Abstract
The latest World Health Organization Classification of Tumors, Fifth Edition, recognizes the invasive encapsulated follicular variant of papillary thyroid carcinoma (IEFVPTC) as a distinct malignant entity rather than a subtype of papillary thyroid carcinoma (PTC). This reclassification highlights the need to explore potential prognostic differences between IEFVPTC and classic PTC. This study utilized the Surveillance, Epidemiology, and End Results (SEER) database to compare prognoses of patients diagnosed with IEFVPTC and classic PTC between 2004 and 2019. Propensity score matching (PSM) was employed to adjust for confounding variables and reduce selection bias. Kaplan-Meier survival curves and Cox regression models were used to evaluate overall survival (OS) between the two groups. A total of 1,530 IEFVPTC and 81,508 classic PTC patients were analyzed. Before PSM, significant differences were noted in race, T-stage, N-stage, M-stage, laterality, radiotherapy, surgical modality, tumor size, and income. Post-PSM, these differences were not statistically significant (p > 0.05). Kaplan-Meier curves and Cox regression models showed no significant differences in OS between IEFVPTC and classic PTC both before and after PSM. This PSM analysis revealed no significant differences in overall survival between patients with IEFVPTC and classic PTC, suggesting that the reclassification of IEFVPTC does not translate into distinct prognostic outcomes.
Similar content being viewed by others
Introduction
Invasive encapsulated follicular variant of papillary thyroid carcinoma (IEFVPTC) is a malignant well-differentiated tumor type of follicular cell origin. It has a distinctive envelope structure with unique or nearly unique follicular structure and shows typical nuclear features and the invasive growth pattern of papillary thyroid carcinoma (PTC)1. According to the latest World Health Organization (WHO) Classification of Tumors, Fifth Edition, IEFVPTC is no longer classified as a subtype of PTC. This is because the RAS mutations and transcriptomic profile of IEFVPTC are similar to those of follicular adenomas and follicular thyroid carcinomas, and do not correspond to the BRAFV600Eemolecular profiles of typical PTC or the aggressive follicular form of PTC2,3,4,5. IEFVPTC typically presents as a fibrocystic tumor or has well-defined borders and lacks the histologic features of aggressive follicular PTC6. Similar to follicular thyroid cancer, IEFVPTC is capable of invading nearby blood vessels and producing distant metastases7.
IEFVPTC occurs predominantly in adults, with a median age at diagnosis of 40–50 years, and a female-to-male ratio of more than 3:18,9,10. In children, approximately 15% of PTC cases belong to the IEFVPTC subtype11,12,13. The majority of patients present with a painless mass, and approximately 5% have distant metastases at the time of diagnosis14. The ultrasonographic features of IEFVPTC overlap with those of noninvasive follicular thyroid tumors with nuclear features, which typically appear as isolated lesions with round-to-oval shape, smooth margins, variable echogenicity, and absence of calcification15,16. In addition, the prevalence of IEFVPTC varies between different populations17,18.
Despite the genotypic differences between IEFVPTC and typical PTC, it remains unclear whether the pair has a significant difference in prognosis. Therefore, based on the Surveillance, Epidemiology, and End Results (SEER) database samples and related variables, the aim of this study was to evaluate the prognostic differences between IEFVPTC and classic PTC. The objective was to provide data to support the treatment and management of patients with IEFVPTC. In this study, propensity score matching (PSM) was used to reduce selection bias.
Materials and methods
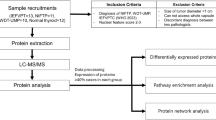
Samples and variables recode
The 2019 edition of the SEER database records information on patients with cancer from 17 states in the USA, encompassing approximately 28% of the population. The database collects detailed demographic data: age, sex, race, income, and marital status at diagnosis; tumor characteristics, such as tumor size, TNM stage, and laterality; treatments, including surgery and radiotherapy for the primary site; and first treatment and follow-up. The data used in this study were publicly available, covering treatment and income information between 2000 and 2019, and were downloaded via SEER*Stat software version 8.4.3 (https://seer.cancer.gov/seerstat/) in 2022.
