Abstract
Bone health problem is one of the important concomitant diseases of breast cancer (BC). This study aimed to investigate the bone health status of newly diagnosed female BC patients in China. A total of 636 newly diagnosed female BC patients and 268 women undergoing routine physical examinations (control group) were included. Bone mineral density and bone metabolism parameters were assessed. The association between BC and abnormal bone mass (ABM) was analyzed by logistic regression. We found that approximately 15.3% of BC patients presented with hypocalcemia after albumin adjustment. 25-OHVitD deficiency or insufficiency was observed in 92.3% of BC patients. ABM was identified in 63.2% of BC patients, comprising 36.4% with osteopenia and 26.8% with osteoporosis. ABM prevalence was significantly higher in BC patients under 40 years old (40.8%) compared to 8% in the age-matched control group. The severity of bone loss correlated with elevated bone turnover markers. Logistic regression analysis showed that a 5.5-fold and 3.4-fold increased risk of ABM and osteoporosis, respectively, in newly diagnosed BC patients versus the control group. All BC subtypes were associated with a markedly higher risk of ABM. Young BC patients (< 45 years) exhibited a nearly 9-fold higher risk of ABM compared to their age-matched counterparts. Vitamin D deficiency/insufficiency, osteopenia, and osteoporosis were highly prevalent among newly diagnosed female BC patients. Regardless of age and BC subtype, BC patients face a higher risk of ABM compared to those physical examination women, especially among the young.
Similar content being viewed by others
Introduction
According to the Global Cancer Statistics of 2020, breast cancer (BC) has surpassed lung cancer as the most commonly diagnosed cancer, accounting for approximately 2.26 million new cases (11.7%), posing a significant threat to the women’s physical and mental health1. In recent years, advancements in dignostic and therapeutic technologies have led to a gradual increase in the 5-year survival rate for patients. Consequently, many BC patients live with chronic disease status, underscoring the importance of long-term follow-up and management strategies to enhance patients’ prognosis and quality of life. The concomitant diseases of breast cancer (CDBC) encompass a spectrum of conditions indirectly associated with BC, arise from multiple factors including aging, changes in the internal microenvironment, lifestyle alterations, and adverse effects of cancer treatments. CDBC significantly impacts a patient’s quality of life and, in severe cases, can lead to disabilities or life-threatening complications2. The Comprehensive Management Guideline for Breast Cancer Followed-up and Concomitant Diseases3 (2019) highlights that CDBC primarily encompass dyslipidemia, abnormal bone metabolism, and mental health issues such as anxiety and depression. Abnormal bone metabolism refers to bone diseases caused by various reasons mainly characterized by an imbalance between bone formation and resorption, manifests clinically as changes in bone density and strength, bone pain, deformity, and fracture4. Abnormal bone metabolism is one of the most important CDBCs with a high incidence, and requires comprehensive management.
In addition to bone metastasis, BC patients may experience a range of bone-related issues including vitamin D deficiency, calcium deficiency5, osteopenia, and osteoporosis, as well as osteoarthritis and bone pain related to abnormal bone metabolism. Bone metabolic markers play an important role in bone resorption and formation, mainly including mineral ions (calcium, magnesium, phosphorus), bone metabolism-related hormones l (parathyroid hormone [PTH], vitamin D, calcitonin), and bone turnover markers like osteocalcin, bone alkaline phosphatase, type I procollagen N/C-terminal propeptide, type I collagen N/C-terminal peptide crosslink, etc. Calcium, vitamin D, and PTH are crucial in oncogenesis and tumor progression, with deficiencies in calcium and vitamin D, along with elevated PTH levels, exhibiting carcinogenic and tumor-promoting effects6,7. Researches reported that 66.2–95.6% of BC patients experience vitamin D deficiency or insufficiency, a rate significantly higher than in healthy women8,9,10. The intricate interplay between vitamin D and PTH regulates intestinal calcium and phosphorus absorption, maintaining calcium balance and modulating bone resorption and formation11. Furthermore, BC patients face a heightened risk of osteoporosis due to the effects of the disease and its treatments. Osteoporosis, an independent risk factor for fractures, may create a conducive bone microenvironment for BC bone metastasis12. Hence, assessing bone mineral density (BMD) is as important as monitoring bone metabolism markers in the management and follow-up of BC patients. In clinical practice, measurement of BMD can reflect the extent of bone loss and help evaluate the risk of bone fracture. Dual-energy X-ray absorptiometry (DXA), quantitative CT and quantitative ultrasound are commonly uesd methods for BMD assessment. DXA is the preferred method due to its low radiation exposure, rapid detection and convenience13. This study aims to reveal the current status of BMD and bone metabolism in female BC patients utilizing a substantial data set from a single center of China. It focuses on exploring the correlations and differences in BMD and bone metabolism among different BC subtypes.
