Abstract
In the current era of immune therapy, lenvatinib (LEN) continues to be vital for treating unresectable hepatocellular carcinoma (uHCC) patients. This study investigates the importance of nutritional status in the prognosis of uHCC patients receiving LEN and evaluates a new prognostic scoring system that combines the geriatric nutritional risk index (GNRI) and systemic inflammatory response. From 2018 to 2022, 484 uHCC patients treated with LEN (384 males, median age 73). Prognostic value was compared between GNRI and C-reactive protein (CRP) scoring (GNRI-C score), GNRI, and neo-Glasgow prognostic score (neo-GPS). Evaluation was based on the Akaike information criterion (AIC) and concordance index(c-index). Median progression-free survival (mPFS) was 9.3/6.8/4.6 months for GNRI no-risk/low-risk/moderate-to-major risk (p < 0.01, AIC 4742.4/c-index 0.585). Median overall survival (mOS) was 27.8/15.2/9.5 months (p < 0.01, AIC 3433.34/c-index 0.639). For GNRI-C score, mPFS was 10.8/7.1/5.6/4.0 months (score 0/1/2/3) (p < 0.01, AIC 4732.82/c-index 0.6), while neo-GPS showed mPFS of 8.5/5.1/5.2 months (p < 0.01, AIC 4745.89/c-index 0.562). For mOS, GNRI-C score demonstrated 28.6/20.0/10.1/8.4 months (score 0/1/2/3) (p < 0.01, AIC 3420.27/c-index 0.652), while neo-GPS indicated 21.0/12.4/4.5 months (p < 0.01, AIC 3468.84/c-index 0.564). The newly devised GNRI-C score, incorporating nutritional and inflammatory markers, could offer improved prognostic predictions for uHCC patients treated with LEN.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC) is the third leading cause of cancer death worldwide1. In Japan, sorafenib2 and lenvatinib (LEN)3, first-line multi-molecular target agents (MTAs), as well as regorafenib4, ramucirumab5, and cabozantinib6, later-line MTAs, have been approved for unresectable HCC (uHCC) cases. Moreover, atezolizumab plus bevacizumab (Atez/Bev)7 and durvalumab plus tremelimumab (Durva/Treme)8 have been developed as first-line immune-combined therapeutic agents. Patients treated with LEN have been reported to have a favorable therapeutic response, thus, this drug has an important role not only as first-line therapy for patients with autoimmune diseases or those who are not suitable for combined immunotherapy, such as pre-transplant patients9, but also as a late-line therapy with good outcomes after Atez/Bev failure10.
It is well known that better nutritional status is required for obtaining better prognosis from treatments for uHCC. Several indexes, nutritional assessment tools, and combinations of nutritional index and inflammatory status have been reported, including Onodera’s prognostic nutritional index (O-PNI)11, neutrophil-to-lymphocyte ratio (NLR)12, Glasgow prognostic score (GPS)13, and neo-GPS14. On the other hand, muscle volume loss has been reported as a negative prognostic factor in patients undergoing LEN treatment for uHCC15, and low body mass index (BMI) has been found to be associated with shorter treatment duration16, so assessment of nutritional status may be important in LEN therapy. Another study reported geriatric nutritional risk index (GNRI) score/grade, calculated using serum albumin level, present body weight, and ideal body weight, as a simple and accurate tool for predicting the risk of morbidity and mortality in elderly patients17. Subsequently, that index was shown useful not only for the elderly, but also for predicting postoperative survival in patients with HCC18 and also prognosis of patients treated with Atez/Bev19.
Since nutritional status and systemic inflammatory response may influence the prognosis of LEN treatment, the present study was conducted to examine the usefulness of GNRI, as well as a newly developed scoring system derived from combining GNRI and CRP, a measure of systemic inflammatory reaction, for predicting prognosis of patients undergoing LEN treatment for uHCC.
Materials and methods
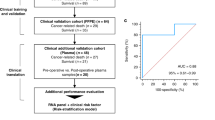
Patients
From April 2018 to December 2022, 756 patients underwent LEN treatment for uHCC at our affiliated hospitals. After excluding those with poor performance status or incomplete data, 484 uHCC patients were included.
Positive anti-HCV findings were considered to indicate that HCC was due to hepatitis C virus (HCV), whereas HCC due to hepatitis B virus (HBV) was determined when the HBV surface antigen was positive. For patients with a history of alcohol abuse (≥ 60 g/day), underlying liver disease was judged as related to alcohol.
Diagnosis of HCC and hepatic function assessment
HCC diagnosis was determined based on findings obtained with dynamic computed tomography (CT) and Gd-EOB-DTPA-enhanced magnetic resonance imaging (EOB-MRI)20. Tumor burden staging was evaluated using the Barcelona Clinic Liver Cancer (BCLC) staging system9.
Hepatic function assessment was based on Child–Pugh classification21, albumin-bilirubin (ALBI) grade22,23, and mALBI grade24, with the latter determined by dividing ALBI grade 2 into two sub-grades (mALBI 2a and 2b) using an ALBI score of − 2.27 as the cut-off value.
