Abstract
Repeated muscle micro-trauma may cause severe muscle damage. Diffusion tensor imaging (DTI) exhibits sensitivity to microstructural changes in skeletal muscle. We hypothesize that longer diffusion times enhance sensitivity to micro-trauma and that membrane permeability increases with micro-trauma. We obtained DTI scans of the thighs in ten male runners 1 week before (TP-0), 24–48 h after (TP-1), and 2 weeks after (TP-2) they completed a marathon. Diffusion times were 28.1, 116.7, and 316.7 ms. The random permeable barrier model (RPBM) was fitted to the radial diffusivities to obtain estimates for fiber diameter and membrane permeability. Hamstring and quadriceps muscles were manually segmented. A linear mixed model assessed variations across time points and diffusion times within the DTI and RPBM parameters and assessed sensitivity to micro-trauma by comparing %-changes in DTI parameters at TP-1 and TP-2 to TP-0. All DTI parameters except FA significantly changed between TP-0 and TP-1, and between TP-1 and TP-2. The %-change did not differ between diffusion times. The permeability increased at TP-1 and TP-2 compared to TP-0. In conclusion, longer diffusion times did not improve sensitivity to micro-trauma. The increased permeability post-marathon underscores the potential of RPBM-derived parameters as a biomarker for micro-trauma and muscle injuries.
Similar content being viewed by others
Introduction
Skeletal muscle micro-traumas are small injuries that typically occur during exercise. Most micro-traumas are related to eccentric exercise and can include myofibrillar disruptions, Z-line disturbances, increased permeability, and damage to the extracellular matrix1,2. Reported symptoms are pain, swelling, and reduced muscle force production3. While most micro-traumas tend to heal naturally, and even stimulate muscle adaptation to exercise3, repetitive muscle micro-trauma can result in more severe muscle injuries4, such as overuse injury. Therefore, a better understanding of muscle micro-traumas is desirable.
Magnetic resonance imaging (MRI) provides non-invasive, detailed volumetric images of skeletal muscles, positioning it as a promising tool for tracking micro-trauma. Traditional qualitative MRI methods, like T2-weighted MRI, often struggle to identify muscle micro-trauma5,6, as the subtle changes in tissue structure are not always visually detectable. Diffusion tensor imaging (DTI), a quantitative MRI technique that probes the diffusion of water molecules in tissue, enables a non-invasive comprehensive characterization of the underlying tissue microstructure. The diffusion processes in skeletal muscle are restricted by the cell membranes, which results in a more free diffusion along muscle fibers than perpendicular to the muscle fibers. Changes in the muscle microstructure, like membrane or fiber disruptions, will alter the diffusion properties. DTI is sensitive to severe skeletal muscle injuries, characterized by disruption of muscle membranes and tissue inflammation7, displaying an increased diffusivity post-injury, which recovered towards return-to-play time8,9,10. Recent work showed that DTI is also sensitive to muscle micro-trauma, capturing alterations that were not detectable with traditional qualitative methods11,12. These previous works excluded IVIM and T2 effects as contributors to the detected subtle changes in DTI indices in muscle micro-trauma. However, the precise microstructural basis for these subtle alterations remains unclear, potentially involving cell swelling, fiber disruptions, increased permeability, or damage to the extracellular matrix1,13,14,15.
Increasing the sensitivity of DTI to subtle muscle damage and employing sophisticated biophysical models could uncover the microstructural basis of subtle changes in DTI indices. However, conventional diffusion experiments do not probe water diffusion at a large enough scale. Particularly, the 2D Stokes-Einstein relation states that < r > 2 = 4\(\:\cdot\:\)Dt, where < r>² is the mean square displacement of the particles and t is the time diffusion took place. Conventional skeletal muscle DTI, with diffusion times of 30–60 ms and radial diffusivity, D, of 1.5\(\:\cdot\:\)10−3mm²/s, hence typically probes a water diffusion distance scale of 15–30 μm. Considering the average muscle fiber diameter ranges from 30 to 80 μm16, one should probe a larger length scale to enhance sensitivity to micro-trauma. This can be achieved by selecting a diffusion time greater than 100 ms. In a conventional spin-echo sequence, longer diffusion times, however, would extend the echo time (TE) and, consequently, increase T2 decay and therefore reduce the available signal excessively. To circumvent this, a stimulated echo sequence is preferable. This technique preserves the transverse magnetization during the mixing time by storing it longitudinal, facilitating longer diffusion times without adversely affecting the TE. Additionally, by applying DTI at multiple diffusion times, estimations of the muscle fiber diameter and membrane permeability can be obtained non-invasively by fitting the data to the random permeable barrier model (RPBM)17,18. The RPBM assumes that the radial diffusion in skeletal muscle – perpendicular to the long-axis of the muscle fibers – is hindered by randomly oriented permeable membranes. It has recently been demonstrated that the RPBM can capture changes in fiber diameter in Becker muscular dystrophy19and muscle atrophy20, and therefore has potential for characterizing microstructural damage in muscle micro-trauma.
This study investigates if muscle micro-trauma detection can be improved by longer diffusion times and if micro-trauma is related to changes in cell size and permeability by using time-dependent DTI in a cohort of subjects that completed a marathon run. We hypothesize that: (i) stimulated-echo DTI with longer diffusion times is more sensitive to subtle changes in skeletal muscle structure due to micro-trauma than conventional DTI; and (ii) skeletal muscle micro-trauma leads to changes in muscle membrane permeability as assessed by fitting time-dependent diffusion data with the RPBM.
