Abstract
The efficacy of neoadjuvant therapy varies significantly with hormone receptor (HR) status for patients with human epidermal growth factor receptor 2 (HER2) positive breast cancer (BC). Despite extensive research on HER2 + BC, the optimal neoadjuvant strategy for HR+/HER2 + BC remains inconclusive. This study aimed to identify the optimal neoadjuvant regimen for HR+/HER2 + BC treatment. We conducted a systematic search for trials comparing neoadjuvant regimens for HR+/HER2 + BC and a network meta-analysis. Odds ratios for pathological complete response (pCR) and hazard ratios for event-free survival (EFS) were calculated. Treatment regimens were ranked using the surface under the cumulative ranking curve. 20 trials with 2809 patients were included. In pCR analysis, three neoadjuvant regimens sequentially ranked at the top, namely those comprising T-DM1, pertuzumab with trastuzumab, and tyrosine kinase inhibitor with trastuzumab, demonstrating significantly higher pCR rates than monotherapies. In EFS analysis, pertuzumab with trastuzumab ranked the first while T-DM1 containing regimen ranked the last. Anthracycline-free regimens showed a marginally higher pCR rate than anthracycline-containing regimens, while carboplatin-containing regimens demonstrated a numerically higher pCR rate than carboplatin-free regimens. Significant heterogeneity was observed in endocrine therapy analysis, which may be caused by different strategies for incorporating endocrine therapy. In conclusion, trastuzumab plus pertuzumab stands out as the optimal neoadjuvant HER2-targeting regimen for HR+/HER2 + BC Furthermore, anthracycline-free carboplatin-containing chemotherapy emerges as a promising combination treatment. Further investigation is required to clarify the role of endocrine therapy in HR+/HER2 + BC to guide its clinical application.
Similar content being viewed by others
Introduction
Neoadjuvant treatment is highly recommended for patients with human epidermal growth factor receptor 2-positive (HER2+) breast cancer (BC), given its well-established benefits in improving surgery outcome and survival1,2. Pathological complete response (pCR) is a standard endpoint for measuring the short-term outcome of neoadjuvant treatment, while the long-term endpoints are often survival outcomes3. Approximately 50–70% of HER2 + BC cases also express hormone receptors (HR), which have a complex crosstalk with HER24,5. The HR-positive (HR+)/HER2 + population faces higher treatment resistance and a less favorable prognosis6. Achieving pCR in neoadjuvant therapy is more challenging in the HER2+/HR + population when compared with the HER2+/HR-negative (HR-) population7. This highlights an unmet clinical need to determine the optimal neoadjuvant strategy for HR+/HER2 + BC. Commonly used regimens and drugs are summarized in Supplementary Table S1.
Targeted therapy for HER2 + BC has advanced significantly over the past decades. Trastuzumab combined with pertuzumab is the current standard of care for primary HER2 + BC in the neoadjuvant setting1,2. Besides, novel HER2-targeting therapies showed promising results in the neoadjuvant setting, such as antibody-drug conjugate trastuzumab emtansine (T-DM1)8,9 or trastuzumab deruxtecan (T-DXd)10 and tyrosine kinase inhibitor (TKI) neratinib11 or pyrotinib12. These trials confirmed that the HR + population achieved lower pCR rates than the HR- population. Notably, no head-to-head comparison of all regimens has been conducted in the HR+/HER2 + population, raising the question of whether the HR + population might benefit from different HER2-targeting regimens compared to the overall HER2 + population.
Chemotherapy exhibits reduced benefits in the HR + BC population compared to HR- BC13. Therefore, there is a growing trend to minimize chemotherapy to balance risks and benefits14. Conventionally, anthracyclines were frequently used in chemotherapy regimens. However, recent studies have shown that the cardiotoxicity of anthracyclines may be superimposed with antibodies15, and omitting the use of anthracyclines does not influence pCR or survival outcomes in patients with HER2 + BC16. The TRYPHAENA trial added carboplatin to anthracycline-free neoadjuvant chemotherapy, which yielded similar pCR and event-free survival (EFS) between both groups17, establishing the role of carboplatin in treating HER2 + BC. Therefore, there are clinical considerations regarding whether anthracyclines could be omitted and whether carboplatin should be added to neoadjuvant chemotherapy regimens for HR+/HER2 + BC treatment.
Due to the complex interaction between the downstream pathways of HR and HER2, endocrine therapy (ET) is recommended for HR+/HER2 + BC treatment18,19. Dual pathway blockade has demonstrated considerable efficacy in advanced BC20,21,22. Therefore, neoadjuvant ET has been well studied in the HR+/HER2 + population and yielded positive outcomes23,24,25,26. Nonetheless, debates persist regarding the clinical applications of neoadjuvant ET, including its optimal timing, potential long-term impact on prognosis, the suitability of pCR as an efficacy endpoint, and its potential to replace chemotherapy.
Previous network meta-analyses have primarily focused on the overall HER2 + BC population, with limited exploration of the HR+/HER2 + subgroup.16,27,28,29,30, While a few studies have evaluated pCR rates across regimens for HR+/HER2 + BC, these analyses often lacked comprehensive consideration of long-term outcomes16,30,31.
Leveraging newly released data from recent trials, such as WGS-TP-II32 and PHEDRA12, this study aims to demonstrate the optimal HER2-targeting regimen for HR+/HER2 + BC by integrating both short-term and long-term outcomes. Additionally, we aimed to explore the roles of carboplatin, anthracycline, and ET in the neoadjuvant period, providing updated insights into the management of this challenging subgroup.
Materials and methods
Search strategy and selection criteria
This study is a systematic review with network meta-analysis. Our review protocol was registered on the PROSPERO website (CRD42023385644), and this systematic review is reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and its extension for network meta-analysis33,34,35.
Literature was retrieved from Medline, EMBASE, Cochrane Library, and Web of Science with no restrictions on publication year or language. Detailed strategies used in each database are provided in Supplementary Table S2–S5. Search terms were built based on population, intervention, and outcome of interest. References of formerly published trials and reviews were also checked for missing literature. Unpublished trials and gray literature were not included.
The predefined inclusion and exclusion criteria are as follows: Neoadjuvant clinical trials were eligible if they met all the following criteria: (1) included patients with HR+/HER2 + BC, (2) compared any neoadjuvant regimens that included HER2-targeting therapies, and (3) reported any pCR or EFS (or disease-free survival) outcome. Trials were excluded if they (1) were bioequivalence studies, (2) did not report the outcome of patients with HR+/HER2 + BC, and (3) compared solely on variations in dose or sequence between treatment regimens. The literature retrieved was selected by two reviewers independently.
