin was significantly negatively related to the medium–high-risk of ASCVD in both male and female T2DM patients (men: standardized β, -0.08, P < 0.05; women: standardized β, -0.03, P < 0.05), respectively, and CVAI was significantly positively related to the medium–high-risk of ASCVD in both male and female T2DM patients (men: standardized β, 0.01, P < 0.05; women: standardized β, 0.25, P = 0) in linear regression analysis. For logistic regression analysis, after controlling for traditional cardiovascular risk factors in the Crude Model, Model 1, and Model 2, compared to the low-risk ASCVD group, osteocalcin was significantly negatively related to medium–high-risk of ASCVD in males with T2DM (OR, 0.97; 95% CI 0.94,1.00), and CVAI was significantly positively linked with medium–high risk of ASCVD in females with T2DM (OR, 1.05; 95% CI 1.02,1.08).
Beyond traditional cardiovascular risk factors, Model 3 additionally adjusted for non-traditional cardiovascular risk factors showed that osteocalcin and CVAI were significantly negatively and positively related to the medium–high risk of ASCVD in male and female patients with T2DM, respectively,compared to the low-risk ASCVD group.
Furthermore, in Model 4, which incorporated traditional and non-traditional cardiovascular risk factors, along with osteocalcin and CVAI, the results demonstrated that osteocalcin (men: OR,0.96, 95% CI 0.92, 1.00, P < 0.05; women: OR, 0.93, 95% CI 0.8, 1.08, P < 0.05) and CVAI (men: OR,1.01,95% CI 1.00,1.02, P < 0.05; women: OR, 1.08, 95% CI 1.02,1.14, P < 0.05) remained significantly negatively and positively related to the medium–high-risk of ASCVD in both male and female T2DM patients, when compared to the low-risk ASCVD group. Osteocalcin and CVAI are independent negative and positive risk factors for medium–high risk of ASCVD in both men and women with T2DM, respectively, even in patients with no prior history of cardiovascular disease, as shown in Supplementary Table 3.
Correlation between osteocalcin and CVAI with arterial stiffness
After controlling for confounding factors, we found a significant negative correlation between osteocalcin and arterial stiffness in male patients with T2DM (OR, 0.98, 95% CI 0.94,1.01, P < 0.05), and a significant positive link between CVAI and arterial stiffness (OR,1.0, 95% CI 0.99,1.01, P < 0.01). Osteocalcin and CVAI are independent risk factors for arterial stiffness in males with T2DM.
After controlling for confounding factors, such as menopausal status, HOMA-β, hypertension, creatinine, and eGFR, osteocalcin showed a significant negative correlation with arterial stiffness in female patients with T2DM(OR, 0.98, 95% CI 0.90,1.06, P < 0.05). Additionally, CVAI showed a significant positive correlation with arterial stiffness in female patients with T2DM (OR, 1.02, 95% CI 1.00,1.04, P < 0.05), as shown in Table 6. Osteocalcin levels and CVAI are independent risk factors for arterial stiffness in females with T2DM.
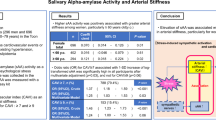
Four models were constructed, and the predictive values of osteocalcin and CVAI for arterial stiffness were assessed using ROC curves by comparing the AUCs. Model 4’s AUC was slightly higher than that of the other models (AUC(Model 4) = 82.4%, Calibrability(Model 4) = 0.8; Difference of AUC(Model 41 vs. Model 11) = 1.5%, P < 0.05), and the net weight classification improvement (NRI) of Model 4’s was also slightly higher than that of the Model 1’s (NRI(Model 41 vs. Model 11): 0.06 (0.0,0.4), P < 0.05) in male T2DM patients, as shown in Supplementary Table 4 and Fig. 1. This suggests that combining osteocalcin with CVAI maximizes the predictive accuracy of the model for identifying arterial stiffness in male T2DM patients. For females, Model 4’s AUC was notably elevated compared to the other models, while the difference being not statistically significant (Difference in AUC(Model 42vs. Model 12) = 3.9%), as shown in Supplementary Fig. 1.
Prediction value of osteocalcin and CVAI for arterial stiffness in men with T2DM. OC: osteocalcin; CVAI: China visceral adiposity index. Model 1: Controlling LDL, TG,hypertension, antihypertensive therapy, diabetes duration,eGFR, current smoking, leukocyte counts; Model 4: Model 1 + osteocalcin + CVAI.
