Abstract
Health-related behavioral changes may occur following traumatic brain injury. We focused on understanding the impact of mild traumatic brain injury (TBI) on health-related behaviors and identifying factors associated with such changes. We utilized health check-up records from the Korean National Health Insurance Service database spanning January 1, 2009, to December 31, 2017. The sample included 49,212 patients diagnosed with mild TBI and 1:1 matched controls who participated in national health check-ups in 2009–2010, 2011–2012, and 2016–2017. Multivariable logistic regression analysis was utilized to examine the association between mild TBI and short- and long-term health-related behavioral changes. Mild TBI was significantly associated with an increased risk of insufficient physical activity at the short- [odds ratio (OR), 1.04; 95% confidence interval (CI), 1.01 − 1.07] and long-term (OR, 1.06; 95% CI, 1.03 − 1.09) follow-ups. Age ≥ 65 years and female sex were significant effect modifiers for insufficient physical activity (OR, 1.11; 95% CI, 1.02 − 1.21) and smoking (OR, 1.31; 95% CI, 1.14 − 1.51), respectively. Mild TBI may lead to detrimental health-related behavioral changes, varying by age and sex. Thus, age- and sex-specific interventions may be needed to address these changes.
Similar content being viewed by others
Introduction
Traumatic brain injury (TBI) can cause a wide range of long-term psychiatric and behavioral sequelae, such as depression, anxiety, apathy, disinhibition, psychosis, suicide, and substance-use disorders1,2,3. A previous study reported varying rates of psychiatric disorders following TBI of all severities, with up to 61% for depression, 18% for obsessive-compulsive disorder, 9.8% for psychotic disorders, and 51% for substance-use disorders1.
Contrary to common belief, mild TBI, which accounts for the majority of brain trauma, can also lead to long-term neuropsychiatric complications4,5. Between 15 and 30% of patients who experience mild TBI have persisting cognitive, mood, and somatic symptoms beyond 1 year post-injury1,5. A retrospective cohort study of 9,205 adult patients with mild TBI reported three times greater odds for depression6. In an epidemiological study of adolescents, history of mild TBI was associated with two times greater odds of substance use7. These findings raise the possibility that physical symptoms such as headache, dizziness, and neuropsychiatric complications following mild TBI may influence health-related behaviors, though the mechanism is not yet fully understood.
Importantly, substance-use disorders, and health-related behavior such as smoking and sedentary lifestyle can affect TBI recovery8,9,10. In a multicenter cohort study of 3,063 children and adolescents with acute mild TBI, the 28-day postconcussive symptoms were significantly higher in the rest group (40.1% vs. 28.7%) compared to the physical activity group within 1 week of injury11. Alcohol misuse is associated with negative outcome following TBI and poorer rehabilitation compliance12.
However, previous studies on behavioral changes following TBI focused on moderate-to-severe TBI or all severities levels combined13,14,15,16. A systematic review, which included four studies with no definition of severity, and two studies with severe TBI, concluded that patients with TBI had physical activity levels below recommended guidelines for health maintenance. A prior study reported higher smoking rates among veteran and service members following TBI of all injury severities, compared to the general adult population16.
Therefore, this large population-based study aimed to evaluate the long-term changes in health-related behaviors and associated factors following mild TBI, including age- and sex-specific changes over time.
Methods
Data source
Research data from the Korean National Health Insurance Service (NHIS) were obtained. The NHIS is a mandatory social insurance scheme for South Korea’s population of > 50 million people, with medical information from hospitalizations and outpatient treatment. Medical information is recorded by a clinician upon discharge according to the International Classification of Diseases, 10th revision (ICD-10) and comprises information, including primary and additional diagnoses, surgical history, treatments, and medications. It also provides free annual or biennial health check-ups to adults aged ≥ 40 years or workers aged ≥ 20 years. Health check-ups are commonplace in Korea, with screening rates of > 70%17. The health check-up data include basic health parameters, including height, weight, blood pressure, chest radiography findings, laboratory test results for urine and blood, and information on lifestyle behaviors such as regular exercise, alcohol consumption, and smoking, obtained using self-administered questionnaires.