Treatment protocol
LEN dosage was determined according to patient body weight, with an initial oral dose of 12 mg/day for individuals weighing ≥ 60 kg and 8 mg/day for those weighing < 60 kg. Based on the attending physician’s judgment, the initial dose of LEN in some cases was reduced based on hepatic reserve function and general condition. LEN treatments were continued until diagnosis of progressive disease (PD), emergence of an unmanageable adverse event (AE), or upon patient request to halt the treatment. When there were unacceptable or severe AEs, the drug dosage was reduced, or treatment was suspended. Therapeutic response was evaluated according to the Response Evaluation Criteria in Solid Tumors (RECIST) guidelines, version 1.125, and AEs were assessed according to the National Cancer Institute Common Terminology Criteria for Adverse Events, version 5.026.
Definition and grouping of GNRI
GNRI score was calculated as follows: 1.489 × serum albumin (g/l) + 41.7 × present body weight (kg)/ideal body weight (kg)17. Ideal body weight was calculated as follows: for males, height (cm)-100-[height (cm)-150]/4; and for females, height (cm)-100-[height (cm)-150]/2.5. GNRI grade in a previous report was categorized into four groups: no-risk (score: > 98), low-risk (score: 92 to ≤ 98), moderate-risk (score: 82 to < 92), and major-risk (score: < 82)17, while in the present study, the patients were grouped into three GNRI grade groups: no-risk (score: > 98), low-risk (score: 92 to ≤ 98), and moderate-to-major-risk (score: < 92).
Scoring for assessment of prognosis of uHCC patients treated with LEN
A new scoring system was constructed using GNRI and CRP (GNRI plus CRP score: GNRI-C score), with the GNRI no-risk group receiving 0 points, the low-risk group 1 point, and the moderate-to-major risk group 2 points, with 1 point added when CRP was ≥ 1. A CRP score ≥ 1 was determined based on the cut-off value for CRP noted for GPS13 and neo-GPS14,27 systems. For comparing ability to predict prognosis [progression-free survival (PFS) and overall survival (OS)], GNRI, GNRI-C score, neo-GPS14,27, composed of modified albumin-bilirubin (mALBI) grade and c-reactive protein (CRP) as a systemic inflammatory reaction, O-PNI11, NLR12, and mALBI grade were used for analyses in the present study. Data presented in previous reports for cut-off values for O-PNI (> 40)11 and NLR (< 4)12 were also used.
Data collection
The prognosis was evaluated in a retrospective manner. Each of the enrolled patients provided written informed consent for treatment with LEN. The entire study protocol was approved by the Institutional Ethics Committee of our affiliated hospitals. The present study was conducted as a retrospective analysis of database records in accordance with the Guidelines for Clinical Research issued by the Ministry of Health and Welfare of Japan. All procedures adhered to the declaration of Helsinki.
Statistical analysis
In this retrospective analysis, power calculations were not performed prior to the study due to the observational nature of the design. However, the sample size was considered sufficient to observe differences in OS across the score stratifications based on previous studies and the available sample size in our dataset.
For this retrospective study, data were extracted from records stored in a database application. Qualitative variables were compared using Fisher’s exact test or a chi-squared test, and the results are presented as numbers with percentage. Quantitative values were compared using Student’s t-test or a Mann–Whitney U test, as appropriate, and are presented as median along with interquartile range (IQR). P values less than 0.05 were considered to indicate statistical significance. Multivariate Cox proportional hazards modeling analysis was conducted to evaluate factors associated with OS. For statistical analyses, the Kaplan–Meier method and log-rank test results were utilized. These methods were employed to evaluate PFS and OS following introduction of LEN. Patient background differences existed between those with and without GNRI risk. To improve the reliability of causal inference by balancing group characteristics and controlling for confounding factors, inverse probability weighting (IPW) was applied. This approach minimized uncorrectable bias by standardizing propensity scores across groups. Probabilities (propensity scores) for GNRI risk and no-risk groups were calculated using logistic regression analysis with covariates likely to impact OS. IPW weights were assigned as 1/(propensity score) for the no-risk group and 1/(1 − propensity score) for the GNRI risk group. Differences in OS was evaluated using an IPW‐adjusted log-rank test. Akaike information criterion (AIC) and concordance index (c-index) results were used for comparisons between both prognostic predictive scores. AIC was used to assess the usefulness of scores for progression-free survival and overall survival, while c-index was used to evaluate prognostic prediction.
All statistical analyses were performed using EZR, ver. 1.61 (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria), and a modified version of R commander designed to include statistical functions frequently used in biostatistics28.
Results
Patient characteristics
The median age of all patients was 73 years (IQR 67–78) and there were 384 males (79.3%). There were 107 patients with CRP ≥ 1 who had significantly worse BCLC stage (< 1 vs. ≥ 1: BCLC-0:A:B:C = 8:27:169:173 vs. 0:4:34:69, p = 0.005), worse median ALBI score (− 2.48 vs. − 2.10, p < 0.001), and higher median AST (38 vs. 47, p = 0.003) compared to the group with CRP < 1.The median follow-up period was 12.9 months (IQR 6.3–23.6). The patient characteristics for each GNRI group are shown in Table 1. Eastern Cooperative Oncology Group performance status was significantly worse with each increase in GNRI risk (p = 0.001). There was no significant difference in BCLC stage by GNRI group (p = 0.053). There was no significant difference in the number of patients who used LEN as first-line treatment across the groups (p = 0.637).
