Abstract
More attention should be paid to the deviations between the actual diameter of the rhexis reference circle which projected by the Image-guided systems and its intended size, and assess the influence of ocular biometric parameters on the deviation. In this study, the Callisto eye image-guided system was employed to generate a digital rhexis reference circle (rhexis overlay) set at an intended diameter of 6 mm and a screenshot of the video was taken at the end of the cataract surgery, then to compare the deviation between the observed rhexis overlay diameter (ROD) and the optic diameter (6 mm). The factors influencing diameter deviation were identified with univariate and multivariate linear regression. Subgroup analyses were conducted based on factors identified in the multivariate regression. And we observed that a total of 213 eyes of 174 patients were included in the final analysis. The diameter deviation averaged − 0.24 ± 0.28 mm (P = 0.0001) and was positively correlated with phakic anterior chamber depth (ACD) (P < 0.001) and negatively correlated with white-to-white (WTW) measurement (P < 0.001). Subgroup analyses revealed significantly greater diameter deviation in cases with preoperative ACD < 2.5 mm and WTW ≥ 12.0 mm (all P < 0.05). Following optimization, the mean diameter deviation was 0.00047 ± 0.26 mm (P > 0.05). In conclusion, the Callisto eye image-guided system demonstrates good precision in CCC assistance. However, there remains a slight deviation from the intended size when generating the rhexis reference circle in eyes with shallow anterior chambers and larger corneas. Implementing an optimization process could be beneficial for these eyes.
Similar content being viewed by others
Introduction
Cataract remains the leading cause of visual impairment worldwide, and surgery is the primary treatment modality for cataracts1. Continuous curvilinear capsulorhexis (CCC), is a fundamental technique in modern cataract surgery2. During CCC, a circular opening is meticulously created on the lens anterior capsule. This opening serves as a gateway for accessing and removing the cataractous lens while preserving the integrity of the capsule. Since its development in the 1980s3, CCC has demonstrated enhanced safety compared to earlier techniques for opening the anterior capsule4.
With the evolution of refractive cataract surgery, cataract surgeons strive to achieve a perfectly sized and well-centered CCC with complete intraocular lens (IOL) optic overlap. Specifically, this precision in size of CCC is crucial, as an appropriately sized CCC enhances postoperative refraction, IOL stability, and visual quality, which is particularly important for premium IOL implantation outcomes5. Research indicated that CCC with larger diameter can lead to anterior movement of the IOL, resulting in a myopic shift6. Kránitz et al. reported that larger CCC might lead to incomplete capsule-optic overlap, causing IOL decentration and tilt7. Moreover, a larger CCC has been associated with an increased risk of long-term complications, such as uveitis-glaucoma-hyphema syndrome8 and posterior capsule opacification9,10. Conversely, an undersized CCC may be associated with image distortion and heightened glare sensitivity11, and also can also contribute to anterior capsular contraction syndrome and subsequent IOL decentration12.
Due to the challenges in achieving precise CCC through surgical experience alone, several devices have been introduced to assist in this process. These include circular corneal markers13, semicircular markers14, ring-shaped markers15, and open ring-shaped calipers16. However, the use of these devices carries the risk of damaging or infecting the cornea, iris, anterior chamber, and other ocular tissues17. In response to these concerns, image-guided systems have been developed. These systems project a virtual rhexis reference circle onto the eyepiece, providing guidance for CCC creation without the need for additional surgical instruments18.
Previous studies have assessed the effectiveness of image-guided systems in assisting CCC17,19. For instance, Haeussler-Sinangin et al. reported that intraoperative image guidance facilitated the precision of CCC creation significantly during standard phacoemulsification17. Nevertheless, these studies typically assessed the size of the actual capsulorhexis created rather than the virtual rhexis reference circle itself. It is important to consider that subjective interpretations and cognitive biases among surgeons may contribute to size inconsistency between the created capsulorhexis and the digital guiding circle. Additionally, even if the created capsulorhexis perfectly matches the digital guiding circle initially, its size may change over time due to the morphological changes of the capsular bag and mechanical impact from the IOL haptic20,21, leading to differences from the digital guiding circle. Therefore, measuring the size of actual capsulorhexis created cannot truly reflect the precision of the image-guided system. In our practice, we have observed deviations between the actual diameter of the rhexis reference circle and its intended size. Therefore, this study aims to investigate the diameter deviation of the rhexis reference circle generated by an image-guided system in cataract surgery using the IOL optic as a scale, as well as the impact of ocular biometric parameters on this deviation. The findings aim to contribute to achieving more precise capsulorhexis in all cataract surgery.
