Abstract
Objective
This study aimed to examine the levels of physical activity (PA), sleep, and mental health (MH), specifically depression, anxiety, and stress, among Chinese university students. It also aimed to analyze the influencing factors of MH, providing a theoretical foundation for developing intervention programs to improve college students’ mental health.
Methods
A stratified, clustered, and phased sampling method was employed. In September 2022, a survey was conducted among 36,756 university students from 104 higher education institutions across 31 provinces, autonomous regions, and municipalities in China. The participants’ PA behaviors, sleep patterns, depressive symptoms (use the CES-D), anxiety symptoms (use the GAD-7), smoking and drinking behaviors, and demographic information were assessed through an online questionnaire using Questionnaire Star software.
Results
A total of 30,475 valid questionnaires were completed. The proportion of university students engaging in light-intensity PA was 77.6%. The prevalence of insufficient sleep was 39.5%, whereas the prevalence of poor sleep quality was 16.7%. The prevalence of depressive symptoms was 10%, and the prevalence of anxiety symptoms was 23.3%. Binary logistic regression analysis revealed that engaging in moderate to high-intensity PA and having sufficient and high-quality sleep were associated with a lower likelihood of depressive symptoms (OR = 0.207–0.800, P < 0.01), whereas appropriate sleep duration and higher sleep quality were associated with a lower likelihood of anxiety symptoms (OR = 0.134–0.827, P < 0.001).
Conclusion
The intensity of PA among university students is predominantly light, and the reported rate of insufficient sleep is relatively high. Moderate to high-intensity PA and sufficient high-quality sleep may alleviate MH issues among college students, with an interaction effect observed among PA, sleep, and depression symptoms. Future studies should further explore targeted interventions combining PA and sleep behaviors to enhance the MH of university students.
Similar content being viewed by others
Introduction
In recent years, the prevalence of mental health (MH) disorders, represented by depression and anxiety, has been rising sharply worldwide1,2. Particularly, university students are in a transitional stage from adolescence to adulthood; moreover, MH problems among Chinese university students have become increasingly common because of COVID-19 control measures and their own negative cognition3,4,5. In April 2023, the Chinese Ministry of Education and other 17 departments issued the Special Action Plan for Comprehensive Strengthening and Improvement of Student Mental Health Work in the New Era (2023–2025). It places student MH work in a more prominent position, strengthens MH monitoring, conducts MH assessments, and comprehensively strengthens and improves student MH work in the modern context. In summary, promoting students’ MH is a key focus of student work in the new era. Depression and anxiety are the most common MH issues among university students6. These mental disorders increase the risks of cardiovascular diseases and all-cause mortality and are important influencing factors of global disability-adjusted life years and disease burden7. The latest research data from a study involving over 1.4 million people show that being diagnosed with depression at any age is associated with a doubled to tripled risk of dementia8. Therefore, intervention measures targeting the risk factors for depression and anxiety should be considered to enhance the MH level of Chinese university students.
Regular engagement in physical activity (PA) is a key protective factor for the prevention and management of noncommunicable diseases. Regular PA is also beneficial for MH, including preventing symptoms of cognitive decline, depression, and anxiety9. Existing studies have shown that insufficient PA is independently associated with an increased risk of depression and anxiety10. However, 27.5% of adults do not meet the PA levels recommended by the World Health Organization (WHO) in 201011, and little improvement has been observed over the past decade9. In addition to PA, sleep is also an important factor affecting the MH of university students12,13. Research has found that short-term sleep deprivation reduces efficiency in learning, weakens cognitive functioning, and prolongs reaction time14,15. Long-term sleep deprivation and poor sleep quality are strong risk factors for obesity, diabetes, and peripheral arterial diseases16,17,18. Existing studies have shown that insufficient PA, inadequate sleep, and poor sleep quality are independently associated with an increased risk of depression and anxiety10,19,20,21. However, few studies have comprehensively explored the combination of these risk factors.
The relationship between exercise and health promotion has rapidly developed, especially in the field of promoting physical health and MH from a behavioral change perspective, which has received considerable attention from scholars22. However, inconsistency is observed in the topics of focus, paradigms, and methods employed by scholars. Uncertain, inconsistent, and even contradictory research findings still exist23. Furthermore, although studies on PA, sleep, and MH among university students have been conducted, large-scale epidemiological data remain lacking.
Therefore, this study aims to analyze the levels of PA, sleep, and MH among Chinese university students through an epidemiological survey approach. The main objectives are as follows: (1) Provide foundational data for health behavior research among Chinese university students, focusing on PA and sleep levels through a large-scale epidemiological survey; (2) Investigate the prevalence of MH issues among students using paper-based assessments, supporting MH promotion and intervention programs (3) Examine the associations between PA, sleep patterns, and MH statistically, offering theoretical support for intervention strategies based on behavioral changes.
Methods
Participants
The study primarily utilized an epidemiological survey method. A total of 36,756 university students from 104 universities in 31 provinces, autonomous regions, and municipalities across China were surveyed. The survey targeted regular university students in Mainland China and referred to the list of regular institutions of higher learning provided by the Chinese Ministry of Education (“National List of Regular Institutions of Higher Learning as of September 30, 2021”). This included undergraduate students and junior university students, excluding graduate students (Master’s and Ph.D. programs). In view of the ongoing COVID-19 pandemic during the survey period, the selection of participants was limited to those who had already returned to campus.
The study employed a stratified, cluster, and staged sampling method to select the survey participants. For more information on the sampling process, please refer to our team’s published literature24,25.
Stratification and sample size
The sample population was divided into two primary groups based on gender (male and female) and further stratified into eight categories according to grade level. Each category required a minimum sample size of 45 individuals. The total sample size per province (or autonomous region or municipality) was set at 1,080 participants, aiming for a national total of 33,480 participants. The questionnaire was administered electronically using the Questionnaire Star platform in late September 2022, ultimately collecting 36,756 responses.
Measures
The survey collected sociodemographic data, health behavior information (smoking and drinking), and responses to standardized scales. The average time to complete the survey was 6 min and 12 s. To ensure data quality, well-established scales tested among Chinese university students were used, along with normative data specific to this population.
Sociodemographic information
Sociodemographic information included gender, grade level, age, school, and school ___location (postal code). The school locations were classified into eastern, central, and western regions based on the geographical division of China26.
Assessment of physical activity
The International Physical Activity Questionnaire (IPAQ)-Short Form was used to measure the PA levels of university students27. Based on scoring guidelines, PA was categorized into three intensities: vigorous (VPA), moderate (MPA), and light (LPA)28. The IPAQ has demonstrated strong reliability and validity in the Chinese population29,30. Qu’s study reported over 70% consistency between the questionnaire and recorded PA levels, with test-retest correlations ranging from 0.626 to 0.88728. Xu’s study further showed a correlation of 0.543 between the IPAQ and accelerometer-measured PA, supporting its overall accuracy. VPA, MPA, and LPA were classified based on IPAQ recommendations31.
