Abstract
Metabolic dysfunction associated fatty liver disease (MAFLD) is a prevalent liver condition and presents a major clinical and public health problem worldwide. TyG index and its related parameters TyG-WHtR, TyG-WC and TyG-BMI have been proven to label insulin resistance reliably, which makes it an important parameter to reflect the composition and health status of human body. Recent studies in the general population have demonstrated that there exists a correlation between elevated TyG index and the development of MAFLD, but in the nondiabetic US population, this correlation remains unclear. We included 945 nondiabetic adult participants from NHANES 2017–2020 cycle in this cross-sectional study. To find the relationship that exists between TyG, TyG-WHtR, TyG-WC, TyG-BMI, HOMA-IR, QUICKI and the risk of MAFLD, we used four conventional multivariate adjusted logistic regression models, plotted the RCSs to conduct this study, analyzed the thresholds using a two-stage logistic model. We performed stratified and interaction analyses to identify whether the relationships were stable in different subgroups. Moreover, we assessed the predictive ability of these parameters for MAFLD by plotting ROCs. We found that there was a positive correlation between TyG index and the incidence of MAFLD as well as its related parameters in the nondiabetic population.
Similar content being viewed by others
Introduction
MAFLD, a new diagnostic definition proposed in 2020 by an international panel of experts from 22 countries, emphasizing the metabolic disorders that accompany fatty liver disease. MAFLD, originally known as nonalcoholic fatty liver disease (NAFLD), is one of the leading cause of the global epidemic of chronic liver disease, the prevalence of which is increasing annually and is trending towards younger population, which poses a major health and economic burden to the society1,2,3,4. To detect and evaluate the degree of hepatic steatosis is crucial for the evaluation and clinical prognosis of MAFLD patients. Currently, the gold standard for assessing the degree of hepatic steatosis remains biopsy. Controlled attenuation parameter (CAP) values have been proved to be a reliable, noninvasive method for quantitatively assessing and classifying hepatic steatosis, which is measured by vibration controlled transient elastography (VCTE) devices5,6.
IR is closely related to MAFLD. It relates to the formation mechanism of MAFLD and its further development7. Recently, TyG related parameters have been recognized as a simple, reliable and easy to calculate biomarker of IR8,9,10. TyG index is a key anthropometric parameter that provides valuable insights into the composition of the human body and its health status. While many studies have proved the association of TyG index with cardiovascular diseases, our study focused on the prevalence of MAFLD in a nondiabetic population to further investigate the interrelationship between TyG and its derivatives and MAFLD in a nondiabetic population11,12. This study, using data from the National Health and Nutrition Examination Survey (NHANES) from 2017 to 2020, intended to explore which associations exist between TyG related parameters and MAFLD.
Materials and methods
Data sources
This study used 2017–2020 data from NHANES. It is a survey conducted biennially by the National Center for Health Statistics (NCHS) to assess the health and nutritional status of non-hospitalized populations in the United States and is representative of the whole country (http://www.cdc.gov/nchs/nhanes.htm). The information on Liver Ultrasound Transient Elastography in adults aged 20 and older is only available for the 2017–2020 NHANES cycle. Data were analyzed in February 2024. The study protocol for NHANES was approved by the NCHS Research Ethics Review Board. All methods were performed in accordance with the relevant guidelines and regulations. Participants completed an informed consent form at the time of enrollment (https://www.cdc.gov/nchs/nhanes/irba98.htm). De-identified open data were used in our study, so informed consent was not required. This methodology was in accordance with the reporting guidelines in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE).
Study design and population
A total of 15,560 participants were enrolled in NHANES 2017–2020, 6328 subjects were initially excluded because they were younger than 20 years old. We then excluded 1668 persons who did not have complete VCTE test data; 4034 without laboratory data on fasting glucose and triglycerides. We also excluded 83 participants with liver disease, 456 heavy drinkers and 2046 people with prediabetes or diabetes. Our study finally included 945 nondiabetic participants. The flow chart of exclusion criteria was shown in Fig. 1.