Methods
Subjects
The study was approved by the local medical research ethics committee (METC Amsterdam University Medical Center, #NL61873.018.17) and conducted according to the principles of the most recent version of the Declaration of Helsinki and in accordance with the Medical Research Involving Human Subjects Act (WMO).
Twelve male marathon runners were included and written informed consent was obtained from all participants before the start of the study. More information on participant recruitment can be found in Hooijmans et al.11. Some of the data—namely, the T2-weighted imaging and spin-echo-based DTI data—were previously analyzed and presented in Hooijmans et al.11. In this research, analysis focused solely on the mid-thigh level, examining stimulated-echo in comparison to spin-echo based DTI data. The previously published spin-echo DTI data were therefore re-analyzed exclusively at the mid-thigh level, as detailed below.
MRI protocol
All subjects underwent a bilateral MRI examination of the upper leg muscles at the mid-thigh level and at three time points: one week before (pre-marathon; TP-0), 24–48 h after (post-marathon; TP-1) and two weeks after (follow-up; TP-2) completing the Amsterdam Marathon. The detailed MRI scan parameters can be found in Table 1. A wide-bore 3T MRI scanner (Ingenia, Philips Healthcare, Best, The Netherlands) was used for imaging, with the body coil for transmission and a 16-element anterior coil and 12-channel posterior coil for reception. Participants were positioned in the feet-first supine position. The scan protocol included an anatomical T2-weighted turbo spin-echo (TSE) sequence, a 4-point chemical-shift-based water-fat-separation gradient echo (Dixon) scan, a spin-echo echo-planar imaging (SE-EPI) DTI scan and two stimulated echo (STE) EPI DTI scans with mixing times of 100 and 300 ms. The resulting diffusion times were 28.1, 116.7, and 316.7 ms respectively. Additionally, a noise scan was obtained by playing the SE and STE sequences without RF power and used to calculate the DTI signal-to-noise ratio (SNR).
Data post-processing
The b-matrix of each DTI scan was corrected for the additional diffusion-weighting from the imaging gradients using QMRITools21. Further data processing was performed in Matlab (R2021b, The MathWorks, Natick, CA). The data from all DTI scans were denoised using a Marchenko-Pastur Principal Component Analysis (MP-PCA) algorithm22. The data were register over all b-values with elastix23 using an affine transformation to correct for motion and eddy-current induced displacements. Subsequently, the DTI data were registered to the anatomical Dixon water image using a rigid followed by a b-spline transformation. DTI fitting was performed voxel-wise using an iteratively weighted least squares fit (iWLLS) in combination with the REKINDLE outlier rejection algorithm24 from ExploreDTI25 to reduce signal voids from spontaneous muscle twitches26. For each voxel, the outcome parameters mean diffusivity (MD), fractional anisotropy (FA), diffusion tensor eigenvalues (λ1, λ2, and λ3), and radial diffusivity (RD) were calculated, with RD = mean(λ2, λ3).
Subsequently, the RPBM model was fitted voxel-wise to λ1 (axial diffusivity) and the diffusion time-dependent RD. To increase the precision of the RPBM fit, the axial diffusivity was fixed to the mean λ1value at Δ > 100 ms (namely, the two STE-DTI scans)18. The SE-DTI images were interpolated to match the STE-DTI resolution. As a data quality control step, the model was only fitted if RD(Δ = 28.1 ms) > RD(Δ = 116.7 ms) > RD(Δ = 316 ms) in the voxel. The outcome parameters were the mean fiber diameter a and the membrane permeability κ. For a, the correction factor proposed by Berry et al.27 was applied.
As a further quality control, the SNR of the b= 0 s/mm² DTI images was calculated pixel-wise for each diffusion time using the standard deviation of the noise-only scans for each mixing time and correcting for Rician noise28. For each diffusion time, muscles with a mean SNR < 15 were excluded from the DTI analysis. As for the RPBM analysis the data from all three diffusion times is required, muscles with a mean SNR < 15 at any diffusion time were excluded from the RPBM analysis.
Muscle segmentation and analysis
Regions of interest (ROIs) were drawn manually in both legs on all slices on the Dixon out-of-phase and scanner reconstructed Dixon water images in ITK-snap29 (version 3.8.0, www.itksnap.org). The eight upper leg muscles evaluated in this study are the: biceps femoris long head (BFL), biceps femoris short head (BFS), semimembranosus (SM), semitendinosus (ST), vastus medialis (VM), vastus intermedius (VI), vastus lateralis (VL) and rectus femoris (RF). An example segmentation is shown in Fig. 1. The ROIs were eroded by one voxel to avoid partial volume with surrounding subcutaneous and intermuscular fat tissue. The median of the DTI and RPBM parameters were obtained per muscle and leg (right/left) for all time points and diffusion times.
Field of view and muscle segmentations. Left: Location chosen for the field of view centered at mid-thigh level, shown on a surface render plot of the upper legs. Right: Axial Dixon water image with segmentations drawn in the hamstring and quadriceps muscles of both legs. VL: vastus lateralis, VI: vastus intermedius, RF: rectus femoris, VM: vastus medialis, BFS: biceps femoris short head, BFL: biceps femoris long head, ST: semitendinosus, SM: semimembranosus.
As some severe muscle twitches were observed even after the REKINDLE fit, an additional outlier rejection was performed. For each diffusion time, muscle and leg (right/left), the z-score of MD was calculated as \(\:z=\:\frac{x\:-\:\mu\:}{\sigma\:}\), with x the individual value, µ the mean over all subjects and time points, and σ the standard deviation over all subjects and time points. MD was chosen as it is the most stable DTI parameter30. Muscles with an MD z-score greater than 3 (namely, more than 3 standard deviations from the mean) were considered outliers and were excluded from further analysis.