PA levels were classified according to the IPAQ working group’s recommendations as follows. VPA is defined as at least 3 days of high-intensity activity, totaling at least 1500 MET-min/week, or a combination of three intensities over 7 days, with a total of at least 3000 MET-min/week. MPA involves at least 20 min of high-intensity activity on 3 days or at least 30 min of moderate/walking activity on 5 days, or a combination of three intensities totaling at least 600 MET-min/week over 5 days. LPA refers to no activity or failure to meet the moderate or high-intensity criteria28,30.
Sleep
The Pittsburgh Sleep Quality Index (PSQI) was used to assess sleep quality among university students, with scores ranging from 0 to 21, where higher scores indicate poorer sleep quality. Liu et al. found the PSQI reliable for Chinese university students, reporting a Cronbach’s alpha of 0.842 across its 7 components, with correlation coefficients between components and the total score ranging from 0.631 to 0.81032. The split-half reliability was 0.866, and test-retest reliability was 0.809. Exploratory factor analysis revealed a single factor with strong factor loadings (> 0.5). In this study, the PSQI’s Cronbach’s alpha was 0.819.
Based on the PSQI scores, sleep quality among university students was categorized as “good” (combining “very good” and “fairly good,” total score ≤ 8), “average” (9 ≤ total score < 16), or “poor” (total score ≥ 17). Sleep duration was defined based on the Joint Consensus Statement of the American Academy of Sleep Medicine and the Sleep Research Society published in 2015 for adult individuals33. sleep duration of < 7 h was considered “insufficient,” 7–9 h as “adequate,” and ≥ 9 h as “excessive” for young adults aged 18–25.
Mental health
On the basis of the methods used in the Blue Book of Mental Health: Report on the Development of Mental Health in the Chinese Population (2019–2020), two indicators, namely, depression and anxiety, were selected to reflect the MH status of university students34.
The Center for Epidemiological Studies Depression Scale (CES-D), which is widely employed internationally for screening depressive symptoms in the general population, was utilized for depression screening35. The scale requires respondents to rate the frequency of symptoms occurring in the past week on a scale ranging from 0 to 3. A cutoff score of 10 and a high-risk cutoff score of 17 were established35. He et al. found the CES-D reliable and valid among 30,801 individuals, with Cronbach’s alpha ranging from 0.85 to 0.88 and item correlations above 0.5. In this study, Cronbach’s alpha was 0.822 for positive items and 0.859 for reverse items36.
The Generalized Anxiety Disorder-7 (GAD-7) scale was used to assess the level of anxiety in the general population37. The scale requires respondents to rate the frequency of anxiety symptoms experienced in the past two weeks on a scale ranging from 0 to 3. The scoring algorithm involves summing the scores of 7 items, resulting in a total score ranging from 0 to 21. Scores of 0–4 represent no anxiety, 5–9 represent mild anxiety, 10–14 represent moderate anxiety, and 15–21 represent severe anxiety34. Fu et al. validated the GAD-7 with a reliability coefficient of 0.901 among Chinese university students. In this study, GAD-7 had a Cronbach’s alpha of 0.781. Depression and anxiety levels were categorized as “normal,” “low risk,” and “high risk,” with mild and moderate GAD-7 scores grouped as low risk38.
In this study, the classification of depression and anxiety symptom levels was divided into three categories: “normal,” “low risk,” and “high risk.” Specifically, the categories of “mild” and “moderate” in GAD-7 were combined and classified as low risk. In the binary logistic regression analysis, high risk was defined as the “detection” outcome.
Health behaviors
Smoking behavior was categorized into three groups: “never smoked,” “occasional smoking,” and “regular smoking,” following the definitions provided by the WHO for smoking-related terminology.
Alcohol consumption behavior was classified into three groups: “never consumed alcohol,” “previously consumed alcohol but never been intoxicated, and “previously experienced intoxication,” based on the number of days of alcohol consumption and the number of days of intoxication in the past month. This categorization followed the guidelines set by the Youth Risk Behavior Surveillance System questionnaire used in the United States.
Data analysis
Data processing was performed using SPSS 25.0 and Excel software. First, data preprocessing involved selecting valid questionnaires according to specific criteria for valid data.
Chi square tests were conducted to analyze the differences of each variable in demographic factors and health behaviors. Cramer’s V coefficient (V coefficient) was used as an effect size measure in the analysis of differences. V coefficients between 0.1 and 0.3 indicated the presence of differences with a small effect size (small), V coefficients between 0.3 and 0.5 represent the presence of differences with a medium effect size (medium), and V > 0.5 indicates the presence of differences with a large effect size39.
Binary logistic regression analysis was employed to examine the odds ratio (OR) of developing MH issues under exposure to PA and sleep factors. The analysis controlled for sociodemographic variables, such as gender, grade, age, school, and ___location, as well as health behavior variables including smoking and alcohol consumption. The OR represents how many times more likely an outcome is for the exposed group compared with the unexposed group. OR > 1 indicates that the variable’s risk is increased due to exposure, implying a positive association between exposure and the variable. OR < 1 indicates that the variable’s risk is decreased due to exposure, implying a negative association between exposure and the variable. Furthermore, confidence intervals should be calculated for the OR, and if the interval spans 1, then it generally suggests that the factor is inignificant40.
Quality control
Standardization of research protocol and questionnaire administration: Special training was provided to the investigators prior to the formal survey. Standardized instructions and guidelines were developed to ensure consistency in introducing the study and providing instructions for questionnaire completion. The investigators involved in the survey were student counselors or teachers.
Data cleaning rules: Data cleaning was conducted to ensure external validity of the analyzed data. In the data preprocessing stage, logical errors, omissions, inaccuracies, and indiscernible responses were identified and either retested or excluded to ensure data accuracy and validity. The following rules were applied for inclusion of valid questionnaires (1) Questionnaires with unidentifiable school full names were deleted, resulting in 298 exclusions. (2) Questionnaires with ages below 15 or above 30 were deleted, resulting in 490 exclusions. (3) Questionnaires with codes indicating complete consistency for at least 21 consecutive entries were deleted, resulting in 1,911 exclusions. (4) Following the data cleaning and outlier exclusion principles of the IPAQ30, 195 questionnaires were excluded. (5) The average time for questionnaire completion was 6 min and 12 s. Questionnaires with completion times falling within (0, 5%] and (95%, 100%] were excluded. Finally, a total of 30,475 valid questionnaires were included in the analysis.