Results
Demographic and ocular characteristics
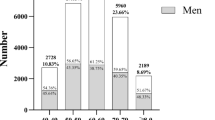
A total of 213 eyes from 174 patients, with a mean age of 70.19 ± 10.97 years, were included in the analysis. The mean preoperative ACD was 3.03 ± 0.40 mm, the mean AL was 23.70 ± 1.27 mm, and the mean WTW was 11.80 ± 0.40 mm. Detailed demographic and ocular characteristics of the study participants are listed in Table 1.
Diameter deviation
The distribution of diameter deviation is presented in Table 2; Fig. 1. The mean diameter deviation was − 0.24 ± 0.28 mm, which was statistically significant (p < 0.0001, one-sample t-test). A negative deviation was observed in 170 eyes (79.8%). Characteristics of eyes with negative or positive deviation are detailed in Table 3. WTW was significantly smaller in eyes with positive deviation compared to those with negative deviation.
Univariate and multivariate analyses
To explore the influencing factors related to diameter deviation, univariate and multivariate linear regression analyses were conducted with diameter deviation as the dependent variable, and AL, ACD, LT, WTW, TK1, TK2, Average K as independent variables (Table 4). Among the seven variables included in the model, diameter deviation was positively associated with phakic ACD (p < 0.001) and negatively associated with WTW (p < 0.001). The equation derived from the multivariate linear regression analysis was:
\(diameter\;deviation=0.{\text{21}}ACD - 0.243WTW+1.992\)
Subgroup analysis of diameter deviation
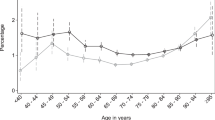
Further subgroup analyses were conducted to examine diameter deviation across different subgroups (Fig. 2). Patients were categorized based on ACD (˂ 2.5 mm; 2.5–3.0 mm; ˃ 3.0 mm) and WTW (˂ 12.0 mm; ≥ 12.0 mm). The results showed that the diameter deviation was significantly greater in patients with preoperative ACD < 2.5 mm and WTW ≥ 12.0 mm (all P < 0.05, one-way ANOVA followed by LSD’s post hoc tests for ACD subgroups and independent student’s t test for WTW subgroups).
Rhexis overlay diameter optimization
Optimization was conducted using the equation: RODoptimized = RODintended − (0.21ACD − 0.243WTW + 1.992). After optimization, the mean of diameter deviation was 0.00047 ± 0.26 mm. The distribution was shown in Fig. 3A, and the comparison of distributions before and after optimization is illustrated in Fig. 3B. Overall, diameter deviation in most cases approached zero after optimization. This trend was consistently observed across all subgroups based on ACD or WTW (Fig. 3C, D).
Rhexis overlay diameter optimization. (A) Distribution of diameter deviation after optimization. The red dashed line represents the mean deviation. (B) Comparison of deviation distribution before (gray) and after (blue) optimization. The red dot line indicates the mean deviation. (C) (D) Diameter deviation in different ACD and WTW subgroups after optimization. ns = no significance.
Discussion
For decades, achieving a well-centered and appropriately sized CCC has been a paramount goal for cataract surgeons. This precision is crucial in mitigating adverse effects on intraoperative procedures and postoperative IOL stability6,7,8,9,10,11,12. Modern digital image guidance systems now offer a safer and more convenient method for guiding CCC creation by projecting a digital reference circle onto the eyepiece18, contrasting with traditional methods that require additional surgical instruments13,14,15,16 and carry the risk of ocular tissue damage17. Despite these advancements, the accuracy of the rhexis reference circle size remains incompletely evaluated. This study aimed to investigate the diameter deviation of the rhexis reference circle and explore the influence of ocular biometric parameters on this deviation.