The samples included in this study fulfilled the following criteria: (1) time of diagnosis between January 2004 and December 2019; (2) according to the WHO International Classification of Diseases (ICD-O-3) coding, the histologic type codes 8260 and 8343 were defined as classic PTC and IEFVPTC, respectively; and (3) the mode of diagnosis was confirmed by histopathology. Exclusion criteria included: (1) imprecise tumor size or tumors measuring < 1 mm; (2) missing TNM staging data or labeled as unknown; (3) unknown race; (4) unknown or 0 months of survival; and (5) no surgery or unknown surgical approach. Race variables were categorized as White, Black, and other. Primary site surgical procedure was categorized as total thyroidectomy and other. Annual household income less than US$75,000 was categorized as low income, while other was categorized as high income; this variable was adjusted for 2019 criteria. Laterality was categorized as left-sided (origin of primary), right-sided (origin of primary), and other. Marital status was categorized as married and other. Two variables, age at diagnosis and tumor size, were categorized. Overall survival (OS) was the primary outcome metric of interest in this study. The SEER database did not require ethical approval from the authors’ organizations because it provides free data download services for researchers and ensures confidentiality of the personal information of patients.
Statistical analysis
In this study, categorical data were organized in the form of frequencies and percentages, and differences between the two groups were analyzed by the χ2 test. Observed differences in baseline covariates between the two groups were adjusted for selection bias using the PSM method19. The PSM model included all covariates except the histologic subtype of interest and was constructed using the “nearest” method with a ratio of 3, a caliper of 0.00001, and “glm” as the distance metric. Baseline patient characteristics before and after matching were assessed using standard mean difference (SMD), and an SMD > 0.1 denoted imbalance between the two groups20. The effect of patient characteristics on OS was analyzed univariately by the Kaplan–Meier method, and statistical significance was assessed using the log-rank test. Univariate and multivariate stepwise Cox regression models were used to assess prognostic factors affecting OS in the study sample. All statistical analyses and visualizations for this study were conducted using the R language (version 4.3.2, https://www.r-project.org/) and RStudio (https://posit.co/) environments. All statistical tests were two-sided, and p-values < 0.05 denoted statistical significance.
Results
Demographic characteristics
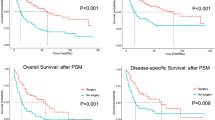
Between 2004 and 2019, 1,530 and 81,508 patients with IEFVPTC and classic PTC, respectively, in the SEER database were identified as eligible for inclusion in the present study. In both groups, there was a higher percentage of women and patients aged < 46 years; however, there was no statistically significant difference in frequency distribution. In terms of racial distribution, the IEFVPTC group included more black patients, while the classic PTC group included more patients of other races; these differences were statistically significant. The numbers of patients with T1 stage, N1 stage, and M1 stage disease were higher in the classic PTC group versus the IEFVPTC group, and there was a statistically significant difference in the distribution of these indicators between the two groups. In addition, the proportion of unilateral (left or right) distribution was lower in the classic PTC groups versus the IEFVPTC group, and the difference was statistically significant. The proportion of patients who underwent radiotherapy and total thyroidectomy was higher in the classic PTC group compared with the IEFVPTC group. The percentage of patients with tumor size measuring > 22 mm was higher in the IEFVPTC group than the classic PTC group. In the original cohort, there were differences in the frequency distributions of race, T-stage, N-stage, M-stage, laterality, radiotherapy, surgical approach, tumor size, and income between the two groups. However, after PSM correction, these confounding factors no longer showed statistically significant differences between the groups (Table 1). SMD distribution plots indicated that, prior to PSM, the baseline data between the two groups were unevenly distributed. After PSM weighting, the SMDs approached the 0-value line (< 0.1), indicating a balanced profile between the groups (Fig. 1).
Survival analysis
Kaplan–Meier curves showed that, in the original cohort, OS was lower in patients with classic PTC than in those with IEFVPTC. However, the log-rank test did not reveal a statistically significant difference in OS (p = 0.17). Consistent with these results, there was no statistically significant difference in OS between the two groups after PSM (p > 0.05) (Fig. 2). In the one-way Cox regression analysis of the original cohort, there was also no difference in OS between the classic PTC and IEFVPTC groups (hazard ratio: 1.18, 95% confidence interval: 0.93–1.51). The histologic type was not identified as a prognostic factor for OS in the multivariate stepwise Cox model. The results of the PSM-weighted cohort were consistent with those obtained from the original cohort. Moreover, the findings of the univariate or multivariate Cox models confirmed that histologic type was not a prognostic factor in this setting (Supplemental Table 1).