Strict adherence to statistical data processing requirements was followed. Corresponding statistical methods were applied for different data categories. Prior to conducting binary logistic regression analysis, parallelism tests were performed to verify the absence of multicollinearity among independent variables and the absence of significant outliers.
Common method bias testing was conducted before data analysis. Harman’s single-factor test was employed to examine common method bias. Five items with eigenvalues greater than 1 were identified, and the variance explained by the first factor was 28.780%, which was below the critical value of 40%41. This indicates the absence of significant common method bias.
Results
A total of 30,475 valid questionnaires were obtained in this survey. The response rate was highest in the central region and relatively lower in the western region. Overall, the response rate complied with the sampling requirements.
Status of PA and sleep quality of Chinese university students
Table 1 provides an overview of PA levels and sleep conditions among university students. Most university students exhibited low PA levels, accounting for 77.6%. Differences were observed based on gender (V = 0.311), smoking behavior (V = 0.168), and alcohol consumption behavior (V = 0.171). Specifically, the report rate of low PA was higher among females (87.9%) compared with males (62.6%). Among nonsmokers, the highest reported rate of low PA was 79.4%. Among nondrinkers, the highest reported rate of low PA was 50.3%.
The overall reported rate of insufficient sleep among university students was 39.5%. Differences were found among students from different school locations (V = 0.127). Specifically, the highest reported rate of insufficient sleep was among students in eastern region schools (47.7%), whereas the lowest reported rate was among students in central region schools (34.0%).
The overall reported ratio of poor sleep quality among university students was 16.7, with differences observed in terms of academic year (V = 0.175) and alcohol consumption behavior (V = 0.106). Specifically, fourth-year students had the highest rate of reporting poor sleep quality (19.3%). Among students who had experienced drunkenness, the highest rate of reporting poor sleep quality was observed (29.7%).
MH detection rate among Chinese university students
Table 2 provides an overview of the detection of depressive and anxiety symptoms among university students. Overall, the proportion of university students at high risk for depressive symptoms was 10%, whereas the proportion at high risk for anxiety symptoms was 23.3%. In terms of gender differences, males had a higher proportion of high-risk depressive symptoms (14.9%, V = 0.136) and high-risk anxiety symptoms (28.3%, V = 0.109) compared with females. Regarding differences across academic years, significant differences were observed in the detection of depressive (V = 0.108) and anxiety (V = 0.106) symptoms among students at different academic levels. Moreover, an increasing trend was observed in the detection of high-risk symptoms with higher academic years.
School ___location did not show significant differences in the detection of depressive and anxiety symptoms among university students. In terms of smoking behavior, differences existed in the detection of depressive symptoms among university students with different smoking behaviors. Specifically, frequent smokers had the highest proportion of high-risk depressive symptoms (22.9%, V = 0.185). In terms of alcohol consumption behavior, differences were observed in the detection of anxiety symptoms among university students with different drinking behaviors. Specifically, those who had experienced drunkenness had the highest proportion of high-risk anxiety symptoms (39.2%, V = 0.186).
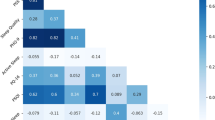
Association among PA, sleep, and MH among university students
Table 3 provides an overview of the correlation analysis among PA, sleep, and MH among university students. In the binary logistic regression analysis with depressive symptoms as the dependent variable, compared with LPA, MPA (OR = 0.596, 95% CI: 0.519–0.683, P < 0.001) and VPA (OR = 0.697, 95% CI: 0.588–0.824, P = 0.003) were protective factors against depression.
In comparison with insufficient sleep duration, appropriate (OR = 0.652, 95% CI: 0.570–0.744, P < 0.001) and excessive (OR = 0.800, 95% CI: 0.702–0.911, P < 0.001) sleep durations were protective factors against depression. In comparison with poor sleep quality, fair (OR = 0.232, 95% CI: 0.212–0.254, P < 0.001) and good (OR = 0.207, 95% CI: 0.187–0.228, P < 0.001) sleep qualities were also protective factors against depression. When PA, sleep duration, and sleep quality were simultaneously included in the regression analysis (Model 4), the protective effects of all the three variables slightly increased, indicating the presence of an interaction effect between sleep and PA.
In the binary logistic regression analysis with anxiety symptoms as the dependent variable, PA did not have a statistically significant effect on the detection of anxiety. In comparison with insufficient sleep duration, appropriate sleep duration (OR = 0.827, 95% CI: 0.758–0.902, P < 0.001) was a protective factor against anxiety. Compared with poor sleep quality, fair (OR = 0.134, 95% CI: 0.125–0.144, P < 0.001) and good (OR = 0.243, 95% CI: 0.226–0.261, P < 0.001) sleep qualities were protective factors against anxiety. When PA, sleep duration, and sleep quality were simultaneously included in the regression analysis, sleep factors remained protective factors against anxiety.
Discussion
As an essential component of overall health, mental health (MH) serves as a vital foundation for individual achievement and happiness. Recently, topics related to students’ MH have drawn significant societal attention5. University students are in a transitional phase from adolescence to adulthood, which is a critical period prone to MH issues. Continuously monitoring their MH, exploring influencing factors, and identifying potential problems early on for necessary interventions are imperative3,4. This study analyzed the levels of physical activity (PA), sleep conditions, and their associations with MH among Chinese university students using epidemiological survey methods. The presentation of data could contribute to the advancement of MH promotion initiatives for Chinese university students.
The results of this study demonstrate that university students in China exhibit predominantly light physical activity (LPA), with males engaging in higher levels of moderate to vigorous intensity PA (MVPA) compared with females. Notably, the participation in various types of PA among university students has been greatly affected by major public health events. During the COVID-19 pandemic, university students’ PA primarily consisted of low-intensity activities, and the quantity of leisure activities centered around sports and exercise drastically decreased. The COVID-19 pandemic has exacerbated the decline in PA across various populations, and the effects of related prevention measures have constrained outdoor sports and exercise among students to some extent. These findings are consistent with previous research42,43,44. A systematic review conducted by Alejandro et al.45 examined the influence of the COVID-19 pandemic on PA levels among university students and found a significant decrease in walking, MPA, VPA, and overall PA levels among university students in different countries.
From a global perspective, a significant trend of decreasing PA levels exists among various populations45. In recent years, a decline has been observed in MVPA among populations worldwide, which is closely associated with changes in nutrition, transportation, and lifestyle46. This decline in PA levels is also observed among Chinese university students. According to the results of the 8th National Survey on Students’ Physical Fitness and Health released by the Chinese Ministry of Education in 2021, the rate of university students meeting the physical fitness standards has not shown improvement, with a failure rate as high as 30%47. Overall, a continuous downward trend exists, which validates the findings of this study from the perspective of physical fitness indicators. In terms of gender differences, males tend to have higher levels of engagement in physical exercises compared with females, which aligns with previous research48,49. University students are in a transitional phase from adolescence to adulthood, and research has shown that male and female students exhibit an upward trend in MVPA before the age of 12, followed by a sustained decline. Researchers believe that this decline may be related to the rapid physiological and psychological development during adolescence50.