MAFLD
Hepatic steatosis in our research was defined by CAP, which was obtained by VCTE (FibroScan®), a well-established clinical technique that has been shown to be a simple and credible noninvasive method for quantitatively assessing hepatic steatosis13. The test is considered meaningful when at least 10 valid measurements are obtained after 3 h of fasting, and the ratio of the inter-quartile range to the median liver stiffness measurement (LSM) is less than 30%14. We used the median CAP value of ≥ 274 dB/m to define hepatic steatosis. The AUC for this threshold was 0.823 (95%CI: 0.809–0.837), with the sensitivity of 0.688 (95%CI: 0.600–0.750) and the specificity of 0.822 (95%CI: 0.761–0.897)15.
Triglyceride glucose index and related parameters
The TyG index and related parameters were calculated by the following formula12,16,17:
\({\text{TyG}}\,=\,{\text{ln }}\left[ {{\text{Fasting triglycerides }}\left( {{\text{mg}}/{\text{dL}}} \right){\text{ }}*{\text{ Fasting glucose }}\left( {{\text{mg}}/{\text{dL}}} \right){\text{ }}/{\text{2}}} \right]\)
WHtR = Waist circumference /Height. BMI = Weight /Height2. TyG-WHtR = TyG * WHtR. TyG-WC = TyG * Waist circumference. TyG-BMI = TyG * BMI. HOMA-IR = [Fasting glucose (mmol/L) * Fasting insulin (µU/mL)]/22.5. QUICKI = 1/ [log Fasting glucose (mg/dL) + log Fasting insulin (µU/mL)]
Prediabetes and diabetes
The diagnostic criteria for prediabetes and diabetes were based on the American Diabetes Association criteria18. The participants who met one or more of the following criteria were defined as prediabetes: (1) FPG of 100–125 mg/dL, (2) HbA1c of 5.7–6.4%, and (3) self-reported diagnosis of prediabetes. And those were defined as diabetes if they met one of the below criteria: (1) FPG ≥ 126 mg/dL, (2) HbA1c ≥ 6.5%, (3) self-reported diagnosis of diabetes, and (4) treated with glucose-lowering medicine or insulin.
Covariate
The covariate data were derived from questionnaires, physical examinations, and laboratory tests. Sociodemographic variables such as age, gender, race and ethnicity (non-Hispanic white, non-Hispanic black, Mexican American and other race), education level (high school or less, some college and college or above), marital status (married or living with partners and living alone) were extracted from Demographic Variables. Participants with self-reported history of hypertension or systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg were defined as hypertension. According to the intensity of the activity, we classified the physical activity of the participants as vigorous, moderate, or sedentary. Vigorous exercise was defined as high-intensity activities, such as running or playing basketball, which could lead to deeper and faster breathing as well as an increased heart rate. Meanwhile, moderate exercise was defined as continuous participation for at least 10 min in the past 30 days in any moderate exercise that would result in a mild increase in breathing and a slight elevation in heart rate, such as sustained weight-bearing. Based on past and current status, smoking status was defined as: never smoked (or smoked less than 100 cigarettes), former smoker (smoked more than 100 cigarettes but quit now), and current smoker. Heavy drinkers were defined as individuals with a “Yes” answer to the question, “Do you drink 4 or 5 cups or more drinks per day?”. Moreover, BMI, height, wait circumference and hip circumference were extracted from Body Measures. WHtR was defined as the ratio of waist circumference to the body height. Indicators of the relevant experimental were extracted from Laboratory data.
Statistical analyses
Continuous variables with normal distribution were presented as means ± SD and analyzed by t-test. Non-normally distributed continuous variables were expressed as median and inter-quartile range and analyzed using the Mann-Whitney U test. Categorical factors are described as frequencies or proportions, and analyzed by chi-square test. Given that some of the covariates data were missing, but in a small proportion (missing rates ranged from 0 to 8.35%), multiple imputation with 5 replications was performed using the chained equation method in the R Statistical Software (Version 4.2.2), aiming to improve statistical power and reduce the bias caused by the missing data19.
To verify the robustness of our findings, we performed sensitivity analyses to evaluate how different association inference models would affect our conclusions. The effect sizes and P-values derived from all these models were reported and compared. Multivariate logistic regression analysis were performed to calculate odds ratios (ORs) and 95% confidence intervals (CIs) to evaluate the relationship between TyG related parameters and the prevalence of MAFLD. We grouped TyG and its derived parameters in quartiles. The reference group was the lowest quartile. We performed logistic regression of TyG related variables as continuous and categorical variables, respectively. The selection of confounding variables was based on clinical significance and existing scientific literature. Four models were developed for analysis: we adjusted for gender, age, race and ethnicity, and marital status among the sociodemographic variables as model (1) Further adjusted for hip circumference as model (2) Then additionally adjusted for hypertension, physical activity and smoking status as Model (3) Model 4 was fully adjusted, including laboratory parameters (SBP, DBP, HDL, LDL, Tc, CRP, ALT, AST, BUN, GGT and sUA).