In our study, we initially analyzed the distribution of diameter deviation and found that the mean deviation of the observed rhexis overlay diameter (ROD) from the intended value was − 0.24 ± 0.28 mm. This finding aligns closely with Haeussler-Sinangin’s study17, which reported an absolute deviation of CCC diameter from the target size of 0.1 ± 0.2 mm horizontally and 0.1 ± 0.18 mm vertically when using an image-guidance system. However, in our analysis, we focused on the raw deviation values and observed a negative deviation in nearly 80% of cases. Dick et al.19 similarly reported a CCC diameter deviation from the target of -0.1 mm (range from − 0.3 to 0 mm), indicating a tendency for the CCC diameter to be slightly smaller than the intended size when guided by a digital rhexis overlay. Eyes with positive deviation showed a smaller WTW, suggesting that a smaller WTW may lead to a larger digital rhexis overlay size than intended.
According to the manufacturer’s instructions of the Callisto eye image-guided system, the size of digital rhexis overlay depends on preoperative ACD, WTW and corneal radius (CR) measured by IOLMaster. The cornea has a magnification effect, and magnifies the anterior capsule approximately 1.15 times when performing CCC22. Therefore, the image-guided system takes into account of this effect when generating the digital rhexis overlay by adjusting the circle size based on ocular parameters (including ACD, WTW and CR), which means that the actual size of the rhexis overlay, despite being set to a specific diameter, can vary under different ocular conditions. To investigate if the deviation is more pronounced in specific populations of cataract patients, we further explored the influencing factors by multivariate linear regression analysis and found that ACD and WTW were both correlated with the deviation. Specifically, larger deviations were noted in the subgroup with ACD < 2.5 mm and WTW > 12 mm, suggesting that the accuracy of digital rhexis guidance may be compromised in these cases. One possible explanation is that the magnification effect of the cornea is less predictable in eyes with shallow anterior depth23 or larger corneas, potentially affecting the algorithm’s performance in determining rhexis overlay size accurately. Therefore, it would be appropriate to apply larger rhexis reference in cataract surgery of these eyes. Of note, our study found the K values (including TK1, TK2 and Average K) were all not associated with deviation. This phenomenon can be attributed to the K values distribution of the patients enrolled in this study, in which all K values are within a normal range (from 39 D to 45 D).
In the field of IOL formulas research, a more accurate IOL power calculation can be achieved after an optimization of intraocular lens constant in the eyes with special ocular characteristics (such as short/long axial length24,25 and ocular comorbidity26,27), as previous studies described. Similarly, our results also showed that more accurate diameter can be calculated after an optimization process based on ACD and WTW values. With the optimization described herein, the mean diameter deviation reduced to 0.00047 mm and approached zero across all subgroups. These results underscore the necessity and feasibility of optimizing CCC diameter according to preoperative ocular parameters, particularly in eyes with shallow anterior depth and/or larger corneas, to enhance the precision of CCC guidance.
To our knowledge, this study represents one of the initial evaluations of the accuracy of the digital rhexis reference circle size and the influencing factors related to diameter deviation. One notable advantage of our study lies in the methodology used to measure the rhexis overlay size. Unlike previous studies that assess the accuracy of CCC-guiding systems by comparing actually created CCC diameter with the target diameter, we directly compared the diameter of the digital guiding circle with the IOL optic. This approach avoids morphological inconsistencies between the actually created capsulorhexis and the digital guiding circle resulting from subjective interpretations and cognitive biases among surgeons, morphological changes of the capsular bag20 and mechanical impact from the IOL haptic21, allowing for a more precise evaluation of the digital rhexis overlay size. Moreover, using the IOL optic diameter as a reference to measure the true ROD provides a constant and reliable metric. However, this study also has limitations. First, the centration of capsulorhexis is also an essential factor for cataract surgery outcome, whether the centration of digital rhexis overlay is precise needs further research. Additionally, this study optimized the reference circle diameter and assessed its theoretical efficacy with a single intended diameter. Future research should explore the practical benefits of optimization across various intended RODs. Moreover, the effectiveness of optimization should be further validated in practical.
In conclusion, the Callisto eye image-guided system demonstrates good precision in CCC assistance. However, there remains a slight deviation from the intended size when generating the rhexis reference circle in eyes with shallow anterior chambers and larger corneas. Implementing an optimization process could be beneficial for these eyes.
Methods
Participants
Patients scheduled for phacoemulsification with IOL implantation were consecutively recruited from January 1, 2023, to May 30, 2023, at Fujian Provincial Hospital, Fuzhou, China. Patients with any of the following conditions were excluded: (1) pharmacologically dilated pupil < 6 mm; (2) corneal disease; (3) presence of other oculopathies, such as pseudoexfoliation, strabismus, uveitis, glaucoma, or lens dislocation/subluxation; (4) history of previous intraocular procedures or trauma. This cross-sectional study received approval from the local ethics committee of Fujian Provincial Hospital and was conducted in accordance with the tenets of the Declaration of Helsinki. All patients provided written informed consent.