Therapeutic response, adverse events, and prognosis according to GNRI grade
Of the 484 enrolled patients, 421 were assessed as having best therapeutic response based on dynamic CT or EOB-MRI findings. As for best response according to GNRI grade, 14 were complete response, 100 were partial response, 83 were stable disease, and 35 were PD in the GNRI no-risk group, while those numbers were 3, 34, 25. and 14, respectively, in the GNRI low-risk group, and 10, 44, 42, and 17, respectively in the moderate-to-major risk group (p = 0.816). Values for objective response rate (ORR) and disease control rate (DCR) based on RECIST were 49.1% and 84.9%, respectively, in the no-risk group, 48.7% and 81.6%, respectively, in the low-risk group, and 47.8% and 85.0%, respectively, in the moderate-to-major-risk group (p = 0.982 and p = 0.745, respectively).
The frequency of AEs (any grade) was 84.1% (217/258) in the GNRI no-risk group, 86.8% (79/91) in the GNRI low-risk group, and 85.9% (116/135) in the GNRI moderate-to-major-risk group, with no significant differences between the groups (p = 0.785). The frequency of AEs (grade ≥ 3) was also not significantly different among the groups (34.9% vs. 34.1% vs. 41.5%, p = 0.374). AEs with an incidence of 10% or greater included anorexia (38.4%), fatigue (37.4%), hypertension (26.0%), hand-foot syndrome (25.4%), proteinuria (21.5%), thyroid dysfunction (19.8%), diarrhea (19.0%), hoarseness (13.4%), and liver damage (11.2%). A comparison of anorexia in patients with and without GNRI risk showed that 34.1% (88/258) in the GNRI no-risk and 40.7% (92/226) in the GNRI risk (low-risk and moderate-to-major-risk) groups had significantly decreased appetite when GNRI risk was present (p = 0.040). As for the frequency of other AEs in the GNRI no-risk and risk groups, there were no significant differences for fatigue (33.7% vs. 41.6%, p = 0.09), hypertension (29.5% vs. 22.1%, p = 0.078), hand-foot syndrome (28.3% vs. 22.1%, p = 0.143), proteinuria (22.9% vs. 19.9%, p = 0.44), thyroid dysfunction (22.5% vs. 16.8%, p = 0.138), diarrhea (19.8% vs. 18.1%, p = 0.728), hoarseness (12.8% vs. 14.2%, p = 0.69), or liver disorder (11.2% vs. 11.1%, p = 1.0).
Median PFS (mPFS) was 9.86 months (95% CI 7.82–11.86) for the GNRI no-risk, 7.04 months (95% CI 5.04–7.96) for the low-risk, and 4.54 months (95% CI 3.56–6.0) for the moderate-to-major-risk (p < 0.001) groups (Fig. 1a). Furthermore, median OS (mOS) for those groups was 28.21 months (95% CI 22.46–35.11), 16.18 months (95% CI 11.71–20.14), and 8.82 months (95% CI 8.21–11.54), respectively (p < 0.001) (Fig. 1b). Even for patients using LEN as first-line therapy, mPFS (8.82 months, 6.57 months and 5.64 months; p < 0.001) and mOS (33.21 months, 15.29 months and 10.14 months; p < 0.001) were significantly different among the GNRI no-risk, low-risk, and moderate-to-major-risk groups. After adjusting for the following factors related to OS (sex, age, BCLC stage, AFP, AST, ALT, PS) using IPW, the OS of the GNRI risk (low-risk and moderate-to-major-risk, mOS 12.4 months) and no-risk groups (mOS 28.1 months) was analyzed, and it was found that the OS in the GNRI no-risk group was significantly better (p < 0.001) (Supplementary Fig. 1).
Progression-free and overall survival of patients treated with lenvatinib (LEN) according to GNRI. (a) Median progression-free survival (PFS) for GNRI no-risk was 9.86 months (95% CI 7.82–11.86), for GNRI low-risk was 7.04 months (95% CI 5.04–7.96), and for GNRI moderate-to-major risk was 4.54 months (95% CI 3.56–6.0) (p < 0.001). (b) Median overall survival (mOS) for GNRI no-risk was 28.21 months (95% CI 22.46–35.11), for GNRI low-risk was 16.18 months (95% CI 11.71–20.14), and for GNRI moderate-to-major risk was 8.82 months (95% CI 8.21–11.54) (p < 0.001).
Therapeutic response, adverse events, and prognosis according to GNRI-C grade
A GNRI-C score of 0 was noted in 220, a score of 1 in 109, a score of 2 in 106, and a score of 3 in 49 patients. Multivariate analysis showed female [hazard ratio (HR) 1.403, 95% CI 1.034–1.903; p = 0.03], BCLC stage ≥ C (HR 1.4, 95% CI 1.091–1.797; p < 0.01), AFP level > 100 ng/mL (HR 1.424, 95% CI 1.114–1.820; p < 0.001), GNRI low-risk (HR 1.686, 95% CI 1.212–2.345; p < 0.01), GNRI moderate-to-major-risk (HR 2.469, 95% CI 1.866–3.268; p < 0.01), and CRP ≥ 1 ng/mL (HR 1.766, 95% CI 1.331–2.343; p < 0.01) to be associated with OS (Supplementary Table).