Interventions
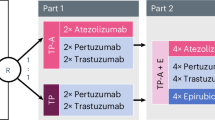
Interventions were merged according to HER2-targeting therapies of the neoadjuvant regimens, and interventions of interest included six types as follows:
-
(1)
T-DM1-based regimens (T-DM1), which include T-DM1 alone, T-DM1 + pertuzumab, or T-DM1 + lapatinib, either with or without chemotherapy or ET.
-
(2)
trastuzumab and pertuzumab with chemotherapy (HP + C).
-
(3)
trastuzumab and TKI with chemotherapy (H + TKI + C). TKI includes lapatinib, neratinib, and pyrotinib.
-
(4)
trastuzumab with chemotherapy (H + C).
-
(5)
lapatinib with chemotherapy (L + C).
-
(6)
any chemotherapy with no HER2-targeting regimen (C).
Outcomes
The primary outcome of this study was the number of patients achieving pCR, defined as the absence of residual invasive cancer in the breast and no pathological involvement of axillary lymph nodes (ypT0/Tis ypN0). Other definitions of pCR were also accepted as (1) the absence of residual invasive and in situ cancer in the breast and no pathological involvement of axillary lymph nodes (ypT0 ypN0) or (2) the absence of residual invasive cancer in the breast (ypT0/Tis) since some trials did not report ypT0/Tis ypN0, and sensitivity analysis was conducted to assess the potential bias involved by this. The secondary outcome was EFS, defined as the time from randomization to an event which may include disease progression, discontinuation of the treatment for any reason, or death.
Data analysis
All data were independently extracted by two reviewers. Data were extracted on summary estimates, including trial characteristics (trial name, register number, starting year, country, and total participants), patient characteristics (age, tumor stage, tumor size, menopausal status, and HR status), intervention details (regimen and total duration), and interested outcomes. For pCR, the number of patients and the pCR definitions in the corresponding trial were extracted. For EFS, three-year or five-year EFS rates, hazard ratios (HRs), and the 95% confidence interval (CI) between treatment arms were extracted.
All studies included were assessed for the risk of bias with the Cochrane risk-of-bias tool (RoB2)36 by two reviewers independently. Five domains listed below were checked and reported as low risk, some concern, or high risk for each trial.
-
(1)
Bias arising from the randomization process, assessing the generation and concealment of allocation sequence, and the differences between intervention groups.
-
(2)
Bias due to deviations from intended interventions, assessing the blinding of participants and personnel, and deviations from the intended interventions.
-
(3)
Bias due to missing outcome data, assessing the availability of outcome data.
-
(4)
Bias in the measurement of the outcome, assessing the appropriateness and blinding of outcome assessment.
-
(5)
Bias in the selection of the reported result.
All statistical analyses were conducted based on the HR+/HER2 + BC population. For each comparison of regimens reported in more than one trial, we performed a direct meta-analysis with odds ratios (ORs) of pCR for pooling effect sizes. A common effect model was used, and ORs were reported with 95% CIs, where a random effects model was also conducted for sensitivity analysis. All tests were two-sided and statistical significance was set at p < 0·05. Cochran’s Q test was performed to assess the statistical heterogeneity. For comparison groups with I2 statistic > 25% or p-value of the Q test < 0·1, sensitivity analysis was conducted to identify the source of heterogeneity by deleting each trial. Peter’s test was conducted to assess publication bias in each direct comparison, and results were presented by funnel plots37.
For indirect comparisons, we conducted a network meta-analysis with the common effect model in a Bayesian framework. Four Markov chains were run for 50,000 simulation iterations after 10,000 tuning iterations. ORs with 95% CIs for pCR analysis and HRs with 95% CIs for EFS analysis were reported. A node-splitting analysis was performed to determine the inconsistency between direct and indirect comparisons38, and a comparison-adjusted funnel plot was constructed to evaluate the small-study effects across the network39. Sensitivity analysis was performed by reevaluating the results while excluding trials with a high risk of overall bias, using other TKIs than lapatinib, or reporting pCR outcomes in different definitions. The ranking probability was evaluated for each treatment regimen and summarized with the surface under the cumulative ranking curve (SUCRA). A clustered SUCRA ranking plot considering both pCR and EFS was also presented40.
To further analyze the efficacy of chemotherapy and ET regimens, direct comparisons were performed between anthracycline-containing and non-anthracycline therapy, carboplatin-containing and non-carboplatin therapy, as well as regimens with or without ET. Heterogeneity was assessed with Cochran’s Q test, and subgroup analysis was performed to identify its source.
All statistical analyses were conducted in R version 4.3.1. Plots in risk of bias analysis were made with the ‘robvis’ package. Direct meta-analysis was performed with ‘meta’ package. Bayesian network meta-analysis was performed with ‘gemtc’ and ‘rjags’ package.
Results
Literature retrieval and study characteristics
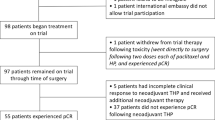
2844 articles were retrieved from four databases, of which 58 articles8,9,11,12,17,25,26,32,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90, including 28 trials, were eligible and were extracted for accessible data (Fig. 1; Table 1). 20 trials with 2809 patients with HR+/HER2 + BC were included in the primary pCR analysis comparing HER2-targeting regimens. Additionally, five trials with 877 patients were assessed for ET efficacy, six trials with 818 patients for carboplatin, and four trials with 482 patients for anthracycline.
The duration of neoadjuvant treatment ranged from 12 to 30 weeks, due to differences in cycle numbers and length. Among all HER2 + cases included, 63·0% (4347/6904) were HR+. All trials reported the number of patients with pCR in the HR + subgroup, while six of them provided EFS results for the HR + subgroup.
The risk of bias assessment identified one trial with a high overall risk of bias due to the missing randomization process. Most trials (21/28) had a low overall risk of bias, while six trials had some concerns about the risk of bias (Supplementary Fig. S1, Supplementary Table S6).