Preoperative assessment
Preoperatively, all patients underwent a comprehensive ophthalmic examination, which included the assessment of visual acuity and intraocular pressure using a noncontact tonometer (NCT). Ocular parameter measurements were conducted, including axial length (AL), anterior chamber depth (ACD), lens thickness (LT), white-to-white distance (WTW), and flat/steep meridian of total keratometric value (TK1/TK2) using the IOLMaster 700 (Carl Zeiss AG, Oberkochen, Germany). Additionally, funduscopy and optical coherence tomography (OCT, Heidelberg Engineering Inc., Heidelberg, Germany) were performed. IOL power was calculated using the Barrett Universal II formula.
Biomorphological detection
Preoperative ocular parameter data and a biometry reference image from the IOLMaster 700 were transferred to the Callisto eye image-guided system for eye-tracking and intraoperative surgical assistance. During surgery, the system superimposed the image onto the patient’s eye through the operative microscope, and a digital rhexis reference circle (rhexis overlay) was created in the eyepiece with a selected diameter.
Surgical technique
All surgeries were performed by a single experienced surgeon (W.J. W) using a standardized phacoemulsification technique with preoperative dilation and topical anesthesia. A temporal 2.4 mm clear corneal tunnel incision was created, and the anterior chamber was filled with an ophthalmic viscosurgical device (OVD; sodium hyaluronate 15 mg/ml, Shanghai Qisheng Biological Preparation Co, Ltd., Shanghai, China). A 5.5-mm continuous curvilinear capsulorhexis (CCC) was performed with the assistance of the Callisto eye image-guided system. Following phacoemulsification, a one-piece 360° square-edge acrylic intraocular lens (IOL) with a 6-mm optic was implanted. Finally, the residual OVD was removed, and the incisions were hydrated.
Rhexis overlay diameter measurement
At the end of the surgery, high-resolution digital coaxial retroillumination screenshots of the surgical video were taken in a standardized fashion. The patient’s head position was carefully checked, and the patient was asked to look straight into the light. Several images were taken, focusing on the capsulorhexis margin (magnification 12×) with the digital rhexis overlay displayed (Fig. 4A). The intended rhexis overlay diameter (ROD) was set at 6 mm (Fig. 4B) to compare it with the 6 mm IOL optic. The images with the best quality were stored on a hard disk.
Measurement of rhexis overlay diameter. (A) Intraoperative image at the end of cataract surgery, with the digital rhexis overlay (blue circles) displayed. The large circle represents the 6-mm reference circle, and the smaller one represents 3-mm. (B) Comparison of diameters between the 6-mm reference circle (white circle) and the intraocular lens optic (yellow circle). The observed rhexis overlay diameter was calculated by comparing the areas of the 6-mm reference circle and the IOL optic.
To measure the observed ROD, all images were imported into Image J software (NIH, Bethesda, USA). The areas of both the 6-mm overlay circle and the IOL optic were measured (Fig. 4B), and observed ROD was calculated using the following equation:
\(RO{D_{observed}}={\text{6}} \times [{(Are{a_{rehxis}}/{\text{pi}})^{{\text{1}}/{\text{2}}}} \times {\text{2]/[}}{(Are{a_{optic}}/{\text{pi}})^{{\text{1}}/{\text{2}}}} \times {\text{2}}].\)
where:
Arearehxis represents the area of the intended 6-mm overlay circle.
Areaoptic represents the area of the IOL optic.
The “6” represents the 6 mm diameter of the IOL optic.
The diameter deviation of the observed ROD from the intended ROD (6 mm in this study) was then calculated.
Rhexis overlay diameter optimization
To improve the accuracy of the rhexis overlay after cataract surgery, an intended 6-mm diameter overlay was optimized to reflect the observed size it represented on the IOL plane, based on multivariate linear analysis results. Optimization was conducted using the following equation:
\(RO{D_{optimized}}=RO{D_{intended}} - ({\text{a}}{X_1}+{\text{b}}{X_2}+{\text{c}}{X_n}+{\text{d}})\)
where:
RODoptimized represents the optimized ROD,
RODintended represents the intended ROD, which is 6 mm in this study,
X1, X2, and Xn represent preoperative ocular parameters associated with diameter deviation.
a, b, c, and d are constants in the multivariate linear regression model.