Subgroup analysis
The results of the subgroup forest plot analysis did not indicate statistically significant differences at all levels of all variables between IEFVPTC and classic PTC (p > 0.05). These findings suggested that these two types of cancer have similar clinical prognoses (Fig. 3).
Discussion
In this study, we compared the prognosis of classic PTC and IEFVPTC using data from the SEER database, which provides extensive coverage and long-term follow-up, making it a valuable resource for studying thyroid cancers with relatively good prognosis. To our knowledge, this study is the first to use PSM to compare the prognostic differences between these two thyroid cancer subtypes following the latest WHO tumor classification.
In recent years, the criteria for the diagnosis and classification of follicular PTC have been revised on several occasions. In the early literature and in the WHO classification system, non-IEFVPTC has been reclassified as noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP)21. In the Fifth Edition of the WHO classification, follicular variant PTC is subdivided into “encapsulated with invasion” and “infiltrative” subtypes. Although the infiltrative type resembles conventional PTC in growth pattern, it predominantly exhibits a follicular structure22. Due to differing genotypes, IEFVPTC is now considered a separate malignant tumor, distinct from PTC23. The molecular profile of IEFVPTC differs from that of classic PTC and is shared with follicular adenomas or minimally invasive follicular thyroid cancer24. It can also metastasize in a similar manner to encapsulated follicular carcinoma25. This highlights that the defining features of PTC are its molecular characteristics, not the typical nuclear changes26. Nevertheless, IEFVPTC, classic PTC, and their subtypes are inextricably linked. The large follicular structure of IEFVPTC and its overlap with benign diseases limit cytologic classification effectiveness in distinguishing NIFTP from IEFVPTC. Although new molecular assays may aid in differentiation, identifying IEFVPTC remains a major challenge10,27,28. Biomarkers like programmed death-ligand 1 may be helpful in identifying IEFVPTC and NIFTP29. Several studies have examined prognostic factors of PTC, but they did not consider histologic factors30,31. The studies by Holoube and colleagues found that subtypes with higher aggressiveness (high-cell and diffuse sclerosing) did not have a significant survival advantage over thyroid micropapillary carcinomas, even with more aggressive treatment32,33. In contrast, Hurthle cell microscopic carcinomas had lower survival rates than follicular and papillary microscopic thyroid carcinomas34. In general, IEFVPTC has been associated with a better prognosis than invasive PTC35. Like follicular thyroid cancer, IEFVPTC spreads to distant sites, often bypassing the lymph nodes6,25. However, in the absence of distant metastases at the time of diagnosis, IEFVPTC is usually indolent14,36.
In this study, we found no significant difference in long-term prognosis between classic PTC and IEFVPTC, and this result was consistent across all factors. However, some studies have reported that IEFVPTC may have a higher recurrence rate compared to other PTC subtypes23. In clinical practice, distinguishing between follicular variant PTC subtypes at the histological level may not have a major impact on treatment decisions. Nonetheless, distinguishing IEFVPTC from classic PTC requires pathologists to carefully examine the tumor capsule and accurately assess the extent of tumor invasion in their histological reports. While patients with IEFVPTC may be at a higher risk of distant metastasis22, our study found no significant differences in overall survival between IEFVPTC and classic PTC patients. Although no survival differences were found, it is important to note that the management of IEFVPTC should follow the same approach as follicular thyroid carcinoma due to their shared genotype.
While we employed the PSM method to adjust for baseline variables and obtained relatively stable results, several limitations should be acknowledged. Firstly, as a retrospective study, there is potential bias in the selection of variables and collection of samples. Secondly, the SEER database lacks data on certain critical variables for patients with PTC, such as recurrence rates. Finally, this study did not thoroughly investigate differences between IEFVPTC and other PTC subtypes, limiting the comprehensiveness of our findings. Therefore, larger multicenter prospective studies are needed to improve the management of IEFVPTC and all PTC subtypes.
Conclusion
This population-based study provides strong evidence that there is no significant difference in overall survival between patients with classic PTC and IEFVPTC, even after adjusting for confounding variables using PSM and in subgroup analyses. These findings suggest comparable prognoses for both histologic types, highlighting the need for more effective treatment strategies to improve the management of PTC and IEFVPTC patients.
Data availability
The data used in this study can be downloaded from the SEER database or obtained from the corresponding author.
References
WHO Classification of Tumours Editorial Board. Endocrine and Neuroendocrine Tumours. (International Agency for Research on Cancer (IARC)).