Pairwise meta-analysis
From trials that reported pCR in the HR+/HER2 + population, six direct comparisons were made: (1) T-DM1 vs. HP + C (2) HP + C vs. H + C (3) H + TKI + C vs. H + C (4) H + TKI + C vs. L + C (5) L + C vs. H + C (6) C vs. H + C. HP + C demonstrated a significantly higher pCR rate compared to H + C, with an OR (95% CI) of 1·77 (1·05–2·98). H + TKI + C achieved a higher pCR rate than both H + C and L + C with ORs (95% CI) of 1·61 (1·22–2·11) and 2·29 (1·63–3·21), respectively. Both L + C and C were associated with significantly lower pCR than H + C, with ORs of 0·64 (95% CI 0·48–0·85) and 0·39 (95% CI 0·23–0·66), respectively (Fig. 2). Sensitivity analyses with random effects models all resulted similarly (Supplementary Fig. S2, Supplementary Table S7).
When comparing T-DM1 vs. HP + C, a high I2 statistic was observed (I2 = 45%, p = 0·12) after the heterogeneity test. Sensitivity analysis showed that the lowest I2 statistic (I2 = 15%, Supplementary Fig. S3) was achieved when the TEAL trial was excluded, with no impact on the outcome of this comparison (OR 0·93, 95%CI 0·66–1·31). No evidence of publication bias was observed after Peter’s test, and all funnel plots were approximately symmetrical (Supplementary Fig. S4).
Forest plots of direct comparisons for pCR. (a) T-DM1 vs. HP + C; (b) HP + C vs. H + C; (c) H + TKI + C vs. H + C; (d) H + TKI + C vs. L + C; (e) L + C vs. H + C; (f) C vs. H + C. T-DM1 = trastuzumab emtansine based regimens; HP + C = trastuzumab and pertuzumab with chemotherapy; H + TKI + C = trastuzumab and TKI with chemotherapy; H + C = trastuzumab with chemotherapy; L + C = lapatinib with chemotherapy; C = chemotherapy with no HER2-targeting regimen. The squares and the lines crossing the square stand for OR and its 95%CI. The diamonds stand for the estimated pooled OR and its 95% CI. Heterogeneity was tested with Cochran’s Q test, and all statistical tests were two-sided.
Network meta-analysis
The network comparing pCR included 20 trials with 15 comparisons, and the network comparing EFS included five trials with ten comparisons (Fig. 3). ORs of pCR and HRs of EFS were listed in Table 2 with their 95% CI. We observed statistically significant differences in 11 comparisons for pCR and no statistically significant difference for EFS across different treatment arms.
The node-splitting model was used for the consistency test, and no significant inconsistency was found (Supplementary Fig. S5). The adjusted funnel plot was symmetrical, indicating no significant small-study effect (Supplementary Fig. S6). Sensitivity analysis was performed by excluding trials with a high risk of overall bias, using other TKIs instead of lapatinib, or reporting pCR in different definitions, and most results remained stable (Supplementary Table S8–S10).
Network plots for pathological complete response (pCR) and event free survival (EFS). (a) pCR, and (b) EFS. Each line represents a direct comparison, and its width is weighted by the number of trials reporting this comparison, which is presented next to it. T-DM1 = trastuzumab emtansine based regimens; HP + C = trastuzumab and pertuzumab with chemotherapy; H + TKI + C = trastuzumab and TKI with chemotherapy; H + C = trastuzumab with chemotherapy; L + C = lapatinib with chemotherapy; C = chemotherapy with no HER2-targeting regimen.
Two-dimensional ranking plot of SUCRA value for highest probability of pCR rate and lowest risk of EFS events. T-DM1 = trastuzumab emtansine based regimens; HP + C = trastuzumab and pertuzumab with chemotherapy; H + TKI + C = trastuzumab and TKI with chemotherapy; H + C = trastuzumab with chemotherapy; L + C = lapatinib with chemotherapy; C = chemotherapy with no HER2-targeting regimen.
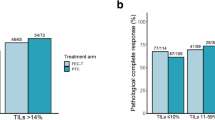
Ranking of regimens
SUCRA values were calculated and indicated that T-DM1 (SUCRA 0.86) had the highest probability of achieving pCR. HP + C (SUCRA 0.82) closely followed in second place, and H + TKI + C (SUCRA 0.71) ranked third. However, when considering EFS, HP + C (SUCRA 0.69) emerged as the top regimen, followed by H + TKI + C (SUCRA 0.63).
A clustered ranking plot was generated by combining the values of SUCRA from both pCR (on the y-axis) and EFS (on the x-axis) (Fig. 4). HP + C emerged as the optimal choice (top right) considering both short-term clinical response and long-term survival outcome. Detailed ranking probabilities are shown in Supplementary Fig. S7.
Chemotherapy and endocrine therapy analysis
Pairwise meta-analyses were performed to further analyze the efficacy of different chemotherapy and ET with the same HER2-targeting regimen. We conducted three direct meta-analyses comparing pCR rates separately between treatments with or without anthracycline (OR 0·74, 95% CI 0·51–1·07), carboplatin (OR 1·27, 95% CI 0·95–1·96), and ET (OR 0·69, 95% CI 0·52–0·92) (Supplementary Fig. S8 A–C). When comparing ET, significant heterogeneity was observed (I2 = 81%, p < 0·01). Therefore, we conducted a subgroup analysis, which indicated that the subgroup where chemotherapy was replaced with ET still presented heterogeneity (I2 = 65%, p = 0·09) (Supplementary Fig. S8 D). This heterogeneity could be attributed to variations in neoadjuvant treatment duration. For example, the ET group in the PHERGain trial received 24 weeks of neoadjuvant therapy, while the chemotherapy group in the PHERGain trial and both groups in the WSG-TP-II trial received 12 weeks. Thus, the random effects model was used to compare results with the common effect model (Supplementary Fig. S8 E). For trials incorporating ET alongside other treatments, higher pCR was observed with no statistical significance in the ET group (OR 1·18, 95% CI 0·80–1·73). However, for trials in which chemotherapy was replaced with ET, the pooled result showed a significantly lower pCR rate in ET in both common effect model (OR 0·34, 95% CI 0·22–0·53) and random effects model (OR 0·35, 95% CI 0·16–0·75).
Discussion
Our findings suggest that the HP + C regimen is the optimal neoadjuvant strategy for HR+/HER2 + BC when considering both pCR and EFS. The anthracycline-free regimen achieved a numerically higher pCR than the anthracycline-containing regimen, and the inclusion of carboplatin also increased the possibility of achieving pCR, although not reaching statistical significance. The efficacy of neoadjuvant ET remains inconclusive.