Injury analysis
To assess potential overt muscle injuries, beyond micro-trauma, resulting from running the marathon, post-marathon data (TP-1) were screened and scored by a radiologist (F.S.) with 5 years of experience in musculoskeletal MRI. Injuries located at the mid-thigh level, within the coverage of the stimulated echo DTI scans, were the only ones taken into account. The T2-TSE data were used for scoring and a modified Peetrons’ classification31 was applied for injury grading (grade 0 – no abnormality on MRI; grade 1 – edema without architectural distortion; grade 2 – edema with architectural disruption; grade 3 – complete tear). ROIs of the injuries were drawn in the slices containing the injured muscle tissue as identified on the T2-TSE data. In those slices, the entire muscle area in-plane of the affected muscle was segmented to account for the challenges associated with a possible mismatch between the ___location of edema and the ___location of a primary muscle injury, or the limited extent of an injury during segmentation. ROIs at TP-0 and TP-2 were drawn at closely matching regions.
Statistical analysis
All statistical analyses were performed in SPSS (SPSS Statistics 28.01.1.1, IBM Corp., Armonk, NY, USA). A linear mixed model was used to assess differences between the time points and the diffusion times for each DTI outcome parameter as an overall time effect (over the time points). The contribution of the individual muscles and the diffusion time to the main time effect were assessed by post-hoc analysis. The significance level was corrected for multiple comparisons (6 outcome parameters × 3 time points) and set to p ≤ 0.05/18 = 0.003. To test if longer diffusion times were more sensitive to subtle changes, the percentage change between TP-0 and TP-1 (%TP-1) was calculated for each diffusion time and DTI parameter as:
with param the DTI parameter. A linear mixed model was used to assess differences in %TP-1 between the diffusion times, and the significance level was corrected for multiple comparisons: p ≤ 0.05/6 = 0.008 (6 DTI parameters). Similarly, differences in the RPBM parameters between the time points were assessed with a linear mixed model, and the significance level was set to p ≤ 0.05/6 = 0.008 (2 outcome parameters × 3 time points). As an exploratory analysis, DTI and RPBM parameters were evaluated in the muscles with injuries using the injury ROIs between the time points and diffusion times. The same linear mixed model was used for the DTI and RPBM parameters and the significance level was set to 0.05.
Results
Participants
Two out of twelve participants were excluded; one participant due to not finishing the marathon and one participant due to missing stimulated-echo DTI data at one of the time points. Ten participants – mean (SD) age 52.9 (6.0) years, range 47–68 years – completed the MRI protocol at all three visits and were included for further analysis.
Data quality
Quantitative MD maps of all time points and diffusion times are shown in Supplementary Fig. SF1. A total of 27 out of 480 muscles were excluded due to SNR < 15 (BFS = 13, RF = 6, SM = 1, ST = 1, VL = 2, VM = 4). All SNR exclusions occurred in the SE-DTI data. For the STE-DTI data, all muscles had SNR > 15 at both, Δ = 116.7 and 316.7 ms. A total of 10 muscles were classified as outliers (MD z-score > 3) and excluded (Δ = 116.7 ms: n = 3, Δ = 316.7 ms: n = 8, 1 overlapping). An example of a muscle classified as an outlier can be found in Supplementary Fig. SF2.
Time-dependent DTI analysis
Marathon time point comparison
The mixed model analysis showed that all DTI parameters except FA significantly changed between TP-0 and TP-1 and between TP-1 and TP-2 (Fig. 2). We found no significant changes between TP-0 and TP-2 in any parameter, suggesting recovery of the injury. The post-hoc analysis in individual muscles did not show a significant time effect in any muscle. The post-hoc analysis for the individual diffusion times revealed that the shortest diffusion time (SE sequence, Δ = 28.1 ms) contributed most to the overall time effect (p < 0.001 for all parameters), whereas for the STE sequences an overall time effect was found for MD and λ1 at Δ = 116 ms (p < 0.001) and for all parameters except λ2 (p = 0.032) at Δ = 316 ms (p < 0.001 for MD, λ1, λ3 and p = 0.003 for RD).
Conventional DTI analysis. Mean fractional anisotropy (FA), mean diffusivity (MD), first diffusion tensor eigenvalue (λ1, axial diffusivity), and radial diffusivity (RD) parameters, averaged over all muscles, for each subject (n = 10, dashed gray lines) at all three time points (TP-0 to TP-2) and diffusion times (Δ). The mean and standard deviation over all subjects are shown in black. * = p < 0.001.
Diffusion time comparison
The DTI parameters for all muscles and diffusion times at TP-0 are listed in Table 2. The diffusivity (MD, RD, λ1, λ2, λ3) decreased with increasing diffusion time, while FA increased (p ≤ 0.001 for all parameters). This is also visible in Figs. 2 and 3. The decrease in diffusivity with increasing diffusion time was most pronounced in the radial diffusivity (RD, λ2, λ3) and least pronounced in the axial diffusivity λ1 (Fig. 3, left).
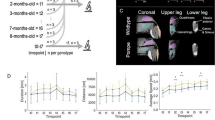
Random permeable barrier model (RPBM) analysis. Left: Axial (top, blue) and radial (bottom, orange) diffusion vs. diffusion time of the right semitendinosus (filled circles) and the right rectus femoris (open circles) at TP-0 for a representative subject. While the changes in axial diffusivity over diffusion time are subtle, the decrease in radial diffusivity with increasing diffusion time is more pronounced. The dashed lines show the RPBM fits to the radial diffusivity (black: semitendinosus, gray: rectus femoris). Right: Line plots of the fiber diameter, a, and the permeability, κ, averaged over all muscles, for each subject (n = 10, dashed gray lines). The mean and standard deviation over all subjects are overlaid in black. * p ≤ 0.008.