Study population
The NHIS data were reviewed from 2009 to 2017. The baseline was designated as 2009–2010, and health-related behavior changes after short (1–3 years)- and long (6–8 years)-term follow-ups were observed between 2011–2012 and 2016–2017, respectively. Mild TBI was defined using ICD-10 codes (S06.0). The data included 89,031 patients diagnosed with mild TBI during 2009–2010 who underwent a national health check-up during the same period. Overall, 2,650,343 participants who had received a national health check-up during 2009–2010 but had never been diagnosed with mild TBI during 2009–2010 were also included as controls. Participants diagnosed with mild TBI in 2008 were excluded (mild TBI, n = 1,727; without mild TBI, n = 14,348), to washout participants who experienced mild TBI in the past. Participants who did not undergo a national health check-up in 2011‒2012 and 2016‒2017 were excluded (mild TBI, n = 36,352; without mild TBI, n = 1,037,648). Additionally, participants with missing values for demographic variables (mild TBI, n = 1,713; without mild TBI, n = 53,892) and adolescents aged < 18 years at baseline (mild TBI, n = 27; without mild TBI, n = 841) were excluded. To extract the mild TBI group and the age- and sex-matched without mild TBI group, an equal number of participants were randomly selected from each sex and age stratum of the mild TBI and without mild TBI groups. Matching was performed by assigning random numbers to each stratum of the mild TBI and without mild TBI groups, sorting them in order, and selecting sequentially from the top. Ultimately, 49,212 patients with mild TBI and 1:1 age and sex matched controls (n = 49,212) were included in this study (Supplementary Fig. 1).
Health-related behaviors
Sufficient physical activity (PA), smoking, and alcohol consumption were examined as health-related behaviors based on a self-reported questionnaire from the health check-up data. Sufficient PA was defined based on the International Physical Activity Questionnaire scoring protocol. Sufficient PA was determined according to the amount of vigorous (running, aerobics, fast bicycling, or mountain climbing) or moderate (fast walking, doubles tennis, or bicycling at a regular pace) PA during the last 7 days18: (1) ≥ 20 min of vigorous PA for at least 3 days; (2) ≥ 30 min of moderate PA for at least 5 days; (3) vigorous PA for at least 1–2 days and moderate PA for at least 4 days; or (4) vigorous PA for at least 2 days and moderate PA for at least 3 days. If any of the four criteria was satisfied, it was classified as sufficient PA; otherwise, it was classified as insufficient. Smoking behavior was determined from the following question based on the Centers for Disease Control and Prevention tobacco glossary: “Have you ever smoked more than five packs (100 cigarettes) in your lifetime? (1) Yes, currently smoking; (2) Yes, quit smoking now; (3) No.” Alcohol drinking behavior was ascertained according to the average number of days when alcoholic drinks were consumed per week: (1) ≥ 4 days was defined as heavy drinking; (2) 1–2 days as moderate drinking; and (3) 0 days as no drinking.
Covariates
All sociodemographic variables, such as age, sex, region of residence, and income level, were included at baseline. Household income levels, based on insurance premiums, were divided into quartiles. The region of residence was categorized into urban and rural according to the administrative districts; urban areas included seven metropolitan cities (Seoul, Busan, Daegu, Incheon, Gwangju, Daejeon, and Ulsan) and rural areas included Gyeonggi, Gangwon, Chungcheongbuk, Chungcheongnam, Jeollabuk, Jeollanam, Gyeongsangbuk, Gyeongsangnam, and Jeju. Comorbidities, including diabetes mellitus (fasting glucose level ≥ 126 mg/dL or ICD-10 codes E11–E14), hypertension (blood pressure ≥ 140/90 or ICD-10 codes I10–I13, and I15), dyslipidemia (total cholesterol level ≥ 240 mg/dL or ICD-10 code E78), cerebrovascular diseases (ICD-10 codes I60–I69), and depression (ICD-10 codes F32, F33, F34.1, F41.2), were defined based on diagnosis within a year before the baseline. Charlson Comorbidity Index (CCI) scores were calculated according to ICD-10 codes and categorized into three classes (weighted scores being ≤ 2, 3–4, and ≥ 5)19.
