Abstract
Several donor-specific factors influence the functional recovery and long-term outcomes of liver grafts. This study investigated the association between donor fasting glucose (DFG) and recipient outcomes after living donor liver transplantation (LDLT) in 950 cases at a single center. Patients were divided into two groups: low-DFG (< 85 mg/dL, n = 120) and control (≥ 85 mg/dL, n = 830). The five-year graft survival rate was significantly lower in the low-DFG group (71.5%) compared to the control group (80.0%) (P = 0.02). Multivariable Cox regression analysis showed that low DFG was independently associated with graft loss (hazard ratio 1.72, 95% CI 1.15–2.56, P = 0.008). In propensity score-matched groups, the low-DFG group also had lower survival rates (71% vs. 83.1%, P = 0.004). The presence of additional risk factors, such as low graft-to-recipient weight ratio, older donor age, and longer cold ischemic time, further reduced graft survival in the low-DFG group. A DFG level < 85 mg/dL is associated with higher risk of graft failure after LDLT, especially when combined with other risk factors. Low DFG should be considered a prognostic marker in LDLT planning, with potential to improve patient outcomes as further research clarifies the underlying pathophysiological mechanisms.
Similar content being viewed by others
Introduction
Liver transplantation is a curative treatment for liver cirrhosis, acute liver failure, and unresectable hepatocellular carcinoma. As the demand for organs far exceeds their supply, the need for living donor liver transplantation (LDLT) has increased1. When planning LDLT, donors should undergo an assessment to screen for possible chronic liver disease and underlying extrahepatic medical problems, including obesity, diabetes, and dyslipidemia2. Several donor-specific factors have been identified as significant contributors to both the functional recovery and long-term outcomes of liver grafts. Notably, these include donor age, sex, and the extent of fatty infiltration within the liver3,4. Despite meticulous screening and selection of living donors based on these criteria, early allograft dysfunction ensues in approximately 20% of cases post transplantation, adversely influencing the patient survival5.
Rationale and knowledge gap
Glucose production in the liver, the principal organ responsible for glucose regulation, occurs via glycogenolysis and gluconeogenesis during fasting6; however, in individuals with liver disease, the liver’s ability to maintain carbohydrate metabolism is compromised7. Hypoglycemia occurs because of decreased gluconeogenesis, altered glycogen storage, and malnutrition8, and patients with acute decompensated liver cirrhosis have a higher risk of mortality due to hypoglycemia9. Additionally, in cases in which hepatectomy has been performed, postoperative glucose control may not be achieved, which can lead to challenges associated with regeneration and poor prognosis10. Some patients with post-hepatectomy liver failure experience hypoglycemia, which is attributed to impaired hepatic gluconeogenesis, excessive insulin secretion, and reduced glycogen stores in the remaining liver11.
Decreased blood flow, hypoxia, and cytokine levels affect hepatic glucose metabolism12,13. It has been revealed that there is a relationship between decreased perfusion rates and reduced gluconeogenesis using rat livers14. However, there is no established research on whether a liver graft with impaired glucose metabolism affects recipient outcomes.
Objective
We hypothesized that liver grafts from living donors with fasting hypoglycemia could have intrinsic functional defects, resulting in poor LDLT outcomes. This study aimed to evaluate the relationship between low fasting glucose levels in living donors and graft survival after LDLT.
Methods
Patients and materials
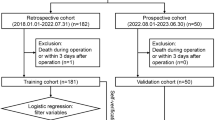
We considered patients who received LDLTs at Severance Hospital, Korea, between July 2005 and December 2022; a total of 1,059 patients. The exclusion criteria were as follows: age < 18 years (n = 92), dual-graft LDLT (n = 2), combined organ transplantation (n = 8), previously diagnosed donor diabetes mellitus (n = 5), and incomplete data (n = 2). Ultimately, 950 eligible patients were included in the study (Supplementary Fig. 1). Informed consent was not required because of the study’s retrospective design.
Definitions and outcomes
The recipient, donor, and operative characteristics were retrieved from the institutional liver transplantation database. The graft-to-recipient weight ratio (GRWR) was calculated using the following formula, with the graft weight measured immediately before implantation:
Graft type was divided into right or non-right lobes, primarily comprising left lobe grafts. Graft steatosis was further stratified into two groups: > 10% and ≤ 10% based on the intraoperative biopsy, with severe steatosis excluded when selecting living donors. Donor surgical methods included open or minimally invasive surgery (laparoscopic or robotic procedures). The primary outcome was graft survival, defined as the need for re-transplantation or death of the recipient. Follow up continued until graft loss occurred, five years after transplantation, or December 2022, whichever event occurred first.
