Abstract
Recently, neoadjuvant short-course radiation therapy (SCRT) has emerged as a valid treatment option for patients with locally advanced rectal cancer (LARC). We assessed SCRT plans using volumetric-modulated arc therapy (VMAT) with Halcyon and Infinity medical linear accelerators (Linacs) and compared the plan quality and delivery efficiency across all cases. Thirty patients who underwent preoperative SCRT for LARC at the hospital were randomly selected. Treatment plans were designed using the Halcyon and Infinity linac platforms, generating Halcyon VMAT plans (Group H) and Infinity VMAT plans (Group I). The target coverage, organ at risk (OAR) dose distribution, number of monitor units, treatment delivery time, and planning complexity of the two groups were compared and analyzed. Plan quality assurance was performed on the ArcCheck phantom. The overall plan quality regarding target volume and OARs was comparable for plans delivered on Halcyon and Infinity Agility machines, with each platform having advantages. Therefore, both radiotherapy platforms are very good options when selecting which technique to use in the clinic.
Similar content being viewed by others
Introduction
The current standard treatment for locally advanced rectal cancer (LARC) involves preoperative concurrent chemoradiation followed by total mesorectal excision (TME). Total neoadjuvant therapy (TNT) is the recommended treatment strategy for LARC. It provides both systemic chemotherapy and neoadjuvant (chemo)radiotherapy before surgery1. Long-course radiotherapy (LCRT) and short-course radiotherapy (SCRT) are two modalities of preoperative neoadjuvant radiotherapy that are equally effective in terms of overall survival, tumor downstaging, and reducing the risk of local recurrence2,3. SCRT has gained increased interest in the treatment of LARC owing to the lower number of treatment cycles involved and higher rates of patient compliance1,4.
Compared with traditional three dimensional conformal radiotherapy (3D-CRT) and intensity modulated radiotherapy (IMRT)5,6, the advantages of the volumetric modulated arc therapy (VMAT) technique include increased treatment accuracy, delivery efficiency and more comfortable target dose distribution, along with better sparing of normal tissues7,8; thus, VMAT has been widely used for LARC in the clinic9,10,11.
The Varian Halcyon linear accelerator (Linac) (Varian Medical Systems, Palo Alto, CA) was recently introduced and is a novel "O-ring" Linac designed with a tungsten-free collimator and a flattening filter-free (FFF) mode. This system is configured with a double-stack multileaf collimator (MLC) to reduce scatter and achieve a maximum 28 cm × 28 cm field size, a 6 MV FFF beam with a high gantry rotation speed of up to 24°/s, and a leaf speed of 5 cm/s12. Additionally, the Elekta Infinity Linac (Elekta AB, Stockholm, Sweden) is a typical C-arm gantry machine equipped with the Agility MLC. The Agility system provides multiple energy beam options (6 MV, 10 MV, 6 MV FFF, and 10 MV FFF) and has 160 leaves with 80 pairs. The maximum field size is 40 cm × 40 cm, with a maximum leaf speed of up to 65 mm/s13. Fathy et al.14 reported that the Agility MLC was associated with better plan dosimetric parameters and a shorter treatment time than the MLCi2, which is Elekta’s second-generation MLC, typically installed in older machines such as the Precise. There are several studies on the differences in various techniques (intensity modulated radiotherapy (IMRT), VMAT, and proton therapy (PT)) for SCRT of rectal cancer15,16,17. Although several studies, including a multicentric comparison of VMAT techniques using different treatment planning systems16, have explored dosimetric performance in rectal cancer, there remains a gap in the literature specifically comparing the dosimetric characteristics of VMAT delivered on different linear accelerator platforms for preoperative short-course radiation therapy in locally advanced rectal cancer. This study aims to address this gap by comparing VMAT plans generated using Halcyon and Infinity linacs, focusing on both dosimetric performance and clinical feasibility. The aim of this study was to compare the plan quality and delivery efficiency of Halcyon VMAT and Infinity VMAT for LARC in preoperative SCRT and to provide a scientific basis and reference for the selection and use of clinical equipment.