Statistical analyses
Descriptive statistics were used to summarize the general characteristics of participants. The Wilcoxon rank-sum test or chi-squared test were used to compare the baseline characteristics of patients with mild TBI and controls. Multivariable logistic regression analysis was utilized to examine the association between mild TBI and short- and long-term health-related behavioral changes. Four logistic regression models were used to adjust for covariates. Model 1 was a crude model, and unadjusted odds ratios (ORs) with 95% confidence intervals (CIs) were calculated; Model 2 was adjusted for age, sex, and baseline health-related behaviors (sufficient PA, smoking, or alcohol consumption, respectively); Model 3 was adjusted for age, sex, baseline health-related behaviors, region of residence, and household income ; and Model 4 was adjusted for age, sex, baseline health-related behaviors, region of residence, household income, comorbidities (diabetes mellitus, hypertension, dyslipidemia, cerebrovascular disease, and depression), and CCI score. In the sensitivity analysis, the definition of sufficient PA was modified as (1) vigorous PA for at least 3 days or (2) moderate PA for at least 5 days.
In addition, we performed stratification analyses for sex and age groups. In the sex stratification analysis, we divided the participants into males and females and performed a multivariable logistic regression analysis with mild TBI as the exposure and health-related behaviors as the outcome in each stratum. We included all covariates in Model 4 except sex as a stratification variable. For the age group stratification analysis, we divided the participants into two strata, 65 years and older and younger than 65 years, and performed a multivariable logistic regression analysis for each stratum. We included all covariates in Model 4, including age as a continuous variable.
To determine whether sex and age were significant effect modifiers that modify the association between mild TBI and health-related behaviors, we further examined the interaction of mild TBI with age and sex. Interaction terms were created by introducing variable × variable. The model to test the interaction was constructed by adding the interaction term to model 4.
The SAS version 9.4 statistical software (SAS Institute, Cary, NC, USA) was used for statistical analysis, which was conducted in 2023. All reported p values are two-sided. Statistical significance was set at P < 0.05.
Statement of ethics
This study was performed in accordance with the ethical standards established in the Declaration of Helsinki. The requirement for ethical approval of this study and the need to obtain informed consent was waived by the Institutional Review Board of Seoul National University Hospital, Seoul, South Korea (IRB no. E-2212-110-1387).
Results
Table 1 presents the characteristics of the study population, age and sex-matched between the mild TBI and control groups at baseline (2009–2010). Fewer participants in the mild TBI group resided in urban areas or belonged to the highest household income bracket compared to those in the control group. Conversely, the control group had more individuals with past dyslipidemia. At baseline, the mild TBI group had a greater prevalence of current smokers and heavy drinkers, while the proportion of participants with sufficient PA was similar between both groups.
Table 2 presents the association of mild TBI and other related factors with insufficient PA. After full adjustment in Model 4, mild TBI was significantly associated with an increased risk of insufficient PA at the short- (OR, 1.04; 95% CI, 1.01 − 1.07) and long-term (OR, 1.06; 95% CI, 1.03 − 1.09) follow-ups. Covariates, including age, sex, baseline PA, residence, and household income levels, were associated with insufficient PA at the short-term and long-term follow-ups, while comorbidities were associated with insufficient PA only at the short-term follow-up. In a sensitivity analysis using the modified definition of sufficient PA, mild TBI showed a significant association with increased risk of insufficient PA at the short- (OR, 1.04; 95% CI, 1.01 − 1.08) and long-term (OR, 1.06; 95% CI, 1.03 − 1.09) follow-ups (Supplementary Table 1).
