Abstract
To investigate the effectiveness of cap-assisted endoscope synchronous advancement and tube direction adjustment for inserting transnasal ileus tubes in patients with malignant adhesive bowel obstruction (MABO). 25 patients with cap-assisted endoscopic synchronous method (Group A, Dec 2023–Apr 2024) were reviewed retrospectively. Accordingly, those with forceps-grasping method (Group B: 27, Aug 2022–Nov 2023) were included as controls. Both groups were similar in terms of age, sex, primary tumor, doctor experience distribution and technical success rate. The proportion of gynecological cancers was the highest in either group. The time required for insertion was shorter in Group A than in Group B (5 vs. 12 min; P = 0.000). Group A also had slightly longer tube insertion length than Group B (129.8 ± 14.1 vs. 121.3 ± 12.0 cm; P = 0.008), and the remission rate of intestinal obstruction symptoms in Group A was similar to that in Group B (75.0% vs. 74.1%; P = 0.940). There were no significant differences in complications between the two groups. One patient suffered MABO recurrence 14 days after withdrawal of the tube. Our findings indicate that transnasal ileus tube insertion with cap-assisted endoscopic synchronous method took shorter time and had the same rate of technical success and advantage of decompression compared with forceps-grasping method.
Similar content being viewed by others
Introduction
Malignant adhesive bowel obstruction (MABO)1,2 caused by peritoneal carcinomatosis is a refractory complication of advanced primary abdominal pelvic malignancy or distant metastasis, leading to poor nutrition and multiple levels of bowel involvement. There is substantial evidence suggesting that bowel rest and effective decompression followed by partial enteral nutrition via long tube play an important role in the treatment for benign and malignant adhesive bowel obstruction. Although transnasal ileus tube decompression in malignant patients is associated with a lower remission rate1,2,3 of intestinal obstruction symptoms compared with that observed in benign cases, the success rate of long tube decompression may reach 80% in all treated malignant cases. It has been recommended as a first-line therapeutic strategy in cancer-related bowel obstruction cases4.
The procedure of transnasal ileus tube insertion can be performed under fluoroscopic5,6,7,8,9 or endoscopic guidance. Fluoroscopic guidance often results in long procedure time and exposure to radiation. Published endoscope-aided techniques include transnasal ultrathin endoscopic guidewire pre-placement and endoscopic forceps-grasping method10,11,12. Transnasal ultrathin endoscope is not available in all hospitals. As for forceps-grasping method, the friction between the tube and the endoscope is considered resistance slowing down the whole procedure9,12.
However, friction can also become power if properly utilized. In this retrospective study, we reported our experiences of using cap-assisted endoscope synchronous advancement and tube direction adjustment technique to insert transnasal ileus tube and evaluate the efficacy and safety of the long tube to achieve decompression for treating malignant adhesive bowel obstruction.
Materials and methods
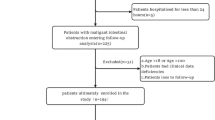
Study design and patients
From August 2022 to April 2024, a total of 54 patients receiving endoscopic transnasal ileus tube insertion at Fujian Cancer Hospital, Fuzhou, China, were enrolled in our single-tertiary-center retrospective cohort comparative study.
Malignant adhesive bowel obstruction was defined as adhesive bowel obstruction caused by abdominal carcinomatosis, the diagnostic criteria included clinical evidence of bowel obstruction, the presence of primary intra-abdominal or extra-abdominal cancer with peritoneal involvement, and extensive intestinal distension with air-fluid level above the end of ileum revealed by computed tomography scanning. Patients with obstructing mass in the colonic lumen or obstruction proximal to the Treitz ligament were excluded from the analysis.
Instruments and descriptions of two endoscopic techniques
A hydrophilic long tube (One-Step Ileus™, Sumitomo Bakelite Co., Japan) was used, with an outer diameter of 16 F, a working length of 3000 mm, two balloons, three chambers and a beaded-type tip. A spring guidewire ( 0.052inch, 300 cm long; Create Medic, Japan) was used for hardening the tube. All procedures were performed under CO2 insufflation to avoid complications caused by severe distress. Both procedures were performed by a team consisting of one endoscopist with more than five years of endoscopic experience and one nurse.