Materials and methods
Patient selection
Thirty patients with clinical stage T3a-T4a rectal cancer who received preoperative SCRT in our clinic between January 2022 and November 2023 were retrospectively selected. The median age of the patients was 61 years, and 77% were male. All of the patients were diagnosed with rectal adenocarcinoma through pathological histological examination. All patient data were anonymized, and the study protocol was approved by the ethics committee of Sir Run Run Shaw Hospital.
Definition of target volumes
All patients underwent computed tomography (CT) simulation in the prone position on a prone board with an abdominal hole and a full bladder. Planning CT scans were acquired with a slice thickness of 3 mm.
The clinical target volume (CTV) included the gross tumor volume (GTV), the complete mesorectal fascia, and the presacral nodes, internal iliac, and obturator lymph nodes. The planning target volume (PTV) was generated by adding a 0.3 cm margin to the CTV, and the small intestine, bladder, left and right femoral heads, and pelvic bone marrow were defined as the organs at risk (OARs). All patients’ target volumes were contoured on fused magnetic resonance imaging (MRI)-CT planning images by the same experienced clinician, following international consensus guidelines18,19 and after multidisciplinary team (MDT) discussions1.
Treatment planning and evaluation
All treatment plans were generated using the Collapsed Cone (CC optimization algorithm and 6 MV FFF beam energy in the RayStation 9A planning system (RaySearch Medical Laboratories AB, Stockholm, Sweden). The dose calculation grid was set to 2.5 mm × 2.5 mm × 2.5 mm. The Infinity VMAT (Group I) and Halcyon VMAT (Group H) plans had a prescribed dose of 25 Gy in 5 fractions. In Group H plans, a maximum dose rate of 800 MU/min was utilized, whereas in Group I plans, a maximum dose rate of 1400 MU/min was utilized. In all VMAT plans, two partial arcs from 204° to 156° and reversed were used11, owing to the complexity of the concave target volume, to reduce the volume of the small intestine receiving radiation. The same planning optimization objectives and constraints were used, and the control point spacing for both sets of plans during optimization was set to 2 degrees. Three consecutive optimization processes were performed, with each process including up to 80 iterations.The following constraints were met for the treatment plan, as previously published20:
Pelvic bone marrow: as low as reasonably achievable, avoiding hotspots. For each patient, the mean dose (Dmean), maximum dose (D2%), minimum dose (D98%), conformity index (CI)21, homogeneity index (HI)21, and gradient index (GI)22 were calculated for PTV.
The OAR analyses included the volume and Dmean. Additionally, the percentage or absolute volume receiving doses of 5 Gy, 10 Gy, 15 Gy, 20 Gy, and 25 Gy was calculated for the small intestine, bladder, femoral head, and pelvic bone marrow.
In addition to dose‒volume metrics, Group H and Group I plans were compared concerning the total number of MUs, beam-on time and modulation complexity score (MCS)23. The MCS ranges from 0 upwards, with higher values indicating greater modulation.
Statistical analysis
All the data were tested for normality via the Shapiro‒Wilk (S‒W) test. A comparison between the two groups was performed using a paired-sample t test for normally distributed intergroup data. A difference was considered statistically significant at P < 0.05. Continuous variables that did not follow a normal distribution were analyzed using the paired non-parametric Wilcoxon signed-rank test. The significance level (α) was set at 0.05 (two-tailed). Measurement data are presented as mean ± standard deviation (x̅ ± s).