Values for ORR and DCR were 51.3% and 84.8%, respectively, in the GNRI-C score 0, 45.7% and 83.0%, respectively, in the GNRI-C score 1, 50.0% and 85.1%, respectively, in the GNRI-C score 2 and 38.9% and 83.3%, respectively, in GNRI-C score 3 (p = 0.517 and p = 0.963, respectively).
No significant differences regarding AEs according to GNRI-C score were observed (data not shown).
Median PFS was 10.79 months (95% CI 8.71–12.82) for a GINRI-C score of 0, 7.46 months (95% CI 5.89–7.96) for a score of 1, 5.75 months (95% CI 3.93–6.82) for a score of 2, and 3.68 months (95% CI 2.75–5.07) for a score of 3, with a significant difference indicated (p < 0.001) (Fig. 2a). Additionally, median OS was 28.61 months (95% CI 22.93–35.75) for a GINRIC score of 0, 19.64 months (95% CI 14.39–26.46) for a score of 1, 10.25 months (95% CI 8.54–14.89) for a score of 2, and 8.21 months (95% CI 4.76–10.21) for a score of 3, again with a significant difference found (p < 0.001) (Fig. 2b). Even for patients using LEN as first-line therapy, mPFS (9.86 months, 7.46 months, 6.43 months, and 4.25 months; p < 0.001) and mOS (34.57 months, 20.14 months, 10.75 months, and 8.21 months; p < 0.001) were significantly different among the GNRI-C score 0, 1, 2 and 3. The one- year cumulative survival rates for GNRI-C score 0, 1, 2 and 3 were 80%, 72%, 43% and 29%, respectively, while the 3-year survival rates were 41%, 30%, 15%, and 5%, respectively (each p < 0.001).
Progression-free and overall survival of patients treated with lenvatinib (LEN) according to GNRI-C score. (a) Median progression-free survival (PFS) for a GNRI-C score of 0, 1, 2, and 3 was 10.79 (95% CI 8.71–12.82), 7.46 (95% CI 5.89–7.96), 5.75 (95% CI 3.93–6.82), and 3.68 (95% CI 2.75–5.07) months, respectively (p < 0.001). (b) Median overall survival (mOS) for a GNRI-C score of 0, 1, 2, and 3 was 28.61 (95% CI 22.93–35.75), 19.64 (95% CI 14.39–26.46), 10.25 (95% CI 8.54–14.89), and 8.21 (95% CI 4.76–10.21) months, respectively (p < 0.001).
Progression-free and overall survival according to mALBI grade, NLR, O-PNI, neo-GPS
Based on mALBI grade, mPFS was 8.82 months (95% CI 7.57–11.75) for grade 1, 7.93 months (95% CI 6.0–10.21) for grade 2a, 5.64 months (95% CI 4.25–6.82) for grade 2b, and 2.16 months (95% CI 0.21–5.07) for grade 3 (p < 0.001) (Fig. 3a). Using NLR, mPFS was 7.75 months (95% CI 6.86–8.71) for NLR < 4 and 6.0 months (95% CI 3.57–7.5) for NLR ≥ 4 (p = 0.013) (Fig. 3b). O-PNI indicated mPFS of 4.32 months (95% CI 3.39–5.86) for a value ≤ 40 and 8.82 months (95% CI 7.75–10.75) for a value > 40 (p < 0.001) (Fig. 3c). As for neo-GPS, mPFS was 8.71 months (95% CI 7.57–10.0) for a score of 0, 5.07 months (95% CI 4.0–6.36) for a score of 1, and 3.38 months [95% CI 0.82-not applicable (NA)] for a score of 2 (p < 0.001) (Fig. 3d).
Progression-free survival of patients treated with lenvatinib (LEN). (a) Median progression-free survival (PFS) for mALBI grade 1, 2a, 2b, and 3 was 8.82 (95% CI 7.57–11.75), 7.93 (95% CI 6.0–10.21), 5.64 (95% CI 4.25–6.82), and 2.16 (95% CI 0.21–5.07) months, respectively (p < 0.001). (b) Median PFS for NLR < 4 was 7.75 (95% CI 6.86–8.71) and for NLR ≥ 4 was 6.0 (95% CI 3.57–7.5) months (p = 0.013). (c) Median PFS for O-PNI < 40 was 4.32 (95% CI 3.39–5.86) and for O-PNI ≥ 40 was 8.82 (95% CI 7.75–10.75) months (p < 0.001). (d) Median PFS neo-GPS 0, 1, and 2 was 8.71 (95% CI 7.57–10.0), 5.07 (95% CI 4.0–6.36), and 3.38 (95% CI 0.82-not applicable) months, respectively (p < 0.001).