The results of this study indicate that the overall prevalence of insufficient sleep among university students is 39.5%, with the highest reported rates in schools located in the eastern region of China. A previous study conducted in 2014 reported a prevalence of 77.2% for insufficient sleep among Han Chinese students aged 9–18 years, with an increase in prevalence with age26. According to data from the second follow-up survey of the China Kadoorie Biobank project in 2014, the overall prevalence of insufficient sleep among Chinese adults was 25.8%51. In a study conducted in 2019, researchers collected Pittsburgh Sleep Quality Index (PSQI) data from 729 university students from two universities in Anhui and Jiangsu Provinces. The findings showed a detection rate of 56.2% for insufficient sleep among university students52. These findings suggest variations in the prevalence of insufficient sleep among university students. Potential reasons for these differences include variations in measurement tools, socioeconomic levels of the study population, and the development of entertainment industries in the areas where the schools are located. However, overall, the prevalence of insufficient sleep among university students is a serious concern, particularly with the emergence of new factors such as smartphone addiction and job-related stress. These factors contribute to an increased incidence of insufficient sleep among university students53. Moreover, the higher prevalence of insufficient sleep reported among students in eastern region schools may be related to the level of economic development. Previous research has shown that in more developed areas, lifestyle factors, such as the pace of life, can affect sleep patterns and other behaviors among the population54.
The overall prevalence of poor sleep quality among university students is 16.7%. Among senior students, the rate of poor sleep quality is the highest, and students who reported having consumed alcohol in the past also show the highest rate of poor sleep quality. However, previous studies have reported substantial variations in the prevalence of poor sleep quality. For example, a survey conducted in 2021 among students from four ordinary universities in Jiangsu, Shaanxi, Hubei, and Chongqing Provinces showed a rate of 13.2% for poor sleep quality using PSQI55. Similarly, the China Sleep Quality Report (2022) utilizing the PSQI found a rate of only 0.36% for poor sleep quality among university students53. Possible reasons for these discrepancies include differences in sampled regions, schools, or regional epidemic prevention and control policies, as well as variations in the anonymity level of questionnaire responses. Several studies have also indicated that senior students tend to have poorer sleep quality53,55,56. This may be attributed to greater pressures faced by senior students, especially those approaching graduation, such as stress related to employment, career choices, and further education. These pressures can potentially affect sleep quality. This highlights the importance for professionals involved in school management and MH to pay closer attention to the physical health and MH issues of senior students.
The results of this study reveal that 10% of university students are at high risk for depression, and 23.3% are at high risk for anxiety, with the prevalence of high-risk depression and anxiety symptoms being higher among males than females. The Blue Book of Mental Health: Report on the Development of Mental Health in China (2019–2020) reported a high-risk depression prevalence of 4.2% among university students in 2020 and a high-risk anxiety prevalence of 8.4%34. The detection rates of high-risk depression and anxiety among university students in this study are significantly higher than those reported in 2020. This finding is supported by a recent study published in The Lancet on June 12, 2023, which examined clinical symptoms in COVID-19 survivors and found that fatigue or muscle weakness, sleep difficulties, anxiety, and depression were among the main manifestations57. Analysis suggests that during major public health events, such as the COVID-19 pandemic, people may experience fear and other psychological responses related to the outbreak itself, which can contribute to the development of anxiety and depression. Moreover, the implementation of preventive measures to control the spread of the virus may reduce the amount of time people spend participating in recreational activities, such as outdoor sports, further contributing to the observed rates of MH issues among university students. These factors likely contribute to the prominent detection rates of MH problems among university students at present.
The results of this study show that university students with low PA levels, insufficient sleep, and poor sleep quality experience higher levels of psychological distress, which is consistent with previous research findings58,59,60,61. Previous studies have mainly explored the association between PA and MH among university students during the COVID-19 pandemic from the field of public health. Xiang et al.62 analyzed the relationship between MH and PA among university students during the COVID-19 pandemic. They found that VPA is significantly associated with lower anxiety, whereas MPA or VPA is significantly associated with reduced depression after controlling for confounding demographic factors. Kathryn’s61 study revealed a significant association between sedentary time (hours/day) and the severity of depression and anxiety among university students during the lockdown period of the COVID-19 pandemic in the United States. During the COVID-19 pandemic, home-based leisure activities dominated the majority of PA, such as stretching exercises and bodyweight resistance training62. Although different measurement methods have been used, the results of these studies are like the findings of the present paper. This suggests that the factors contributing to the MH of university students are multifaceted, and there may be interactive effects among various factors. Therefore, the influence of confounding factors is important to consider in the specific research design.
The results of this study indicate that MVPA and good sleep quality are protective factors for MH among university students. Ample consensus exists regarding the effectiveness of PA promotion, including leisure time activities and regular exercise, in improving MH outcomes, such as depression and anxiety63,64,65,66,67,68,69,70. Specifically, for adults with mild depression, exercise interventions have shown comparable efficacy to medication interventions71, providing foundational evidence for the role of exercise in promoting MH. Previous research has focused on the use of PA interventions to improve the MH status of students. For example, Chen et al.72 suggested that maintaining an active and regular PA routine, primarily through leisure time PA, may help students recover from the MH challenges experienced during the isolation periods of the COVID-19. Similarly, during the COVID-19 pandemic, the WHO released guidelines for individuals under self-isolation, including practical recommendations on how to maintain PA and reduce sedentary behavior at home. As for the protective role of sleep in health, various explanations have been proposed within the academic community73,74; however, a mature theory has not yet emerged75. One possible reason is that increasing sleep duration may compromise the time available for enhancing health behaviors, such as PA. Furthermore, whether a bidirectional causal relationship exists between MH and sleep issues still requires further investigation.