Methods
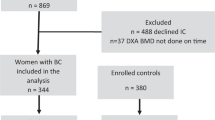
Study populations
This observational cross-sectional study enrolled female BC patients with pathologically confirmed diagnoses, who were hospitalized in the Department of Breast and Thyroid Surgery of The First Affiliated Hospital of Chongqing Medical University (The Chongqing Breast Cancer Center) from 2015 to 2021. Simultaneously, healthy women undergoing routine health examinations at the Health Management Center of the First Affiliated Hospital of Chongqing Medical University (Chongqing Health Management Quality Control Center) from April to October 2021 were included as the control group. Inclusion criteria for this study were: patients with pathologically confirmed in-situ or invasive breast cancer who had not undergone any BC related treatments, were 18 years of age or older, and had completed BMD and/or bone metabolism examinations. Exclusion criteria: (1) Missing the results of both BMD and bone metabolism examination indexes; (2) Death during the study period due to disease progression, recurrence, or other causes; (3) Presence of distant metastases such as bone metastases in initial diagnosis; (4) History of other malignant tumors; (5) Previous history of thyroid and parathyroid surgery; (6) History of severe liver and kidney disease.
Study data collection and interpretation
Patients’ demographic information, medical history, and medication records were obtained from the electronic medical record system or through outpatient follow-ups. General serologic indexes and bone turnover markers of the participants were tested and reviewed by professional technicians in the Clinical Medical Laboratory. All blood samples were collected after a strict fasting period of more than 8 h. For BC patients the blood samples were obtained before any BC related treatments. General serologic indexes were measured by dry chemical method with VITROS5600 (Ortho Clinical Diagnostics, US). 25-OHVitD and PTH were measured using the ECL8000 system (Lifotronic Technology Co., Ltd) via electrochemiluminescence immunoassay. Calcitonin, β-collagen special sequence, osteocalcin, and total type I collagen N-terminal propeptide were determined using E602 (Roche) with electrochemiluminescence immunoassay. It is worth noting that the bone metabolism indexes (25-OHVitD, PTH, calcitonin, bone alkaline phosphatase) of BC patients were measured and reviewed by professional technicians in the Endocrinology Laboratory. In this study, Vitamin D status of deficiency [< 20 ng/mL (50 nmol/L)], insufficiency [20–30 ng/mL (50–75 nmol/L)] and sufficient [≥ 30 ng/mL (75 nmol/L)] were determined by the criteria set by the International Osteoporosis Foundation14 and the American Endocrine Association15.
In this study, HOLOGIC Discovery DXA system was utilized to measure BMD at the hip (femoral neck, femoral trochanter, Ward’s triangle) and lumbar spine (L1–L4 vertebrae). For BC patients, BMD measurements were conducted prior to initiating of any cancer-related treatments, while for the control group, BMD assessments were performed during routine physical examinations. Notably, BMD measurements for the control group were limited to the lumbar spine, providing only an overall lumbar BMD value without detailed data for individual vertebrae. BMD of the measured site was calculated by dividing bone mineral content (g) by the area (cm2). The results were expressed as T-scores and Z-scores. T-scores indicate the difference between the patient’s BMD and the average peak BMD of a healthy young adult, expressed in standard deviation (SD). In contrast, Z-scores compare the patient’s BMD to an age- and ethnicity-matched reference population. In accordance with the diagnostic criteria outlined by the World Health Organization16, BMD in this study was categorized into normal bone mass (T-score ≥ − 1.0 SD), osteopenia (T-score between − 2.5 and − 1.0 SD), and osteoporosis (T-score ≤ − 2.5 SD). For analysis, osteopenia and osteoporosis were collectively categorized to as abnormal bone mass (ABM).