Based on mALBI grade, mOS was 28.61 months (95% CI 23.86–35.36) for grade 1, 20.0 months (95% CI 15.21–24.32) for grade 2a, 12.39 months (95% CI 9.82–15.11) for grade 2b, and 4.68 months (95% CI 0.26–11.54) for grade 3 (p < 0.001) (Fig. 4a). Using NLR, mOS was 22.11 months (95% CI 18.64–27.21) for NLR < 4 and 10.46 months (95% CI 8.39–13.64) for NLR ≥ 4 (p < 0.001) (Fig. 4b). O-PNI indicated mOS of 9.61 months (95% CI 8.39–11.86) for a value ≤ 40 and 27.21 months (95% CI 22.46–30.86) for a value > 40 (p < 0.001) (Fig. 4c). As for neo-GPS, mOS was 22.89 months (95% CI 18.36–27.57) for a score of 0, 12.68 months (95% CI 9.82–18.14) for a score of 1, and 11.0 months (95% CI 4.46–NA) for a score of 2 (p < 0.001) (Fig. 4d).
Overall survival of patients treated with lenvatinib (LEN). (a) Median overall survival (OS) for mALBI grade 1, 2a, 2b, and 3 was 28.61 (95% CI 23.86–35.36), 20.0 (95% CI 15.21–24.32), 12.39 (95% CI 9.82–15.11), and 4.68 (95% CI 0.26–11.54) months, respectively (p < 0.001). (b) Median OS for NLR < 4 was 22.11 (95% CI 18.64–27.21) and for NLR ≥ 4 was 10.46 (95% CI 8.39–13.64) months (p < 0.001). (c) Median OS for O-PNI < 40 was 9.61 (95% CI 8.39–11.86) and for O-PNI ≥ 40 was 27.21 (95% CI 22.46–30.86) months (p < 0.001). (d) Median OS neo-GPS 0, 1, and 2 was 22.89 (95% CI 18.36–27.57), 12.68 (95% CI 9.82–18.14), and 11.0 (95% CI 4.46–not applicable) months, respectively (p < 0.001).
The effectiveness of each score in prognostic prediction using AIC and c-index
In PFS, AIC values for GNRI-C score, GNRI grade, mALBI grade, NLR, O-PNI, and neo-GPS were 4059.08, 4070.33, 4085.08, 4094.95, 4070.96, and 4073.57, respectively, while C-index values were 0.603, 0.589, 0.579, 0.531, 0.587, and 0.563, respectively. GNRI-C score displayed superior AIC and C-index outcomes when compared with the others (Table 2a).
In OS, AIC values for GNRI-C score, GNRI, mALBI grade, NLR, O-PNI, and neo-GPS were 2887.19, 2900.27, 2910.79, 2930.35, 2899.77, and 2933.26, respectively, while C-index values were 0.653, 0.64, 0.64, 0.57, 0.638, and 0.564, respectively. AIC and C-index results for GNRI-C score showed superiority for prediction of OS as well as for PFS as compared to the others (Table 2b).
Discussion
Results obtained in this multicenter study showed that PFS and OS for uHCC patients treated with LEN worsened as GNRI grade and also GNRI-C score became worse. The GNRI was initially proposed by Bouillanne as a means to predict the risk of death for hospitalized elderly patients17, with subsequent reports showing that worse GNRI grade indicated worse survival outcome for non-small cell lung cancer29, gastrointestinal malignancy30, and colorectal cancer31 cases. The usefulness of GNRI grade evaluation for prognosis prediction in patients undergoing treatment for HCC has also been reported in studies of hepatectomy18,32, transarterial chemoembolization33, LEN relability34, and Atez/Bev19. Findings obtained in the present investigation as well suggest that GNRI assessment for risk of nutritional disorder provides important clinical information for uHCC patients undergoing LEN treatment.
Recent studies have also examined the association between systemic inflammatory response and nutritional status for predicting cancer-specific outcomes, including HCC35,36 and GPS13, in which c-reactive protein (CRP) is included as a systemic inflammatory reaction factor, and neo-GPS14, in which mALBI grade is used instead of albumin, with those shown to be useful tools to predict prognosis of patients with uHCC undergoing treatement with a systemic therapy strategy. CRP is a simplified clinical biomarker of inflammatory responses that are synthesized in hepatocytes and used for acute phase substances affected by inflammatory cytokines such as IL-6, with rapid measurements obtained and low cost37. The present proposed GNRI-C score, a combination of GNRI and CRP, for systemic inflammatory response is also considered to be a simple and rapid calculation tool for determination of nutritional status. Indeed, based on the present results, GNRI-C score might be a better prognostic predictive tool for patients undergoing treatment with LEN.