The absolute changes between timepoints were comparable between the diffusion times (Supplementary Table ST1). The percentage changes at TP-1 relative to TP-0 were not different between the diffusion times for any DTI parameter (p = 0.02 (λ1), 0.31 (λ2), 0.05 (λ3), 0.12 (MD), 0.06 (RD) and 0.08 (FA)). This can also be observed in Fig. 4. While the median values in the boxplots are not different between the diffusion times, more variation towards higher %TP-1 are detected in RD and FA at higher diffusion times (Δ = 116.7 and 316.7 ms).
Percentage change in DTI parameters. The boxplots show the relative change between TP-1 and TP-0 for λ1, radial diffusivity (RD) and fractional anisotropy (FA) for each diffusion time. The individual datapoints for each subject, muscle and leg (left/right) are overlaid in blue (n = 160). The red line indicates no change between TP-1 and TP-0 (0%). Although the median values are similar for all diffusion times, some very high percentage changes are found in RD at the diffusion time of 316.7 ms.
RPBM analysis
Example parameter maps of the fiber diameter and permeability are shown in Fig. 5 and the detailed parameters per muscle are listed in Table 3. Example RPBM fit curves are shown in Fig. 3 and for all time points in Supplementary Figure SF3. For the fiber diameter, no change over time was observed (p = 0.02, Fig. 3). However, a significant overall time effect was found for the permeability (κ) (p = 0.008). Post-hoc analysis for the permeability revealed a time effect between TP-0 and TP-1 (p = 0.005) and between TP-0 and TP-2 (p = 0.008), but not between TP-1 and TP-2 (p = 0.86). No time effect in individual muscles was found.
Random permeable barrier model (RPBM) parameter maps. Maps of the fiber diameter (top) and permeability (bottom) of one subject are shown at all three time points (TP-0 – TP-2). Between the time points, no clear differences are visible in the maps. The excluded voxels that failied the quality control step of the radial diffusivity (RD) (RD(Δ = 28.1 ms) > RD(Δ = 116.7 ms) > RD(Δ = 316 ms)) are black in both maps, the fiber diameter and permeability.
Injury analysis
At TP-1, a total of 25 injuries were detected in 8 out of 10 participants (11 right legs, 14 left legs, affected muscles: ST = 7, SM = 1, BFL = 3, VI = 4, VM = 6, VL = 4). All injuries were scored as grade 1. None of the injured muscles were classified as outliers. Anatomical T2-weighted TSE example images of the injuries are given in Supplementary Figure SF4.
In the subset of injured muscles, a significant overall time effect was found for MD, λ1, λ3 and RD (p < 0.05), but not for λ2 and FA. Post-hoc analysis showed a significant time effect between TP-0 and TP-1 and between TP-1 and TP-2 (Fig. 6). Similar to the whole muscle analysis, no significant difference between TP-0 and TP-2 was found. No post-hoc test for individual muscles was performed due to the low number of injuries.
Injury analysis. Mean diffusivity (MD) and radial diffusivity (RD) at all diffusion times (Δ) (a) and the RPBM parameters a and κ (b) of the injured muscles (n = 25, dashed gray lines) at all three time points (TP-0 to TP-2) are shown. The mean and standard deviation over all injuries are overlaid in black. * p ≤ 0.05.
For the RPBM parameters, a significant time effect was found for the permeability (p = 0.01), but not for the fiber diameter (p = 0.23). Pairwise comparisons revealed an increase in the permeability in the injured region post-marathon (TP-0 vs. TP-1: p = 0.004, TP-0 vs. TP-2: p = 0.02). No difference was found between TP-1 and TP-2 (p = 0.47), similar to the whole muscle analysis.
Discussion
In this paper, we investigated exercise-induced muscle micro-trauma with DTI and RPBM at multiple diffusion times. All DTI parameters, except FA, changed significantly 24–48 h after the marathon (TP-1). Contrary to our expectations, longer diffusion times did not improve sensitivity to those changes for DTI. The RPBM revealed an increased membrane permeability after the marathon (TP-1 and TP-2), but no change in fiber diameter. Even though the conventional DTI parameters were back to normal at follow-up (TP-2), the permeability remained higher than pre-marathon (TP-0) at TP-2. Our exploratory analysis in injured muscles (grade 1) yielded similar results to those of the whole muscle analysis.
The overall time-effect observed in DTI parameters after the marathon is in line with the previous DTI analysis of these data in the whole thighs11 and with previous studies on muscle injuries9,12. These results indicate that micro-trauma was present post-marathon. No significant difference was found between TP-0 and TP-2, which suggests that micro-trauma recovers within two weeks after the marathon. While we found an overall time effect, we did not find significant differences between the time points in individual muscles. Results from the previous DTI analysis of the whole muscle revealed that the most changes in DTI are found in the muscle end regions, i.e. most proximal and most distal11. In the middle part of the thighs, only minor changes are expected, which agrees with our findings. Also in our subanalysis of injured muscles, we found the same trends as in the whole-muscle analysis. A reason for that might be that all injuries were of grade 1 (modified Peetrons’ classification), which is characterized by edema without visual architectural disruption, and therefore only minor changes in DTI parameters are expected. While we found an overall increased diffusivity post-marathon, no changes in FA were observed. This is in line with the previous DTI analysis of the whole thighs11. A previous study performed after marathon running reported altered FA values, however, those changes were only significant in two thigh muscles (BFL and RF)12.