Based on the immunohistochemistry results, the BC patients were classified into three groups: the Luminal group [estrogen receptor (ER) and/or progesterone receptor (PR) positive), the human epidermal growth factor receptor 2 (Her-2) overexpression group (ER and PR negative, Her-2 positive), and the triple-negative group (ER, PR and Her-2 negative).
Statistical analysis
All statistical analyses were performed in Statistical Package for the Social Sciences (SPSS) version 26.0. Continuous variables in this study were presented as medians (interquartile range) following normality testing, while categorical variables were described as A% (n/N). Mann–Whitney U test/Kruskal–Wallis test was utilized to compare continuous variables due to their non-normal distribution. The Chi-square test was performed to compare the risk of bone loss between different groups. Binary logistic regression models were applied to estimate odds ratios (OR) and 95% confidence intervals (CI) for the association between BC and ABM, using the physical examination women as the reference. A two-tailed P value of < 0.05 was considered statistically significant.
Results
Basic characteristics of participants
This study included 636 newly diagnosed BC patients with pathologically confirmed diagnosis, with a median age of 52 years. Among them, 435 patients completed DXA examination and 432 completed bone metabolism examination. Additionally, 268 healthy women were enrolled as a control group with a median age of 51 years. The Body Mass Index (BMI) of newly diagnosed BC patients was significantly higher than that of control group (median BMI = 22.27 kg/m2, P < 0.05). The levels of liver enzymes and cholesterol in BC patients were notably lower than those in the control group, but there was no significant difference in kidney function indexes. A detailed summary of their baseline characteristics is presented in Supplementary Table 1.
General overview of bone health in newly diagnosed BC patients
The average serum calcium level of BC patients was 2.29 mmol/L, significantly lower than that of the control group (2.34 mmol/L, P < 0.05). Approximately 2.5% of BC patients presented with hypocalcemia at initial diagnosis, which increased to 15.3% after adjustment for albumin. 83.8% of the BC patients had serum calcium concentrations within the range of 2.11–2.40 mmol/L. The median levels of 25-OHVitD in BC patients and the physical examination women were 17.4 ng/mL and 14.09 ng/mL, respectively. In this study, 25-OHVitD sufficiency (30 ng/mL) was achieved in only 6.7% of BC patients. 25-OHVitD deficiency and insufficiency were highly prevalent, affecting 92.3% of BC patients, of which 25-OHVitD deficiency accounting for 62.7%, and about 10.2% of patients exhibited severe 25-OHVitD deficiency (< 10 ng/mL). Vitamin D deficiency and insufficiency was also common in the control group, highlighting a widespread issue in the general population. A detailed breakdown of these findings is provided in Table 1.
The average BMD of the hip and lumbar spine in BC patients were 0.850 g/cm2 and 0.874 g/cm2, respectively. The lumbar spine BMD in BC patients was significantly lower than 0.927 g/cm2 observed in the physical examination women. The proportion of normal bone mass, osteopenia and osteoporosis of BC patients were 25.3%, 48.0% and 26.7%, respectively (Supplementary Table 2).
Among BC patients, 63.2% exhibited ABM in the lumbar spine, with 36.4% classified as osteopenia and 26.8% diagnosed with osteoporosis. These rates were markedly higher than the control group, where 22.8% exhibited osteopenia and 13.4% had osteoporosis (P < 0.001). While 43.7% of the control group had an overall T-score for the lumbar spine greater than or equal to 0, only 11.5% of BC patients achieved this benchmark. Furthermore, severe osteoporosis (T ≤ -3.5) was observed in 8.0% of BC patients (Table 2) .