A phase II study of LEN in patients with advanced HCC showed that the median body weight of those who withdrew from treatment or had their dose reduced early was lower than that of patients who did not withdraw or undergo dose reduction (54.1 vs. 67.6 kg)38. The initial dosage of LEN is 8 mg/day for patients weighing less than 60 kg and 12 mg/day for those greater than 60 kg. In a previous study, we found that BMI was lower in uHCC patients treated with LEN who presented anorexia (any grade) as an AE as compared with those who did not (20.3 ± 3.0 vs. 23.6 ± 4.0 kg/m2, p < 0.001)16. Thus, it is suggested that weight, one of the components of GNRI, is related to LEN tolerability. Another study found that the relative dose intensity during the initial four weeks of LEN therapy (≥ 70%) was associated with favorable radiological response and longer OS (hazard ratio 0.28, 95% CI 0.09–0.90, p = 0.03)39. In the present study, there was no significant difference in best response based on the RECIST guidelines associated with GNRI, though the GNRI risk-group had significantly greater appetite loss as an AE, and significantly worse PFS and OS as compared to the GNRI no-risk group. Other previous reports have indicated that appetite loss and fatigue are highly prevalent adverse events associated with LEN, ranging from 30 to 50% of treated patients, and such AEs or poor hepatic function often lead to LEN withdrawal or dose reduction40,41. Therefore, prediction of LEN tolerability in patients with uHCC before its introduction as well as preparations for early response to AEs are important for obtaining a favorable survival prognosis. GNRI and GNRI-C score, which can assess body weight and nutritional status related to tolerability prediction, are considered to be highly useful in clinical practice for the early prediction of AEs.
Although several studies have suggested that nutritional assessment is important for treatment of LEN, the large number of indicators makes it difficult to determine which is most useful. The present findings indicated that AIC and c-index of the GNRI-C score provided favorable results, namely, lowest AIC and highest c-index, among all indexes in terms of PFS (AIC = 4059.08, c-index = 0.603) and OS (AIC = 2887.19, c-index = 0.653). It is thus suggested that GNRI-C score may be more useful than other scoring systems for predicting prognosis of patients undergoing LEN therapy for uHCC.
In this study, Nutrition screening tools such as the Mini Nutritional Assessment42, Malnutrition Universal Screening Tool43, and Nutritional Risk Screening 200244 were not used. These tools require patients to assess their own rate of weight loss and food intake, which is considered difficult to evaluate objectively. On the other hand, GNRI-C has the advantage of being affordable and easy to quantify using only data, providing objective data. Additionally, GNRI-C does not take into account information such as sex, AFP values, and BCLC stage; it is a score based solely on the degree of variation in nutrition and inflammation that may fluctuate status. In the future, this score may not only serve to assess nutritional status but also become an indicator for introducing appropriate nutritional therapy to enable more efficient administration of LEN.
The present study has some limitations. First, though conducted as a multicenter study, it was performed in a retrospective manner. Second, large amounts of data related to LEN withdrawal and dose reduction during the clinical course of several of the enrolled patient were not available, and calculation of relative dose intensities could not be performed. Therefore, it was not possible to confirm whether there is a correlation between nutritional status and LEN weight loss. Third, muscle volume has not been assessed in all patients using baseline CT volume data to evaluate sarcopenia and frailty, and further objective data on nutritional status and physical balance has not been obtained. In the near future, it will be important to conduct large prospective studies that compensate for these missing values to confirm that GNRI grade and GNRI-C score are easy to use and effective clinical predictive prognostic assessment tools for patients undergoing LEN.
In conclusion, the present study demonstrated that GNRI-C score is a simple and easy-to-use tool, and useful for predicting prognosis of uHCC patients undergoing treatment with LEN. It may play an important clinical role in this immune-therapy era.
Data availability
Due to the nature of this research, the participants could not be contacted regarding whether the findings could be shared publicly, thus supporting data, including datasets generated and/or analyzed for the current study, are not publicly available. Further enquiries can be directed to the corresponding author.
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. https://doi.org/10.3322/caac.21660 (2021).
Llovet, J. M. et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 359, 378–390. https://doi.org/10.1056/NEJMoa0708857 (2008).
Kudo, M. et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet 391, 1163–1173. https://doi.org/10.1016/s0140-6736(18)30207-1 (2018).
Bruix, J. et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 389, 56–66. https://doi.org/10.1016/s0140-6736(16)32453-9 (2017).
Zhu, A. X. et al. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 20, 282–296. https://doi.org/10.1016/s1470-2045(18)30937-9 (2019).
Abou-Alfa, G. K. et al. Cabozantinib in patients with advanced and progressing hepatocellular carcinoma. N. Engl. J. Med. 379, 54–63. https://doi.org/10.1056/NEJMoa1717002 (2018).
Finn, R. S. et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N. Engl. J. Med. 382, 1894–1905. https://doi.org/10.1056/NEJMoa1915745 (2020).
Abou-Alfa, G. K. et al. Phase 3 randomized, open-label, multicenter study of tremelimumab (T) and durvalumab (D) as first-line therapy in patients (pts) with unresectable hepatocellular carcinoma (uHCC): HIMALAYA. J. Clin. Oncol. 40, 379–379. https://doi.org/10.1200/JCO.2022.40.4_suppl.379 (2022).
Reig, M. et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J. Hepatol. 76, 681–693. https://doi.org/10.1016/j.jhep.2021.11.018 (2022).
Hiraoka, A. et al. Lenvatinib as second-line treatment after atezolizumab plus bevacizumab for unresectable hepatocellular carcinoma-clinical results show importance of hepatic reserve function. Oncology https://doi.org/10.1159/000531316 (2023).