Both direct and indirect comparisons indicate that the T-DM1-based or dual HER2-targeting regimens are better than single HER2-targeting regimens in improving pCR rates. Though no significant differences were observed in pCR and EFS when comparing T-DM1, HP + C, and H + TKI + C regimens, HP + C had the highest probability of ranking first when considering both pCR and EFS. T-DM1 showed certain advantages in ranking when comparing pCR but ranked lower when comparing EFS. Although the result of the EFS analysis may not be robust enough due to insufficient data, we found that both the KRISTINE9 and I-SPY II8 trials reported higher risks of EFS events in the T-DM1 group, suggesting T-DM1 may not be the preferred choice for long-term survival benefits. Moreover, results from the KRISTINE9 and KAITLIN91 trials demonstrated that T-DM1 combined with pertuzumab did not outperform HP + C in either neoadjuvant or adjuvant settings. Thus, further studies are necessary to investigate short-term and long-term benefits of T-DM1 and other antibody-drug conjugates. Based on the existing evidence, the H + TKI + C regimen does not demonstrate significant advantages over the HP + C regimen. Considering that TKIs have a significantly higher incidence of grade 3 or higher adverse events (AEs) in the overall HER2 + population, and there is no evidence suggesting that the risk of AEs is associated with HR status, we could not recommend H + TKI + C over HP + C at present. We noticed that pyrotinib, a new TKI drug, achieved a relatively higher pCR rate12. New TKI drugs with improved clinical benefits and safety profiles may hold promise in the future. We conclude that HP + C remains the current optimal neoadjuvant strategy for HR+/HER2 + BC.
The optimal chemotherapy regimen to combine with targeted therapy is controversial. An EBCTCG meta-analysis in the overall BC population demonstrated that adding anthracycline to a taxane regimen yields better outcomes, and higher cumulative doses of anthracycline and taxane are associated with greater benefits92. A phase II trial presented at ASCO 2023 showed that albumin-bound paclitaxel combined with trastuzumab and pertuzumab, followed by anthracycline-based regimens, achieved a higher pCR in the HER2+/HR- BC subgroup (81·8%) compared to the HER2+/HR + subgroup (31·6%)93. The TRYPHAENA trial reported similar long-term outcomes between groups with or without anthracycline17, and the TRAIN-2 trial found that the neoadjuvant treatment of the HR + subgroup favored the non-anthracycline strategy numerically87. Our results support the omitting of anthracycline in the neoadjuvant chemotherapy for HR+/HER2 + BC, as we observed higher pCR in anthracycline-free regimens in all included trials, although not statistically significant in the pooled result. Furthermore, the addition of carboplatin to the neoadjuvant chemotherapy regimen appears to increase the likelihood of achieving pCR in this population. Further trials are needed to support this inference since the CI still includes 1.
ET is recommended for HER2+/HR + BC treatment. However, it remains unclear if ET should be initiated in the neoadjuvant period. Our analysis identified significant heterogeneity among trial results, likely due to varied strategies in incorporating ET, including adding ET to standard treatments or replacing chemotherapy with ET. The NSABP B52 trial reported an insignificant improvement in pCR rate for the group adding ET to the HP + C regimen94. Our subgroup analysis demonstrated no heterogeneity among the results of studies with ET added to standard treatments, all of which observed higher pCR in the ET group, although the pooled result showed no statistical significance. On the other hand, in trials where neoadjuvant chemotherapy was replaced with ET, relatively low pCR rates were reported. For example, the single-arm trials PAMELA and TBCRC006 reported pCR rates of 18% and 21%, respectively, when ET was combined with trastuzumab and lapatinib without chemotherapy95,96. Similar pCR were reported in the PerELISA and PHERGain trials when combining ET with trastuzumab and pertuzumab (21% and 35%, respectively)23,26. In our study, only two included trials replaced chemotherapy with ET, both reporting lower pCR in the ET group compared to the chemotherapy group.
For the sole goal of reducing tumor size in neoadjuvant therapy, replacing neoadjuvant chemotherapy with ET may not be optimal, given ET’s lack of a direct inhibitory effect on cancer cell growth. However, neoadjuvant treatment is not limited to local control but is focused on prognosis and guiding postoperative treatment. In this case, even if neoadjuvant ET may not significantly improve the pCR rate, long-term outcomes should be considered when evaluating its benefits. Notably, the three-year follow-up of PHERGain showed that the invasive disease-free survival rate was highest in patients who achieved pCR with ET and without chemotherapy97. This indicates that pCR might not be the optimal endpoint for evaluating responses to neoadjuvant ET, and future trials should explore alternative indicators such as preoperative endocrine prognostic index and endocrine sensitive disease rate for their clinical significance.
Patients with HER2+/HR + BC exhibit a lower likelihood of achieving pCR and face poorer prognoses than those with HER2+/HR- BC6,7. Our study provided a precise perspective and a focused and detailed analysis on the HR + subgroup of HER2 + BC, addressing an unmet need in this challenging population. Notably, this is the first study to compare EFS across different neoadjuvant regimens specifically for HR+/HER2 + BC, offering insights into both short-term (pCR) and long-term (EFS) outcomes. Furthermore, our work is pioneering in evaluating the role of ET in the neoadjuvant setting for this subgroup.
Some unavoidable limitations should be noted. First, the network of EFS analysis included only five trials, which may limit the robustness of the findings. Second, safety analysis was not conducted due to insufficient data in the HR+/HER2 + population. However, we anticipate a similar safety profile as the overall HER2 + population, which has been extensively studied. Notably, TKI agents are generally associated with more serious AEs than antibodies16,27,29. Third, this analysis did not account for variations in TNM staging, the duration of neoadjuvant treatment, or subsequent adjuvant therapy across the included trials. These differences could contribute to heterogeneity in patient cohorts, treatments, and endpoint evaluations.
In conclusion, despite the result being insignificant in EFS comparisons, the HP + C regimen emerged as the optimal neoadjuvant treatment for HR+/HER2 + BC when considering both pCR and EFS outcomes. Additionally, anthracycline-free carboplatin-containing chemotherapy may be a viable combination treatment, although the result did not reach statistical significance. Further studies on neoadjuvant ET are essential to explore appropriate endpoints for evaluating its efficacy and to provide deeper insights into its role in the treatment of HR+/HER2 + BC.
Data availability
All data included in this study will be shared upon request. Please contact the corresponding author at [email protected].
References
Cardoso, F. et al. Early breast cancer: ESMO Clinical Practice guidelines for diagnosis, treatment and follow-up†. Ann. Oncol. 30, 1194–1220 (2019).