We plotted RCSs models, which was built and adjusted with covariates in Model 4, to generate smoothing curves and to test the nonlinear relationships in order to further explore whether there was a link between TyG derived indicators and the incidence of MAFLD. Here, all TyG related parameters were considered as continuous variables. For the linearly variables, we used pearson correlation analysis to calculate the correlation coefficients (r) between the variables and the CAP. For the nonlinearly variables, we used a two-stage logistic model to analyse and deeply evaluate the correlations and thresholds, and here we also adjusted for the covariates in Model 4.
Moreover, logistic regression models were used for interaction and subgroup analyses based on gender, age, race and ethnicity, marital status, hip circumference, hypertention, physical activity, smoking status, SBP, DBP, HDL, LDL, Tc, CRP, ALT, AST, BUN, GGT and sUA. To evaluate the diagnostic efficacy of TyG, TyG-WHtR, TyG-WC and TyG-BMI for MAFLD in a nondiabetic population, we used the area under the receiver operating characteristic curve (AUROC).
The R statistical software (version 4.2.2) and the Free Statistics software (version 1.9) were used for all statistical analyses. A two-sided test P value of less than 0.05 was considered significant.
Results
Baseline features of participants
From the 9232 participants, 6241 individuals with missing or unreliable data for FPG, Tg and CAP values were not included, leaving 945 nondiabetic participants available for analysis. The baseline features of the subjects, grouped by the presence or absence of MAFLD, were displayed in Table 1. Among them, 206 (21.799%) had MAFLD while 739 (78.201%) were free of it. The age of the subjects was (40.197 ± 15.670) years, 590 (62.434%) were female, with a higher number of non-Hispanic whites (345, 36.508%). In the nondiabetic population, compared to non-MAFLD group, participants in MAFLD group were more likely to be female, lower level of education, married or living with a partner, and were noted to have higher BMI, height, waist and hip circumference, WHtR, fasting glucose, HbA1c, insulin, LDL, Tc, Tg, CRP, ALT, AST, BUN, GGT, sUA, TyG related parameters and HOMA-IR, while HDL and QUICKI were lower.
Associations between TyG related parameters and MAFLD
The results of multivariate logistic proportional hazards’ regression are shown in Table 2, which evaluated the effect of TyG, TyG-WHtR, TyG-WC, TyG-BMI, HOMA-IR and QUICKI on the prevalence of MAFLD. When these parameters were analyzed as continuous variables, in the unadjusted crude model, there was a significant and independent correlation between the each unit increases in TyG related parameters and the incidence of MAFLD (TyG index: OR:5.421, 95%CI: 3.831–7.671; TyG-WHtR: OR:4.155, 95%CI:3.317–5.204; TyG-WC: OR:1.009, 95%CI: 1.008–1.011; TyG-BMI: OR:1.023, 95%CI:1.019–1.026; HOMA-IR: OR: 1.712, 95%CI: 1.531–1.914; log2QUICKI: OR: 0.001, 95%CI: 0 – 0.003). It showed that the higher the TyG related parameters, the higher the prevalence of MAFLD. After further adjusting covariates, the results did not change significantly. We then expressed TyG related parameters as quartiles of categorical variables separately and performed sensitivity analyses, finding that MAFLD rates increased with increasing levels of each parameter. In the fully adjusted model 4, compared with Q1, subjects in Q4 for each parameter were more likely to develop MAFLD (TyG index: OR: 3.235, 95%CI: 1.280–8.173; TyG-WHtR: OR: 4.699, 95%CI: 1.950-11.321; TyG-WC: OR: 3.659, 95% CI: 1.347–9.938; TyG-BMI: OR: 4.140, 95%CI:1.481–11.572). The same findings were observed in Models 1–3.