The diameter deviation of the observed ROD from the optimized ROD was then calculated.
Statistical analysis
Statistical analyses were conducted using SPSS for Windows Version 24.0 software (SPSS Inc., Chicago, IL, USA). Continuous variables were expressed as means and standard deviations, while categorical variables were expressed as counts and percentages. The Kolmogorov-Smirnov test was used to confirm the normal distribution of variables. For variables with normal distribution, student’s two-sample t test or analysis of variance (ANOVA) with post hoc test were used. The Mann-Whitney U test was employed for comparing continuous variables with non-normal distribution. One-sample t test was performed to test whether the mean diameter deviation differed significantly from zero. Univariate and multivariate linear regression models were used to identify the influencing factors of diameter deviation. Factors with a p-value < 0.05 in the univariate models were included in the multivariate linear regression models. Subgroup analysis was also conducted based on the influencing factors identified by multivariate regression analyses. A p-value < 0.05 was considered statistically significant.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Cicinelli, M. V., Buchan, J. C., Nicholson, M., Varadaraj, V. & Khanna, R. C. Cataracts Lancet 401(10374), 377–389 (2023).
Sela, T. C. & Hadayer, A. Continuous Curvilinear Capsulorhexis - A Practical Review. Semin. Ophthalmol. 37 (5), 583–592 (2022).
Gimbel, H. V. & Neuhann, T. Development, advantages, and methods of the continuous circular capsulorhexis technique. J. Cataract Refract. Surg. 16 (1), 31–37 (1990).
Sharma, B., Abell, R. G., Arora, T., Antony, T. & Vajpayee, R. B. Techniques of anterior capsulotomy in cataract surgery. Indian J. Ophthalmol. 67 (4), 450–460 (2019).
Langenbucher, A., Szentmáry, N., Cayless, A., Wendelstein, J. & Hoffmann, P. Prediction of IOL decentration, tilt and axial position using anterior segment OCT data. Graefe’s archive Clin. experimental Ophthalmol. 262 (3), 835–846 (2024).
Cekiç, O. & Batman, C. The relationship between capsulorhexis size and anterior chamber depth relation. Ophthalmic Surg. Lasers. 30 (3), 185–190 (1999).
Kránitz, K. et al. Femtosecond laser capsulotomy and manual continuous curvilinear capsulorrhexis parameters and their effects on intraocular lens centration. J. Refract. Surg. (Thorofare N J. : 1995). 27 (8), 558–563 (2011).
Razeghinejad, M. R. & Havens, S. J. Large Capsulorhexis Related Uveitis-Glaucoma-Hyphema Syndrome Managed by Intraocular Lens Implant Exchange and Gonioscopy Assisted Transluminal Trabeculotomy. J. Ophthalmic Vis. Res. 14 (2), 215–218 (2019).
Aykan, U., Bilge, A. H., Karadayi, K. & Akin, T. The effect of capsulorhexis size on development of posterior capsule opacification: small (4.5 to 5.0 mm) versus large (6.0 to 7.0 mm). Eur. J. Ophthalmol. 13 (6), 541–545 (2003).
Hollick, E. J., Spalton, D. J. & Meacock, W. R. The effect of capsulorhexis size on posterior capsular opacification: one-year results of a randomized prospective trial. Am. J. Ophthalmol. 128 (3), 271–279 (1999).
van der Meulen, I. J. et al. (ed ) Contributions of the capsulorrhexis to straylight. Archives Ophthalmol. (Chicago Ill. : 1960) 127 10 1290–1295 (2009).
Lin, X., Ma, D. & Yang, J. Exploring anterion capsular contraction syndrome in cataract surgery: insights into pathogenesis, clinical course, influencing factors, and intervention approaches. Front. Med. 11, 1366576 (2024).
Wallace, R. B. 3rd. Capsulotomy diameter mark. J. Cataract Refract. Surg. 29 (10), 1866–1868 (2003).
Suzuki, H., Shiwa, T., Oharazawa, H. & Takahashi, H. Usefulness of a semicircular capsulotomy marker. J. Nippon Med. Sch. 79 (3), 195–197 (2012).