The association of mild TBI and other related factors with current smoking status is shown in Table 3. In the fully adjusted model, mild TBI was significantly associated with an increased risk of current smoking at both short- (OR, 1.10; 95% CI, 1.05 − 1.15) and long-term (OR, 1.16; 95% CI, 1.11 − 1.21) follow-ups. This was also true for other covariates, including age, sex, baseline smoking behavior, and household income level.
The association of mild TBI and other related factors with heavy alcohol consumption is shown in Table 4. After full adjustment, a significantly increased risk of heavy drinking was observed at both short- (OR, 1.19; 95% CI, 1.11 − 1.28) and long-term (OR, 1.13; 95% CI, 1.06 − 1.21) follow-ups. Among the other covariates, age, sex, baseline alcohol drinking behavior, and household income levels were also significantly associated with heavy alcohol consumption.
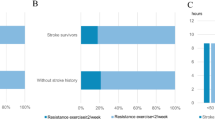
After stratification by sex, we found that mild TBI was significantly linked to insufficient PA only in women at both short-term (OR, 1.09; 95% CI, 1.04–1.14) and long-term (OR, 1.09; 95% CI, 1.04–1.14) follow-ups. A significant interaction between mild TBI and sex on insufficient PA was observed at the short-term follow-up (p for interaction = 0.0041). Significant interactions between mild TBI and sex, on current smoking were observed at both short-term (p for interaction < 0.001) and long-term (p for interaction < 0.001) follow-ups. Furthermore, mild TBI showed a significantly increased association with heavy drinking regardless of sex at the short-term follow-up. There was no significant interaction between mild TBI and sex on heavy drinking (Fig. 1).
Associations of mild TBI with health-related behaviors after stratification by sex. The model for stratification by sex was adjusted for age, baseline health-related behaviors (sufficient physical activity, smoking, or drinking, respectively), region of residence, household income, comorbidities (diabetes mellitus, hypertension, dyslipidemia, cerebrovascular diseases, and depression), and CCI score. The model to evaluate the p-value for interaction was created by adding the interaction term to the full adjustment model, which is model 4. TBI, traumatic brain injury; CCI, Charlson Comorbidity Index; OR, odds ratio; CI, confidence interval.
After stratification by age group, mild TBI was significantly associated with insufficient PA in the older age group (≥ 65 years), at both short- and long-term follow-ups. However, in the younger age group (< 65 years), mild TBI showed a significant association with insufficient PA only at long-term follow-up. A significant interaction between mild TBI and age group on insufficient PA was observed at both short- (p for interaction < 0.001) and long-term (p for interaction < 0.001) follow-ups. There was no significant interaction between mild TBI and age group on current smoking and heavy drinking (Fig. 2).
Associations of mild TBI with health-related behaviors after stratification by age groups. The model for stratification by age group was adjusted for age, sex, baseline health-related behaviors (sufficient physical activity, smoking, or drinking, respectively), region of residence, household income, comorbidities (diabetes mellitus, hypertension, dyslipidemia, cerebrovascular diseases, and depression), and CCI score. The model to evaluate the p-value for interaction was created by adding the interaction term to the full adjustment model, which is model 4. TBI, traumatic brain injury; CCI, Charlson Comorbidity Index; OR, odds ratio; CI, confidence interval.
Discussion
Health-related behaviors may change up to eight years following mild TBI, with potentially increased odds of insufficient PA, current smoking, and heavy alcohol use. Women appear to have higher odds of insufficient PA post-mild TBI compared to women without mild TBI. They also seem to face higher odds of smoking than men. Individuals aged ≥ 65 years may be at higher odds of insufficient PA following TBI, compared to younger individuals.