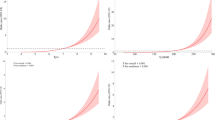
Restricted cubic spline curve
We depicted the RCS curves to further investigate the nonlinear relationship of TyG related parameters, HOMA-IR and QUICKI with MAFLD, as shown in Fig. 2. After considering all potential confounders, all parameters were confirmed to be directly related to MAFLD. It revealed that TyG, TyG-WC, HOMA-IR and QUICKI were linearly correlated with MAFLD (non-linearity: P = 0.542, 0.606, 0.08, 0.861), while TyG-WHtR showed an S-shaped, TyG-BMI suggested a “J-shaped” correlation with it (non-linearity: P = 0.03, 0.015). We then conducted pearson correlation analysis for the parameters of linear relationship, as presented in Table 3. The results showed that TyG, TyG-WC and HOMA-IR were positively correlated with the incidence of MAFLD, with correlation coefficients of 0.360, 0.557 and 0.383 (P < 0.001), respectively, while QUICKI was negatively correlated to it, with a correlation coefficients of -0.423 (P < 0.001). We analyzed the two-stage regression model for the parameters of the non-linear relations, as presented in Table 4. It was found that two inflection points were identified at 4.048 and 6.000 for TyG-WHtR. When TyG-WHtR greater than 4.048 but less than 6.000, a positive association between TyG-WHtR and MAFLD risk was observed (95%CI: 2.264–7.136; P < 0.001). When TyG-WHtR was less than 4.048 or greater than 6.000, MAFLD risk no longer increased with increasing TyG-WHtR. Participants with a TyG-BMI less than 343.965 had an adjusted OR of 1.024 (95%CI: 1.014–1.035; P < 0.001) for the occurrence of MAFLD, whereas the risk of MAFLD no longer increased with increasing TyG-BMI when it was greater than 343.965.
The restricted cubic spline for the relationship between TyG parameters and MAFLD. The restricted cubic spline curves for the relationship between TyG index (A), TyG-WHtR (B), TyG-WC (C), TyG-BMI (D), HOMA-IR (E), QUICKI (F) and MAFLD. The solid lines represent the multivariate-adjusted hazard ratios, while the dashed lines depict the 95% CIs obtained from restricted cubic spline regression. Knots were positioned at the 5th, 35th, 65th, and 95th percentiles for each parameters.
Subgroup analyses
Herein, we conducted stratified and interaction analyses to ascertain whether the association between TyG related parameters and MAFLD incidence was consistent across several subgroups (Fig. 3). The results of the subgroup analyses for HOMA-IR and QUICKI were shown in Supplementary Fig. 1. Consistent results were observed when the analysis was stratified by gender, age, race and ethnicity, educational level, marital status, BMI, hypertension, physical activity and smoking status. As shown in Fig. 3, TyG was associated with MAFLD incidence in all subgroups except those aged ≥ 65, and we did not find statistically significant interactions in the stratified analyses (P all > 0.05). We found a similar association between TyG-WHtR and MAFLD, with interactions for race and education level (P = 0.048, 0.024). In addition, we detected that TyG-WC was associated with MAFLD among subgroups of participants, except the subgroup of ≥ 65 years, non-Hispanic blacks, BMI < 25, with hypertension, moderate physical activity and former smoking, with interactions for physical activity (P = 0.023). What’s more, TyG-BMI had similar findings with MAFLD prevalence in subgroups, except the subgroup of male, ≥ 65 years, non-Hispanic blacks, with hypertension and former smoking, with interactions for race, education level and physical activity (P = 0.024, 0.038, 0.035). In addition, as shown in supplementary Fig. 1, we found similar findings in HOMA-IR and QUICKI, both of which were associated with MAFLD in all subgroups with an interaction of education level (P = 0.002, 0.04).
Association between TyG related parameters and MAFLD in different subgroups. Subgroups analysis of the relationship between TyG index (A), TyG-WHtR (B), TyG-WC (C), TyG-BMI (D), and MAFLD. Except for the stratification component itself, each stratification factor was adjusted for gender, age, race and ethnicity, marital status, hip circumference, hypertention, physical activity, smoking status, SBP, DBP, HDL, LDL, Tc, CRP, ALT, AST, BUN, GGT and sUA. OR, odds ratio; 95% CI, 95% confidence interval.