Hiraoka, A. et al. Nutritional index as prognostic indicator in patients receiving lenvatinib treatment for unresectable hepatocellular carcinoma. Oncology 98, 295–302. https://doi.org/10.1159/000506293 (2020).
Tada, T. et al. Neutrophil-to-lymphocyte ratio is associated with survival in patients with unresectable hepatocellular carcinoma treated with lenvatinib. Liver Int. 40, 968–976. https://doi.org/10.1111/liv.14405 (2020).
Tada, T. et al. Glasgow prognostic score predicts survival in patients with unresectable hepatocellular carcinoma treated with lenvatinib: a multicenter analysis. Eur. J. Gastroenterol. Hepatol. 34, 857–864. https://doi.org/10.1097/meg.0000000000002398 (2022).
Tada, T. et al. New prognostic system based on inflammation and liver function predicts prognosis in patients with advanced unresectable hepatocellular carcinoma treated with atezolizumab plus bevacizumab: A validation study. Cancer Med. 12, 6980–6993. https://doi.org/10.1002/cam4.5495 (2023).
Hiraoka, A. et al. Clinical importance of muscle volume in lenvatinib treatment for hepatocellular carcinoma: Analysis adjusted with inverse probability weighting. J. Gastroenterol. Hepatol. 36, 1812–1819. https://doi.org/10.1111/jgh.15336 (2021).
Hiraoka, A. et al. Prognostic factor of lenvatinib for unresectable hepatocellular carcinoma in real-world conditions-multicenter analysis. Cancer Med. 8, 3719–3728. https://doi.org/10.1002/cam4.2241 (2019).
Bouillanne, O. et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am. J. Clin. Nutr. 82, 777–783. https://doi.org/10.1093/ajcn/82.4.777 (2005).
Kanno, H. et al. Geriatric nutritional risk index predicts prognosis in hepatocellular carcinoma after hepatectomy: a propensity score matching analysis. Sci. Rep. 11, 9038. https://doi.org/10.1038/s41598-021-88254-z (2021).
Hiraoka, A. et al. Geriatric nutritional risk index as an easy-to-use assessment tool for nutritional status in hepatocellular carcinoma treated with atezolizumab plus bevacizumab. Hepatol. Res. https://doi.org/10.1111/hepr.13934 (2023).
Heimbach, J. K. et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 67, 358–380. https://doi.org/10.1002/hep.29086 (2018).
Pugh, R. N., Murray-Lyon, I. M., Dawson, J. L., Pietroni, M. C. & Williams, R. Transection of the oesophagus for bleeding oesophageal varices. Br. J. Surg. 60, 646–649. https://doi.org/10.1002/bjs.1800600817 (1973).
Johnson, P. J. et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J. Clin. Oncol. 33, 550–558. https://doi.org/10.1200/jco.2014.57.9151 (2015).
Hiraoka, A. et al. Usefulness of albumin-bilirubin grade for evaluation of prognosis of 2584 Japanese patients with hepatocellular carcinoma. J. Gastroenterol. Hepatol. 31, 1031–1036. https://doi.org/10.1111/jgh.13250 (2016).
Hiraoka, A. et al. Validation and potential of albumin-bilirubin grade and prognostication in a nationwide survey of 46,681 hepatocellular carcinoma patients in Japan: the need for a more detailed evaluation of hepatic function. Liver Cancer 6, 325–336. https://doi.org/10.1159/000479984 (2017).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer 45, 228–247. https://doi.org/10.1016/j.ejca.2008.10.026 (2009).
US Department of Health and Human Services, National Institutes of Health & Institute., N. C. Common Terminology Criteria for Adverse Events (CTCAE) Version 5. https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_50, https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_50.
Kaibori, M. et al. Comparison of the new neo-glasgow prognostic score based on the albumin-bilirubin grade with currently used nutritional indices for prognostic prediction following surgical resection of hepatocellular carcinoma: A multicenter retrospective study in Japan. Cancers (Basel) https://doi.org/10.3390/cancers14092091 (2022).
Kanda, Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 48, 452–458. https://doi.org/10.1038/bmt.2012.244 (2013).
Sonehara, K. et al. Prognostic value of the geriatric nutritional risk index among patients with previously treated advanced non-small cell lung cancer who subsequently underwent immunotherapy. Thorac. Cancer 12, 1366–1372. https://doi.org/10.1111/1759-7714.13909 (2021).
Xie, H., Tang, S., Wei, L. & Gan, J. Geriatric nutritional risk index as a predictor of complications and long-term outcomes in patients with gastrointestinal malignancy: a systematic review and meta-analysis. Cancer Cell Int. 20, 530. https://doi.org/10.1186/s12935-020-01628-7 (2020).
Sasaki, M. et al. The Geriatric Nutritional Risk Index predicts postoperative complications and prognosis in elderly patients with colorectal cancer after curative surgery. Sci. Rep. 10, 10744. https://doi.org/10.1038/s41598-020-67285-y (2020).
Li, L. et al. Geriatric nutritional risk index predicts prognosis after hepatectomy in elderly patients with hepatitis B virus-related hepatocellular carcinoma. Sci. Rep. 8, 12561. https://doi.org/10.1038/s41598-018-30906-8 (2018).