PA
Mild TBI is associated with a greater likelihood of reduced PA, persisting after adjustments for age, sex, pre-injury activity levels, comorbidities, and socioeconomic status. These findings are consistent across various definitions of PA (Supplementary Table 1), corroborating studies that noted decreased PA post-TBI15,20. A systematic review found that individuals with TBI have PA levels that are below recommended guidelines15. However, the review included six small studies, only two of which reported TBI severity. Both studies included patients with severe TBI. In a study by Mercier et al., 27% of patients with mild TBI reported meeting PA guidelines post-injury, compared with 85% pre-injury20. Unlike our research, their study was a cross-sectional cohort of patients aged 18–65 years who visited a single center. Additionally, their study did not examine the effect of age and sex.
Our findings suggest that women may be more prone to insufficient PA after mild TBI compared to women without mild TBI, and that adults aged ≥ 65 years could remain at risk for up to 8 years. The literature on women’s behavioral changes post-TBI is limited, with small sample sizes and lack of direct comparisons between genders15. One study reported lower PA levels in moderate-to-severe TBI patients aged ≥ 45 compared to the general population21. Our study extends these finding by indicating that adults aged ≥ 65 are at higher odds of insufficient PA even after mild TBI.
Increased physical inactivity after TBI may stem from factors including an avoidance coping strategy, fear of exacerbating symptoms, trauma, or falling22. It may manifest from neurobehavioral dysregulation after TBI23, impacting an individual’s ability or inclination to engage in PA. Despite its prevalence, the precise mechanism and underlying pathophysiology of physical inactivity following TBI remains unknown. Men and women differ in the mechanism of injury and endogenous hormonal profiles, which may distinctly affect behavior24. Disparities in PA levels according to age and sex could be attributed to barriers hindering PA engagement25. Further studies should explore the potential association of age and sex with PA following TBI.
Smoking
The current research on smoking and TBI shows mixed results. A recent survey of Ohioans with a lifetime TBI history found a 1.7 times higher risk of smoking26, and a study of Canadian adults with a TBI history reported a 2.15 times increased risk of smoking27. However, a nationally representative cross-sectional survey of Canadians did not identify a significant difference in smoking risk between patients with TBI and non-injured controls14. These studies relied on a cross-sectional design, and TBI was evaluated through self-report. Our study adds new findings, suggesting a heightened odds of smoking among patients diagnosed with mild TBI, particularly in women. The reasons for the differing smoking risks according to sex remain unclear, but stress and depression, which may increase significantly after TBI28, could contribute. Previous research has highlighted sex-specific differences in depressive symptoms after mild-to-moderate TBI, with women experiencing higher rates of chronic stress than men in the 6–12 months following injury29. Adjusting for depression did not mitigate the smoking risk post-TBI, indicating the possible influence of other factors.
Alcohol consumption
Substance abuse and binge drinking subsequent to TBI are well documented9,13,26. Bogner et al. reported a 1.7-fold increased risk of heavy drinking in individuals with a TBI history26. Moreover, a prospective study of patients with TBI demonstrated that 17.4% of these patients were binge drinking at 1 year and 25.4% by 2 years post-injury13. Our study suggests that the odds of heavy drinking may increase following mild TBI and could extend up to 7–8 years post-injury. In contrast to previous studies that reported the association of the male sex and young age with heavy alcohol use following TBI13,30, age and sex were not significant effect modifiers following mild TBI.
Social disparities
Social disparities in health-related behaviors and diseases have been reported in other populations31,32,33. Similarly, our findings suggested social disparities in health behaviors among Koreans. Insufficient PA was observed to rise significantly with rural residence. Conversely, the risk of insufficient PA, current smoking and heavy alcohol consumption appeared lowest in the highest-income group during both short- and long-term follow-ups.