ROC analysis
In order to assess the role of TyG and its derived parameters in the identification of MAFLD in the nondiabetic population, we performed ROC analysis (Fig. 4). It was found that TyG-BMI had the largest AUROC of 0.825 (95%CI: 0.795–0.857), with sensitivity, specificity and accuracy of 0.738, 0.786 and 0.776, respectively (Table 5) .
ROC curve analysis of MAFLD related indicators. ROC, receiveroperating characteristic; TyG, triglyceride glucose index; TyG-WHtR, triglyceride glucose-waist-to-height ratio; TyG-WC, triglyceride glucose-waist circumference index; TyG-BMI: triglyceride glucose-body mass index; HOMA-IR, homeostasis model assessment of insulin resistance; QUICKI, quantitative insulin sensitivity check index.; FPG, fasting plasma glucose; TG, triglyceride.
Discussion
MAFLD is a prevalent and widely neglected type of chronic liver disease, with a high mortality rate20. IR was recognized as a driver of MAFLD pathogenesis21,22. In the physiological conditions, insulin regulates glucose and lipid metabolism by binding to target receptors in liver, muscle or adipose tissue, inhibiting gluconeogenesis and promoting lipid synthesis. IR impairs the insulin signaling pathway and reduces sensitivity of tissues to insulin, causing disorders of glucose and lipid metabolism, leading to impaired multiorgan functions23. In addition, excessive free fatty acids are transported to various parts of the body including the liver, aggravating ectopic fatty deposits in the liver and leading to further development of IR24,25. Therefore, it is crucial for early detection of patients who are at high risk of MAFLD to provide adequate early treatment to delay disease progression and prevent further deterioration into cirrhosis or even hepatic cancer. It is also necessary and essential to find a noninvasive, convenient, and rapid test for epidemiologic investigations, especially on a larger scale, to detect the presence or absence of MAFLD.
TyG was initially used as a marker of IR in normal individuals16. TyG index can be calculated from simple measurements of fasting glucose and triglycerides, which are also fundamental mechanisms in the pathogenesis of MAFLD. Thus TyG index can accurately predict the prevalence of MAFLD. Parameters such as TyG-WHtR, TyG-WC and TyG-BMI are also associated with waist circumference, height or body mass index, which can depict the medical profile of the patient to predict the potential of MAFLD. It has been found and confirmed in several studies:
A meta-analysis of 20 studies with 165,725 participants with MAFLD illustrated that TyG had the highest AUC value for the prediction of IR, and the diagnosis of MAFLD with the sensitivity of 0.73 (95%CI: 0.69–0.76), the specificity of 0.67 (95%CI: 0.65–0.70), and the AUC of 0.75 (95%CI: 0.71–0.79)26. Sheng G et al. measured and calculated 15 indicators for obesity or lipid, including TyG index and related indices, and found that the most superior parameters in the prediction of NAFLD were TyG and its related indices27. TyG index and related parameters can be used as potential biomarkers for monitoring the presence of NAFLD in children with obesity, as suggested in a study by Chang PS et al.28. Wang R et al.29 concluded that TyG and the risk of NAFLD were positively associated among general population, which was confirmed by a cohort study. Malek M et al. explored that the largest AUC in identifying NAFLD from type 2 diabetic patients was TyG-WHtR (0.783, 95% CI: 0.714–0.842)30. However, in our study, TyG-BMI showed the largest AUC in defining MAFLD (0.825, 95% CI: 0.795–0.857), which was different from the findings of Malek M et al. Possible reasons for this may be: The different subjects of the two studies. While the current study was aimed at nondiabetic American cohort, the above-mentioned study was carried out on Iranian individuals with type 2 diabetes mellitus. Moreover, the criteria for diagnosing MAFLD were different, median CAP value ≥ 274 dB/m was defined as MAFLD in this study, while the other used B-mode ultrasound to define it. In addition, the occurrence of MAFLD varies in sex, different ages, races and dietary habits.