Results
Dosimetric data of target volumes and OARs
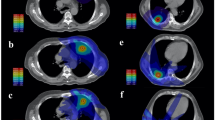
The mean volumes of PTV and CTV for the 30 patients were 792.7 cm3 (141.9) and 606.0 cm3 (112.6), respectively. The dosimetric results of PTV for the Halcyon and Infinity VMAT plans are presented in Table 1. With similar PTV coverage, Group I plans had significantly lower D2% and GI values than Group H plans, while there were no clinical differences in D98%, Dmean, D50%, HI, or CI between the plans. Figure 1 shows the dose distributions, dose–volume histograms (DVHs), and dose differences between the plans for the same patient. There were slight variations in the dose distributions and related DVHs between the plans for the same patient.
Both groups with FFF-VMAT techniques met the clinical acceptance criteria of the plan and provided better OAR sparing. The OAR dosimetric parameters for the Group H and Group I plans are shown in Table 2.
For the bladder and pelvic bone marrow, Group H plans exhibited evaluation metrics similar to Group I plans, except for significantly lower V5 of pelvic bone marrow and significantly higher V15 of the bladder. No significant differences or only negligible differences in V10, V25, or Dmean between the groups.
Compared with Group H plans, Group I plans had significantly lower V10, V15, V23 and D2% values, as well as significantly higher V5 values for the small intestine. Additionally, Group I plans showed significantly lower V5 and Dmean values for the left and right femoral heads. However, there were no significant differences in V18, Dmean or femoral head V15 values between the groups.
Plan quality and delivery verification
The total number of MUs, MCS and average beam-on time are shown in Table 3. In terms of plan quality, the total number of MUs and beam-on time for Group H plans were significantly greater than those for Group I plans. However, the MCS of Group H plans was significantly lower than that of Group I plans.
Dosimetric verification of the two groups of VMAT plans was performed with ArcCheck phantom (Sun Nuclear Corporation, Melbourne, FL, USA) and SNC patient software. The gamma passing rates for the 3 mm/3% (according to TG-218) criterion were higher than 95% for both groups, thereby meeting the quality assurance requirements of our clinic.
Discussion
Radiotherapy plays a critical role in TNT for preoperative LARC patients. However, with the emergence of new Linacs, a remaining issue in treatment planning is determining which technique to adopt to achieve optimal dose distribution, improve treatment efficiency, and reduce plan complexity, all while ensuring treatment accuracy.
The benefit of the FFF-VMAT technique is increased delivery efficiency, as its higher dose rates mean that the modulation range of the dose rate can be increased, likely reducing the treatment time at a single control point. However, the FFF-VMAT technique is also affected by linac limitations, such as gantry rotation speed and MLC speed.
In this study, we compared Halcyon VMAT and Infinity VMAT for preoperative SCRT of LARC. The results indicate that plans based on the Infinity + RayStation platform performed equally or better in terms of controlling target hotspots, cold spots and dose falloff outside the target compared with Halcyon VMAT in all cases. This performance may be attibuted to the Infinity Agility systems, which offer a much higher MLC speed (65 mm/s), reduced leakage, narrower penumbra width, and a higher available dose rate (1400 MU/min). These findings are consistent with previous reports14,24,25,26 on prostate cancer, cervical cancer, and thoracoabdominal tumors.
Regarding OAR doses, the plans based on the Halcyon + RayStation platform showed significantly lower V5 values for the bladder, bowel bag, and pelvic bone marrow compared to those in Group I plans.
However, Group H plans exhibited higher values than Group I plans for the bladder V15 and V21, bowel bag V10, V15, V23, and D2%, and the left and right femoral head V5 and Dmean. For concave targets such as those used in adjuvant radiotherapy for rectal cancer, better target conformality and faster edge dose fall-off are highly important, as they reduce the exposure of surrounding normal tissue to scattered doses.
The two accelerators, Halcyon and Infinity, each have distinct advantages in terms of dose distribution for different OARs, likely due to their unique performance characteristics. First, the Halcyon accelerator has a maximum dose rate of 800 MU/min and a gantry rotation speed of 12 degrees per second in treatment mode, whereas the Infinity accelerator has a dose rate of 1400 MU/min and a speed of 6 degrees per second. In VMAT plan optimization with variable dose rate, the Infinity accelerator offers a wider modulation range of dose rate, whereas the Halcyon accelerator provides a greater modulation range of gantry rotation speeds.