Limitations
Our research has some limitations. First, mild TBI was diagnosed based on ICD-10 codes and not a clinical diagnosis confirmed by physicians. However, previously reported overall specificity and positive predictive value of ICD-10 codes were high34,35. Second, our participants received regular health check-ups, potentially leading to selection bias towards people who are somewhat health-conscious. Despite this, our results suggest that even health-conscious people may be at risk of health-related behavioral change. Third, self-reporting was used to evaluate health-related behavior, which may not be as reliable as objective measures. Fourth, not all possible confounding factors, including medication, family support, education, and stress levels, were studied36. Lastly, information on PA intensity and amount of alcohol consumption was unavailable. Despite these limitations, our study had strengths. It was a large population-based study with a long-term follow-up of up to eight years. We focused specifically on mild TBI, which was not previously studied in depth13,14,15,16.
Conclusion
Although mild TBI is not typically associated with long-term disabilities, it may prompt changes in health behaviors. Patients with mild TBI aged ≥ 65 years appear to have increased odds of insufficient PA. Women with mild TBI may be more prone to smoking than those without mild TBI. Consequently, routine monitoring of health behaviors, patient education, and tailored interventions for age and sex could be beneficial after mild TBI. These findings, noted in Korea, may differ in other ethnic and socioeconomic contexts. Cross-cultural validation is necessary to confirm these results’ applicability.
Data availability
The data that support the findings of this study are available from the Korean National Health Insurance Service Database (NHIS-2023-1-026) but restrictions apply to the availability of these data, which were used under license for the current study and so are not publicly available. Data are however available from the corresponding author, Byung-Mo Oh in aggregate form upon reasonable request and with permission from the Korean National Health Insurance Service. Byung-Mo Oh had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
Haarbauer-Krupa, J. et al. Epidemiology of chronic effects of traumatic brain injury. J. Neurotrauma 38, 3235–3247. https://doi.org/10.1089/neu.2021.0062 (2021).
Li, L. M., Carson, A. & Dams-O’Connor, K. Psychiatric sequelae of traumatic brain injury—Future directions in research. Nat. Rev. Neurol. 19, 556–571. https://doi.org/10.1038/s41582-023-00853-8 (2023).
Pavlovic, D., Pekic, S., Stojanovic, M. & Popovic, V. Traumatic brain injury: Neuropathological, neurocognitive and neurobehavioral sequelae. Pituitary 22, 270–282. https://doi.org/10.1007/s11102-019-00957-9 (2019).
Williams, W. H., Potter, S. & Ryland, H. Mild traumatic brain injury and postconcussion syndrome: A neuropsychological perspective. J. Neurol. Neurosurg. Psychiatry 81, 1116–1122. https://doi.org/10.1136/jnnp.2008.171298 (2010).
Sterr, A., Herron, K. A., Hayward, C. & Montaldi, D. Are mild head injuries as mild as we think? Neurobehavioral concomitants of chronic post-concussion syndrome. BMC Neurol. 6, 7. https://doi.org/10.1186/1471-2377-6-7 (2006).
Izzy, S. et al. Concussion and risk of chronic medical and behavioral health comorbidities. J. Neurotrauma 38, 1834–1841. https://doi.org/10.1089/neu.2020.7484 (2021).
Veliz, P., McCabe, S. E., Eckner, J. T. & Schulenberg, J. E. Concussion, sensation-seeking and substance use among US adolescents. Subst. Abus. 42, 183–191. https://doi.org/10.1080/08897077.2019.1671938 (2021).
Zhang, Y. et al. The benefits of exercise for outcome improvement following traumatic brain injury: Evidence, pitfalls and future perspectives. Exp. Neurol. 349, 113958. https://doi.org/10.1016/j.expneurol.2021.113958 (2022).
Weil, Z. M., Corrigan, J. D. & Karelina, K. Alcohol use disorder and traumatic brain injury. Alcohol Res. 39, 171–180 (2018).