Discussion
Increasing clinical evidence suggests that osteocalcin and CVAI are closely correlated with the occurrence and progression of cardiovascular disease, T2DM and its associated complications. Our study primarily examines the relationship between osteocalcin, CVAI, and ASCVD risk, emphasizing the predictive performance for arterial stiffness in the context of sex differences.
T2DM patients with long duration, poor glycemic control, visceral obesity, and normal renal function were the main subjects of this study. Men in the medium–high-risk of the ASCVD group had lower osteocalcin levels than those in the low-risk of ASCVD group, which is consistent with previous studies7. Compared to the low-risk ASCVD group, women in the medium–high-risk of ASCVD group had higher CVAI levels10. However, no significant difference was observed in CVAI levels among men across the two ASCVD risk categories. Similarly, there was no notable variation in osteocalcin levels among women across the ASCVD risk categories or between pre- and post-menopausal female T2DM patients, which contrasts with prior research12.
Osteocalcin and CVAI and glycolipid metabolism disorder in individuals with T2DM
Osteocalcin is a hormone with pleiotropic effects. An increasing number of studies have found that osteocalcin regulates glucose and lipid metabolism5, calcific atherosclerotic formation. It has been observed to negatively correlate with adverse outcomes in glucose metabolism19. In this study, we demonstrated a positive relationship between osteocalcin level and FIN, and HOMA-β, and a negative correlation between HOME-IR and osteocalcin levels in men individuals with T2DM, which is consistent with other studies20,21,22,23. Osteocalcin is involved in lipid metabolism, linked to fat distribution patterns24, and is closely related to visceral obesity in all obesity types25,26. This study indicated a negative association between osteocalcin and CVAI in male individuals with T2DM. Osteocalcin can also decrease inflammatory factor secretion from hyperglycemia and reduce inflammation through the PI3K/Akt/NF-kB signaling pathway27. Moreover, creatinine was positively correlated with osteocalcin levels in both male and female T2DM patients in this study. As the relationship between osteocalcin and skeletal muscle metabolism has been reported28,29, we speculate that the lower serum osteocalcin levels may reflect lower skeletal muscle quantity in male and female patients in our study.
Recently, the relationship between innovative indicators and the incidence of ASCVD and T2DM has shown improvement over traditional anthropometric indicators8,30. This has garnered increasing research interest and attention27. The CVAI can distinguish between excessive central obesity in Chinese adults and is the most powerful replacement marker for visceral fat dysfunction30. Previous studies have shown that visceral fat is closely associated with insulin resistance31. Vascular active substances, such as adipose cytokines, inflammatory factors, anticoagulant molecular markers, and growth factors, are secreted by visceral adipocytes, promoting the formation of atherosclerosis and increasing the risk of cardiovascular disease32. This study showed that DBP, FCP, HDL, uric acid, eGFR, and osteocalcin are negatively associated with CVAI in male T2DM patients, while WC, SBP, HOMA-IR, CP-2, FIN, VFA, and the TyG index are positively linked with CVAI. In women, age was positively associated with CVAI. After controlling for age and sex, Wei et al. demonstrated a close association between CVAI and a wide range of metabolic variable levels in healthy adults, which is consistent with our study33.
Association between osteocalcin and CVAI and ASCVD risk in individuals with T2DM
Low serum osteocalcin levels are associated with a higher occurrence of T2DM and its complications, as well as a higher rate of all-cause and cardiovascular death in T2DM34,35. The CVAI is the best obesity parameter for predicting the prevalence of diabetes and has the strongest relationship with the occurrence rate of CVD in T2DM8,36. Furthermore, CVAI has emerged as the most reliable indicator for increased ASCVD risk in adults among various innovative cardiovascular and metabolic indicators. This is supported by prior research that introduced markers such as the TyG index, VFA, and TyG-BMI8. This study is the first to investigate the association between osteocalcin level, CVAI, and ASCVD risk in T2DM patients. In this study, we found that in males with T2DM, a lower osteocalcin level is associated with a higher medium-to-high risk of ASCVD than in those with a low risk of ASCVD. CVAI was positively correlated with a medium–high risk of ASCVD in women with T2DM compared to those with a low risk of ASCVD. After adjusting for traditional and non-traditional cardiovascular risk factors, both osteocalcin levels and CVAI maintained their independent associations with medium–high ASCVD risk in male and female T2DM patients, in contrast to the low-risk ASCVD group. Specifically, osteocalcin in men and CVAI in women were identified as independent risk factors for ASCVD, though other factors might mask these relationships. When traditional and non-traditional cardiovascular risk factors, osteocalcin, and CVAI were all incorporated into the model, it was shown that, compared to the low risk of ASCVD, osteocalcin and CVAI were still negatively and positively related to the medium–high risk of ASCVD in both men and women with T2DM, respectively. This may explain the association of glycol-lipid metabolism between osteocalcin and CVAI and its contribution to the occurrence of ASCVD25. Interestingly, low levels of osteocalcin remained independently associated with CVD risk even after adjustment CVAI. In terms of mechanism, this may be related to the recent discovery that circulating OC + monocytes and vascular wall OC + smooth muscle cells participate in the formation of calcifying atherosclerotic lesions and directly affect the risk of cardiovascular events37,38. Previous study’s findings align with our research, their study investigated the relationship between osteocalcin and ASCVD risk in men aged over 40 years6. Similarly, Huang et al. revealed that CVAI is an independent risk factor for ASCVD in adults, which is consistent with our conclusion8.