Measurement and categorization of donor fasting glucose (DFG)
DFG levels were measured after at least 8 h of fasting and at least three days before the operation, along with other blood tests. To categorize the study population according to DFG levels, the relationship between DFG levels and graft survival was explored using a smoothing spline curve adjusted for other risk factors for graft survival (Fig. 1). In quantitative analysis of the threshold effect, the inflection point was determined to be 85 mg/dL for graft survival. Patients were categorized based on whether their fasting glucose levels were < 85 mg/dL (low DFG) or ≥ 85 mg/dL (control).
Adjusted smoothing spline curve for graft survival by donor fasting glucose (DFG). The graph shows the adjusted log hazard ratio (solid line) and the 95% confidence interval (dashed lines). This is estimated using the Cox proportional hazards model with body mass index, pre-transplantation model for end-stage liver disease score, pre-transplant hospital stay, re-transplantation, operation time, cold ischemic time, portal flow modulation, red blood cell transfusion, donor age, donor body mass index, ABO incompatibility, and graft type.
Propensity score matching
To decrease the risk of confounding bias, the low DFG and control groups were matched in a 1:3 ratio with the propensity score. Matching was performed using the nearest-neighbor method with a caliper of 0.1, discarding individuals who lacked a suitable match. An adequate balance of variables was considered when the standardized mean differences were < 0.115.
Statistical methods
Categorical variables were analyzed using the chi-square test or Fisher’s exact test, whereas continuous variables were compared using the t-test. Graft survival was assessed using the Kaplan–Meier method and statistical significance was determined using the log-rank test. Graft survival was defined as the duration from the date of surgery to the date of death from any cause or re-transplantation. For survival, univariate and multivariate analyses were conducted using the Cox proportional hazards regression model to evaluate variable associations. Variables with P-values less than 0.1 in the univariate analysis were identified and subsequently included in the multivariable Cox proportional hazards regression model to assess independent risk factors. The hazard ratio (HR) and 95% confidence intervals (CIs) were used for statistical analysis.
To elucidate the influence of DFG on the presence of other risk factors for LDLT, subgroup analysis was performed based on previously known risk factors for LDLT16. A GRWR < 1.0, cold ischemic time (CIT) of ≥ 150 min, and donor age of > 40 years were used as cutoffs for subgroups, established by adjusted smoothing spline curves for graft survival. Subgroup analyses were performed for four groups by low-DFG and binary risk groups, and then additionally performed for those who had two risk factors simultaneously versus others (e.g., low-DGF and donor age ≥ 40 vs. others). Multivariate Cox analyses, including subgroup analyses, were adjusted for the same covariates as those used in the analysis of the entire population.
All statistical analyses were performed using SPSS (SPSS Inc., Chicago, IL, USA) and R software (version 4.3.2; R-project, Institute for Statistics and Mathematics, Vienna, Austria). The threshold for statistical significance was set at P < 0.05.
Ethical approval
This study was performed following the Declaration of Helsinki and the Declaration of Istanbul. Study design was approved and the requirement for informed consent from the study subjects was waived by the Institutional Review Board at Severance Hospital, Yonsei University Health System (IRB No. 4–2024-1092).
Results
Baseline characteristics of patients
Among the 950 patients with LDLTs, two groups were established based on the fasting glucose level of the living donor: those with < 85 mg/dL (low-DFG group, n = 120) and those with > 85 mg/dL (control group, n = 830). The baseline characteristics of the patients are presented in Table 1. In terms of recipient characteristics, all other parameters, such as age, sex, body mass index (BMI), and pre-transplant model for end-stage liver disease (MELD) score, were equally distributed. The low-DFG group showed a younger donor age (32 [25.0–42.0] years vs. 29.5 [23.0–38.5] years, P = 0.03) and higher proportion of female donors (37.3% vs. 48.3%, P = 0.02) compared to the control group. There was no significant difference observed in donor BMI between the low-DFG group and control group (22.6 [20.7–24.6] kg/m2 vs. 23.0 [21.0–24.8] kg/m2, P = 0.11). The GRWR was similar between the two groups (1.1 [0.9–1.3] vs. 1.1 [1.0–1.3], P = 0.75). A comparison of macrovesicular steatosis greater than 10% revealed no significant differences between the low-DFG group and control group (10.5% vs. 14.8%, P = 0.28). Among the donor laboratory results, the low-DFG group showed lower aspartate aminotransferase (P = 0.02), alanine transaminase (P = 0.02), and hemoglobin (P = 0.01) levels than the control group, although the differences were not significant (Supplementary table 1).