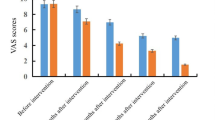
Figure 1 illustrates the BMD of lumbar vertebra of participants stratified by age, revealing a clear trend: with increasing age, the proportion of ABM rises in both in BC patients and the control group. However, across all age brackets, BC patients consistently exhibit significantly higher rates of osteopenia and osteoporosis compared to the physical examination group. In BC patients over 40, 50 and 60 years old, the rates of osteoporosis were 28.5%, 45.8%, 57.3%, respectively, while the rates of opteopenia were 37.9%, 40.1%, 31.7%. In the control group within the same age brackets, the rates of osteoporosis were 16.6%, 21.6%, 34.9%, and osteopenia rates were 26.3%, 34.0%, 46.0%, respectively, closely aligning with general epidemiological survey results. The proportion of ABM in BC patients younger than 40 was 40.8%, markedly higher than the 8% observed in the same age control group. Moreover, among patients over 54 years, only 9.2% had normal bone mass, and the osteoporosis rate was double that of the same age control group (56.0% vs. 28.0%; P < 0.001). It is noteworthy that 22% of female BC patients over 60 years old exhibited severe osteoporosis, compared to only 11.2% in the control group.
Correlation between lumbar spine BMD and bone metabolism
Serum calcium levels consistent at approximately 2.30mmol/L across patients with normal bone mass, osteopenia and osteoporosis, showing no statistical difference (P = 0.175). Although the median levels of 25-OHVitD and PTH appeared to increase with bone loss, the differences were not statistically significant (P25 -OHVitD = 0.244, PPTH = 0.097). In contrast, Bone turnover markers such as bone alkaline phosphatase, β collagen special sequence, osteocalcin, total type I collagen N-terminal propeptide, exhibited a gradual increase with bone loss. The severity of bone loss correlated with a more pronounced increase in bone turnover markers (P < 0.001) (Table 3). According to the overall T-score of lumbar spine, the results of five stratification (Supplementary Table 3) were consistent with those of the three layers. As the T-score value decreased, various bone turnover markers exhibited a significant increase (P < 0.001), indicating a notable enhancement in the bone transformation rate. Specifically, osteocalcin levels in patients with severe osteoporosis (T ≤ − 3.5) was nearly double those in individuals with normal bone mass (T ≥ 0), measuring 23.76 ng/mL versus 12.94 ng/mL, respectively (P < 0.001).
Comparative analysis of BMD and bone metabolism across different BC subtypes
This study included 435 newly diagnosed BC patients who underwent DXA examination. Among these, 28 cases (6.4%) were diagnosed with ductal carcinoma in situ, 33 cases (7.6%) with special type invasive cancer, and 374 cases (86.0%) with non-special type invasive cancer. The invasive BC cases were further categorized by molecular subtypes: the luminal type comprised 69.8% (n = 284), the Her-2 overexpression group 12.5% (n = 51), and the triple-negative type 17.7% (n = 72). Quantitative and categorical analyses of BMD and bone metabolism were conducted across these three groups (Supplementary Tables 4 and 5), and the results showed no statistically significant differences in each index among the three groups.
Association between BC and ABM
In order to explore whether BC population is more prone to ABM, and whether ABM is related to BC molecular subtypes, binary logistic regression analysis was performed using the physical examination women as a reference (Table 4). BC was identified as a risk factor for ABM. After adjusting for age and BMI, the BC patients exhibited a 5.53-fold higher risk of ABM compared with the physical examination group (OR 5.53, 95% CI 3.71–8.26, P < 0.001), and a 3.41-fold higher risk of osteoporosis (OR 3.41, 95% CI 2.10–5.55, P < 0.001). When stratified by molecular subtypes, all BC types had a significantly higher risk of ABM than the physical examination women (Luminal type OR 5.21, 95% CI 3.38–8.02; Her-2 overexpression type OR 5.17, 95% CI 2.49–10.72; triple-negative type OR 8.30, 95% CI 4.20–16.43) with statistical differences. For osteoporosis specifically, the risk was increased in luminal (OR 3.58, 95% CI 2.13–6.02, P < 0.001) and triple-negative (OR 3.41, 95% CI 1.63–7.11, P = 0.001) BC subtypes compared with the physical examination women, while Her-2 overexpression BC showed no statistical difference (OR 2.48, 95% CI 0.97–6.34, P = 0.058). Age stratification revealed: premenopausal BC patients (< 45 years) had nearly 9 times higher ABM risk compared with the age-matched control group (OR 8.90, 95% CI 3.47–22.84, P < 0.001). The risk of ABM in perimenopausal BC patients (45–54 years) was also five times (OR 5.09, 95% CI 2.82–9.19, P < 0.001) higher than that in the physical examination women, but the risk of osteoporosis was not statistically significant (OR 1.84, 95% CI 0.78–4.32, P = 0.16). Postmenopausal BC patients (> 54 years) had more than three times the risk of osteoprosis compared with women who underwent physical examination (OR 3.37, 95% CI 1.94–5.86, P < 0.001).