Comparing the diffusion times, we found a decrease in diffusivity and an increase in FA with increasing diffusion time, which is in line with previous research32,33,34,35. Contrary to our hypothesis, we observed no enhancement in sensitivity (percentage change) between pre- and post-marathon DTI parameters as diffusion time increased. Based on a muscle model, Berry et al. concluded that the greatest contrast between simulated healthy and damaged muscle should occur at diffusion times between 130 and 250 ms, with the most pronounced changes expected in FA27. However, our experimental findings did not demonstrate such changes in FA, aligning instead with observations by Monte et al.9 and Giraudo et al.36. A possible limitation of the histology-informed muscle model by Berry et al. is its lack of micro-trauma representation and the omission of the impact of noise on the data. In vivo experiments always suffer from noise, which can severely impact the DTI parameter estimation, especially λ337. As the FA is derived from the eigenvalues, erroneous eigenvalues can impact the sensitivity of FA. Although we excluded low SNR data in our study and covered the suggested diffusion time range (Δ = 116.7/316.7 ms), noise might still have impacted the DTI parameter estimation. The optimal diffusion times for muscle damage due to injury may differ from the simulation results. In other pathologies, the sensitivity of diffusion times to muscle damage have been investigated32,38,39,40. In Duchenne muscular dystrophy, a diffusion time of around 200 ms was found to be optimal for detecting differences between diseased and healthy muscles32,39. Nevertheless, the pathophysiology of Duchenne muscular dystrophy differs significantly from the impact caused by muscle injuries. Another study in older individuals employed diffusion times ranging from 30 to 600 ms and found only minor changes in diffusion parameters compared to young individuals which were indepedent of diffusion times40. This suggest that more in vivo work is warranted in a variety of pathologies to identify suitable diffusion times for the characterization of skeletal muscle damage.
Taken together, our research revealed that the sensitivity to micro-trauma, measured by %TP-1, was comparable across all three diffusion times utilized. The shortest diffusion time, acquired with the conventional spin-echo DTI sequence, successfully identified subtle changes due to muscle micro-trauma across all parameters, except for FA. In contrast, the longer diffusion times, achieved by stimulated-echo DTI sequences, were only able to detect alterations in certain parameters.
The RPBM parameters found in this work are in line with literature values of RPBM-derived parameters in the lower legs19,40 and with histology values of the fiber diameter of the thighs16. We found an increase in permeability at TP-1, but no difference in the fiber diameter. This is consistent with increased diffusivity, but no change in FA at TP-1. Increased permeability can be related to increased flux of water molecules through the cell membrane, damage of the cell membrane, or both15. In the previous analysis of our data for the complete upper leg muscle volumes, no increase in water T2 was found after the marathon11, which is an indication that there was no inflammation post-marathon. This suggests that the increase in permeability may be caused by membrane damage. The permeability remained increased at TP-2 compared to TP-0. In the RPBM model the information from all three diffusion times is combined to derive the permeability. It could thus be more sentitive to subtle micro-structural changes two weeks after the marathon, that did not reach significance with conventional DTI anymore. We did not find a time effect in individual muscles, which can be attributed to the fact that only very subtle changes were found at a group level. Our results indicate that RPBM is a promising biomarker for muscle injuries, as it provides estimates of tissue microstructure, specifically muscle fiber diameter and membrane permeability, non-invasively. This potentially offers better insights into the pathological processes of muscle (micro-) injuries and their healing. Our work adds to a growing body of literature where the RPBM has proven useful for characterizing muscle atrophy20, Becker muscular dystrophy19, a mouse model of Duchenne muscular dystrophy39, and exercise-induced changes in both healthy controls and chronic exertional compartment syndrome patients41.
In most previous studies, more and longer diffusion times were used for RPBM analysis (up to 9 diffusion times and Δ up to 1,500 ms18,20,39,40,41), compared to the three diffusion times employed in this study. Three diffusion times are the minimum requirement for the RPBM fit, and consequently the fit is susceptible to experimental noise, which might reduce the precision and accuracy of the fit. A greater number of diffusion times could potentially enhance the sensitivity to microstructural changes after muscle micro-trauma. Typically, the axial diffusivity stabilized at diffusion times > 300 ms18. Employing more and longer diffusion times permits fitting of the axial diffusivity, or allows it to be fixed to a (mean) value at higher diffusion times, where a stable infinity limit is reached. To accurately and precisely estimate the permeability, the use of longer diffusion times would be beneficial – allowing for more interaction between water molecules and the sarcolemma – and diffusion times longer than the mean residence time of a particle in a cell are desirable20,38. In the lower leg the residence time was found to be ~ 450 ms18, suggesting that diffusion times beyond the 316.7 ms used in this work might increase the stability of the permeability estimation.
In this study we performed no correction for perfusion effects. While it has been shown that correction for intravoxel incoherent motion (IVIM) effects can improve the reproducibility of DTI estimations42, IVIM modelling requires the acquisition of multiple b-values at all diffusion times, which dramatically increases the acquisition time. The typical perfusion fractions in skeletal muscle in the legs at rest account for 3–7% of the signal43, and a recent study found that the IVIM-derived perfusion fraction does not change in muscle injuries of Peetrons’ grade 0–244. There is currently no indication that the perfusion signal fraction changes at long diffusion times; however, at short diffusion times (< 100 ms) a time-dependence of the IVIM-derived perfusion fraction was observed in the abdomen and brain45,46, and the time-dependence at diffusion times > 100 ms should be investigated in future research. Taken together, the bias in DTI parameters due to IVIM-effects can be considered to be stable over the time points and diffusion times used in this study, and was thus neglected. However, future work could use a b-value > 50 s/mm² – where the perfusion-related signal has largely decayed – as the lowest b-value, to reduce perfusion effects.