Association between osteocalcin and CVAI and arterial stiffness in individuals with T2DM
To our knowledge, this study is the first to investigate the link between CVAI and arterial stiffness as well as the predictive ability of CVAI in patients with T2DM. In this study, the incidence of arterial stiffness in female patients with T2DM was positively associated with CVAI, meanwhile osteocalcin was negatively associated with the incidence of arterial stiffness in male T2DM patients. After controlling for confounding factors, osteocalcin level and CVAI were significantly negatively and positively related to the occurrence rate of arterial stiffness in male and female T2DM patients, respectively. Osteocalcin and CVAI offer enhanced predictive values for arterial stiffness in male and female patients with T2DM. Combining these values slightly improves the prediction accuracy for arterial stiffness incidence in males (AUC diff. (%) = 1.5%). However, the AUC in female patients with T2DM group notably increased (AUC diff. (%) = 3.9%), but the difference was not statistically significant. But findings from Kanazawa et al., Yun et al. and Tacey et al. are consistent with our conclusions39,40,41. The ongoing debate surrounding the correlation between osteocalcin and arterial stiffness in earlier studies42,43, can be attributed to variations in the impact of metabolic factors across different research. Disorders in glucose and lipid metabolism disorders, as well as hypertension, are closely associated with osteocalcin and the progression of atherosclerosis. In addition, confounding factors affecting the relationship between osteocalcin and arteriosclerosis can differ between men and women. Additionally, these studies included female populations of different ages, reflecting different bone turnover rates, since menopause is the watershed for their bone turnover changes12.
Osteocalcin and CVAI may be potential biomarkers of cardiovascular risk and offer a fresh understanding of how to reduce residual cardiovascular risk2. Moreover, osteocalcin can be obtained directly from the blood36, and CVAI is based on hematological indicators likely, as well as age, BMI, and WC. Considering that they are all able to objectively show changes in their levels at different stages of the disease, are universally available in all healthcare facilities (including primary healthcare facilities), and are inexpensive, osteocalcin and CVAI may be more favorable for improving ASCVD risk assessment and arterial stiffness predicting in patients with T2DM2.
In addition to regulating glucose and lipid metabolism and inflammatory responses, future research should focus on determining whether osteocalcin has a direct function in the blood vessel itself in terms of delaying the development of atherosclerosis and CVD42. Mechanically, repeated cyclic shear stress and intracavity pressure not only lead to increased vessel fibrosis and calcification, but also cause endothelial dysfunction40. In several recent studies, osteocalcin was shown to have a potential protective effect on vascular endothelial cells in atherosclerosis by regulating PI3K/Akt/ eNOS signaling. Similar studies have shown that addition of osteocalcin enhances human umbilical vein endothelial cell function in vitro43. However, a New Zealand white rabbit with 4-week diet-induced atherosclerosis underwent perfusion myography to detect carotid vascular activity. After the intervention of ucOC, this study showed that ucOC had no direct impact on the arterial endothelial function of the rabbit in the short term40. Therefore, the direct effects of osteocalcin on vascular function should be investigated in the future. A clear relationship between osteocalcin and early atherosclerosis is vital for improving the prevention and treatment of many ASCVDs.