Procedures
Transparent cap-assisted endoscopic synchronous advancement and tube direction adjustment technique (Group A) (video 1)
First, a long ileus tube was inserted into the cardia via nasal cavity, followed by a therapeutic endoscope (GIF-Q260J/H290T; Olympus, Tokyo, Japan) mounted with a distal transparent hood (D-201-11804, Olympus Co.) advancing to the same site trans-orally, with the patient in the left lateral position. Then both the tube and the endoscope were moved forward synchronously by using the friction between the two until the posterior balloon of the tube passed through the horizontal part of duodenum. Aspiration of excess gas in the stomach via endoscopic working channel to adjust gastric morphology if necessary. Subsequently the endoscope was removed and the tube was advanced as distally as possible to the dilated bowel. Finally, the anterior balloon was inflated with 25 ml of sterile water, and the spring guidewire was withdrawn.
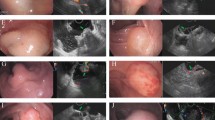
Endoscopic forceps-grasping technique (Group B) (Fig. 1)
First, two sutures were tied to the beaded-type tip and the posterior balloon of a long ileus tube respectively. Then the ileus tube was inserted into the greater curvature of the stomach via nasal cavity, followed by a conventional endoscope (GIF-H260/Q260/H290; Olympus, Tokyo, Japan) advancing to the same site trans-orally, with the patient in the left lateral position. The suture at the tip of the tube was grasped first by forceps to facilitate passage of the tube through the pylorus (Fig. 1A). Then the suture at the tip was released and endoscope was withdrawn to the stomach to grasp the suture at the posterior balloon of the tube to carry the posterior balloon of the tube across the horizontal part of duodenum (Fig. 1B). The forceps released the suture at the posterior balloon (Fig. 1C) and the tube was advanced as far as possible to the dilated bowel. Finally, the anterior balloon was inflated with 25 ml of sterile water, and the spring guidewire was withdrawn.
Endoscopic forceps-grasping technique. (A) The suture at the tip of the tube grasped first by forceps to facilitate passage of the tube through the pylorus. (B) Then suture at the posterior balloon of the tube grasped by forceps to carry the posterior balloon of the tube across the horizontal part of duodenum. (C) The suture at the posterior balloon of the tube released by the forceps.
Outcome measurements
The primary endpoint of our analysis was the rate of successful insertion. Successful intubation was defined as insertion of a long tube beyond the duodenojejunal flexure confirmed by postprocedural fluoroscopy.
Secondary study endpoints were the tube insertion length, the time required for intubation, and the remission rate of intestinal obstruction symptoms. The procedure time was determined from insertion of the tube. The failure of clinical decompression was defined as no improvement of abdominal pain and distension 48 h after the successful insertion.
Sample size calculation
As for one non-inferiority test between two independent sample rates, assuming the rate of successful insertion in Group A to be 0.95, the rate in Group B to be 0.99, △ to be -0.1, α to be 0.025, β to be 0.2, the ratio to be 1, according to the formulae proposed by Farrington CP et al.13, the sample size required in either group was 23. Finally, 25 cases in Group A and 27 cases in Group B were used in this study (Fig. 2).
Statistical analysis
Study data are presented as median and interquartile range for skewed distributed continuous variables, mean ± standard deviation (SD) for normally distributed continuous variables, and frequencies and percentages for qualitative variables. Fisher’s exact test and Pearson X2 tests were used for comparisons involving qualitative variables, and the Wilcoxon rank-sum test was used for comparisons involving continuous variables. Multivariate logistic regression analysis regarding the rate of clinical remission was subsequently performed to calculate odds ratios (ORs) and 95% confidence intervals (CIs). All P values were two-tailed, and two-tailed P values < 0.05 were considered significant. All the statistical analyses were performed using IBM SPSS statistical software version 23.0.
Ethics declarations
This study was in accordance with the ethical guidelines of the 1964 Declaration of Helsinki and approved by the Institutional Review Board of Fujian Cancer Hospital (K2023-310-01). All the patients signed written informed consent before procedure and gave written informed consent to the use of their clinical data as anonymous record for research and publication.