Discussion
This retrospective cross-sectional study investigated the status of bone health of newly diagnosed BC patients by examining BMD and bone metabolism markers. In this study, the median serum calcium level in BC patients was 2.29mmol/L, with 15.3% experienced hypocalcemia at the time of initial diagnosis. This underlines a frequently overlooked phenomenon, emphasizing the need for routine calcium monitoring in newly diagnosed BC patients.
Vitamin D deficiency or insufficiency is a recognized as a global public health concern, affecting over 1 billion people worldwide11. Epidemiological data from China spanning 2010 to 2012 showed that the median vitamin D level in women ranged from 20.1 ng/mL to 22.7 ng/mL, with 38.7–49.5% classified as deficient and only 15.1–21.8% of women achieving adequate vitamin D level17,18. In our study, the median vitamin D level of BC patients was 17.4 ng/mL, which was lower than the epidemiological level. Alarmingly, only 6.7% of BC patients exhibited adequate vitamin D. Moreover, the proportions of severe deficiency, deficiency, insufficient were 10.2%, 52.5% and 30.6% respectively, which were much higher than the epidemiological data, aligning with previous study10.
Preclinical trials have unequivocally demonstrated the critical role of calcitriol in modulating BC cells behavior, demonstrating its ability to suppress proliferation, angiogenesis, invasion, and metastasis. The deficiency and insufficiency of vitamin D have been identified as a potential risk factor for BC initiation and progression7. However, clinical evidence linking vitamin D status to BC occurrence and outcomes remains inconclusive. Some studies have shown that the risk of BC decreased significantly with the increase of serum 25-OHVitD concentration19,20, and adequate vitamin D can also reduce the mortality and improve the prognosis of patients21,22. Conversely, an international pooling project of 17 cohorts23 revealed that there was no significant association between vitamin D status and the subsequent incidence of invasive BC. Still, it suggested an inverse, though non-significant, association with and distant metastatic and triple-negative BC (TNBC) without statistical significance. Previous study has revealed a strong association between severe vitamin D deficiency and an increased risk of TNBC. For example, one study24 reported that 18% of patients with severe vitamin D had TNBC, compared to only 8% of those with vitamin D levels above 10 ng/mL, with a relative risk increase of 2.54 times in the severely deficient group. In our study, TNBC accounted for 27.78% of patients with severe vitamin D deficiency, notably higher than 16.24% in patients with vitamin D > 10 ng/mL, though this difference was not statistically significant. The median serum vitamin D level of TNBC patients (17.2 ng/mL) was lower than that in luminal (18.3 ng/mL) and Her-2 overexpression (20.5 ng/mL) subtypes. Similarly, the proportion of vitamin D deficiency (74.4%) and severe deficiency (11.6%) in TNBC exceeded those in luminal and Her-2 overexpression types. It can be seen that patients with TNBC have lower vitamin D levels, although a statistical difference has not been reached, likely due to the limited sample size. Large-scale, well-designed trials are essential to elucidate the relationship between vitamin D status and BC subtypes, particularly TNBC, and to clarify its potential as a modifiable risk factor and therapeutic target.