Sivandzade, F., Alqahtani, F., Sifat, A. & Cucullo, L. The cerebrovascular and neurological impact of chronic smoking on post-traumatic brain injury outcome and recovery: An in vivo study. J. Neuroinflamm. 17, 133. https://doi.org/10.1186/s12974-020-01818-0 (2020).
Grool, A. M. et al. Association between early participation in physical activity following acute concussion and persistent postconcussive symptoms in children and adolescents. JAMA 316, 2504–2514. https://doi.org/10.1001/jama.2016.17396 (2016).
Weil, Z. M., Corrigan, J. D. & Karelina, K. Alcohol abuse after traumatic brain injury: Experimental and clinical evidence. Neurosci. Biobehav. Rev. 62, 89–99. https://doi.org/10.1016/j.neubiorev.2016.01.005 (2016).
Ponsford, J., Whelan-Goodinson, R. & Bahar-Fuchs, A. Alcohol and drug use following traumatic brain injury: A prospective study. Brain Inj. 21, 1385–1392. https://doi.org/10.1080/02699050701796960 (2007).
Allen, S., Stewart, S. H., Cusimano, M. & Asbridge, M. Examining the relationship between traumatic brain injury and substance use outcomes in the canadian population. Subst. Use Misuse 51, 1577–1586. https://doi.org/10.1080/10826084.2016.1188955 (2016).
Hamilton, M., Khan, M., Clark, R., Williams, G. & Bryant, A. Predictors of physical activity levels of individuals following traumatic brain injury remain unclear: A systematic review. Brain Inj. 30, 819–828. https://doi.org/10.3109/02699052.2016.1146962 (2016).
Silva, M. A. et al. Prevalence and predictors of tobacco smoking in veterans and service members following traumatic brain injury rehabilitation: A VA TBIMS study. Brain Inj. 32, 994–999. https://doi.org/10.1080/02699052.2018.1468576 (2018).
Kang, H. T. Current status of the national health screening programs in South Korea. Korean J. Fam. Med. 43, 168–173. https://doi.org/10.4082/kjfm.22.0052 (2022).
Lee, Y. et al. The effect of health-related behaviors on disease progression and mortality in early stages of chronic kidney disease: A Korean nationwide population-based study. J. Clin. Med. 8, https://doi.org/10.3390/jcm8081100 (2019).
Glasheen, W. P. et al. Charlson comorbidity index: ICD-9 update and icd-10 translation. Am. Health Drug Benef. 12, 188–197 (2019).
Mercier, L. J. et al. Characterizing physical activity and sedentary behavior in adults with persistent postconcussive symptoms after mild traumatic brain injury. Arch. Phys. Med. Rehabil. 102, 1918-1925.e1911. https://doi.org/10.1016/j.apmr.2021.05.002 (2021).
Pham, T. et al. Physical activity and perceived barriers in individuals with moderate-to-severe traumatic brain injury. Pm R https://doi.org/10.1002/pmrj.12854 (2022).
Cassetta, B. D., Cairncross, M., Brasher, P. M. A., Panenka, W. J. & Silverberg, N. D. Avoidance and endurance coping after mild traumatic brain injury are associated with disability outcomes. Rehabil. Psychol. 66, 160–169. https://doi.org/10.1037/rep0000372 (2021).
Howlett, J. R., Nelson, L. D. & Stein, M. B. Mental health consequences of traumatic brain injury. Biol. Psychiatry 91, 413–420. https://doi.org/10.1016/j.biopsych.2021.09.024 (2022).
Blaya, M. O., Raval, A. P. & Bramlett, H. M. Traumatic brain injury in women across lifespan. Neurobiol. Dis. 164, 105613. https://doi.org/10.1016/j.nbd.2022.105613 (2022).
Pinto, S. M., Newman, M. A. & Hirsch, M. A. Perceived barriers to exercise in adults with traumatic brain injury vary by age. J. Funct. Morphol. Kinesiol. 3, https://doi.org/10.3390/jfmk3030047 (2018).