Secondly, both accelerators feature an MLC modulation precision of 0.5 cm. However, the Halcyon MLC moves at a speed of 5 cm/s, whereas the Infinity MLC moves at a speed of 6.5 cm/s. A higher MLC motion speed allows for more flexible adjustments to the radiation field shape, thereby better protecting the OARs.
Furthermore, the MLC lateral modulation range is a critical parameter. The Halcyon MLC has a lateral modulation range of 28 cm, whereas the Infinity MLC over-center modulation range is 15 cm, with the combined span of the motion of the two MLCs exceeding 35 cm. This larger MLC modulation range facilitates more flexible adjustments to the radiation field shape, increasing OAR protection.
Finally, the Halcyon MLC has two layers, with each layer being 7.7 cm thick, whereas the Infinity MLC is 9 cm thick and is equipped with a Y-direction jaw-following system. Due to reduced MLC leakage and interleaf transmission, the use of Group H plans resulted in much lower doses (V5) to OARs, consistent with the findings of Richter et al.27, thus maximally spare OARs.
In terms of delivery efficiency, Group I plans reduced the beam-on time (by approximately 18.6%) but increased the plan complexity compared to Group H plans. To achieve a clinically acceptable dose distribution, a certain level of plan complexity is necessary28. However, plans with excessive modulation involve a high degree of complexity, which may affect the overall accuracy of the treatment23,29. When the Elekta Infinity Linac is used to design FFF-VMAT plans, a high degree of modulation results in a significantly higher number of MUs. Based on the clinical physicist’s experience in the optimization of infinity plans, the number of MUs for each arc is limited to 750, resulting in an average of 1509.68 ± 42.66 MUs for Group I plans. Specifically, human intervention decreases the average beam-on time by approximately 20 s.
SCRT is a type of hypofractionation, and image-guided radiation therapy (IGRT) before each treatment is essential for rectal cancer patients8. LARC patients treated with IGRT + IMRT have fewer acute gastrointestinal adverse effects and higher local control rates30. IGRT is performed on Halcyon for daily treatment, improving treatment accuracy and stability31. Although the beam-on time for Infinity is shorter, Halcyon accelerator offers one-step setup for automatic couch shifts to the isocenter, automated field sequencing and delivery, and faster gantry rotation, resulting in less time spent in actual treatment compared to Infinity32.
For rectal cancer SCRT, Jeans et al.15 reported that pencil beam scanning proton therapy (PBS-PT) provided dosimetric results superior to those of three-dimensional conformal radiation therapy (3D-CRT) and VMAT plans in critical organs such as the small intestine, bladder, and femoral head while maintaining similar target coverage. Pedone et al.17 compared the effects of PBT-PT and VMAT in SCRT for 20 patients with LARC and reported that compared with photon therapy, PT clearly protected normal tissues, reducing the radiation dose to OARs. Specifically, the volumes of the bowel bag at V5Gy, V10Gy, V15Gy, and V25Gy for the PT plans vs. VMAT plans were (712.8 ± 329.7) vs. (247.1 ± 132.3), (461.5 ± 230.9) vs. (182.9 ± 102.9), (215.3 ± 136.4) vs. (141.2 ± 83.6), and (17.9 ± 18.2) vs. (23.6 ± 26.3), respectively. Our work complements their study by further evaluating the differences in VMAT plans with different accelerator models for SCRT, providing more options for clinical practice.