Epidemiological data25 showed that the prevalence of osteoporosis in women aged over 40, 50 and 60 years old was 13.39%, 25.99% and 38.67%, respectively. In this study, comparable rates of 16.6%, 21.6%, and 34.9% were observed among the physical examination group, affirming the validity of our BMD measurements. The proportion of lumbar spine osteoporosis in BC patients was 25.2%, significantly surpassing the 13.4% observed in the physical examination women. According to the data derived from National Health and Nutrition Examination Survey database26, patients with breast, lung, and skin cancer were more prone to osteopenia/osteoporosis than those without cancer. Upon age stratification, 39% of young BC patients (< 45 years old)exhibited ABM, a stark contrast to the 7.9% observed in healthy women of the same age group. Among older BC patients (> 54 years), only 9.2% had normal bone mass, with the prevalence of osteoporosis doubling that of the age-matched control group (56% vs. 28%; P < 0.001). These findings underscore the significant bone health challenges BC patients face even before receiving interventions such as chemotherapy or endocrine therapy, which are known to exacerbate bone loss. The risk of ABM in young female BC patients is nearly 9 times higher than that in healthy women, a significantly higher risk than that seen in perimenopausal and postmenopausal BC patients. This highlights the importance of early BMD assessment and monitoring not only in older women but also in younger BC patients to enable timely preventive and therapeutic interventions. In addition to its diagnostic use, assessment of BMD is also used to predict fracture risk. Each standard deviation decrease in BMD approximately doubles fracture risk, though the risk gradient varied depending on measuring site, detecting technique, patient age, and fracture outcome27,28. According to the recommendations of the World Health Organization and the International Osteoporosis Foundation29,30, the femoral neck of the hip is the preferred site for the diagnosis of osteoporosis because of its higher predictive value for fracture risk. While bone density measurements of the spinal vertebrae are often used for the evaluation of treatment response, but the lumbar spine is also an important evaluation site for osteoporosis. Most vertebral compression fractures go unnoticed and therefore remain undiagnosed. Moderate or severe vertebral fractures, even if asymptomatic, constitute a strong risk factor for subsequent fractures at the spine and other skeletal sites31,32,33. These considerations reinforce the need for comprehensive and site-specific BMD evaluations in BC patients.
While numerous studies have explored the impact of systematic treatment of BC on bone, research linking BC subtypes to bone mass remains limited. In this study, regardless of the BC molecular type, the risk of ABM and osteoporosis in BC patients was higher than that in healthy individuals. The incidence of osteoporosis was lower in patients with Her-2 overexpression type BC (hip: 3.9%, lumbar: 16.0%) compared to luminal (hip: 9.6%, lumbar: 26.3%) and triple-negative (hip: 9.7%, lumbar: 25.0%) type BC, although the differences were not statistically significant. Binary logistic regression model further substantiated that the risk of ABM and osteoporosis was lower in the Her-2 overexpression type compared to the other two types. Given the well-known substantially impact of hormone receptor-positive BC on reducing bone mass, it is necessary to strengthen the BMD assessments at the time of luminal type BC diagnosis. Timely prevention or intervention is essential to mitigating progressive bone loss and reducing fracture risk.
This cross-sectional study integrated the results of bone metabolism and BMD to provide a comprehensive analysis of bone health in female BC patients. Its strengths lie in its large sample size and novel findings. However, limitations include the absence of detailed patient symptomatology and prior treatment histories, such as supplementation with vitamin D, calcium, or anti-osteoporosis medications. Such therapies could have influenced bone density measurements and serum calcium levels, potentially leading to an underestimation of the prevalence of ABM and calcium deficiency in our study. These omissions limit definitive conclusions regarding the role of such interventions in improving bone health. Further longitudinal research is warranted to explore these factors and validate the findings.
Data availability
Raw data and additional information can be obtained with the consent of the corresponding author upon reasonable request.
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. https://doi.org/10.3322/caac.21660 (2021).
Kong, L., Li, H., Li, H., Ren, G. & Wu, K. To strengthen the diagnosis and treatment of concomitant diseases of breast cancer. Chin. J. Endocr. Surg. 12, 353–357. https://doi.org/10.3760/cma.j.issn.1674-6090.2018.05.001 (2018).