In addition to the individual effects of PA and sleep on the MH of university students, the results of this study also reveal an interactive effect of PA and sleep factors in the protection against depressive symptoms among university students. This finding suggests that scholars and clinicians engaged in student MH interventions can adopt combined approaches involving PA and sleep. As previously mentioned, in prospective cohort studies, physical inactivity, inadequate sleep, and poor sleep quality have been associated with increased risks of depression and anxiety when studied as separate risk factors76,77,78,79,80,81,82,83. However, few studies have provided insights into how the combination of PA and sleep factors influences MH status77,83. The coexistence of insufficient sleep and poor sleep quality is more strongly correlated with the occurrence of chronic MH symptoms compared with the presence of inadequate sleep alone84. Furthermore, physical inactivity and sleep problems often co-occur and exhibit bidirectional relationships, with a vicious cycle where physical inactivity leads to sleep problems, which, in turn, affect PA levels85,86. This finding necessitates researchers to adequately control confounding factors when designing univariate intervention studies targeting either PA or sleep. Moreover, Huang et al.’s75 research indicated a time dependency between PA and sleep behaviors, where extending sleep duration may reduce the time available for PA. Specifically, intervention studies based on a 24-hour activity behavior have already been validated in promoting child and adolescent health87,88, but research targeting university students as intervention subjects is limited. A recent study published in The Lancet demonstrated the crucial importance of regular physical exercise and healthy sleep in preventing cognitive decline. Relevant commentary highlights that a better understanding of the interaction between physical exercise and sleep in cognitive health would contribute to providing evidence for future lifestyle interventions and reducing the risk of dementia89. Given these findings, future research on student MH interventions should comprehensively consider PA and sleep factors and adopt integrated intervention methods to promote students’ MH levels.
This study has several strengths, including a large sample size, precise sampling, and broad geographical coverage. However, it also has some limitations to consider. First, being a cross-sectional study, establishing causal relationships had certain limits. Second, sleep and PA were not objectively measured, and the study relied on self-reporting, introducing risks of recall, and reporting biases. Moreover, this study did not collect data on participants’ history of mental illness, thereby failing to definitively determine whether students had been diagnosed MH issues, such as depression or anxiety, only examining symptoms of depression and anxiety. Additionally, the study was conducted during the COVID-19 pandemic, which may have influenced students’ physical activity levels, sleep patterns, and mental health. The pandemic’s impact on these factors could have affected the study results. Finally, several factors contribute to MH (e.g., diet and nutrition, social and peer relationships, home environment, socioeconomic status, dormitory environment, screen time, and built environment)90,91,92,93. Due to limitations in the study design, this research only explored PA, sleep, and factors such as smoking and drinking. Despite these limitations, an increasing body of research suggests that ensuring sufficient sleep time and increasing PA can alleviate, and even prevent, MH disorders among students. Our findings further underscore the need for researchers and clinicians to consider the combined effects of PA and sleep on the MH of adolescents when conducting research and designing intervention measures. In the future, large-scale longitudinal research that analyzes additional factors related to MH should be conducted to explore how PA and sleep affect these symptoms.
Conclusion
In this study, the university students mainly engaged in light physical activity, and a high prevalence of insufficient sleep was reported. Senior university students had poorer sleep quality and more severe mental health problems. Moderate to vigorous physical activity and adequate high-quality sleep may alleviate mental health issues among university students, and an interactive effect between PA and sleep in relieving depressive symptoms is possible.
This study used a large-sample epidemiological survey paradigm to understand the current physical activity levels, sleep conditions, and mental health status of university students in China, providing basic data for scholars conducting research on college student health behaviors. Based on the results of this study, the authors recommend that higher education institutions should pay attention to physical activity, sleep, and mental health issues among university students and develop relevant strategies and methods to increase physical activity levels and optimize students’ sleep environment, ensuring high-quality sleep. Moreover, scientific measurement methods should be implemented to regularly assess students’ mental health issues. For scholars engaged in promoting students’ mental health, further exploration should focus on targeted interventions combining physical activity and sleep behaviors to improve university students’ mental health levels. Finally, this study calls for university students to engage in regular moderate to vigorous physical activity, refrain from smoking and drinking alcohol, improve deep slow-wave sleep quality, and stay away from mental health problems.
Data availability
The raw data supporting the conclusions of this article will be available from Bo Li ([email protected]) on reasonable requests.
References
Santomauro, D. F. et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 398, 1700–1712. https://doi.org/10.1016/S0140-6736(21)02143-7 (2021).
Herrman, H. et al. Time for united action on depression: a Lancet-World Psychiatric Association Commission. Lancet 399, 957–1022. https://doi.org/10.1016/s0140-6736(21)02141-3 (2022).
Jinjian, Z. H. A. N. G. & Hong, C. H. E. N. A 4-year follow-up study of suicidal ideation among college students. Chin. School Health. 42, 1524–1526. https://doi.org/10.16835/j.cnki.1000-9817.2021.10.019 (2021).
Wathelet, M. et al. Factors Associated with Mental Health Disorders among University Students in France Confined during the COVID-19 pandemic. JAMA Netw. open. 3, e2025591. https://doi.org/10.1001/jamanetworkopen.2020.25591 (2020).
HUANG Chao. Take multiple measures to promote students’ mental health. People’s Daily. (2023). http://paper.people.com.cn/rmrb/html/2023-06/05/nw.D110000renmrb_20230605_3-05.htm 2023-06-05.
World Health, O. Depression and Other Common Mental Disorders: Global Health Estimates (World Health Organization, 2017).
Zergaw, A. et al. The Burden of Mental disorders in Ethiopia, from 1990 to 2019: a systematic analysis of the Global Burden of diseases Study 2019. Ethiop. J. Health Dev. 37, 6 (2023).
Elser, H. et al. Association of Early-, Middle-, and late-life Depression With Incident Dementia in a Danish cohort. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2023.2309 (2023).
Bull, F. C. et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 54, 1451–1462. https://doi.org/10.1136/bjsports-2020-102955 (2020).
Duncan, M. J., Holliday, E. G., Burton, N. W., Glozier, N. & Oftedal, S. Prospective associations between joint categories of physical activity and insomnia symptoms with onset of poor mental health in a population-based cohort. J. Sport Health Sci. https://doi.org/10.1016/j.jshs.2022.02.002 (2022).
Guthold, R., Stevens, G. A., Riley, L. M. & Bull, F. C. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Global Health. 6, 1077–1086. https://doi.org/10.1016/s2214-109x(18)30357-7 (2018).
Xie, L. et al. Sleep drives metabolite clearance from the adult brain. Science 342, 373–377. https://doi.org/10.1126/science.1241224 (2013).
Walker, M. P. & Stickgold, R. Sleep, memory, and plasticity. Annu. Rev. Psychol. 57, 139–166. https://doi.org/10.1146/annurev.psych.56.091103.070307 (2006).
Miyata, S. et al. Insufficient sleep impairs driving performance and cognitive function. Neurosci. Lett. 469, 229–233. https://doi.org/10.1016/j.neulet.2009.12.001 (2010).
Calhoun, S. L. et al. Learning, attention/hyperactivity, and conduct problems as sequelae of excessive daytime sleepiness in a general population study of young children. Sleep 35, 627–632. https://doi.org/10.5665/sleep.1818 (2012).