Results
Clinical characteristics of the patients between two groups (Table 1)
Group A (Dec 2023-Apr 2024) contained 25 patients and Group B (Aug 2022-Nov 2023) 27 patients. Both groups were similar in terms of age, sex, primary tumor and doctor experience distribution. The primary tumor consisted of gynecological cancers, gastric cancer, colorectal cancer, pancreatic cancer, retroperitoneal liposarcoma, and peritoneal metastasis from pulmonary cancer and breast cancer. The proportion of gynecological cancers was the highest in either group, the female-to-male ratio was greater than one accordingly. The characteristics of the patients are shown in Table 1.
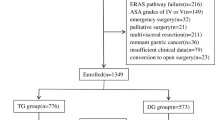
Clinical outcomes of the patients between two groups (Tables 2 and 3; Fig. 3)
The technical success rate of radiologically confirmed post-duodenojejunal flexure intubation was almost 100% in both groups (96% in Group A vs. 100% in Group B; P = 0.481). In Group A, the reason for the failure in one patient was the patient could not tolerate non-sedated endoscopy. In Group B, the failure happened to two patients was caused by the post-ulcer stenosis and angulation of the junction of the duodenal bulb and descending part, leading to the inability to deeply insert both the ileus tube and the forceps. Logically, the two cases were excluded from the subsequent analysis.
The time required for intubation was significantly shorter in Group A than in Group B (5 (IQR 3) vs. 12 (IQR 4) min; P = 0.000). Group A also had significantly longer tube insertion length than Group B (129.8 ± 14.1 vs. 121.3 ± 12.0 cm; P = 0.008), and the clinical remission rate of intestinal obstruction symptoms in Group A was similar to that in Group B (75.0% vs. 74.1%; P = 0.940). In the 13 patients without clinical remission, 2 in Group A and 3 in Group B received emergency enterostomy, presenting complete mechanical bowel obstruction caused by fixed angulation, 3 in Group A and 1 in Group B refused any further invasive therapy, and 1 in Group A and 3 in Group B died of septic shock (2), bowel necrosis (1) and IV myelosuppression (1).
The association between various factors and the clinical remission rate, as well as the OR for clinicopathological determinants and endoscopic techniques in both univariate and multivariate logistic regression analyses, are delineated in Table 3. Univariate analysis showed no significant relationship between variables and the clinical remission rate, while multivariate logistic regression revealed the doctor experience as the only independent predictor (P = 0.020, OR 0.119, 95% CI 0.020–0.714). The more experienced the doctor, the higher the clinical remission rate.
Complications
No complications relevant to the tube intubation, including epistaxis, delayed gastrointestinal bleeding and perforation, were encountered in either group.
Follow‑up
For those 38 patients who achieved clinical remission, the median follow-up period after tube intubation was 7 months (IQR 7). One patient suffered MABO recurrence 14 days after withdrawal of the tube, and then underwent emergency enterostomy.
Discussion
Although many non-operative managements14,15,16 have been developed for palliation of benign or malignant bowel adhesive obstruction, transnasal ileus tube decompression is still considered to be preferred. Initially, transnasal ileus tube insertion under fluoroscopy guidance is a standard clinical procedure for bowel obstruction6, resulting in the median tube insertion length of 170 cm, longer than that only guided by endoscopy. However, a longer procedure time and tube insertion length mean the larger radiation dose exposure. Placement of an ileus tube exclusively by endoscopy may lessen invasiveness and bring greater safety for both medical personnel and patients. With our experience, once the beaded-type tip of long tube was beyond the duodenojejunal flexure, it could make steady progress with small intestinal peristalsis aided by the gravity of its anterior balloon. So excessively deep insertion of the tube may be unnecessary. Moreover, based on the distance between the beaded-type tip and the posterior balloon of a long ileus tube, once we saw the posterior balloon passed through the horizontal part of duodenum, we could deduce that the beaded-type tip must be beyond the duodenojejunal flexure. Therefore, postprocedural fluoroscopy confirmation was no longer performed from May 2024. Additionally, in our study, the tube insertion length in Group A was significantly longer than that in Gorup B, the possible reason may be that the longer procedure time in Group B means the higher possibility of gastrointestinal distension caused by unintentional excessive CO2 insufflation during the procedure, which may interfere with deep insertion of the tube. However, the significant difference of the tube insertion length has no clinical significance because the tube can make steady progress if its tip is beyond the duodenojejunal flexure, as mentioned above.