After propensity score matching, no statistically significant differences were observed between the low-DFG and control groups across all 40 characteristics examined (Table 1 and Supplementary table 1). The standardized differences for all covariates before and after propensity score matching are presented in Table 1 and Supplementary Fig. 2.
Recipient outcome
The median follow-up period was 50.1 [19.5–97.3] months. During follow-up, 33 (27.5%) patients in the low-DFG group died and seven (5.8%) patients underwent re-transplantation. In the control group, 169 (20.4%) patients died and 34 (4.1%) patients underwent re-transplantation.
The changes in recipient glucose levels were assessed serially from pre-transplant to one month post-transplant, but no significant differences were identified between the two groups (Supplementary Fig. 3). Early allograft dysfunction was analyzed for its potential influence, but with 9 cases (8.1%) in the low-DFG group and 63 (7.8%) in the control group, no significant difference was observed (P = 0.999; Supplementary table 2).
The low-DFG group had significantly poorer graft survival than that of the control group (83.3%, 76.6%, and 71.5% in the low-DFG group vs. 89.5%, 83.7%, and 80.0% in the control group at one, three, and five years, P = 0.024; Fig. 2A). This result remained consistent even after propensity score matching (five-year graft survival rates: 83.3%, 76.3%, and 71.0% vs. 92.3%, 86.7%, and 83.1%, respectively; P = 0.004; Fig. 2B).
Graft survival curves according to DFG. (A) Five-year graft survival between the low-DFG group and control group. (B) Graft survival curves according to donor fasting glucose after propensity score matching. Donor fasting glucose is categorized according to whether the fasting glucose of donors is < 85 mg/dL (low-DFG group) or ≥ 85 mg/dL (control group). LT liver transplant, DFG donor fasting glucose.
In the uni- and multivariable Cox regression, low DFG was an independent risk factor for graft loss (HR = 1.72, 95% CI 1.15–2.56, P = 0.008; Table 2). Other risk factors were higher BMI (HR = 0.94, 95% CI 0.89–0.98, P = 0.005), above milan criteria in hepatocellular carcinoma (HR = 2.55, 95% CI 1.72–3.79, P < 0.001), a higher pretransplant MELD score (HR = 1.03, 95% CI 1.0–1.05, P = 0.02), a longer pretransplant stay in the intensive care unit (HR = 3.71, 95% CI 1.66–8.31, P = 0.001), intraoperative red blood cell transfusion (HR = 1.03, 95% CI 1.02–1.04, P < 0.001), and other than right lobe graft (HR = 1.90, 95% CI 1.01–3.57, P = 0.04).
In the analysis of graft loss causes (Supplementary table 4), rejection was the most common in the low-DFG group, with 3 out of 7 cases (42.9%), while biliary complications were the most frequent in the control group, with 6 out of 34 cases (17.6%). The most frequent cause of patient death in both groups was infection, with 13 cases (40.6%) in the low-DFG group and 44 cases (26%) in the control group.
Donor post-operative course
Supplementary Fig. 4 presents the pre- and post-operative changes in donor AST, ALT, bilirubin, and INR levels, showing no significant differences between the two groups. Donor fasting glucose levels did not show statistically significant difference. There was no donor mortality in both group, and incidence of major post-operative complication (Clavien-Dindo grade III or more) was similar between the low-DFG group and the control group (1.7% vs. 3.6%, P = 0.633, Table 3).