According to the RAPIDO trial4, diarrhea was the most common gastrointestinal toxicity during preoperative treatment in both the SCRT and LCRT groups, making limiting the radiation dose to the intestines crucial. Baglan et al.33 reported a strong correlation between the volume of the small bowel receiving 15 Gy (V15Gy) and the incidence of toxicity. When V15Gy was < 150 cc, the occurrence of grade 2 + toxicity was lower; among patients with V15Gy > 300 cc, most experienced grade 3 + acute small bowel toxicity. The findings of Robertson et al.34 subsequently confirmed this, demonstrating that when V15Gy was ≤ 130 cc, the incidence of grade 3 diarrhea was 11%. These findings suggest that V15Gy, along with other intermediate dose levels, such as V20Gy and V25Gy, are crucial parameters for predicting the occurrence of diarrhea. Holyoake et al.35 reported that multiple small intestine dose volumes (V5Gy, V10Gy, V30Gy and V45Gy) can predict toxicity risk, with V10Gy being the most significant. Our results effectively reduced these key indicators, thereby reducing the occurrence of toxic reactions.
The pelvic bone marrow is the primary site for adult hematopoiesis. A correlation between myelosuppression and the volume of bone exposed to radiation has been reported36.The dosimetric results from our two groups were similar, with both plans effectively reducing the incidence of acute myelosuppression toxicity.
One limitation of our study is that we did not compare techniques other than FFF-VMAT. However, VMAT has become more widely used in radiotherapy and has demonstrated specific advantages in clinical practice9,10,12,37,38. Furthermore, the dosimetric differences observed between the two systems have potential clinical implications. For example, higher dose levels in the bowel bag may increase the risk of radiation-induced enteritis, while elevated V10 values in the pelvic bone marrow could impact hematopoietic function. Additionally, this clinical dosimetric evaluation was based on simulated radiotherapy plans, eliminating variability related to patient-specific factors such as comorbidities or tumor biology. Despite these limitations, our study provides a valuable clinical reference for SCRT in the management of LARC, contributing to the optimization of treatment safety and efficacy.
Conclusions
For preoperative neoadjuvant SCRT for rectal cancer, the overall plan quality in terms of target coverage and OAR dose distribution was comparable between the Halcyon and Infinity Agility machines, with each system offering its own advantages. With respect to treatment efficiency, Halcyon VMAT plan was associated with a higher number of MUs and beam-on time, but the actual delivery time was similar to or even less than that of the Infinity VMAT plan when IGRT was incorporated. Additionally, Halcyon VMAT plans were less complex. Therefore, both radiotherapy platforms are very good options when selecting which technique to use in the clinic.
Data availability
The datasets generated and analyzed during the current study are not publicly available due to institutional data protection law and confidentiality of patient data but are available from the corresponding author on reasonable request in person.
References
Benson, A. B. et al. Rectal cancer, Version 2.2022, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Canc. Netw. 20, 1139–1167 (2022).
Jin, J. et al. Multicenter, randomized, phase III trial of short-term radiotherapy plus chemotherapy versus long-term chemoradiotherapy in locally advanced rectal cancer (STELLAR). Journal of Clinical Oncology 40, 1681–1692 (2022).
Ngan, S. Y. et al. Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman radiation oncology group trial 01.04. Journal of Clinical Oncology 30, 3827–3833 (2012).
van der Valk, M. J. M. et al. Compliance and tolerability of short-course radiotherapy followed by preoperative chemotherapy and surgery for high-risk rectal cancer – Results of the international randomized RAPIDO-trial. Radiotherapy and Oncology 147, 75–83 (2020).
Palma, D. et al. Volumetric modulated arc therapy for delivery of prostate radiotherapy: Comparison with intensity-modulated radiotherapy and three-dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys. 72, (2008).
Wen, G. et al. Dosimetric comparison of volumetric modulated arc therapy (VMAT), 5F intensity modulated radiotherapy (IMRT) and 3D conformal radiotherapy (3DCRT) in rectal carcinoma receiving neoadjuvant chemoradiotherapy. Int J Med Phys Clin Eng Radiat Oncol. 04, (2015).