Fei, M., Binghe, X. & Zhimin, S. Comprehensive management guideline for breast cancer follow-up and concomitant diseases. Chin. J. Oncol. 41, 29–41. https://doi.org/10.3760/cma.j.issn.0253-3766.2019.01.006 (2019).
Medicine CSoP. Consensus on the diagnosis and treatment of pain diseases related to abnormal bone metabolism. Chin. Med. J. 100, 15–21. https://doi.org/10.3760/cma.j.issn.0376-2491.2020.01.005 (2020).
Lingquan, K. et al. Strengthening the management of vitamin D deficiency/insufficiency and its associated hyperparathyroidism in breast cancer patients. Chin. J. Endocr. Surg. 14, 353–357. https://doi.org/10.3760/cma.j.cn.115807-20200611-00178 (2020).
Almquist, M., Manjer, J., Bondeson, L. & Bondeson, A. G. Serum calcium and breast cancer risk: Results from a prospective cohort study of 7,847 women. Cancer Causes Control CCC 18, 595–602. https://doi.org/10.1007/s10552-007-9001-0 (2007).
Welsh, J. Vitamin D and breast cancer: Past and present. J. Steroid Biochem. Mol. Biol. 177, 15–20. https://doi.org/10.1016/j.jsbmb.2017.07.025 (2018).
de Sousa, A.-F. et al. Vitamin D deficiency is associated with poor breast cancer prognostic features in postmenopausal women. J. Steroid Biochem. Mol. Biol. 174, 284–289. https://doi.org/10.1016/j.jsbmb.2017.10.009 (2017).
Karthikayan, A., Sureshkumar, S., Kadambari, D. & Vijayakumar, C. Low serum 25-hydroxy vitamin D levels are associated with aggressive breast cancer variants and poor prognostic factors in patients with breast carcinoma. Arch. Endocrinol. Metab. 62(4), 452–459. https://doi.org/10.20945/2359-3997000000062 (2018).
Hsieh, E. et al. Vertebral fractures among breast cancer survivors in China: A cross-sectional study of prevalence and health services gaps. BMC Cancer 18, 104. https://doi.org/10.1186/s12885-018-4014-5 (2018).
Holick, M. F. Vitamin D deficiency. N. Engl. J. Med. 357, 266–281. https://doi.org/10.1056/NEJMra070553 (2007).
Salamanna, F., Borsari, V., Contartese, D., Nicoli Aldini, N. & Fini, M. Link between estrogen deficiency osteoporosis and susceptibility to bone metastases: A way towards precision medicine in cancer patients. Breast (Edinburgh, Scotland) 41, 42–50. https://doi.org/10.1016/j.breast.2018.06.013 (2018).
Yuanzheng, M. et al. 2018 Chinese guideline for the diagnosis and treatment of senile osteoporosis. Chin. J. Health Manag. 12, 484–509. https://doi.org/10.3760/cma.j.issn.1674-0815.2018.06.002 (2018).
Dawson-Hughes, B. et al. Estimates of optimal vitamin D status. Osteoporos. Int. 16, 713–716. https://doi.org/10.1007/s00198-005-1867-7 (2005).
Holick, M. F. et al. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 96, 1911–1930. https://doi.org/10.1210/jc.2011-0385 (2011).
Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group World Health Organ Tech Rep Ser 843 (1994).
Xiaobing, L. et al. Serum vitamin D levels of Chinese rural women of childbearing age in 2010–2012. J. Hyg. Res. 46, 367–372. https://doi.org/10.19813/j.cnki.weishengyanjiu.2017.03.005 (2017).
Jiaxi, L. et al. The vitamin D nutritional status in Chinese urban women of child-bearing age from 2010 to. Chin. J. Prev. Med. 51, 112–116. https://doi.org/10.3760/cma.j.issn.0253-9624.2017.02.003 (2012).
Chen, P. et al. Meta-analysis of vitamin D, calcium and the prevention of breast cancer. Breast Cancer Res. Treat. 121, 469–477. https://doi.org/10.1007/s10549-009-0593-9 (2010).
Mohr, S. B. et al. Serum 25-hydroxyvitamin D and prevention of breast cancer: Pooled analysis. Anticancer Res. 31, 2939–2948 (2011).