Donor fasting glucose and other risk factors in LDLT
Figure 3 shows a comparison of graft survival between subgroups according to the presence of low DFG or other risk factors. When patients had low DFG and a GRWR < 1.0 (80.8%, 69.1%, and 65.3% at one, three, and five years, respectively), graft survival was significantly lower than that of the others (89.1%, 83.4%, and 79.5% at one, three, and five years, respectively; P = 0.20). Moreover, when patients had low DFG and CIT ≥ 150 min (73.6%, 68.1%, and 61.1% at one, three, and five years, respectively), graft survival was significantly lower than that of others (89.4%, 83.4%, and 79.7% at one, three, and five years, respectively, P = 0.003). Furthermore, when patients had low DFG and a donor age ≥ 40 years (75.4%, 61.2%, and 61.2% at one, three, and five years, respectively), graft survival was significantly lower than that of the others (89.1%, 83.3%, and 79.4% at one, three, and five years, respectively, P = 0.001).
When those subgroups with low DFG and another risk factor were inputted in the multivariable models, low DFG + CIT ≥ 150 min (HR 1.87, 95% CI 1.03–3.38, P = 0.04; Supplementary table 5) and low DFG + donor age ≥ 40 years (HR 2.18, 95% CI 1.08–4.42, P = 0.03; Supplementary table 6) were significant risk factors for graft survival, although the result for low DFG + GRWR < 1.0 was marginal (HR 1.71, 95% CI 0.94–3.11, P = 0.08; Supplementary table 7).
Discussion
The liver is the major organ involved in gluconeogenesis, and previous studies have shown an association between impaired liver function and hypoglycemia. We hypothesized that living liver donors who showed impaired or marginal regulation of hypoglycemia possibly had intrinsic defects in liver functional capacity, which resulted in poor graft survival after transplantation, despite normal liver function test results. Our results demonstrated that a low preoperative DFG (< 85 mg/dL) was associated with a significant risk of graft failure after LDLT. These hazardous effects of low DFG were more prominent when other risk factors were present, such as a lower GRWR, longer CIT, and older donor age.
Patients with lower fasting glucose levels (< 85 mg/dL), for whom the criteria employed in this study did not meet the literal definition of hypoglycemia (< 70 mg/dL)17, were evaluated as having normal liver function and no obvious comorbidities. Altered liver function may not be distinctly evident in healthy liver donors because of compensation from other organs, such as the kidney18. However, after donor hepatectomy and transplantation, factors such as reduced volume and a compromised medical condition of the recipient could render donor livers with lower fasting glucose levels more vulnerable, even within the euglycemic range (80–85 mg/dL)19, potentially leading to graft failure. This is the first study to our knowledge to evaluate the relationship between donor glucose levels and LDLT outcomes using large-volume, single-center data.
Low DFG may have acted as a concealed predictor of impaired function of the donor liver, although the precise cause behind the finding that low DFG independently lowered graft survival is not clearly defined. The liver plays a crucial role in blood sugar regulation through the synthesis, storage, decomposition, and release of glycogen20, and hypoglycemic episodes are well-recognized as poor prognostic factors for patients with cirrhosis and hepatocellular carcinoma21. Therefore, hypothetically, livers with lower fasting glucose levels may exhibit subtle impairments in liver function, including alterations in hepatic gluconeogenesis22.
Gluconeogenesis is essential for survival as it provides glucose derivatives to synthesize normal constituents of cell membranes and dispose of lactate produced by glycolysis, thus mitigating metabolic acidosis23. In addition, improving glucose levels during surgery can protect the liver from ischemia–reperfusion injury by preventing adenosine triphosphate depletion24 and improving recovery during organ preservation25,26. A recent study reported that phosphoenolpyruvate carboxykinase 1, one of the rate-limiting enzyme of gluconeogenesis, was markedly upregulated in human post-ischemia–reperfusion liver specimens and mouse models23. This upregulation is associated with a more favorable prognosis for liver transplantation, whereas its inhibition exacerbates hepatic injury. While we could not directly confirm this mechanism in our study, this study suggests that livers with impaired hepatic gluconeogenesis may be relatively vulnerable to damage after transplantation compared to livers without such impairment. Donor evaluation is conducted with the objective of identifying any potential conditions that might heighten the risk of perioperative complications in the healthy donor. Transplant surgery is performed with a primary emphasis on donor safety and recipient prognosis. The criteria for donor selection includes age, BMI, remnant liver volume, GRWR, anatomical suitability for donation, and presence of fatty liver to determine eligibility27. In order to aid in donor selection, Goldberg et al.28 have developed a risk index that incorporates donor and recipient factors, which can predict graft survival. However, it has limitations as it is predominantly composed of recipient factors, making it challenging to consider during donor selection. Despite its informative value, the model could benefit from additional donor-related variables that enhance its applicability during the selection process. Donor glucose levels can also be considered when making donor selection decisions.