Gradishar, W. J. et al. Breast cancer, version 3.2022, NCCN Clinical Practice guidelines in Oncology. J. Natl. Compr. Cancer Netw. JNCCN 20, 691–722 (2022).
Delgado, A. & Guddati, A. K. Clinical endpoints in oncology - a primer. Am. J. Cancer Res. 11, 1121–1131 (2021).
Giaquinto, A. N. et al. Breast cancer statistics, CA. Cancer J. Clin. 72, 524–541 (2022).
Pegram, M., Jackisch, C. & Johnston, S. R. D. Estrogen/HER2 receptor crosstalk in breast cancer: combination therapies to improve outcomes for patients with hormone receptor-positive/HER2-positive breast cancer. Npj Breast Cancer 9, 45 (2023).
Kay, C. et al. Current trends in the treatment of HR+/HER2 + breast cancer. Future Oncol. 17, 1665–1681 (2021).
Cortazar, P. et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet Lond. Engl. 384, 164–172 (2014).
Clark, A. S. et al. Neoadjuvant T-DM1/pertuzumab and paclitaxel/trastuzumab/pertuzumab for HER2 + breast cancer in the adaptively randomized I-SPY2 trial. Nat. Commun. 12 (2021).
Hurvitz, S. A. et al. Neoadjuvant trastuzumab, pertuzumab, and chemotherapy versus trastuzumab emtansine plus pertuzumab in patients with HER2-positive breast cancer (KRISTINE): a randomised, open-label, multicentre, phase 3 trial. Lancet Oncol. 19, 115–126 (2018).
NCT05704829. NeoAdjuvant Therapy With Trastuzumab-deruxtecan Versus Chemotherapy + Trastuzumab + Pertuzumab in HER2 + Early Breast Cancer. https://doi.org/10.1002/central/CN-02519466 (2023).
Jacobs, S. A. et al. NSABP FB-7: a phase II randomized neoadjuvant trial with paclitaxel + trastuzumab and/or neratinib followed by chemotherapy and postoperative trastuzumab in HER2(+) breast cancer. Breast Cancer Res. BCR 21, 133 (2019).
Wu, J. et al. Neoadjuvant pyrotinib, trastuzumab, and docetaxel for HER2-positive breast cancer (PHEDRA): a double-blind, randomized phase 3 trial. BMC Med. 20, 498 (2022).
Berry, D. A. et al. Estrogen-receptor status and outcomes of modern chemotherapy for patients with node-positive breast cancer. JAMA 295, 1658–1667 (2006).
Agostinetto, E., Gligorov, J. & Piccart, M. Systemic therapy for early-stage breast cancer: learning from the past to build the future. Nat. Rev. Clin. Oncol. 19, 763–774 (2022).
Slamon, D. et al. Adjuvant trastuzumab in HER2-positive breast cancer. N. Engl. J. Med. 365, 1273–1283 (2011).
Villacampa, G. et al. Landscape of neoadjuvant therapy in HER2-positive breast cancer: a systematic review and network meta-analysis. Eur. J. Cancer 190, (2023).
Schneeweiss, A. et al. Long-term efficacy analysis of the randomised, phase II TRYPHAENA cardiac safety study: evaluating pertuzumab and trastuzumab plus standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer. Eur. J. Cancer 89, 27–35 (2018).
Korde, L. A. et al. Neoadjuvant chemotherapy, endocrine therapy, and targeted therapy for breast cancer: ASCO guideline. J. Clin. Oncol. 39, 1485–1505 (2021).
Thanopoulou, E. et al. Therapeutic strategies for the management of hormone receptor-positive, human epidermal growth factor receptor 2-positive (HR+/HER2+) breast cancer: a review of the current literature. Cancers 12, 3317 (2020).
Kaufman, B. et al. Trastuzumab plus anastrozole versus anastrozole alone for the treatment of postmenopausal women with human epidermal growth factor receptor 2-positive, hormone receptor-positive metastatic breast cancer: results from the randomized phase III TAnDEM study. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 27, 5529–5537 (2009).
Johnston, S. R. D. et al. Phase III, randomized study of dual human epidermal growth factor receptor 2 (HER2) blockade with lapatinib plus trastuzumab in combination with an aromatase inhibitor in postmenopausal women with HER2-positive, hormone receptor-positive metastatic breast cancer: updated results of ALTERNATIVE. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 39, 79–89 (2021).
Arpino, G. et al. Pertuzumab, trastuzumab, and an aromatase inhibitor for HER2-positive and hormone receptor-positive metastatic or locally advanced breast cancer: PERTAIN final analysis. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 29, 1468–1476 (2023).
V, G. et al. De-escalated therapy for HR+/HER2 + breast cancer patients with Ki67 response after 2-week letrozole: results of the PerELISA neoadjuvant study. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 30 (2019).
Gianni, L. et al. Neoadjuvant treatment with trastuzumab and pertuzumab plus palbociclib and fulvestrant in HER2-positive, ER-positive breast cancer (NA-PHER2): an exploratory, open-label, phase 2 study. Lancet Oncol. 19, 249–256 (2018).
Harbeck, N. et al. De-escalated neoadjuvant trastuzumab-emtansine with or without endocrine therapy versus trastuzumab with endocrine therapy in HR+/HER2 + early breast cancer: 5-year survival in the WSG-ADAPT-TP trial. J. Clin. Oncol. https://doi.org/10.1200/JCO.22.01816 (2023).
Pérez-García, J. M. et al. Chemotherapy de-escalation using an (18)F-FDG-PET-based pathological response-adapted strategy in patients with HER2-positive early breast cancer (PHERGain): a multicentre, randomised, open-label, non-comparative, phase 2 trial. Lancet Oncol. 22, 858–871 (2021).
Nakashoji, A. et al. The updated network meta-analysis of neoadjuvant therapy for HER2-positive breast cancer. Cancer Treat. Rev. 62, 9–17 (2018).
Cai, Y. W., Shao, Z. M. & Yu, K. D. Determining the optimal (neo)adjuvant regimen for human epidermal growth factor receptor 2-positive breast cancer regarding survival outcome: a network meta-analysis. Front. Immunol. 13, 919369 (2022).
Gunasekara, A. D. M. et al. Neoadjuvant treatment with HER2-targeted therapies in HER2-positive breast cancer: a systematic review and network meta-analysis. Cancers 14 (2022).