Tymoszuk, U., Perkins, R., Spiro, N., Williamon, A. & Fancourt, D. Longitudinal associations between Short-Term, repeated, and sustained arts Engagement and Well-being outcomes in older adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 75, 1609–1619. https://doi.org/10.1093/geronb/gbz085 (2020).
Chapman, D. P. et al. Frequent insufficient sleep and anxiety and depressive disorders among U.S. community dwellers in 20 states, 2010. Psychiatr Serv. 64, 385–387. https://doi.org/10.1176/appi.ps.201200226 (2013).
Yuan, S. et al. Sleep duration, daytime napping, and risk of peripheral artery disease: multinational cohort and mendelian randomization studies. Eur. Heart J. Open. 3, oead008. https://doi.org/10.1093/ehjopen/oead008 (2023).
Woods, J. A. et al. The COVID-19 pandemic and physical activity. Sports Med. Health Sci. 2, 55–64. https://doi.org/10.1016/j.smhs.2020.05.006 (2020).
Herrman, H. et al. Reducing the global burden of depression: a Lancet-World Psychiatric Association Commission. Lancet 393, 42–43. https://doi.org/10.1016/s0140-6736(18)32408-5 (2019).
Cuijpers, P., Stringaris, A. & Wolpert, M. Treatment outcomes for depression: challenges and opportunities. Lancet Psychiatry. 7, 925–927. https://doi.org/10.1016/S2215-0366(20)30036-5 (2020).
Qiu Junqiang, C., Lin, Y. X. Y. F., Dan, L. & Wenhua, Z. Exercise for Health: a review and Prospect based on the theory of Energy Balance. J. Beijing Sport Univ. 44, 2–20. https://doi.org/10.19582/j.cnki.11-3785/g8.2021.05.001 (2021).
Qi Changzhu, G., Yuanbing, G. & Rujie Research Progress on Exercise for Mental Health: a method-based perspective. J. Wuhan Univ. Phys. Educ. 54, 86–92. https://doi.org/10.19582/j.cnki.11-3785/g8.2021.05.001 (2020).
Mu, F. et al. Influence of physical exercise on negative emotions in college students: chain mediating role of sleep quality and self-rated health. Front. Public. Health. 12, 1402801. https://doi.org/10.3389/fpubh.2024.1402801 (2024).
Li, B. et al. Influence of moderate-to-high intensity physical activity on depression levels: a study based on a health survey of Chinese university students. BMC Public. Health. 24, 1023. https://doi.org/10.1186/s12889-024-18433-w (2024).
Dongmei, L. et al. Study on sleep deprivation and its relationship with physical exercise among Han students aged 9 ~ 18 in China in 2014. Chin. J. Epidemiol. 39, 1298–1320. https://doi.org/10.3760/cma.j.issn.0254-6450.2018.10.002 (2018).
Bauman, A. et al. Progress and pitfalls in the use of the International Physical Activity Questionnaire (IPAQ) for adult physical activity surveillance. J. Phys. Act. Health. 6 (Suppl 1), S5–8. https://doi.org/10.1123/jpah.6.s1.s5 (2009).
Qu Ningning, L. Reliability and validity of the Chinese version of the International Physical Activity Questionnaire. Chin. J. Epidemiol. 25, 265–268. https://doi.org/10.3760/j.issn:0254-6450.2004.03.021 (2004).
D, M., E, C. & A, C. & Examining the validity and reliability of the Chinese version of the International Physical Activity Questionnaire, long form (IPAQ-LC). Public. Health Nutr. 14, 443–450. https://doi.org/10.1017/S1368980010002806 (2011).
Mengyu, F. A. N., Yun, L. V. & Pingping, H. E. Calculation of physical activity level in the International Physical Activity Questionnaire. Chin. J. Epidemiol. 35, 961–964. https://doi.org/10.3760/cma.j.issn.0254-6450.2014.08.019 (2014).
Xu Jinfu, L. & Yu A study on the reliability and validity of the International Physical Activity Questionnaire in College Students. J. Changchun Normal Univ. 37, 106–108 (2018).
Xiangchen, L. & Maoqin, T. A. Study of the Reliability and Validity of the Pittsburgh Sleep Quality Index. Chin. J. Psychiatry. 29 https://doi.org/103-105 (1996).
Nathaniel et al. Recommended amount of Sleep for a healthy adult: a Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 38, 843–844. https://doi.org/10.5665/sleep.4716 (2015).
Fu Xiaolan, Z. & Kan, C. Xuefeng. Blue Book of Mental Health: Report on the Development of National Mental Health in China (2019–2020). Beijing: Social Sciences Academic Press; (2021).
Zhang Jie, W., Zhenyun, F., Ge, L., Juan, H. & Buxin, C. Establishment of the National Urban Norm of the Depression Scale of the Epidemiological Center. Chin. J. Mental Health. 24, 139–143. https://doi.org/10.3969/j.issn.1000-6729.2010.02.015 (2010).
Jin, H. E. et al. Compilation of the Chinese Simplified Version of the Depression Scale of the Flow Control Center. Chin. J. Behav. Med. Brain Sci. 22, 1133–1136. https://doi.org/10.3760/cma.j.issn.1674-6554.2013.12.023 (2013).
Spitzer, R. L., Kroenke, K., Williams, J. B. & Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166, 1092–1097. https://doi.org/10.1001/archinte.166.10.1092 (2006).
Fu, W. et al. Mental health of college students during the COVID-19 epidemic in China. J. Affect. Disord. 280, 7–10. https://doi.org/10.1016/j.jad.2020.11.032 (2021).
McHugh, M. L. The chi-square test of independence. Biochem. Med. (Zagreb). 23, 143–149. https://doi.org/10.11613/bm.2013.018 (2013).
Simon, S. D. Understanding the odds ratio and the relative risk. J. Androl. 22, 533–536 (2001).
Hao, Z. H. O. U. & Lirong, L. O. N. G. Statistical testing and control methods for common method bias. Adv. Psychol. Sci. 12, 942–950. https://doi.org/10.3969/j.issn.1671-3710.2004.06.018 (2004).
Wang Keping, W. & Yanying, L. Physical exercise behavior and influencing factors of college students during the novel coronavirus pneumonia epidemic. Chin. School Health. 42, 87. https://doi.org/10.16835/j.cnki.1000-9817.2021.01.021 (2021).
Ding, Y., Ding, S. & Niu, J. The impact of COVID-19 on college students’ physical activity: a protocol for systematic review and meta-analysis. Med. (Baltim). 100, e27111. https://doi.org/10.21203/rs.3.rs-715532/v1 (2021).