This was a retrospective study conducted at a single center, and there could have been selection bias in the detailed analysis. In addition, factors that may affect liver function, such as alcohol consumption history, family history, and dietary habits, were not considered. However, propensity score matching analysis was conducted to adjust for differences between the two groups. A notable limitation of this study was the lack of a comprehensive understanding of the pathophysiological mechanisms underlying these phenomena. Further research is required to clarify these intricate molecular and cellular processes and to confirm whether consistent findings can be replicated in large cohort studies.
As preoperative blood glucose levels are routinely measured in all patients, further research is necessary to elucidate the potential mechanisms related to liver regeneration and glucose metabolism. This study highlights the need to consider donor glucose levels as an attainable criterion for organ allocation and the optimization of graft outcomes. Understanding the influence of glucose levels on graft outcomes can lead to more informed decisions regarding donor selection and posttransplant management.
Conclusions
DFG < 85 mg/dL was associated with an elevated risk of graft failure after LDLT, especially when combined with a lower GRWR, longer CIT, and older donor age. Low DFG should be considered a potential prognostic marker when planning LDLT, although further studies are needed to determine the pathophysiological correlation.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Change history
17 March 2025
A Correction to this paper has been published: https://doi.org/10.1038/s41598-025-93291-z
References
Goldaracena, N. & Barbas, A. S. Living donor liver transplantation. Curr. Opin. Organ. Transplant 24, 131–137. https://doi.org/10.1097/mot.0000000000000610 (2019).
Miller, C. M. et al. The international liver transplantation society living donor liver transplant recipient guideline. Transplantation 101, 938–944. https://doi.org/10.1097/TP.0000000000001571 (2017).
Lué, A. et al. How important is donor age in liver transplantation?. World J. Gastroenterol. 22, 4966–4976. https://doi.org/10.3748/wjg.v22.i21.4966 (2016).
Chu, M. J., Dare, A. J., Phillips, A. R. & Bartlett, A. S. Donor hepatic steatosis and outcome after liver transplantation: A systematic review. J. Gastrointest. Surg. 19, 1713–1724 (2015).
Agrawal, D. & Saigal, S. Early allograft dysfunction after living donor liver transplantation-current concepts and future directions. Liver Transpl 29, 871–884. https://doi.org/10.1097/lvt.0000000000000173 (2023).
Adeva-Andany, M. M., Pérez-Felpete, N., Fernández-Fernández, C., Donapetry-García, C. & Pazos-García, C. Liver glucose metabolism in humans. Biosci. Rep. https://doi.org/10.1042/bsr20160385 (2016).
Kawaguchi, T. et al. Insulin resistance and chronic liver disease. World J. Hepatol. 3, 99 (2011).
Arky, R. A. Hypoglycemia associated with liver disease and ethanol. Endocrinol. Metab. Clin. North Am. 18, 75–90 (1989).
Pfortmueller, C. A. et al. Hypoglycemia is associated with increased mortality in patients with acute decompensated liver cirrhosis. J. Crit. Care 29(316), e317–e312. https://doi.org/10.1016/j.jcrc.2013.11.002 (2014).
Luo, J. et al. Diabetes mellitus and postoperative blood glucose value help predict posthepatectomy liver failure in patients with hepatocellular carcinoma. J. Gastrointest. Oncol. 12, 2377 (2021).
Søreide, J. A. & Deshpande, R. Post hepatectomy liver failure (PHLF) - Recent advances in prevention and clinical management. Eur. J. Surg. Oncol. 47, 216–224. https://doi.org/10.1016/j.ejso.2020.09.001 (2021).
Villalobos-Molina, R., Saavedra-Molina, A. & Devlin, T. M. Effect of hypoxia and reoxygenation on metabolic pathways in rat hepatocytes. Arch. Med. Res. 29, 219–223 (1998).
Mallett, S. et al. in Transplantation proceedings, p. 3529–3529.
Sumida, K. D., Urdiales, J. H. & Donovan, C. M. Impact of flow rate on lactate uptake and gluconeogenesis in glucagon-stimulated perfused livers. Am. J. Physiol.-Endocrinol. Metabol. 290, E185–E191 (2006).
Austin, P. C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 28, 3083–3107. https://doi.org/10.1002/sim.3697 (2009).