A limitation of our work is that two different sequences were used to acquire the short and long diffusion times, namely SE-DTI and STE-DTI. Currently, an SE sequence is the standard for DTI, while STE-DTI implementations are not available for all vendors on clinical scanners. Therefore, a SE-DTI sequence was chosen for the shortest diffusion time and the whole-leg DTI analysis described in11. Short diffusion times can also be achieved with a STE-DTI sequence and future studies should preferably acquire all diffusion times with the same sequence. The scan protocols for the SE-DTI and STE-DTI varied in terms of the number of b-values, diffusion directions, spatial resolution, and fat suppression, which could potentially have biased the estimation of RPBM parameters. These differences were needed to keep the scan time within an acceptable range. With the SNR constraint set at 15 for our analysis, we assumed the DTI fit quality was adequate for the comparisons conducted in this study. However, the reduced resolution of the STE-DTI protocol might have averaged out the effects of injury or micro-trauma, potentially impacting our results. In the SE-DTI and STE-DTI protocols, different fat suppression schemes were applied, which could potentially affect the level of fat suppression and bias the DTI estimates. However, in our study population, only healthy active people were included, which are expected to have fat fractions in the thighs < 10%47. As the olefinic fat peak is not suppressed by SPAIR, a research prepulse was used in both protocols. In the SE-DTI protocol, additionally, slice-selective gradient reversal fat suppression was used, which was not part of the STE-DTI protocol. Given that the olefinic fat peak accounts for only 5–10% of the total fat spectrum48 we consider it unlikely that this difference in fat suppression schemes caused a fat bias and visual inspection of the data did not show fat artifacts. Also, data acquisition focused on the central region of the thighs to ensure the maximal inclusion of muscle tissue within the available field of view. Hooijmans et al., however, noted that micro-trauma was most pronounced at the most proximal and distal parts of the muscle11. This accounts for the variations in the spin-echo DTI derived diffusion indices reported here compared to those previously documented by Hooijmans et al. An expanded, whole-muscle protocol with multiple diffusion times would be worth investigating. While the RPBM adds specificity to the characterization of muscle micro-trauma by providing estimates for the fiber diameter and membrane permeability, the need for multiple diffusion times consequently prolongs the total scan time. However, the ability to estimate those parameters non-invasively might reduce the need for (repeated) biopsies in the future and might justify a longer scan time. A single short-diffusion time DTI protocol, on the other hand, is fast and robust and has proven to be feasible for detecting micro-trauma. The choice of sequence and diffusion times should thus be considered carefully and be adjusted for the specific research question.
Conclusion
To summarize, we investigated skeletal muscle micro-trauma in marathon runners using time-dependent diffusion and the RPBM. We show that RPBM modelling revealed an increased permeability post-marathon. Each diffusion time demonstrated comparable sensitivity in detecting muscle micro-trauma, indicating limited advantage in using longer diffusion times in the range of 100–300 ms. While our findings indicate that spin-echo DTI is adequate for detecting micro-trauma, they also highlight the potential of the RPBM modelling to provide more specific insights into microstructural changes following micro-trauma.
Data availability
The data used in this study are available from the corresponding author on reasonable request.
References
Hyldahl, R. D. & Hubal, M. J. Lengthening our perspective: Morphological, cellular, and molecular responses to eccentric exercise. Muscle Nerve. 49, 155–170. https://doi.org/10.1002/mus.24077 (2014).
Fridén, J., Sjoestroem, M. & Ekblom, B. A morphological study of delayed muscle soreness. Experientia 37, 506–507 (1981).
Clarkson, P. M. & Tremblay, I. Exercise-induced muscle damage, repair, and adaption in humans. J. Appl. Physiol. 65, 1–6 (1988).
Butterfield, T. A. Eccentric exercise in vivo: Strain-induced muscle damage and adaptation in a stable system. Exerc. Sport Sci. Rev. 38, 51–60. https://doi.org/10.1097/JES.0b013e3181d496eb (2010).
Reurink, G. et al. Magnetic resonance imaging in acute hamstring injury: Can we provide a return to play prognosis? Sport Med. 45, 133–146. https://doi.org/10.1007/s40279-014-0243-1 (2014).
Ekstrand, J. et al. Hamstring muscle injuries in professional football: the correlation of MRI findings with return to play. Br. J. Sports Med. 46, 112–117. https://doi.org/10.1136/bjsports-2011-090155 (2012).
Koulouris, G. & Connell, D. Hamstring muscle complex: an imaging review. RadioGraphics 25, 571–586. https://doi.org/10.1177/0363546511419277 (2005).
Zaraiskaya, T., Kumbhare, D. & Noseworthy, M. D. Diffusion tensor imaging in evaluation of human skeletal muscle injury. J. Magn. Reson. Imaging. 24, 402–408. https://doi.org/10.1002/jmri.20651 (2006).
Monte, J. R. et al. DTI and qT2-mapping to monitor muscle recovery following hamstring injury. NMR Biomed. https://doi.org/10.1002/NBM.4902 (2023).