Si, Y., Xu, P., Xu, A., Wang, P. & Zhao, K. Geriatric nutritional risk index as a prognostic factor in patients with hepatocellular carcinoma following transarterial chemoembolization: A retrospective study. Medicine (Baltimore) 101, e32322. https://doi.org/10.1097/md.0000000000032322 (2022).
Kinoshita, A. et al. The geriatric nutritional risk index predicts tolerability of lenvatinib in patients with hepatocellular carcinoma. In Vivo 36, 865–873. https://doi.org/10.21873/invivo.12775 (2022).
Ishizuka, M. et al. Usefulness of a modified inflammation-based prognostic system for predicting postoperative mortality of patients undergoing surgery for primary hepatocellular carcinoma. J. Surg. Oncol. 103, 801–806. https://doi.org/10.1002/jso.21857 (2011).
Morimoto, M. et al. Inflammation-based prognostic score for hepatocellular carcinoma patients on sorafenib treatment. Anticancer Res. 32, 619–623 (2012).
Morris-Stiff, G., Gomez, D. & Prasad, K. R. C-reactive protein in liver cancer surgery. Eur. J. Surg. Oncol. 34, 727–729. https://doi.org/10.1016/j.ejso.2008.01.016 (2008).
Ikeda, K. et al. Phase 2 study of lenvatinib in patients with advanced hepatocellular carcinoma. J. Gastroenterol. 52, 512–519. https://doi.org/10.1007/s00535-016-1263-4 (2017).
Kirino, S. et al. Relative dose intensity over the first four weeks of lenvatinib therapy is a factor of favorable response and overall survival in patients with unresectable hepatocellular carcinoma. PLoS One 15, e0231828. https://doi.org/10.1371/journal.pone.0231828 (2020).
Hiraoka, A. et al. Clinical features of lenvatinib for unresectable hepatocellular carcinoma in real-world conditions: Multicenter analysis. Cancer Med. 8, 137–146. https://doi.org/10.1002/cam4.1909 (2019).
Tsuchiya, K. et al. The real-world data in Japanese patients with unresectable hepatocellular carcinoma treated with lenvatinib from a nationwide multicenter study. Cancers (Basel) https://doi.org/10.3390/cancers13112608 (2021).
Vellas, B. et al. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 15, 116–122. https://doi.org/10.1016/s0899-9007(98)00171-3 (1999).
Gomes-Neto, A. W. et al. Malnutrition universal screening tool and patient-generated subjective global assessment short form and their predictive validity in hospitalized patients. Clin. Nutr. ESPEN 45, 252–261. https://doi.org/10.1016/j.clnesp.2021.08.015 (2021).
Kondrup, J., Rasmussen, H. H., Hamberg, O. & Stanga, Z. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin. Nutr. 22, 321–336. https://doi.org/10.1016/s0261-5614(02)00214-5 (2003).
Funding
None of the authors received funding for this study that requires delcaration.
Author information
Authors and Affiliations
Contributions
H.O., A.H., and T.K. conceived the study, and H.O., A.H., H.O., and T.K. participated in its design and coordination. H.O., A.H., T.T., M.H., K.K., J.T., M.A., K.T., E.I., S.F., K.T., T.I., K.T., S.Y., H.T., C.O., T.N., T.H., S.K., N.S., K.K., A.N., H.K., T.M., H.K., Y.Y., H.N., H.S., F.T., K.N., A.M., A.T., T.N., N.I., T.O., T.A., M.I., Y.K., S.N., H.I., M.K., Y.H., and T.K. performed data curation. H.O., H.T., and T.K. performed statistical analyses and interpretation. H.O. and A.H. drafted the text. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Statement of ethics
The entire study protocol was approved by the Institutional Ethics Committee of Ehime Prefectural Central Hospital (No.2022-46). After receiving official approval, this study was conducted as a retrospective analysis of database records based on the Guidelines for Clinical Research issued by the Ministry of Health and Welfare of Japan. All procedures were done in accordance with the declaration of Helsinki. The data were made anonymous before analysis to protect patient privacy. Written informed consent was obtained from all patients before treatment and this study received ethical approval for use of an opt-out methodology based on low risk to the participants.
Competing interests
Atsushi Hiraoka, MD, PhD: lecture fees; AstraZeneca, Bayer, and Eli Lilly. Takashi Kumada, MD, PhD: lecture fees; Eisai. Toshifumi Tada, MD, PhD: Abbvie and Eisai. Takeshi Hatanaka, MD, PhD: Eisai. None of the other authors have potential conflicts of interest to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ohama, H., Hiraoka, A., Tada, T. et al. Geriatric nutritional risk index and newly developed scoring system as prognosis prediction for unresectable hepatocellular carcinoma patients treated with lenvatinib. Sci Rep 15, 72 (2025). https://doi.org/10.1038/s41598-024-78539-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-78539-4
Keywords
This article is cited by
-
Prognostic nutrition index reveals LAG3 in cytotoxic CD8+ T cells and MHC class II in gastric cancer cells
Cancer Immunology, Immunotherapy (2025)