Kim, D.-G. et al. Outcomes and risk factors for liver transplantation using graft-to-recipient weight ratio less than 0.8 graft from living donors: multicentric cohort study. Ann, Surgery https://doi.org/10.1097/SLA.0000000000006104 (2024).
Davis, S. N. & Cryer, P. E. in Harrison’s Principles of Internal Medicine, 21e (eds Joseph Loscalzo et al.) (McGraw-Hill Education, 2022).
Lauritsen, T. L., Grunnet, N., Rasmussen, A., Secher, N. H. & Quistorff, B. The effect of hepatectomy on glucose homeostasis in pig and in man. J. Hepatol. 36, 99–104. https://doi.org/10.1016/s0168-8278(01)00241-0 (2002).
Cheng, K. W. et al. Comparison of glucose loads and blood glucose changes in patients with and without diabetes mellitus undergoing living donor liver transplantation. Transplant Proc. 52, 1794–1797. https://doi.org/10.1016/j.transproceed.2020.01.143 (2020).
Rui, L. Energy metabolism in the liver. Compr. Physiol. 4, 177–197. https://doi.org/10.1002/cphy.c130024 (2014).
Hung, T. H., Tseng, C. W., Tsai, C. C. & Lee, H. F. Prognosis of hypoglycemia episode in cirrhotic patients during hospitalization. BMC Gastroenterol. 21, 319. https://doi.org/10.1186/s12876-021-01895-2 (2021).
Changani, K. K. et al. Evidence for altered hepatic gluconeogenesis in patients with cirrhosis using in vivo 31-phosphorus magnetic resonance spectroscopy. Gut 49, 557–564. https://doi.org/10.1136/gut.49.4.557 (2001).
Yu, S. et al. m6A-mediated gluconeogenic enzyme PCK1 upregulation protects against hepatic ischemia-reperfusion injury. Hepatology https://doi.org/10.1097/hep.0000000000000716 (2023).
Nishimura, Y., Romer, L. H. & Lemasters, J. J. Mitochondrial dysfunction and cytoskeletal disruption during chemical hypoxia to cultured rat hepatic sinusoidal endothelial cells: the pH paradox and cytoprotection by glucose, acidotic pH, and glycine. Hepatology 27, 1039–1049. https://doi.org/10.1002/hep.510270420 (1998).
Dimicoli, J. L. et al. A magnetic resonance study of the effect of nutritional status on cold-preserved murine liver. Gastroenterology 107, 1764–1773. https://doi.org/10.1016/0016-5085(94)90819-2 (1994).
Cywes, R. et al. Effect of intraportal glucose infusion on hepatic glycogen content and degradation, and outcome of liver transplantation. Ann. Surg. 216, 235–246. https://doi.org/10.1097/00000658-199209000-00003 (1992) (discussion 246-237).
Rela, M. & Rammohan, A. Patient and donor selection in living donor liver transplantation. Digest. Med. Res. 3 (2020).
Goldberg, D. S., French, B., Abt, P. L., Olthoff, K. & Shaked, A. Superior survival using living donors and donor-recipient matching using a novel living donor risk index. Hepatology 60, 1717–1726 (2014).
Acknowledgements
The authors thank the members of the Organ Transplant Support Team at the Severance Hospital for their support in conducting this study.
Author information
Authors and Affiliations
Contributions
D.G.K. has full access to all aspects of the study and takes responsibility for the integrity of the data and accuracy of the data analysis; H.H.K, and D.G.K. participated in the research design; M.L, M.K, S.H.Y., M.C.C, E.K.M., J.G.L., D.J.J., and M.S.K. participated in performing the research; H.H.K, M.K, S.H.Y, and M.C.C participated in the data acquisition; H.H.K, and D.G.K. participated in the statistical analysis; H.H.K. participated in the writing of the paper; J.S.L and D.G.K. supervised the study. All the authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: In the original version of this Article, Jae Seung Lee was omitted as a corresponding author. Furthermore, Jae Seung Lee and Deok-Gie Kim were omitted as equally contributing authors. Full information regarding the corrections made can be found in the correction for this Article.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Koh, HH., Lee, M., Kang, M. et al. Association between low fasting glucose of the living donor and risk of graft loss in the recipient after liver transplantation. Sci Rep 15, 951 (2025). https://doi.org/10.1038/s41598-024-80604-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-80604-x