Yanagisawa, O., Kurihara, T., Okumura, K. & Fukubayashi, T. Effects of strenuous exercise with eccentric muscle contraction: Physiological and functional aspects of human skeletal muscle. Magn. Reson. Med. Sci. 9, 179–186. https://doi.org/10.2463/mrms.9.179 (2010).
Hooijmans, M. T. et al. Quantitative MRI reveals microstructural changes in the Upper Leg muscles after running a Marathon. J. Magn. Reson. Imaging. 52 https://doi.org/10.1002/jmri.27106 (2020).
Froeling, M. et al. Muscle changes detected with diffusion-tensor imaging after long-distance running. Radiology 274, 548–562. https://doi.org/10.1148/radiol.14140702 (2015).
Tidball, J. G. Mechanisms of muscle injury, repair, and regeneration. Compr. Physiol. 1, 2029–2062. https://doi.org/10.1002/cphy.c100092 (2011).
Fridén, J. & Lieber, R. L. Structural and mechanical basis of exercise-induced muscle injury. Med. Sci. Sports Exerc. 24, 521–529. https://doi.org/10.1249/00005768-199205000-00005 (1992).
Berry, D. B., Regner, B., Galinsky, V., Ward, S. R. & Frank, L. R. Relationships between tissue microstructure and the diffusion tensor in simulated skeletal muscle. Magn. Reson. Med. 80, 317–329. https://doi.org/10.1002/mrm.26993 (2018).
Polgar, J., Johnson, M. A., Weightman, D. & Appleton, D. Data on fibre size in thirty-six human muscles. An autopsy study. J. Neurol. Sci. 19, 307–318. https://doi.org/10.1016/0022-510X(73)90094-4 (1973).
Novikov, D. S., Fieremans, E., Jensen, J. H. & Helpern, J. A. Random walks with barriers. Nat. Phys. 7, 508–514. https://doi.org/10.1038/nphys1936 (2011).
Fieremans, E. et al. In vivo measurement of membrane permeability and myofiber size in human muscle using time-dependent diffusion tensor imaging and the random permeable barrier model. NMR Biomed. 30 https://doi.org/10.1002/nbm.3612 (2017).
Cameron, D. et al. Diffusion-tensor magnetic resonance imaging captures increased skeletal muscle fibre diameters in Becker muscular dystrophy. J. Cachexia Sarcopenia Muscle (2023).
Lemberskiy, G. et al. Assessment of myofiber microstructure changes due to atrophy and recovery with time-dependent diffusion MRI. NMR Biomed. 34, 1–11. https://doi.org/10.1002/nbm.4534 (2021).
Froeling, M. QMRTools: A Mathematica toolbox for quantitative MRI analysis. J. Open. Source Softw. 4, 1204. https://doi.org/10.21105/joss.01204 (2019).
Veraart, J. et al. Denoising of diffusion MRI using random matrix theory. Neuroimage 142, 394–406. https://doi.org/10.1016/J.NEUROIMAGE.2016.08.016 (2016).
Klein, S., Staring, M., Murphy, K., Viergever, M. A. & Pluim, J. P. W. Elastix: A toolbox for intensity-based medical image registration. IEEE Trans. Med. Imaging. 29, 196–205. https://doi.org/10.1109/TMI.2009.2035616 (2010).
Tax, C. M. W., Otte, W. M., Viergever, M. A., Dijkhuizen, R. M. & Leemans, A. REKINDLE: Robust extraction of kurtosis INDices with linear estimation. Magn. Reson. Med. 73, 794–808. https://doi.org/10.1002/MRM.25165/ASSET/SUPINFO/MRM25165-SUP-0006-SUPPFIG6.TIF (2015).
Leemans, A., Jeurissen, B., Sijbers, J. & Jones, D. K. ExploreDTI: A graphical toolbox for processing, analyzing, and visualizing diffusion MR data. Proc. Intl Soc. Mag Reson. Med. 17, 3537 (2009).
Steidle, G. & Schick, F. Addressing spontaneous signal voids in repetitive single-shot DWI of musculature: spatial and temporal patterns in the calves of healthy volunteers and consideration of unintended muscle activities as underlying mechanism. NMR Biomed. 28, 801–810 (2015).
Berry, D. B., Englund, E. K., Galinsky, V., Frank, L. R. & Ward, S. R. Varying diffusion time to discriminate between simulated skeletal muscle injury models using stimulated echo diffusion tensor imaging. Magn. Reson. Med. 1–13. https://doi.org/10.1002/mrm.28598 (2020).
Dietrich, O., Raya, J. G., Reeder, S. B., Reiser, M. F. & Schoenberg, S. O. Measurement of signal-to-noise ratios in MR images: Influence of multichannel coils, parallel imaging, and reconstruction filters. J. Magn. Reson. Imaging. 26, 375–385. https://doi.org/10.1002/jmri.20969 (2007).
Yushkevich, P. A. et al. User-guided 3D active contour segmentation of anatomical structures: Significantly improved efficiency and reliability. Neuroimage 31, 1116–1128. https://doi.org/10.1016/J.NEUROIMAGE.2006.01.015 (2006).
Froeling, M., Nederveen, A. J., Nicolay, K. & Strijkers, G. J. DTI of human skeletal muscle: The effects of diffusion encoding parameters, signal-to-noise ratio and T2 on tensor indices and fiber tracts. NMR Biomed. 26, 1339–1352. https://doi.org/10.1002/nbm.2959 (2013).
Peetrons, P. Ultrasound of muscles. Eur. Radiol. 12, 35–43. https://doi.org/10.1007/s00330-001-1164-6 (2002).