This study has several limitations. Firstly, the cross-sectional design of the research precludes the establishment of a causal relationship among osteocalcin, CVAI, ASCVD risk, and arterial stiffness. Secondly, the relatively small sample size may have contributed to the slight overfitting observed in the male ASCVD risk model, as well as the inverse correlation between HOMA-β and male ASCVD risk (results not shown). Thirdly, the inflammatory index utilized in this study was limited to white leukocyte counts, omitting other relevant markers such as interleukin-6 and highly sensitive C-reactive protein. Lastly, the study’s participants were exclusively hospitalized patients. Compared to low-risk men, those categorized as having a medium to high risk of ASCVD were more likely to receive statin therapy, which may explain their lower TG levels. Consequently, potential selection biases may have influenced the findings of this study. Future research should involve well-designed multicenter prospective cohort studies to further elucidate the causal relationships among osteocalcin levels, CVAI, ASCVD risk, and arterial stiffness.
Conclusion
Osteocalcin and CVAI are independent risk factors for medium–high ASCVD risk and arterial stiffness in both men and women with type 2 diabetes mellitus, with osteocalcin being a negative factor and CVAI being a positive one. Combining the two indicators enhances the recognition of arterial stiffness in male T2DM patients. This will inject fresh blood into the stratification of ASCVD risk and management of early atherosclerosis in patients with type 2 diabetes.
Data availability
The data that support the findings of this study are not publicly available due to patient confidentiality concerns but are available from the corresponding authors upon reasonable request.
References
American Diabetes Association Professional Practice Committee. American Diabetes Association Professional Practice Committee 10 Cardiovascular disease and risk management: standards of medical care in diabetes-2022. Diabetes Care 45(Suppl 1):S144- S174 (2022).https://doi.org/10.2337/dc22-S010.
Tacey, A. et al. Potential role for osteocalcin in the development of atherosclerosis and blood vessel disease. Nutrients 10(10), 1426. https://doi.org/10.3390/nu10101426 (2018).
Pennells, L. et al. SCORE2-diabetes: 10-year cardiovascular risk estimation in type 2 diabetes in europe. Europ. Heart J. 44(28), 2544–2556. https://doi.org/10.1093/eurheartj/ehad260 (2023).
Dziopa, K., Asselbergs, F. W., Gratton, J., Chaturvedi, N. & Schmidt, A. F. Cardiovascular risk prediction in type 2 diabetes: A comparison of 22 risk scores in primary care settings. Diabetologia 65(4), 644–656. https://doi.org/10.1007/s00125-021-005640-y (2022).
Shen, Y. et al. Low total osteocalcin levels are associated with all-cause and cardiovascular mortality among patients with type 2 diabetes: a real-world study. Cardiovasc. Diabetol. 21(1), 98. https://doi.org/10.1186/s12933-022-01539-z (2022).
Liu, J. et al. Circulating osteocalcin is associated with time in range and other metrics assessed by continuous glucose monitoring in type 2 diabetes. Diabetol. Metab. Syndr. 14(1), 109. https://doi.org/10.1186/s13098-022-00863-4 (2022).
Yiting, X. et al. Osteocalcin value to identify subclinical atherosclerosis over atherosclerotic cardiovascular disease (ASCVD) risk score in middle-aged and elderly Chinese asymptomatic men. Clin. Chem. Lab. Med. 56(11), 1962–1969. https://doi.org/10.1515/cclm-2018-0320 (2018).
Yongcheng, R. et al. Dose-response association of Chinese visceral adiposity index with comorbidity of hypertension and diabetes mellitus among elderly people. Front Endocrinol. 14, 1187381 (2023).
Leon, B. M. & Maddox, T. M. Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World J. Diabetes 6(13), 1246–58. https://doi.org/10.4239/wjd.v6.i13.1246 (2015).
Wan, H. et al. Associations between abdominal obesity indices and diabetic complications: Chinese visceral adiposity index and neck circumference. Cardiovasc. Diabetol. 19(1), 118. https://doi.org/10.1186/s12933-020-01095-4 (2020).
Qiao, T. et al. Association between abdominal obesity indices and risk of cardiovascular 12 events in Chinese populations with type 2 diabetes: a prospective cohort study. Cardiovasc. Diabetol. 21(1), 225. https://doi.org/10.1186/s12933-022-01670-x (2022).
Maddaloni, E. et al. Association of osteocalcin, osteoprotegerin, and osteopontin with cardiovascular disease and retinopathy in type 2 diabetes. Diabetes. Metab. Res. Rev. 39(5), e3632. https://doi.org/10.1002/dmrr.3632 (2023).
Yang, X. et al. Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population. Circulation 134(19), 1430–1440. https://doi.org/10.1161/CIRCULATIONAHA.116.022367 (2016).
Arnett, D. K. et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation 140(11), e596–e646. https://doi.org/10.1161/CIR.0000000000000678 (2019).