Zhang, J. et al. Efficacy and safety of neoadjuvant therapy for HER2-positive early breast cancer: a network meta-analysis. Ther. Adv. Med. Oncol. 13, 17588359211006948 (2021).
Chen, D., Jin, L., Xu, Y., Bhandari, A. & Wang, O. ErbB inhibitors as neoadjuvant therapy for triple-positive breast cancer: a network meta-analysis. Am. J. Transl. Res. 13, 12129–12140 (2021).
Gluz, O. et al. Efficacy of endocrine therapy plus trastuzumab and pertuzumab vs de-escalated chemotherapy in patients with hormone receptor–Positive/ERBB2-positive early breast cancer: the neoadjuvant WSG-TP-II randomized clinical trial. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2023.0646 (2023).
Hutton, B. et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 162, 777–784 (2015).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339 (2009).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71 (2021).
Sterne, J. A. C. et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366, l4898 (2019).
Peters, J. L., Sutton, A. J., Jones, D. R., Abrams, K. R. & Rushton, L. Comparison of two methods to detect publication bias in meta-analysis. JAMA 295, 676–680 (2006).
van Valkenhoef, G., Dias, S., Ades, A. E. & Welton, N. J. Automated generation of node-splitting models for assessment of inconsistency in network meta-analysis. Res. Synth. Methods 7, 80–93 (2016).
Chaimani, A. & Salanti, G. Using network meta-analysis to evaluate the existence of small-study effects in a network of interventions. Res. Synth. Methods 3, 161–176 (2012).
Chaimani, A. & Salanti, G. Visualizing assumptions and results in network meta-analysis: the network graphs package. Stata J. 15, 905–950 (2015).
Gianni, L. et al. 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): a multicentre, open-label, phase 2 randomised trial. Lancet Oncol. 17, 791–800 (2016).
Masuda, N. et al. A randomized, 3-arm, neoadjuvant, phase 2 study comparing docetaxel + carboplatin + trastuzumab + pertuzumab (TCbHP), TCbHP followed by trastuzumab emtansine and pertuzumab (T-DM1 + P), and T-DM1 + P in HER2-positive primary breast cancer. Breast Cancer Res. Treat. 180, 135–146 (2020).
Patel, T. A. et al. A randomized, controlled phase II trial of neoadjuvant ado-trastuzumab emtansine, lapatinib, and nab-paclitaxel versus trastuzumab, pertuzumab, and paclitaxel in HER2-positive breast cancer (TEAL study). Breast Cancer Res. 21, 100 (2019).
Firouzabadi, D., Dehghanian, A., Rezvani, A., Mahmoudi, L. & Talei, A. Addition of carboplatin-gemcitabine as second-line neoadjuvant chemotherapy in non-responsive locally advanced breast cancer patients to standard neoadjuvant chemotherapy and evaluation of factors affecting response: a randomized controlled trial. BMC Cancer. 21, 47 (2021).
Gao, H. F. et al. Anthracycline-containing versus carboplatin-containing neoadjuvant chemotherapy in combination with trastuzumab for HER2-positive breast cancer: the neoCARH phase II randomized clinical trial. Ther. Adv. Med. Oncol. 13, 17588359211009003 (2021).
Nuciforo, P. G. et al. Benefit to neoadjuvant anti-human epidermal growth factor receptor 2 (HER2)-targeted therapies in HER2-positive primary breast cancer is independent of phosphatase and tensin homolog deleted from chromosome 10 (PTEN) status. Ann. Oncol. 26, 1494–1500 (2015).
Azim, H. A. J. et al. Circulating tumor cells and response to neoadjuvant paclitaxel and HER2-targeted therapy: a sub-study from the NeoALTTO phase III trial. Breast 22, 1060–1065 (2013).
Rothé, F. et al. Circulating Tumor DNA in HER2-amplified breast cancer: a translational research substudy of the NeoALTTO phase III trial. Clin. Cancer Res. 25, 3581–3588 (2019).
Banys-Paluchowski, M. et al. Clinical relevance of collagen protein degradation markers C3M and C4M in the serum of breast cancer patients treated with neoadjuvant therapy in the GeparQuinto trial. Cancers 11 (2019).
Harbeck, N. et al. De-escalation strategies in human epidermal growth factor receptor 2 (HER2)–positive early breast cancer (BC): final analysis of the west German study group adjuvant dynamic marker-adjusted personalized therapy trial optimizing risk assessment and therapy response prediction in early BC HER2- and hormone receptor–positive phase II randomized Trial—Efficacy, Safety, and predictive markers for 12 weeks of Neoadjuvant Trastuzumab Emtansine with or without endocrine therapy (ET) Versus Trastuzumab Plus ET. J. Clin. Oncol. https://doi.org/10.1200/JCO.2016.71.9815 (2017).
Di Cosimo, S. et al. Effect of body mass index on response to neo-adjuvant therapy in HER2-positive breast cancer: an exploratory analysis of the NeoALTTO trial. Breast Cancer Res. 22, 115 (2020).
Gianni, L. et al. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol. 13, 25–32 (2012).
Masuda, N. et al. Efficacy and safety of trastuzumab, lapatinib, and paclitaxel neoadjuvant treatment with or without prolonged exposure to anti-HER2 therapy, and with or without hormone therapy for HER2-positive primary breast cancer: a randomised, five-arm, multicentre, open-label phase II trial. Breast Cancer Tokyo Jpn. 25, 407–415 (2018).
Shao, Z. et al. Efficacy, Safety, and tolerability of Pertuzumab, Trastuzumab, and Docetaxel for patients with early or locally Advanced ERBB2-Positive breast Cancer in Asia: the PEONY phase 3 Randomized Clinical Trial. JAMA Oncol. 6, e193692 (2020).
Schneeweiss, A. et al. Evaluating the predictive value of biomarkers for efficacy outcomes in response to pertuzumab- and trastuzumab-based therapy: an exploratory analysis of the TRYPHAENA study. Breast Cancer Res. 16, R73 (2014).
Harbeck, N. et al. Immune markers and tumor-related processes predict neoadjuvant therapy response in the WSG-ADAPT HER2-positive/hormone receptor-positive trial in early breast cancer. Cancers 13 (2021).
Dieci, M. V. et al. Integrated evaluation of PAM50 subtypes and immune modulation of pCR in HER2-positive breast cancer patients treated with chemotherapy and HER2-targeted agents in the CherLOB trial. Ann. Oncol. 27, 1867–1873 (2016).