Kim, T. H. et al. Molecular genotyping of the non-invasive encapsulated follicular variant of papillary thyroid carcinoma. Histopathology 72, 648–661 (2018).
Lee, S. R. et al. Molecular genotyping of follicular variant of papillary thyroid carcinoma correlates with diagnostic category of fine-needle aspiration cytology: values of RAS mutation testing. Thyroid 23, 1416–1422 (2013).
Jung, C. K. et al. Clinical utility of EZH1 mutations in the diagnosis of follicular-patterned thyroid tumors. Hum. Pathol. 81, 9–17 (2018).
Jung, C. K. et al. Molecular correlates and nuclear features of encapsulated follicular-patterned thyroid neoplasms. Endocrinol. Metab. 36, 123–133 (2021).
Jung, C. K., Bychkov, A. & Kakudo, K. Update from the 2022 World Health Organization classification of thyroid tumors: a standardized diagnostic approach. Endocrinol. Metab. 37, 703–718 (2022).
Rivera, M. et al. Encapsulated papillary thyroid carcinoma: a clinico-pathologic study of 106 cases with emphasis on its morphologic subtypes (histologic growth pattern). Thyroid 19, 119–127 (2009).
Liu, J. et al. Follicular variant of papillary thyroid carcinoma: a clinicopathologic study of a problematic entity. Cancer 107, 1255–1264 (2006).
Vivero, M., Kraft, S. & Barletta, J. A. Risk stratification of follicular variant of papillary thyroid carcinoma. Thyroid 23, 273–279 (2013).
Kim, M. J. et al. Clinical characteristics of subtypes of follicular variant papillary thyroid carcinoma. Thyroid 28, 311–318 (2018).
O’Gorman, C. S. et al. Thyroid cancer in childhood: a retrospective review of childhood course. Thyroid 20, 375–380 (2010).
Balachandar, S. et al. Pediatric differentiated thyroid carcinoma of follicular cell origin: prognostic significance of histologic subtypes. Thyroid 26, 219–226 (2016).
Samuels, S. L. et al. Characteristics of follicular variant papillary thyroid carcinoma in a pediatric cohort. J. Clin. Endocrinol. Metab. 103, 1639–1648 (2018).
M, R. et al. Encapsulated papillary thyroid carcinoma: a clinico-pathologic study of 106 cases with emphasis on its morphologic subtypes (histologic growth pattern). Thyroid: Official J. Am. Thyroid Association 19, (2009).
Hahn, S. Y. et al. Role of ultrasound in predicting tumor invasiveness in follicular variant of papillary thyroid carcinoma. Thyroid 27, 1177–1184 (2017).
Yang, G. C. H., Fried, K. O. & Scognamiglio, T. Can cytology and the thyroid imaging, reporting, and data system (TI-RADS) identify noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) before surgery? J. Am. Soc. Cytopathol. 9, 159–165 (2020).
Pereira, M., Williams, V. L., Johnson, H., Valderrabano, P. & J. & Thyroid cancer incidence trends in the United States: association with changes in professional guideline recommendations. Thyroid 30, 1132–1140 (2020).
Bychkov, A., Jung, C. K., Liu, Z. & Kakudo, K. Noninvasive follicular thyroid neoplasm with papillary-like nuclear features in Asian practice: perspectives for surgical pathology and cytopathology. Endocr. Pathol. 29, 276–288 (2018).
Kuss, O., Blettner, M. & Börgermann, J. Propensity score: an alternative method of analyzing treatment effects. Dtsch. Arztebl Int. 113, 597–603 (2016).
Austin, P. C. Goodness-of-fit diagnostics for the propensity score model when estimating treatment effects using covariate adjustment with the propensity score. Pharmacoepidemiol Drug Saf. 17, 1202–1217 (2008).
Nikiforov, Y. E. et al. Nomenclature revision for encapsulated follicular variant of papillary thyroid carcinoma: a paradigm shift to reduce overtreatment of indolent tumors. JAMA Oncol. 2, 1023–1029 (2016).
Basolo, F., Macerola, E., Poma, A. M. & Torregrossa, L. The 5th edition of WHO classification of tumors of endocrine organs: changes in the diagnosis of follicular-derived thyroid carcinoma. Endocrine 80, 470–476 (2023).
Mariani, R. A., Kadakia, R. & Arva, N. C. Noninvasive encapsulated follicular variant of papillary thyroid carcinoma: should it also be reclassified in children? Pediatr. Blood Cancer. 65, e26966 (2018).