McDowell, A. R., Feiweier, T., Muntoni, F., Hall, M. G. & Clark, C. A. Clinically feasible diffusion MRI in muscle: Time dependence and initial findings in Duchenne muscular dystrophy. Magn. Reson. Med. 1–9. https://doi.org/10.1002/mrm.28945 (2021).
Tanner, J. E. Self diffusion of water in frog muscle. Biophys. J. 28, 107–116. https://doi.org/10.1016/S0006-3495(79)85162-0 (1979).
Sigmund, E. E. et al. Stimulated echo diffusion tensor imaging and SPAIR T2-weighted imaging in chronic exertional compartment syndrome of the lower leg muscles. J. Magn. Reson. Imaging. 38, 1073–1082. https://doi.org/10.1002/jmri.24060 (2013).
Teruel, J. R. et al. Stimulated echo diffusion tensor imaging (STEAM-DTI) with varying diffusion times as a probe of breast tissue. J. Magn. Reson. Imaging. 45, 84–93. https://doi.org/10.1002/jmri.25376 (2017).
Giraudo, C. et al. Normalized STEAM-based diffusion tensor imaging provides a robust assessment of muscle tears in football players: Preliminary results of a new approach to evaluate muscle injuries. Eur. Radiol. 28, 2882–2889. https://doi.org/10.1007/s00330-017-5218-9 (2018).
Basser, P. J. & Jones, D. K. Diffusion-tensor MRI: Theory, experimental design and data analysis - A technical review. NMR Biomed. 15, 456–467. https://doi.org/10.1002/nbm.783 (2002).
Porcari, P. et al. Time-dependent diffusion MRI as a probe of microstructural changes in a mouse model of Duchenne muscular dystrophy. NMR Biomed. 33, e4276. https://doi.org/10.1002/NBM.4276 (2020).
Winters, K. V., Reynaud, O., Novikov, D. S., Fieremans, E. & Kim, S. G. Quantifying myofiber integrity using diffusion MRI and random permeable barrier modeling in skeletal muscle growth and Duchenne muscular dystrophy model in mice. Magn. Reson. Med. 80, 2094–2108. https://doi.org/10.1002/mrm.27188 (2018).
Malis, V. et al. Time-dependent diffusion tensor imaging and diffusion modeling of age-related differences in the medial gastrocnemius and feasibility study of correlations to histopathology. NMR Biomed e4996. (2023). https://doi.org/10.1002/nbm.4996
Sigmund, E. E. et al. Time-dependent diffusion in skeletal muscle with the random permeable barrier model (RPBM): Application to normal controls and chronic exertional compartment syndrome patients. NMR Biomed. 27, 519–528. https://doi.org/10.1002/nbm.3087 (2014).
Monte, J. R. et al. The repeatability of bilateral diffusion tensor imaging (DTI) in the upper leg muscles of healthy adults. Eur. Radiol. 30, 1709–1718. https://doi.org/10.1007/s00330-019-06403-5 (2019).
Englund, E. K., Reiter, D. A., Shahidi, B. & Sigmund, E. E. Intravoxel incoherent motion magnetic resonance imaging in skeletal muscle: Review and future directions. J. Magn. Reson. Imaging. 55 https://doi.org/10.1002/jmri.27875 (2022).
Rauh, S. S. et al. Accelerated IVIM–corrected DTI in acute hamstring injury: Towards a clinically feasible acquisition time. Eur. Radiol. Exp. 1, 1–14. https://doi.org/10.1186/s41747-024-00437-1 (2024).
Wu, D. & Zhang, J. Evidence of the diffusion time dependence of intravoxel incoherent motion in the brain. Magn. Reson. Med. 82, 2225–2235. https://doi.org/10.1002/mrm.27879 (2019).
Thian, Y. et al. Effect of diffusion time on intravoxel incoherent motion parameters in abdominal organs. Proc. 22nd Sci. Meet Int. Soc. Magn. Reson. Med. 22, 4457 (2014).
Lopez Kolkovsky, A. L. et al. Multiparametric aging study across adulthood in the leg through quantitative MR imaging, 1H spectroscopy, and 31P spectroscopy at 3T. J Magn Reson Imaging. (2024). https://doi.org/10.1002/jmri.29368
Burakiewicz, J. et al. Improved olefinic fat suppression in skeletal muscle DTI using a magnitude-based dixon method. Magn. Reson. Med. 79, 152–159. https://doi.org/10.1002/mrm.26655 (2018).
Acknowlegements
Grans Support: Dutch Technology Foundation TTW (DIMASK #15500). Sportinnovator grant of The Netherlands Organization for Health Research and Development, ZonMw(#50-53800-98-PR020).
Author information
Authors and Affiliations
Contributions
Conceptualization: D.C., M.M., M.F., A.N., G.S., M.H.Data acquisition: M.H.Data analysis: S.R., D.C., F.S., M.F., M.H.Interpretation: S.R., D.C., O.G-J., M.F., H.K., F.S., M.M., G.S., A.N., M.H.Manuscript draft: S.R., D.C., G.S., M.H.Review and approved final version: all authors.
Corresponding author
Ethics declarations
Competing interests
H.E.K. reports research support from Philips Healthcare during the conduct of the study, and trial support from ImagingDMD-UF outside the submitted work. All reimbursements for H.E.K. were received by the LUMC. No personal financial benefits were received. All other authors do not hold any competing interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Rauh, S.S., Cameron, D., Gurney-Champion, O.J. et al. Investigating skeletal muscle micro-trauma with time-dependent diffusion and the random permeable barrier model. Sci Rep 14, 31998 (2024). https://doi.org/10.1038/s41598-024-83644-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-83644-5