Pizzamiglio, S. et al. Integrated molecular and immune phenotype of HER2-positive breast cancer and response to neoadjuvant therapy: a NeoALTTO exploratory analysis. Clin. Cancer Res. 27, 6307–6313 (2021).
von Minckwitz, G. et al. Integrating bevacizumab, everolimus, and lapatinib into current neoadjuvant chemotherapy regimen for primary breast cancer. Safety results of the GeparQuinto trial. Ann. Oncol. 22, 301–306 (2011).
Robidoux, A. et al. Lapatinib as a component of neoadjuvant therapy for HER2-positive operable breast cancer (NSABP protocol B-41): an open-label, randomised phase 3 trial. Lancet Oncol. 14, 1183–1192 (2013).
Untch, M. et al. Lapatinib versus trastuzumab in combination with neoadjuvant anthracycline-taxane-based chemotherapy (GeparQuinto, GBG 44): a randomised phase 3 trial. Lancet Oncol. 13, 135–144 (2012).
Baselga, J. et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet 379, 633–640 (2012).
de Azambuja, E. et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): survival outcomes of a randomised, open-label, multicentre, phase 3 trial and their association with pathological complete response. Lancet Oncol. 15, 1137–1146 (2014).
Giacchetti, S. et al. Long-term outcome of the REMAGUS 02 trial, a multicenter randomised phase II trial in locally advanced breast cancer patients treated with neoadjuvant chemotherapy with or without celecoxib or trastuzumab according to HER2 status. Eur. J. Cancer. 75, 323–332 (2017).
Tokunaga, E. et al. Long-term outcomes of a randomized study of neoadjuvant induction Dual HER2 blockade with trastuzumab and lapatinib followed by weekly paclitaxel plus dual HER2 blockade for HER2-positive primary breast cancer (Neo-lath study). Cancers 13 (2021).
Carey, L. A. et al. Molecular heterogeneity and response to neoadjuvant human epidermal growth factor receptor 2 targeting in CALGB 40601, a randomized phase III trial of paclitaxel plus trastuzumab with or without lapatinib. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 34, 542–549 (2016).
van Ramshorst, M. S. et al. Neoadjuvant chemotherapy with or without anthracyclines in the presence of dual HER2 blockade for HER2-positive breast cancer (TRAIN-2): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 19, 1630–1640 (2018).
Sun, X. et al. Neoadjuvant therapy and sentinel lymph node biopsy in HER2-positive breast cancer patients: results from the PEONY trial. Breast Cancer Res. Treat. 180, 423–428 (2020).
Buzdar, A. U. et al. Neoadjuvant therapy with paclitaxel followed by 5-fluorouracil, epirubicin, and cyclophosphamide chemotherapy and concurrent trastuzumab in human epidermal growth factor receptor 2-positive operable breast cancer: an update of the initial randomized study population and data of additional patients treated with the same regimen. Clin. Cancer Res. 13, 228–233 (2007).
Hurvitz, S. A. et al. Neoadjuvant trastuzumab emtansine and pertuzumab in human epidermal growth factor receptor 2-positive breast cancer: three-year outcomes from the phase III KRISTINE Study. J. Clin. Oncol. 37, 2206–2216 (2019).
Hatschek, T. et al. Neoadjuvant trastuzumab, pertuzumab, and docetaxel vs trastuzumab emtansine in patients with ERBB2-positive breast cancer: a phase 2 randomized clinical trial. JAMA Oncol. 7, 1360–1367 (2021).
Bonnefoi, H. et al. Neoadjuvant treatment with docetaxel plus lapatinib, trastuzumab, or both followed by an anthracycline-based chemotherapy in HER2-positive breast cancer: results of the randomised phase II EORTC 10054 study. Ann. Oncol. 26, 325–332 (2015).
Hurvitz, S. A. et al. Pathologic and molecular responses to neoadjuvant trastuzumab and/or lapatinib from a phase II randomized trial in HER2-positive breast cancer (TRIO-US B07). Nat. Commun. 11, 5824 (2020).
Holmes, F. A. et al. Pathologic complete response after preoperative anti-HER2 therapy correlates with alterations in PTEN, FOXO, phosphorylated Stat5, and autophagy protein signaling. BMC Res. Notes 6, 507 (2013).
Swain, S. M. et al. Pathologic complete response and outcomes by intrinsic subtypes in NSABP B-41, a randomized neoadjuvant trial of chemotherapy with trastuzumab, lapatinib, or the combination. Breast Cancer Res. Treat. 178, 389–399 (2019).
Schneeweiss, A. et al. Pertuzumab plus Trastuzumab in combination with standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer: a randomized phase II cardiac safety study (TRYPHAENA). Ann. Oncol. 24, 2278–2284 (2013).
Di Cosimo, S. et al. Plasma miRNA levels for predicting therapeutic response to neoadjuvant treatment in HER2-positive breast cancer: results from the NeoALTTO trial. Clin. Cancer Res. 25, 3887–3895 (2019).
Lambertini, M. et al. Pregnancies during and after trastuzumab and/or lapatinib in patients with human epidermal growth factor receptor 2-positive early breast cancer: analysis from the NeoALTTO (BIG 1–06) and ALTTO (BIG 2–06) trials. Cancer 125, 307–316 (2019).
Guarneri, V. et al. Preoperative chemotherapy plus trastuzumab, lapatinib, or both in human epidermal growth factor receptor 2-positive operable breast cancer: results of the randomized phase II CHER-LOB study. J. Clin. Oncol. 30, 1989–1995 (2012).
Guarneri, V. et al. Prospective biomarker analysis of the randomized CHER-LOB study evaluating the dual Anti-HER2 treatment with trastuzumab and lapatinib plus chemotherapy as neoadjuvant therapy for HER2-positive breast cancer. Oncologist 20, 1001–1010 (2015).
Fumagalli, D. et al. RNA sequencing to predict response to Neoadjuvant Anti-HER2 therapy: a secondary analysis of the NeoALTTO randomized clinical trial. JAMA Oncol. 3, 227–234 (2017).
Buzdar, A. U. et al. Significantly higher pathologic complete remission rate after neoadjuvant therapy with trastuzumab, paclitaxel, and epirubicin chemotherapy: results of a randomized trial in human epidermal growth factor receptor 2-positive operable breast cancer. J. Clin. Oncol. 23, 3676–3685 (2005).
Untch, M. et al. Survival analysis after Neoadjuvant Chemotherapy with Trastuzumab or Lapatinib in patients with human epidermal growth factor receptor 2-Positive breast Cancer in the GeparQuinto (G5) study (GBG 44). J. Clin. Oncol. 36, 1308–1316 (2018).