Chiavassa, S., Bessieres, I., Edouard, M., Mathot, M. & Moignier, A. Complexity metrics for IMRT and VMAT plans: A review of current literature and applications. British Journal of Radiology. 92. https://doi.org/10.1259/bjr.20190270 (2019).
Hunte, S. O., Clark, C. H., Zyuzikov, N. & Nisbet, A. Volumetric modulated arc therapy (VMAT): A review of clinical outcomes—what is the clinical evidence for the most effective implementation? Br J Radiol. 95, (2022).
Yamashita, H. et al. Comparison of volumetric-modulated arc therapy using simultaneous integrated boosts (SIB-VMAT) of 45 Gy/55 Gy in 25 fractions with conventional radiotherapy in preoperative chemoradiation for rectal cancers: A propensity score case-matched analysis. Radiation Oncology 12, 156 (2017).
Shang, J. et al. VMAT planning study in rectal cancer patients. Radiation Oncology 9, 219 (2014).
Zhang, Z. et al. Advantages and robustness of partial VMAT with prone position for neoadjuvant rectal cancer evaluated by CBCT-based offline adaptive radiotherapy. Radiation Oncology 18, 102 (2023).
Li, C. et al. Plan quality comparison for cervical carcinoma treated with halcyon and trilogy intensity-modulated radiotherapy. J Cancer 10, 6135–6141 (2019).
Bedford, J. L., Thomas, M. D. R. & Smyth, G. Beam modeling and VMAT performance with the Agility 160-leaf multileaf collimator. J Appl Clin Med Phys 14, 172–185 (2013).
Fathy, M. M., Hassan, B. Z., El-Gebaly, R. H. & Mokhtar, M. H. Dosimetric evaluation study of IMRT and VMAT techniques for prostate cancer based on different multileaf collimator designs. Radiat Environ Biophys 62, 97–106 (2023).
Jeans, E. B. et al. Clinical implementation of preoperative short-course pencil beam scanning proton therapy for patients with rectal cancer. Adv Radiat Oncol 5, 865–870 (2020).
Appelt, A. L. et al. Robust dose planning objectives for mesorectal radiotherapy of early stage rectal cancer – A multicentre dose planning study. Tech Innov Patient Support Radiat Oncol 11, 14–21 (2019).
Pedone, C. et al. Preoperative short-course radiation therapy with PROtons compared to photons in high-risk RECTal cancer (PRORECT): Initial dosimetric experience. Clin Transl Radiat Oncol 39, 100562 (2023).
Nancy, L. Y., & Jiade, J. L. Target volume delineation and field setup. A practical guide for conformal and IMRT. Journal of Chemical Information and Modeling. 53 (2013).
Gay, H. A. et al. Pelvic normal tissue contouring guidelines for radiation therapy: A radiation therapy Oncology Group Consensus Panel Atlas. International Journal of Radiation Oncology Biology Physics 83, e353–e362 (2012).
Appelt, A. L. et al. Robust dose planning objectives for mesorectal radiotherapy of early stage rectal cancer – A multicentre dose planning study. Tech. Innov. Patient Support Radiat. Oncol. 11, 14–21 (2019).
Petrova, D., Smickovska, S. & Lazarevska, E. Conformity index and homogeneity index of the postoperative whole breast radiotherapy. Open Access Maced J Med Sci 5, 736–739 (2017).
Paddick, I. & Lippitz, B. A simple dose gradient measurement tool to complement the conformity index. J Neurosurg 105, 194–201 (2006).
Younge, K. C. et al. Predicting deliverability of volumetric-modulated arc therapy (VMAT) plans using aperture complexity analysis. J Appl Clin Med Phys 17, 124–131 (2016).
Takakusagi, Y. et al. Comparison of moderate hypofractionated volumetric-modulated arc therapy plans with and without flattening filter for localized prostate cancer. Cureus https://doi.org/10.7759/cureus.18034 (2021).