Song, Y. S. et al. Comprehensive transcriptomic and genomic profiling of subtypes of follicular variant of papillary thyroid carcinoma. Thyroid 28, 1468–1478 (2018).
Ganly, I. et al. Invasion rather than nuclear features correlates with outcome in encapsulated follicular tumors: further evidence for the reclassification of the encapsulated papillary thyroid carcinoma follicular variant. Hum. Pathol. 46, 657–664 (2015).
Cancer Genome Atlas Research Network. Integrated genomic characterization of papillary thyroid carcinoma. Cell 159, 676–690 (2014).
Yadav, S. et al. Macrofollicular architecture in invasive encapsulated follicular variant of papillary thyroid carcinoma: a pitfall in thyroid practice. Head Neck Pathol. 17, 899–909 (2023).
Rosario, P. W. Ultrasonography and cytology as predictors of noninvasive follicular thyroid (NIFTP) neoplasm with papillary-like nuclear features: importance of the differential diagnosis with the invasive encapsulated follicular variant of papillary thyroid cancer. Clin. Endocrinol. (Oxf). 87, 635–636 (2017).
Fu, G., Polyakova, O., MacMillan, C., Ralhan, R. & Walfish, P. G. Programmed death - ligand 1 expression distinguishes invasive encapsulated follicular variant of papillary thyroid carcinoma from noninvasive follicular thyroid neoplasm with papillary-like nuclear features. EBioMedicine 18, 50–55 (2017).
Bi, J., Lyu, P. F., Wang, Y. & Zhang, H. Survival benefit of active surveillance for papillary thyroid carcinoma: a propensity score matching analysis based on SEER database. Front. Oncol. 13, 1185650 (2023).
Lang, B. H. H., Lo, C. Y., Chan, W. F., Lam, K. Y. & Wan, K. Y. Staging systems for papillary thyroid carcinoma: a review and comparison. Ann. Surg. 245, 366–378 (2007).
Holoubek, S. A. et al. Aggressive variants of papillary thyroid microcarcinoma are associated with high-risk features, but not decreased survival. Surgery 167, 19–27 (2020).
Holoubek, S. A. et al. Radioactive iodine does not improve overall survival for patients with aggressive variants of papillary thyroid carcinoma less than 2 cm. Surgery 171, 203–211 (2022).
Khokar, A. M. et al. Survival with follicular and hurthle cell microcarcinoma compared to papillary thyroid microcarcinoma: a population study of 84,532 patients. World J. Surg. 44, 469–478 (2020).
Giani, C. et al. Whole tumor capsule is prognostic of very good outcome in the classical variant of papillary thyroid cancer. J. Clin. Endocrinol. Metab. 106, e4072–e4083 (2021).
Xu, B., Wang, L., Tuttle, R. M., Ganly, I. & Ghossein, R. Prognostic impact of extent of vascular invasion in low-grade encapsulated follicular cell-derived thyroid carcinomas: a clinicopathologic study of 276 cases. Hum. Pathol. 46, 1789–1798 (2015).
Acknowledgements
We express our gratitude to the SEER database project team for generously sharing their high-quality data.
Funding
This work was supported by the Eighth Batch of Guizhou High-level Innovative Talents “Thousand-level” Talents (GCC-[2024]020), the Qian Ke He Foundation(ZK[2024]-459), Science and Technology Fund of Guizhou Provincial Health Commission(gzwkj2024-025) and the Hospital for Guizhou Provincial People’s, Foundation([2023]-21), and the Hebei Natural Science Foundation (H2021109008).
Author information
Authors and Affiliations
Contributions
SJ, PL and HWZ were responsible for the conception and design of the study. SJ collected data and performed the statistical analysis. SJ, LX, GYZ, KDX, LL, and PL authored, edited, reviewed, and revised the manuscript. HWZ and PL provided financial support. HZL contributed significantly to the manuscript revision and response to reviewers. All authors reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The SEER database is publicly available and does not contain patient information; consequently, ethical review and approval was waived.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jin, S., Xie, L., Zhang, G. et al. Prognosis of invasive encapsulated follicular variant and classical papillary thyroid carcinoma: a propensity score-matched study using the SEER database. Sci Rep 15, 413 (2025). https://doi.org/10.1038/s41598-024-84425-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-84425-w