Previously published studies10,12 suggest that the friction between the tube and the guidewire or endoscope is unfavorable for deeper insertion. In our opinion, static friction can also become power if the tube has the same direction of advance as the endoscope. The tube direction can be indirectly adjusted by controlling the endoscopic moving directly, especially when the tube is passing through the junction of fundus and body of stomach, pylorus and the junction of the duodenal bulb and descending part. Aspiration of excess gas in the stomach and cap-assisted technique also may have contributed to increase the friction and then shorten the procedure time. Cap-assisted endoscopy17,18,19,20 refers to a procedure in which a short cap made of a polymer (mostly transparent) is attached to the distal tip of the endoscope to enhance its diagnostic and therapeutic capabilities. During the procedure of an ileus tube insertion, shortening and unlooping of the greater curvature of the stomach are important for aligning the axis of the tube and the endoscope. Cap-assisted technique ensures a clear view and enables the cap to push aside the mucosal folds and fiddle with the tube direction during cannulation. In our study, most procedures were proposed under non-sedation, thanks to a short procedure time.
The overall post-insertion remission rate of intestinal obstruction symptoms in our study was 74.5% (38/51), similar to but slightly lower than 80% reported in other studies1,2,3. Multivariate analysis revealed the patients were more likely to receive clinical remission when their procedures were performed by more experienced doctors. It was speculated that those experienced doctors would try to avoid excessive insufflation, thereby reducing the risk of obstruction aggravation. In the 13 patients without clinical remission, 5 cases failed to conservative treatment and underwent emergency enterostomy. Complete mechanical bowel obstruction caused by fixed angulation may have contributed to this result.
Out of 51 patients achieving technical success, 2 (3.9%) patients still died of life-threatening septic shock21,22 with disseminated intravascular coagulation (DIC) in our study. Bacterial translocation was considered, triggered by disturbance of the intestinal microbiota and breakdown of the intestinal mucosal barrier. The early diagnosis of bacterial translocation is quite difficult, the early introduction of polymyxin B-immobilized fiber column direct hemoperfusion may prevent disease progression.
There were some limitations in our study, however. First, this is a retrospective study at a single institution, based on small samples, some potential bias can’t be ignored. Further large-sample prospective research is needed for better understanding the effects of the novel procedure. Second, the median duration of follow-up in our study was only 7 months, far shorter that in Lin SW et al. study23. The long-term risk of recurrent small bowel obstruction requires further evaluation.
Conclusion
Insertion of a transnasal ileus tube may be used as a feasible therapy in malignant adhesive bowel obstruction, especially caused by gynecological cancers. Transnasal ileus tube insertion accompanied with cap-assisted endoscopic synchronous advancement and tube direction adjustment proved to be safe, reproducible, and easy to implement, and took shorter time compared with the procedure conducted with the help of forceps-grasping method.
Data availability
The datasets generated and analyzed in the current study are available from the corresponding author upon reasonable request.
References
Qi, X., Shimin, Y. & Yu, W. The effect of compound Da-Cheng-Qi Decoction on the treatment of malignant bowel obstruction with transnasal ileus tube. Complement. Ther. Clin. Pract. 43, 1013–1016 (2021).
Han, X. J., Zhao, F., Su, H. Y. & Xu, K. Outcome of decompression using a transnasal ileus tube in malignant adhesive bowel obstruction: A retrospective study. Mol. Clin. Oncol. 7, 701–705 (2017).
Zhen, Y. et al. Metachronous small bowel adenocarcinoma after rectal adenocarcinoma: A case report. Med. (Baltim) 100, e27448 (2021).
Yang, W. & Pu, J. Efficacy of ileus tube combined with meglumine diatrizoate in treating postoperative inflammatory bowel obstruction after surgery. World J. Gastrointest. Surg. 15, 1950–1958 (2023).
Tan, Y., Chen, H., Mao, W., Yuan, Q. & Niu, J. Short-term clinical outcomes after using Novel deeper intubation technique (DIT) of ileus tube for acute bowel obstruction patients. Gastroenterol. Res. Pract. 15, 1625154 (2020).
Nagaike, K. et al. Radiation dose and factors related to exceeding the diagnostic reference level in 496 transnasal ileus tube placement procedures from the REX-GI study. Br. J. Radiol. 96(1146), 20230086 (2023).