Bogner, J. et al. Lifetime history of traumatic brain injury and behavioral health problems in a population-based sample. J. Head Trauma Rehabil. 35, E43-e50. https://doi.org/10.1097/htr.0000000000000488 (2020).
Ilie, G. et al. Associations between a history of traumatic brain injuries and current cigarette smoking, substance use, and elevated psychological distress in a population sample of Canadian adults. J. Neurotrauma 32, 1130–1134. https://doi.org/10.1089/neu.2014.3619 (2015).
Choi, Y. et al. Incidence of depression after traumatic brain injury: A nationwide longitudinal study of 2.2 million adults. J. Neurotrauma 39, 390–397. https://doi.org/10.1089/neu.2021.0111 (2022).
Bay, E., Sikorskii, A. & Saint-Arnault, D. Sex differences in depressive symptoms and their correlates after mild-to-moderate traumatic brain injury. J. Neurosci. Nurs. 41, 298–309. https://doi.org/10.1097/jnn.0b013e3181b6be81 (2009).
Horner, M. D. et al. Patterns of alcohol use 1 year after traumatic brain injury: A population-based, epidemiological study. J. Int. Neuropsychol. Soc. 11, 322–330. https://doi.org/10.1017/s135561770505037x (2005).
de Azevedo Barros, M. B., Lima, M. G., Medina, L. P., Szwarcwald, C. L. & Malta, D. C. Social inequalities in health behaviors among Brazilian adults: National Health Survey, 2013. Int. J. Equity Health 15, 148. https://doi.org/10.1186/s12939-016-0439-0 (2016).
Khalatbari-Soltani, S. et al. Socioeconomic status, health-related behaviours, and death among older people: The Concord health and aging in men project prospective cohort study. BMC Geriatr. 20, 261. https://doi.org/10.1186/s12877-020-01648-y (2020).
Lee, Y., Kim, W. S. & Paik, N. J. Gender differences in physical activity and health-related behaviors among stroke survivors: Data from the 5th Korea National Health and Nutrition Examination Survey. Top Stroke Rehabil. 24, 381–387. https://doi.org/10.1080/10749357.2017.1304877 (2017).
St Germaine-Smith, C. et al. Recommendations for optimal ICD codes to study neurologic conditions: A systematic review. Neurology 79, 1049–1055. https://doi.org/10.1212/WNL.0b013e3182684707 (2012).
Warwick, J., Slavova, S., Bush, J. & Costich, J. Validation of ICD-10-CM surveillance codes for traumatic brain injury inpatient hospitalizations. Brain Inj. 34, 1763–1770. https://doi.org/10.1080/02699052.2020.1849801 (2020).
King, A. C. Interventions to promote physical activity by older adults. J. Gerontol. A Biol. Sci. Med. Sci. 56 Spec No 2, 36–46. https://doi.org/10.1093/gerona/56.suppl_2.36 (2001).
Acknowledgements
This study was supported by a grant from the National Research Foundation (NRF-2021R1A2B5B02087294 and RS-2021-NR057975) and the Translational R&D Program on Smart Rehabilitation Exercises (TRSRE-PS02), National Rehabilitation Centre, Ministry of Health and Welfare, Republic of Korea. The funders of this study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
Y.L.: Conceptualization, Methodology, Writing- original draft, review & editing. J.H.L: Conceptualization, Data curation, Methodology, Funding acquisition, Project administration, Writing - review & editing. B.M.O: Conceptualization, Data curation, Methodology, Funding acquisition, Project administration, Writing - review & editing. J.J.: Formal analysis, Writing - review & editing. Y.C.: Data curation, Formal analysis, Writing- original draft, review & editing. D.K.K: Writing - review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lee, Y., Choi, Y., Jeon, J. et al. Impact of mild traumatic brain injury on health behaviors. Sci Rep 15, 1585 (2025). https://doi.org/10.1038/s41598-024-83920-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-83920-4