Tassignon, M. J., Rozema, J. J. & Gobin, L. Ring-shaped caliper for better anterior capsulorhexis sizing and centration. J. Cataract Refract. Surg. 32 (8), 1253–1255 (2006).
Lee, Y. E. & Joo, C. K. Open ring-shaped guider for circular continuous curvilinear capsulorhexis during cataract surgery. J. Cataract Refract. Surg. 41 (7), 1349–1352 (2015).
Haeussler-Sinangin, Y., Dahlhoff, D., Schultz, T. & Dick, H. B. Clinical performance in continuous curvilinear capsulorhexis creation supported by a digital image guidance system. J. Cataract Refract. Surg. 43 (3), 348–352 (2017).
Varsits, R. M., Hirnschall, N., Döller, B. & Findl, O. Evaluation of an intraoperative toric intraocular lens alignment system using an image-guided system. J. Cataract Refract. Surg. 45 (9), 1234–1238 (2019).
Dick, H. B., Peña-Aceves, A., Manns, M. & Krummenauer, F. New technology for sizing the continuous curvilinear capsulorhexis: prospective trial. J. Cataract Refract. Surg. 34 (7), 1136–1144 (2008).
Modesti, M., Pasqualitto, G., Appolloni, R., Pecorella, I. & Sourdille, P. Preoperative and postoperative size and movements of the lens capsular bag: ultrasound biomicroscopy analysis. J. Cataract Refract. Surg. 37 (10), 1775–1784 (2011).
Chen, L., Zhong, Y., Yao, K. & Fu, Q. Effect of intraocular lens material and haptic design on anterior capsule contraction after cataract surgery: A systematic review and meta-analysis. Graefes Arch. Clin. Exp. Ophthalmol. 262 (5), 1421–1432 (2024).
Waltz, K. L. & Rubin, M. L. Capsulorhexis and corneal magnification. Archives of ophthalmology (Chicago, Ill.: 110(2), 170(1992). (1960).
Avetisov, K. S., Fеdorov, A. A. & Novikov, I. A. Light and scanning electron microscopy of anterior lens capsule following different capsulorhexis techniques]. Vestn Oftalmol. 131 (6), 4–10 (2015).
Terzi, E., Wang, L. & Kohnen, T. Accuracy of modern intraocular lens power calculation formulas in refractive lens exchange for high myopia and high hyperopia. J. Cataract Refract. Surg. 35 (7), 1181–1189 (2009).
Zhang, J. Q. et al. X. Effect of lens constants optimization on the accuracy of intraocular lens power calculation formulas for highly myopic eyes. Int. J. Ophthalmol. 12 (6), 943–948 (2019).
Belov, D. F., Potemkin, V. V. & Nikolaenko, V. P. Optimization of intraocular lens power calculation in pseudoexfoliation syndrome]. Vestn Oftalmol. 137 (4), 38–42 (2021).
Bonfadini, G. et al. Optimization of intraocular lens constant improves refractive outcomes in combined endothelial keratoplasty and cataract surgery. Ophthalmology 120 (2), 234–239 (2013).
Acknowledgements
This clinical study was supported by the Medical Innovation Program of Fujian Province (2023CXA001) and Natural Science Foundation of Fujian Province (2022J011006). The sponsors of the study played no role in the study protocol design, data collection, data analysis, data interpretation, manuscript preparation, or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Y.B.F., Y.L.H., X.B.L., W.J.W. and Q.L. were involved in the study conception, design, and funding; Y.B.F., Y.L.H., X.B.L., C.S.K. and W.J.W. conducted the study; Y.B.F., Y.L.H., X.B.L., C.S.K. and W.J.W. collected the data; Y.B.F., Y.L.H., X.B.L., W.J.W. and Q.L. analyzed the data; Y.B.F., Y.L.H., X.B.L., W.J.W. and Q.L. reviewed the manuscript; and Y.B.F., Y.L.H., X.B.L., C.S.K., W.J.W. and Q.L. gave final approval of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fu, Y., Huang, Y., Liu, X. et al. Characteristics and factors associated with diameter deviation of rhexis reference circle generated by an image-guided system in cataract surgery: a cross-sectional study. Sci Rep 14, 31876 (2024). https://doi.org/10.1038/s41598-024-83137-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-83137-5