Joint Task Force for Guideline on the Assessment and Management of Cardiovascular Risk in China. Guideline on the assessment and management of cardiovascular risk in China. Zhonghua Yu Fang Yi Xue Za Zhi 53(1), 13–35. https://doi.org/10.3760/cma.j.issn.0253-9624.2019.01.004 (2019).
Liang, J. et al. Validation and comparison of cardiovascular risk prediction equations in Chinese patients with Type 2 diabetes. Eur. J. Prev. Cardiol. 30(12), 1293–1303. https://doi.org/10.1093/eurjpc/zwad198 (2023).
Eastell, R. & Szulc, P. Use of bone turnover markers in postmenopausal osteoporosis. Lancet. Diabetes Endocrinol. 5(11), 908–923. https://doi.org/10.1016/S2213-8587(17)30184-5 (2017).
Yiting, X. et al. Contribution of low skeletal muscle mass in predicting cardiovascular events: A prospective cohort study. Eur. J. Int. Med. 114, 113–119. https://doi.org/10.1016/j.ejim.2023.05.007 (2023).
Kunutsor, S. K., Apekey, T. A. & Laukkanen, J. A. Association of serum total osteocalcin with type 2 diabetes and intermediate metabolic phenotypes: Systematic review and meta-analysis of observational evidence. Eur. J. Epidemiol. 30(8), 599–614. https://doi.org/10.1007/s10654-015-0058-x (2015).
Hussein, R. M. Biochemical relationships between bone turnover markers and blood glucose in patients with type 2 diabetes mellitus. Diabetes Metab. Syndr. 11(Supp11), S369–S372. https://doi.org/10.1016/j.dsx.2017.03.018 (2017).
Li, W. et al. Age- and sex-specific differences in the association of serum osteocalcin and cardiometabolic risk factors in type 2 diabetes. Diabetol. Metab. Syndr. 15(1), 48. https://doi.org/10.1186/s13098-023-01021-0 (2023).
Díaz-López, A. et al. Reduced serum concentrations of carboxylated and undercarboxylated osteocalcin are associated with risk of developing type 2 diabetes mellitus in a high cardiovascular risk population: A nested case-control study. J. Clin. Endocrinol. Metab. 98(11), 4524–4531. https://doi.org/10.1210/jc.2013-2472 (2013).
Iki, M. et al. Serum undercarboxylated osteocalcin levels are inversely associated with glycemic status and insulin resistance in an elderly Japanese male population: Fujiwara-kyo osteoporosis risk in men (Formen) study. Osteoporos. Int. 23(2), 761–770. https://doi.org/10.1007/s00198-011-1600-7 (2012).
Lin, X., Brennan-Speranza, T. C., Itamar, L. & Bu, B. Y. Undercarboxylated osteocalcin: Experimental and human evidence for a role in glucose homeostasis and muscle regulation of insulin sensitivity. Nutrients 10(7), 847. https://doi.org/10.3390/nu10070847 (2018).
Bao, Y. et al. Inverse relationship between serum osteocalcin levels and visceral fat area in chinese men. J. Clin. Endocrinol. Metab. 98(1), 345–51. https://doi.org/10.1210/jc.2012-2906 (2013).
Hassler, E. et al. Investigation of the relationship between the Mid_Thigh adipose tissue distribution measured by MRI and serum osteocalcin-a sex-based approach. Nutrients 14(1), 112. https://doi.org/10.3390/nu14010112 (2021).
Kanazawa, I., Tanaka, S. & Sugimoto, T. The association between osteocalcin and chronic inflammation in patients with type 2 diabetes mellitus. Calcif. Tissue Int. 103(6), 599–605. https://doi.org/10.1007/s00223-018-0460-y (2018).
Canaud, B. et al. Clinical and predictive value of simplified creatinine index used as muscle mass surrogate in end-stage kidney disease haemodialysis patients results from the international MONitoring dialysis outcome initiative. Nephrol. Dial. Transplant. 35(12), 2161–2171. https://doi.org/10.1093/ndt/gfaa098 (2020).
Chen, P.-Y. et al. Sex differences and positive dose-response relationships between serum osteocalcin levels and low muscle strength. Gerontology 69(9), 1056–1064. https://doi.org/10.1159/000531371 (2023).
Huang, Y.-C. et al. Comparison of innovative and traditional cardiometabolic indices in estimating atherosclerotic cardiovascular disease risk in adults. Diagnostics (Basel). 11(4), 603. https://doi.org/10.3390/diagnostics11040603 (2021).