Huober, J. et al. Survival outcomes of the NeoALTTO study (BIG 1–06): updated results of a randomised multicenter phase III neoadjuvant clinical trial in patients with HER2-positive primary breast cancer. Eur. J. Cancer. 118, 169–177 (2019).
Matikas, A. et al. Survival outcomes, digital TILs, and on-treatment PET/CT during neoadjuvant therapy for HER2-positive breast cancer: results from the randomized PREDIX HER2 trial. Clin. Cancer Res. 29, 532–540 (2023).
Triulzi, T. et al. The TRAR gene classifier to predict response to neoadjuvant therapy in HER2-positive and ER-positive breast cancer patients: an explorative analysis from the NeoSphere trial. Mol. Oncol. 16, 2355–2366 (2022).
van der Voort, A. et al. Three-year follow-up of neoadjuvant chemotherapy with or without anthracyclines in the presence of dual ERBB2 blockade in patients with ERBB2-positive breast cancer: a secondary analysis of the TRAIN-2 Randomized, Phase 3 Trial. JAMA Oncol. 7, 978–984 (2021).
Guarneri, V. et al. Trastuzumab-Lapatinib as neoadjuvant therapy for HER2-positive early breast cancer: survival analyses of the CHER-Lob trial. Eur. J. Cancer Oxf. Engl. 1990. 153, 133–141 (2021).
Salgado, R. et al. Tumor-infiltrating lymphocytes and associations with pathological complete response and event-free survival in HER2-positive early-stage breast cancer treated with lapatinib and trastuzumab: a secondary analysis of the NeoALTTO trial. JAMA Oncol. 1, 448–454 (2015).
Wang, R. X., Chen, S., Jin, X., Chen, C. M. & Shao, Z. M. Weekly paclitaxel plus carboplatin with or without trastuzumab as neoadjuvant chemotherapy for HER2-positive breast cancer: loss of HER2 amplification and its impact on response and prognosis. Breast Cancer Res. Treat. 161, 259–267 (2017).
Krop, I. E. et al. Trastuzumab emtansine plus pertuzumab versus taxane plus trastuzumab plus pertuzumab after anthracycline for high-risk human epidermal growth factor receptor 2–positive early breast cancer: the Phase III KAITLIN Study. J. Clin. Oncol. 40, 438–448 (2022).
Braybrooke, J. et al. Anthracycline-containing and taxane-containing chemotherapy for early-stage operable breast cancer: a patient-level meta-analysis of 100 000 women from 86 randomised trials. Lancet 401, 1277–1292 (2023).
Iwamoto, M. et al. Phase II neoadjuvant trial of albumin-bound paclitaxel, trastuzumab and pertuzumab followed by anthracycline based regimens in patients with operable HER2 positive breast cancer (OMC-BC05). J. Clin. Oncol. 41, e12594–e12594 (2023).
Rimawi, M. et al. Abstract S3-06: a phase III trial evaluating pCR in patients with HR+, HER2-positive breast cancer treated with neoadjuvant docetaxel, carboplatin, trastuzumab, and pertuzumab (TCHP) +/- estrogen deprivation: NRG Oncology/NSABP B-52. Cancer Res. 77, 3–06 (2017).
Llombart-Cussac, A. et al. HER2-enriched subtype as a predictor of pathological complete response following trastuzumab and lapatinib without chemotherapy in early-stage HER2-positive breast cancer (PAMELA): an open-label, single-group, multicentre, phase 2 trial. Lancet Oncol. 18, 545–554 (2017).
Rimawi, M. F. et al. Multicenter phase II study of neoadjuvant lapatinib and trastuzumab with hormonal therapy and without chemotherapy in patients with human epidermal growth factor receptor 2-overexpressing breast cancer: TBCRC 006. J. Clin. Oncol. Off J. Am. Soc. Clin. Oncol. 31, 1726–1731 (2013).
Cortes, J. et al. 3-year invasive disease-free survival (iDFS) of the strategy-based, randomized phase II PHERGain trial evaluating chemotherapy (CT) de-escalation in human epidermal growth factor receptor 2-positive (HER2[+]) early breast cancer (EBC). J. Clin. Oncol. 41, LBA506–LBA506 (2023).
Acknowledgements
This study was sponsored by Shanghai Roche Pharmaceuticals Ltd. We acknowledge the medical writing support provided by Heqi Chen, MSc, employee of CW DATA Technologies (Chengdu) Co., Ltd., funded by Shanghai Roche Pharmaceuticals Ltd.
Funding
This work was supported by Natural Science Foundation of Sichuan Province (No. 2024NSFSC0741), Sichuan Science and Technology Program (No. 2023YFS0103), Special Research Fund for Clinical Studies of Innovative Drugs after Market Launch (No. WKZX2024CX501212), Wu Jieping Medical Foundation (No. 320.6750.2021-10-98), Chen Xiao-Ping Foundation For The Development Of Science And Technology Of Hubei Province (No. CXPJJH122001-2223). This study was sponsored by Shanghai Roche Pharmaceuticals Ltd.
Author information
Authors and Affiliations
Contributions
L.S.W., Y.M., M.K., and W.H. formulated the overarching research goals and aims. L.S.W., T.H., F.Y.J., Y.X., and W.H. designed and discussed the overall study protocol. M.W.H., L.S.H., X.L., and L.H. completed the literature retrieval and screening under the guidance of L.S.W. M.W.H., L.S.H., X.L., and L.H. extracted the original data from included trials, and all disagreements were settled with L.S.W. and W.H. L.S.W., Y.M., and M.E.X. compiled and verified the statistical programs. L.S.W., Y.M., Y.X., M.K., and W.H. drafted the original manuscript, and all authors were involved in the review and modification of the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
Hao Tang, Yajing Feng and Xin Yu are current employees of Shanghai Roche Pharmaceuticals Ltd. The remaining authors have declared no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, S., Yu, M., Mou, E. et al. The optimal neoadjuvant treatment strategy for HR+/HER2 + breast cancer: a network meta-analysis. Sci Rep 15, 713 (2025). https://doi.org/10.1038/s41598-024-84039-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-84039-2
Keywords
This article is cited by
-
Postoperative radiotherapy improves long-term survival in HER2-positive metastatic breast cancer: real-world evidence from the latest SEER database
Breast Cancer Research and Treatment (2025)