Vaughan-Shaw, P. G. et al. The impact of vitamin D pathway genetic variation and circulating 25-hydroxyvitamin D on cancer outcome: Systematic review and meta-analysis. Br. J. Cancer 116, 1092–1110. https://doi.org/10.1038/bjc.2017.44 (2017).
Madden, J. M., Murphy, L., Zgaga, L. & Bennett, K. De novo vitamin D supplement use post-diagnosis is associated with breast cancer survival. Breast Cancer Res. Treat. 172, 179–190. https://doi.org/10.1007/s10549-018-4896-6 (2018).
Visvanathan, K. et al. Circulating vitamin D and breast cancer risk: An international pooling project of 17 cohorts. Eur. J. Epidemiol. 38, 11–29. https://doi.org/10.1007/s10654-022-00921-1 (2023).
Chen, H. M., Chen, F. P., Yang, K. C. & Yuan, S. S. Association of bone metastasis with early-stage breast cancer in women with and without precancer osteoporosis according to osteoporosis therapy status. JAMA Netw. Open 2, e190429. https://doi.org/10.1001/jamanetworkopen.2019.0429 (2019).
Wang, J. et al. The prevalence of osteoporosis in China, a community based cohort study of osteoporosis. Front. Public Health 11, 1084005. https://doi.org/10.3389/fpubh.2023.1084005 (2023).
Huang, J. F. et al. Bone mineral density, osteopenia and osteoporosis among US adults with cancer. QJM Int. J. Med. 115, 653–660. https://doi.org/10.1093/qjmed/hcac015 (2022).
Marshall, D., Johnell, O. & Wedel, H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ (Clin. Res. Ed.) 312, 1254–1259. https://doi.org/10.1136/bmj.312.7041.1254 (1996).
Johnell, O. et al. Predictive value of BMD for hip and other fractures. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 20, 1185–1194. https://doi.org/10.1359/jbmr.050304 (2005).
Kanis, J. A. & Glüer, C. C. An update on the diagnosis and assessment of osteoporosis with densitometry. Osteoporos. Int. 11, 192–202. https://doi.org/10.1007/s001980050281 (2000).
Kanis, J. A. et al. A reference standard for the description of osteoporosis. Bone 42, 467–475. https://doi.org/10.1016/j.bone.2007.11.001 (2008).
Melton, L. J. 3rd., Atkinson, E. J., Cooper, C., O’Fallon, W. M. & Riggs, B. L. Vertebral fractures predict subsequent fractures. Osteoporos. Int. 10, 214–221. https://doi.org/10.1007/s001980050218 (1999).
Lindsay, R. et al. Risk of new vertebral fracture in the year following a fracture. JAMA 285, 320–323. https://doi.org/10.1001/jama.285.3.320 (2001).
Johansson, H., Odén, A., McCloskey, E. V. & Kanis, J. A. Mild morphometric vertebral fractures predict vertebral fractures but not non-vertebral fractures. Osteoporos. Int. 25, 235–241. https://doi.org/10.1007/s00198-013-2460-0 (2014).
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Juan Wu, Ying Li, Xin-yu Liang, Liang Ran and Lei Hu. Analysis was performed by Juan Wu, Rui-ling She, Xiu-quan Qu, Bai-qing Peng. The first draft of the manuscript was written by Juan Wu, Xin-yu Liang and all authors commented on previous versions of the manuscript. Ling-quan Kong, Jing Wang and Kai-nan Wu directed the concept and design of the study and revised the manuscript. All authors read and approved the final manuscript. The work reported in the paper has been performed by the authors, unless clearly specified in the text.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This research was approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University and the study was performed in accordance with the Declaration of Helsinki.
Consent to participate
Due to the retrospective nature of the study, Ethics Committee of the First Affiliated Hospital of Chongqing Medical University waived the need of obtaining informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, J., Liang, Xy., Hu, L. et al. Bone health in newly diagnosed female breast cancer patients in China: a cross-sectional study. Sci Rep 15, 3982 (2025). https://doi.org/10.1038/s41598-024-84698-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-84698-1