However, current studies have not focused on the relationship between MAFLD prevalence and TyG related parameters in nondiabetic populations. This cross-sectional study of 945 nondiabetic individuals from the 2017–2020 NHANES survey looked at the relationship between TyG related parameters and MAFLD prevalence. This is the first time to explore the relationship that exists between TyG related parameters and the incidence of MAFLD among nondiabetic individuals recruited from the general population. Our study found that TyG index, together with TyG-WHtR, TyG-WC, and TyG-BMI, could accurately identify the presence of MAFLD. This method, which is simple, noninvasive, and independent of other procedures, is superior to more complex scores for identifying MAFLD in nondiabetic patients, makes it possible to provide an easy-to-use alternative method for the diagnosis of MAFLD in nondiabetic individuals in practice and in large-scale epidemiological investigations.
Based on our results, we found an independent positive correlation between TyG related parameters and the incidence of MAFLD in a nondiabetic population. In the RCS curves, after controlling for potential confounders, there was a linear relationship between TyG, TyG-WC and MAFLD (non-linearity: P = 0.542, 0.606), whereas TyG-WHtR and TyG-BMI showed a nonlinear relationship with it (non-linearity: P = 0.03, 0.015). In subgroup analysis, TyG related parameters were found to be positively correlated with MAFLD in different subgroups. The ROC curves analyzing these parameters revealed that the AUC for TyG related parameters was greater than that for fasting glucose and triglycerides, with TyG-BMI having the largest AUC of 0.825; the highest accuracy of 0.776. The formula for TyG-BMI makes it reasonable to infer that the higher a person’s BMI, the higher the TyG-BMI. It may seem that TyG-BMI is not an ideal predictor of MAFLD. However, in the subgroup analyses of both lean and non-lean individuals, we found that TyG-BMI was positively associated with the risk of developing MAFLD. That is, among lean individuals with MAFLD, the effects of elevated TyG probably surpass the effects of reduced BMI. IR induced by excessive accumulation of visceral fat may play a more significant role in the development of MAFLD. Therefore, TyG-BMI can better assess the occurrence of MAFLD. In addition, our study found that TyG-WC had the strongest sensitivity of 0.791, which could be attributed to the fact that waist circumference is a better indicator of the volume of abdominal visceral adipose tissue than BMI. These results suggest that TyG related parameters were straightforward and easy to calculate as MAFLD associated markers.
Most previous studies have shown a positive correlation between TyG related parameters and the occurrence of MAFLD31,32, which is consistent with our findings. However, previous studies have not examined the nonlinear association between them and their diagnostic efficacy of MAFLD in nondiabetic populations. Nevertheless, caution is needed in interpreting this finding in this study due to the limited sample size of our survey. It is necessary to conduct prospective cohort studies to validate this finding.
Our study has limitations as well. First, it can only explain the correlation between TyG related parameters and MAFLD owing to the nature of cross-sectional study. So it is important to confirm the causal connection between the two through further longitudinal studies, which should encourage more large prospective cohort studies. Second, this study diagnosed hepatic steatosis on the basis of imaging (FibroScan®) instead of using liver biopsy, which represents the gold standard in histopathology. When it comes to the diagnosis of hepatic steatosis, VCTE has been shown with greater accuracy than ultrasound33,34, but it is still inferior to liver biopsy. Third, this study was limited to nondiabetic U.S. adults. Whether these findings apply to other populations is unclear. Although we included studies with multifactorial analyses, some covariates could not be measured or evaluated in observational studies that might be subject to residual confounding35.
Conclusion
This cross-sectional analysis using NHANES 2017–2020 data of 945 nondiabetic US individuals found a remarkable correlation among elevated TyG parameters and the presence of MAFLD. Early detection and intervention guided by the TyG index may assist in the prevention and management of MAFLD in nondiabetic population, ultimately enhances the outcomes of patients and reduces the burden of disease.
Data availability
NHANES data used in this work are publicly available. All raw data are available on the NHANES website (https://www.cdc.gov/nchs/nhanes/).
Abbreviations
- MAFLD:
-
Metabolic dysfunction-associated fatty liver disease
- NAFLD:
-
Nonalcoholic fatty liver disease
- TyG:
-
Triglyceride glucose
- TyG-WHtR:
-
Triglyceride glucose-waist-to-height ratio
- TyG-WC:
-
Triglyceride glucose-waist circumference index
- TyG-BMI:
-
Triglyceride glucose-body mass index
- CAP:
-
Controlled attenuation parameter
- VCTE:
-
Vibration controlled transient elastography
- RCSs:
-
Restricted cubic spline
- ROC:
-
Receiver operating characteristic curve
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- QUICKI:
-
Quantitative insulin sensitivity check index
- NHANES:
-
the National Health and Nutrition Examination Survey
- NCHS:
-
National Center for Health Statistics
- LSM:
-
Liver stiffness measurement
- ORs:
-
Odds ratios
- CIs:
-
Confidence intervals
References
Eslam, M. et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J. Hepatol. 73(1), 202–209 (2020).