DeYoung, W., Constine, C. N. & Li, K. G. Comparisons of physical activity, sitting time, and substance use among college students before and during the COVID-19 pandemic. J. Am. Coll. Health, 9, https://doi.org/10.1080/07448481.2022.2104613
López-Valenciano, A., Suárez-Iglesias, D., Sanchez-Lastra, M. A. & Ayán, C. Impact of COVID-19 Pandemic on University Students’ Physical Activity Levels: An Early Systematic Review. Front. Psychol. 11 https://doi.org/10.3389/fpsyg.2020.624567 (2021).
Bull, F. C., Al-Ansari, S. S., Biddle, S., Borodulin, K. & Willumsen, J. F. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 54, 1451–1462. https://doi.org/10.1136/bjsports-2020-102955 (2020).
People’s Daily Online. The results of the 8th National Student Physical Fitness and Health Survey Released Students’ height, weight and other developmental indicators continue to improve: Ministry of Education of the People’s Republic of China; (2021). http://edu.people.com.cn/n1/2021/0903/c1006-32216712.html
Alonso-Fernández, N., Jiménez-Garcia, R., Alonso-Fernández, L. & Hernandez-Barrera, V. Palacios-Ceña, D. Health factors related to physical activity among children and adolescents: results from Spanish National Health surveys 2006 and 2011/12: health factors related to physical activity among children and adolescents. J. Spec. Pediatr. Nursing: JSPN. 20, 193–202. https://doi.org/10.1111/jspn.12113 (2015).
Wang Zhenghe, D., Yanhui, S. & Yi Prevalence of physical exercise time of less than 1 hour among 9 ~ 22-year-old students in China in 2014 and its influencing factors. Chin. J. Epidemiol. 38, 341–345 (2017).
Junfang, C. A. O. A study on the physical activity status and influencing factors of children and adolescents in provincial capital cities in China. East. China Normal Univ. https://doi.org/10.27149/d.cnki.ghdsu.2020.000202
Wen Qiaorui, W. et al. Correlation between sleep duration and insomnia symptoms and muscle weight, strength and mass in Chinese adults. Chin. J. Epidemiol. 43, 175–182. https://doi.org/10.3760/cma.j.cn112338-20201020-01252 (2022).
Zhang, D. et al. Correlation between sleep duration and time pattern and unsteady state load in college students. Mod. Prev. Med. 48, 3182–3186 (2021).
Wang, J., Zhang, Y., Liu, Y. & Xilinmen Sleep Research Institute. China Sleep Research Report 2022. Beijing: Social Sciences Academic Press; (2022).
Jin Ye, L. Investigation on the current situation of young residents’ physique and lifestyle in different economic development areas in some provinces and cities in China and its intervention. J. Beijing Sport Univ. 32, 55–59. https://doi.org/10.19582/j.cnki.11-3785/g8.2009.10.017 (2009).
Wang Zhiwei, L., Meibing, C. & Hongxia, G. Effects of moderate-to-high-intensity physical activity and screen time on sleep quality in college students. Mod. Prev. Med. 50, 688–691. https://doi.org/10.20043/j.cnki.MPM.202208331 (2023).
Yang, J. & Zhou, L. The relationship between daily physical activity and sleep quality in college students. Chin. School Health. 42, 1047–1051. https://doi.org/10.16835/j.cnki.1000-9817.2021.07.020 (2021).
Huang, C. et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 397, 220–232. https://doi.org/10.1016/s0140-6736(20)32656-8 (2023).
Chunlei, Z. H. A. N. G., Shouwei, Z. H. A. N. G. & Kunpeng, X. I. A. O. The Effect of Exercise intervention on psychological stress in College students: the mediating effect of Health Belief. J. Chengdu Univ. Phys. Educ. 42, 103–108. https://doi.org/10.15942/j.jcsu.2016.04.018 (2016).
Wei, X. U. & Fengying, C. H. E. N. The subjective health level of college students and its relationship with the quality of sports. Chin. School Health 36, 1408–1410, https://doi.org/10.16835/j.cnki.1000-9817.2015.09.043(2015).
Zhang, Y. et al. Association between the interaction between physical exercise and sleep quality and the mental health of college students. Chin. School Health 36, 1025–1028, https://doi.org/10.16835/j.cnki.1000-9817.2015.07.022(2015).
Coakley, K. E., Lardier, D. T., Holladay, K. R., Amorim, F. T. & Zuhl, M. N. Physical activity behavior and Mental Health among University Students during COVID-19 Lockdown. Front. Sports Act. Living. 3 https://doi.org/10.3389/fspor.2021.682175 (2021).
Xiang, M. Q. et al. Relationship of physical activity with anxiety and depression symptoms in Chinese College Students during the COVID-19 outbreak. Front. Psychol. 11 https://doi.org/10.3389/fpsyg.2020.582436 (2020).
Singh, B. et al. Effectiveness of physical activity interventions for improving depression, anxiety and distress: an overview of systematic reviews. Br. J. Sports Med. https://doi.org/10.1136/bjsports-2022-106195 (2023). bjsports-2022-106195.
Heissel, A. et al. Exercise as medicine for depressive symptoms? A systematic review and meta-analysis with meta-regression. Br. J. Sports Med. 57, 1049–1057. https://doi.org/10.1136/bjsports-2022-106282 (2023).
Davenport, M. H. et al. Impact of prenatal exercise on both prenatal and postnatal anxiety and depressive symptoms: a systematic review and meta-analysis. Br. J. Sports Med. 52, 1376–1385. https://doi.org/10.1136/bjsports-2018-099697 (2018).
Martland, R. et al. Can high-intensity interval training improve mental health outcomes in the general population and those with physical illnesses? A systematic review and meta-analysis. Br. J. Sports Med. 56, 279–291. https://doi.org/10.1136/bjsports-2021-103984 (2022).
Lei, X. U. Meta-analysis of the effects of physical activity on subjective well-being: evidence from experimental studies. Sports Sci. 34, 29–38. https://doi.org/10.3969/j.issn.1000-677X.2014.10.004 (2014).
Hengchan, Y. I. N., Min, L. U., Xinli, W. A. N. G. & Yanfei, C. H. E. N. A study on the Effect of Exercise on the Mental Health of College Students. Sports Sci. 27, 41–46. https://doi.org/10.16469/j.css.2007.05.006 (2007).
Ying, H. E. & Liu, J. I. The Effect of different physical Exercise types on Depression Level in College Students and its body-esteem. Sports Sci. 24, 32–35. https://doi.org/10.16469/j.css.2004.05.011 (2004).
Wangyang, H., Jun, Z., Weizhong, X. & Kailai, L. Effect of physical exercise on anxiety in college students. Sports Sci. 24, 61–62. https://doi.org/10.16469/j.css.2004.02.019 (2004).