Zheng, J. et al. Normal-weight visceral obesity promotes a higher 10-year atherosclerotic cardiovascular disease risk in patients with type 2 diabetes mellitus-a multicenter study in China. Cardiovasc. Diabetol. 22(1), 137. https://doi.org/10.1186/s12933-023-01876-7 (2023).
Lan, X. et al. Viscus fat area contributes to the Framingham 10-year general cardiovascular disease risk in patients with type 2 diabetes mellitus. Life Sci. 220, 69–75. https://doi.org/10.1016/j.lfs.2019.01.036 (2019).
Wei, J., Liu, X., Xue, H., Wang, Y. & Shi, Z. Comparisons of visceral adiposity index, body shape index, body mass index and waist circumference and their associations with diabetes mellitus in adults. Nutrients 11(7), 1580. https://doi.org/10.3390/nu11071580 (2019).
Guo, H. et al. Diabetes mellitus type 2 patients with abdominal obesity are prone to osteodysfunction: A cross-sectional study. J. Diabetes Res. 2023, 3872126. https://doi.org/10.1155/2023/3872126 (2023).
Si, S.-C. et al. Association of bone turnover biomarkers with severe intracranial and extracranial artery stenosis in type 2 diabetes mellitus patients. World J. Diabetes 14(5), 594–605. https://doi.org/10.4239/wjd.v14.i5.594 (2023).
Takashi, Y. & Kawanami, D. The role of bone-derived hormones in glucose metabolism, diabetic kidney disease, and cardiovascular disorders. Int J Mol Sci 23(4), 2376. https://doi.org/10.3390/ijms23042376 (2022).
Shahrour, H. E., Al Fahom, S., Al-Massarani, G., AlSaadi, A. R. & Magni, P. Osteocalcin-expressing endothelial progenitor cells and serum osteocalcin forms are independent biomarkers of coronary atherosclerotic disease severity in male and female patients. J. Endocrinol. Invest. 45(6), 1173–1180. https://doi.org/10.1007/s40618-022-01744-3 (2022).
Fadini, G. P. et al. Widespread increase in myeloid calcifying cells contributes to ectopic vascular calcification in type 2 diabetes. Circ. Res. 108(9), 1112–21. https://doi.org/10.1161/CIRCRESAHA.110.234088 (2011).
Yun, S.-H. et al. Low level of osteocalcin is related with arterial stiffness in korean adults: An inverse j-shaped relationship. J. Clin. Endocrinol. Metab. 101(1), 96–102. https://doi.org/10.1210/jc.2015-2847 (2016).
Alexander, T. et al. Undercarboxylated osteocalcin is associated with vascular function in female older adults but does not influence vascular function in male rabbit carotid artery ex vivo. PLoS One 15(11), e0242774. https://doi.org/10.1371/journal.pone.0242774 (2020).
Kanazawa, I. et al. Serum osteocalcin level is associated with glucose metabolism and atherosclerosis parameters in type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 94(1), 45–9. https://doi.org/10.1210/jc.2008-1455 (2009).
Tacey, A., Hayes, A., Zulli, A. & Levinger, I. Osteocalcin and vascular function: is there a cross-talk?. Mol Metab 49, 101205. https://doi.org/10.1016/j.molmet.2021.101205 (2021).
Yuqi, L. et al. Relationship between serum osteocalcin level and carotid intima-media thickness in a metabolically healthy Chinese population. Cardiovasc. Diabetol. 16(14), 82. https://doi.org/10.1186/s12933-015-0245-9 (2015).
Acknowledgements
Not applicable.
Funding
This study was funded by National Natural Science Foundation of China (No.82360161, and No.81960155), Health industry scientific research project of Gansu Province (No. GSWSKY-2019–07) and The Hospital Fund of the First Hospital of Lanzhou University (ldyyyn2020-01).
Author information
Authors and Affiliations
Contributions
C.G. designed and finished the first draft of the manuscript. C.C., Y.Z., Y.W., K.L., and X.L. devoted themselves to data collection. J.G., and P.Z. assisted C.G. to complete statistical analysis. All authors devoted themselves to previous manuscript versions commenting.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the First Hospital of Lanzhou University (Approval No.: LDYYLL-2023–400). All participants provided written informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gong, C., Chen, C., Zhao, Y. et al. Osteocalcin and Chinese visceral adiposity index are associated with the risk of ASCVD and arterial stiffness in patients with T2DM. Sci Rep 14, 26756 (2024). https://doi.org/10.1038/s41598-024-77620-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-77620-2