Brekner, M. C. et al. Stereotactic body radiotherapy with volumetric intensity-modulated arc therapy and flattening filter-free beams: dosimetric considerations. Strahlentherapie und Onkologie 200, 346–357 (2024).
Blümer, N. et al. New possibilities for volumetric-modulated arc therapy using the AgilityTM 160-leaf multileaf collimator. Strahlentherapie und Onkologie 190, 1066–1074 (2014).
Richter, A. et al. Comparison of sliding window and field-in-field techniques for tangential whole breast irradiation using the halcyon and synergy agility systems. Radiation Oncology 16, 213 (2021).
Hernandez, V. et al. What is plan quality in radiotherapy? The importance of evaluating dose metrics, complexity, and robustness of treatment plans. Radiotherapy and Oncology 153, 26–33 (2020).
Park, J. M. et al. Modulation indices for volumetric modulated arc therapy. Phys Med Biol 59, 7315–7340 (2014).
Huang, C.-M. et al. A retrospective comparison of outcome and toxicity of preoperative image-guided intensity-modulated radiotherapy versus conventional pelvic radiotherapy for locally advanced rectal carcinoma. J Radiat Res 58, 247–259 (2017).
Lim, T. Y., Dragojević, I., Hoffman, D., Flores-Martinez, E. & Kim, G. Y. Characterization of the Halcyon TM multileaf collimator system. J Appl Clin Med Phys 20, 106–114 (2019).
Pokhrel, D. et al. Prostate SBRT using O-Ring Halcyon Linac — Plan quality, delivery efficiency, and accuracy. J Appl Clin Med Phys 22, 68–75 (2021).
Baglan, K. L. et al. The dose-volume realationship of acute small bowel toxicity from concurrent 5-FU-based chemotherapy and radiation therapy for rectal cancer. International Journal of Radiation Oncology Biology Physics 52, 176–183 (2002).
Robertson, J. M., Söhn, M. & Yan, D. Predicting grade 3 acute diarrhea during radiation therapy for rectal cancer using a cutoff-dose logistic regression normal tissue complication probability model. International Journal of Radiation Oncology Biology Physics 77, 66–72 (2010).
Holyoake, D. L. P., Partridge, M. & Hawkins, M. A. Systematic review and meta-analysis of small bowel dose–volume and acute toxicity in conventionally-fractionated rectal cancer radiotherapy. Radiotherapy and Oncology 138, 38–44 (2019).
Huang, W. et al. Effect of pelvic bone marrow sparing intensity modulated radiation therapy on acute hematologic toxicity in rectal cancer patients undergoing chemo-radiotherapy. Front Oncol. 11, (2021).
Zhang, R. et al. Flattening filter-free volumetric-modulated arc radiotherapy for left-sided whole-breast, partial-breast, and postmastectomy irradiations. J Med Phys 47, 166 (2022).
Zhao, L. R., Zhou, Y. B. & Sun, J. G. Comparison of plan optimization for single and dualvolumetric-modulated arc therapy versus intensity-modulated radiation therapy during post-mastectomy regional irradiation. Oncol Lett. 11, (2016).
Author information
Authors and Affiliations
Contributions
Q.Z.wrote the main manuscript text. Q.Z.,X.N.S.and Q.W.reviewed the literature and developed the idea of study.Q.Z.and C.S.participated in collecting data. Q.Z.,Y.W.L.and Q.W. conducted statistical analysis and interpreted the results. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Ethics Committee of Sir Run Run Shaw Hospital, Zhejiang University School of Medicine. It was conducted in accordance with the ethical standards of the Declaration of Helsinki.
Informed consent
Patient consent was waived by the Medical Ethics Committee of Sir Run Run Shaw Hospital, Zhejiang University School of Medicine due to the anonymity of the data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhou, Q., Wang, Q., Li, Y. et al. Dosimetric comparison of VMAT plans in preoperative short-course rectal radiotherapy. Sci Rep 14, 30862 (2024). https://doi.org/10.1038/s41598-024-81310-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-81310-4