Recchia, F. et al. Comparative effectiveness of exercise, antidepressants and their combination in treating non-severe depression: a systematic review and network meta-analysis of randomised controlled trials. Br. J. Sports Med. 56, 1375–1380. https://doi.org/10.1136/bjsports-2022-105964 (2022).
Chen, P. et al. Returning Chinese school-aged children and adolescents to physical activity in the wake of COVID-19: actions and precautions. J. Sport Health Sci. 9, 322–324. https://doi.org/10.1016/j.jshs.2020.04.003 (2020).
Bellavia, A., Åkerstedt, T., Bottai, M., Wolk, A. & Orsini, N. Sleep duration and survival percentiles across categories of physical activity. Am. J. Epidemiol. 179, 484–491. https://doi.org/10.1093/aje/kwt280 (2014).
Chen, L. J. et al. Can physical activity eliminate the mortality risk associated with poor sleep? A 15-year follow-up of 341,248 MJ Cohort participants. Jour Sport Health Sci. 11, 596–604. https://doi.org/10.1016/j.jshs.2021.03.001 (2022).
Huang, B. H. et al. Sleep and physical activity in relation to all-cause, cardiovascular disease and cancer mortality risk. Br. J. Sports Med. 56, 718–724. https://doi.org/10.1136/bjsports-2021-104046 (2022).
Firth, J. et al. A meta-review of lifestyle psychiatry: the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry: Official J. World Psychiatric Association (WPA). 19, 360–380. https://doi.org/10.1002/wps.20773 (2020).
Schuch, F. B. et al. Physical activity and Incident Depression: a Meta-analysis of Prospectie Cohort studies. Am. J. Psychiatry. 175, 631–648. https://doi.org/10.1176/appi.ajp.2018.17111194 (2018).
Schuch, F. B. et al. Physical activity protects from incident anxiety: a meta-analysis of prospective cohort studies. Depress. Anxiety. 36, 846–858. https://doi.org/10.1002/da.22915 (2019).
Li, L., Wu, C., Gan, Y., Qu, X. & Lu, Z. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry. 16, 375. https://doi.org/10.1186/s12888-016-1075-3 (2016).
Hertenstein, E. et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med. Rev. 43, 96–105. https://doi.org/10.1016/j.smrv.2018.10.006 (2019).
Zhai, L., Zhang, H. & Zhang, D. Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress. Anxiety. 32, 664–670. https://doi.org/10.1002/da.22386 (2015).
Rebar, A. L. et al. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol. Rev. 9, 366–378. https://doi.org/10.1080/17437199.2015.1022901 (2015).
Ashdown-Franks, G. et al. Exercise as Medicine for Mental and Substance Use disorders: a Meta-review of the benefits for neuropsychiatric and cognitive outcomes. Sports Med. (Auckland N Z). 50, 151–170. https://doi.org/10.1007/s40279-019-01187-6 (2020).
Biddle, D. J., Hermens, D. F., Lallukka, T., Aji, M. & Glozier, N. Insomnia symptoms and short sleep duration predict trajectory of mental health symptoms. Sleep Med. 54, 53–61. https://doi.org/10.1016/j.sleep.2018.10.008 (2019).
Duncan, M. J. et al. Patterns of physical activity, sitting time, and sleep in Australian adults: a latent class analysis. Sleep. Health. 6, 828–834. https://doi.org/10.1016/j.sleh.2020.04.006 (2020).
Huang, B. H., Hamer, M., Duncan, M. J., Cistulli, P. A. & Stamatakis, E. The bidirectional association between sleep and physical activity: a 6.9 years longitudinal analysis of 38,601 UK Biobank participants. Prev. Med. 143, 106315. https://doi.org/10.1016/j.ypmed.2020.106315 (2021).
Zhenya, C. H. A. N. G. & Shuming, W. A. N. G. Isochronous substitution benefits of the effect of 24-hour motor behavior on physical health of preschool children. Sports Sci. 40, 50–57. https://doi.org/10.16469/j.css.202010006 (2020).
Liang Guo, W., Lijuan, C., Huan, L. & Hao, C. Relationship between 24-hour activity time distribution and substitution and children’s body mass index: based on a component analysis model. Sports Sci. 42, 77–84. https://doi.org/10.16469/j.css.202203008 (2022).
Bloomberg, M., Brocklebank, L., Hamer, M. & Steptoe, A. Joint associations of physical activity and sleep duration with cognitive ageing: longitudinal analysis of an English cohort study. Lancet Healthy Longev. 4, e345–e353. https://doi.org/10.1016/s2666-7568(23)00083-1 (2023).
Xiao, P. et al. Anxiety, Depression, and satisfaction with life among College students in China: nine months after initiation of the outbreak of COVID-19. Front. Psychiatry. 12, 10. https://doi.org/10.3389/fpsyt.2021.777190 (2022).
Liang, K. X. et al. Sleep as a Priority: 24-Hour Movement Guidelines and Mental Health of Chinese College Students during the COVID-19 pandemic. Healthcare 9, 13. https://doi.org/10.3390/healthcare9091166 (2021).
Xu, J. et al. Effects of urban living environments on mental health in adults. Nat. Med. 29, 1456–1467. https://doi.org/10.1038/s41591-023-02365-w (2023).
Alosaimi, N., Sherar, L. B., Griffiths, P. & Pearson, N. Clustering of diet, physical activity and sedentary behaviour and related physical and mental health outcomes: a systematic review. BMC Public. Health. 23, 1572. https://doi.org/10.1186/s12889-023-16372-6 (2023).
Funding
Jiangsu Provincial Education Science Planning Project (B/2022/01/173);Overseas High-level Talent Program of Shanghai Municipality (TP2022102); 2024 General Project of Philosophy and Social Science Research in Jiangsu Universities (No. 2024SJYB1253); Jiangxi Province University Humanities and Social Science Research Youth Project (No.TY22210); Hanjiang Normal University Key Scientific Research Project (No. XJ2020A03).
Author information
Authors and Affiliations
Contributions
YL and BL contributed to the conceptualization and design of the study, interpretation of the data, and critical drafting and revising of the manuscript; BL and SSH conducted the statistical analyses and contributed to the interpretation of the data and critical revision of the manuscript; YPY, YXL, SQM, SF, HL, ZLC, YSZ, YZ, WDZ,QZ and GXW contributed to the interpretation of the data and critical revision of the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Nantong University (No 70/2022). Informed consent was obtained from all participants involved in this study.
Consent for publication
No applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, B., Han, Ss., Ye, Yp. et al. Cross sectional associations of physical activity and sleep with mental health among Chinese university students. Sci Rep 14, 31614 (2024). https://doi.org/10.1038/s41598-024-80034-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-80034-9