Yamaguchi, D. et al. New insertion method of transnasal ileus tube for small bowel obstruction: Anterior balloon method. PLoS One 13(11), e0207099 (2018).
Yamaguchi, D., Morisaki, T. & Tsunada, S. Effective insertion method of transnasal ileus tube for adhesive small bowel obstruction. Dig. Endosc. 30, 120–121 (2018).
Guo, S. B. & Duan, Z. J. Decompression of the small bowel by endoscopic long-tube placement. World J. Gastroenterol. 18, 1822–1826 (2012).
Kanno, Y. et al. Long-tube insertion with the ropeway method facilitated by a guidewire placed by transnasal ultrathin endoscopy for bowel obstruction: A prospective, randomized, controlled trial. Gastrointest. Endosc. 69, 1363–1368 (2009).
Keller, R. T. A technique of intestinal intubation with the fiberoptic endoscope. Gut 14, 143–144 (1973).
Li, S., Yuan, C. & Xu, M. D. Two different endoscopic long intestinal tube placements for small bowel obstruction: Transnasal ultrathin endoscopy versus conventional endoscopy. J. Cancer Res. Ther. 11 Suppl, C248–C252 (2015).
Farrington, C. P. & Manning, G. Test statistics and sample size formulae for comparative binomial trials with null hypothesis of non-zero risk difference or non-unity relative risk. Stat. Med. 9, 1447–1454 (1990).
Cole, J. M. et al. Enhanced gastric decompression for palliation of malignant bowel obstruction. Surg. Endosc. 37, 4000–4004 (2023).
Zuo, L. et al. Strategy to small intestine obstruction caused by Crohn’s disease on the basis of transnasal ileus tube insertion. BMC Surg. 22(1), 183 (2022).
Liu, R. Q. et al. Prospective evaluation of intestinal decompression in treatment of acute bowel obstruction from Crohn’s disease. Gastroenterol. Rep. (Oxf) 7, 263–271 (2019).
Kubo, K., Hayasaka, S. & Tanaka, I. A fish bone embedded in the hypopharynx successfully extracted by cap-assisted endoscopy. Gastrointest. Endosc. 99, 1053–1054 (2024).
Wen, Q. et al. Impact of cap-assisted colonoscopy during transendoscopic enteral tubing: A randomized controlled trial. World J. Gastroenterol. 26, 6098–6110 (2020).
Kim, S. & Lee, B. I. The role of cap-assisted endoscopy and its future implications. Clin. Endosc. 57, 293–301 (2024).
Iqbal, U. et al. Efficacy of cap-assisted endoscopy for the visualization of the major duodenal papilla: A systematic review and meta-analysis. Gastrointest. Endosc. 98, 1004–1008 (2023).
Kazumori, H. & Sato, T. Ileus tube-assisted endoscopic detorsion as a useful initial management for cecal volvulus in a patient with septic shock. Endoscopy 56(S 01), E334–E335 (2024).
Nakanishi, R. et al. Acute infectious Purpura fulminans complicated by bacterial translocation after rectal cancer surgery: A case report. Med. (Kaunas) 60, 644 (2024).
Lin, S. W. et al. Assessing risk of recurrent small bowel obstruction after non-operative management in patients with history of intra-abdominal surgery: a population-based comprehensive analysis in Taiwan. Surg Endosc. 38, 2433–2443 (2024).
Funding
The Joint Funds for the Innovation of Science and Technology, Fujian Province, China. No.2023Y9414.
Author information
Authors and Affiliations
Contributions
Su-Yu Chen and Rui Huang and Yu Zhang contributed equally to this work. Su-Yu Chen, Rui Huang, Yu Zhang and Hong Shi were responsible for the study concept and design, including endoscopic procedures; Su-Yu Chen, Rui Huang, Yu Zhang, Zhao-Fei Xie, He Huang and Hong Shi conducted the endoscopic operations together; Su-Yu Chen drafted the manuscript; Su-Yu Chen and Hong Shi revised and finalized the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, SY., Huang, R., Zhang, Y. et al. A retrospective single-center study of transnasal ileus tube insertion accompanied with cap-assisted endoscopic advancement for malignant adhesive bowel obstruction. Sci Rep 14, 29227 (2024). https://doi.org/10.1038/s41598-024-80304-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-80304-6