Eslam, M. et al. Defining paediatric metabolic (dysfunction)-associated fatty liver disease: an international expert consensus statement. Lancet Gastroenterol. Hepatol. 6(10), 864–873 (2021).
Powell, E. E., Wong, V. W. & Rinella, M. Non-alcoholic fatty liver disease. Lancet 397, 2212–2224 (2021).
Méndez-Sánchez, N. et al. Global multi-stakeholder endorsement of the MAFLD definition. Lancet Gastroenterol. Hepatol. 7, 388–390 (2022).
Mikolasevic, I. et al. Transient elastography (FibroScan(®)) with controlled attenuation parameter in the assessment of liver steatosis and fibrosis in patients with nonalcoholic fatty liver disease—where do we stand? World J. Gastroenterol.22, 7236–7251 (2016).
Eddowes, P. J. et al. Accuracy of FibroScan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology 156, 1717–1730 (2019).
Watt, M. J., Miotto, P. M., De Nardo, W. & Montgomery, M. K. The liver as an endocrine organ-linking NAFLD and insulin resistance. Endocr. Rev. 40, 1367–1393 (2019).
Tao, L. C., Xu, J. N., Wang, T. T., Hua, F. & Li, J. J. Triglyceride glucose index as a marker in cardiovascular diseases: landscape and limitations. Cardiovasc. Diabetol. 21, 68 (2022).
Wang, X. et al. Association between the triglyceride-glucose index and severity of coronary artery disease. Cardiovasc. Diabetol. 21, 168 (2022).
Hirschler, V. et al. Ability of TyG index as a marker of insulin resistance in Argentinean school children. Front. Pediatr. 10, 885242 (2022).
Li, X. et al. Triglyceride glucose index and the risk of heart failure: evidence from two large cohorts and a mendelian randomization analysis. Cardiovasc. Diabetol. 21, 229 (2022).
Alizargar, J., Bai, C. H., Hsieh, N. C. & Wu, S. V. Use of the triglyceride glucose index (TyG) in cardiovascular disease patients. Cardiovasc. Diabetol. 19, 8 (2020).
De Lédinghen, V. et al. Controlled attenuation parameter for the diagnosis of steatosis in non-alcoholic fatty liver disease. J. Gastroenterol. Hepatol. 31, 848–855 (2016).
Siddiqui, M. S. et al. Vibration-controlled transient elastography to assess fibrosis and steatosis in patients with nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 17, 156–163 (2019).
Karlas, T. et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J. Hepatol. 66, 1022–1030 (2017).
Simental-Mendía, L. E., Rodríguez-Morán, M. & Guerrero-Romero, F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab. Syndr. Relat. Disord. 6, 299–304 (2008).
Guerrero-Romero, F. et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic hyperinsulinemic clamp. J. Clin. Endocrinol. Metab. 95, 3347–3351 (2010).
Addendum 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes Care. 44, 2182 (2021).
Farrar, D. et al. Association between hyperglycaemia and adverse perinatal outcomes in south Asian and white British women: analysis of data from the born in Bradford cohort. Lancet Diabetes Endocrinol. 3, 795–804 (2015).
Younossi, Z. & Henry, L. Contribution of alcoholic and nonalcoholic fatty liver disease to the burden of liver-related morbidity and mortality. Gastroenterology 150, 1778–1785 (2016).
Lee, S. H., Park, S. Y. & Choi, C. S. Insulin resistance: from mechanisms to therapeutic strategies. Diabetes Metab. J. 46, 15–37 (2022).
Samuel, V. T. & Shulman, G. I. Mechanisms for insulin resistance: common threads and missing links. Cell 148, 852–871 (2012).
Smith, G. I. et al. Insulin resistance drives hepatic de novo lipogenesis in nonalcoholic fatty liver disease. J. Clin. Invest. 130, 1453–1460 (2020).
Guerra, S., Mocciaro, G. & Gastaldelli, A. Adipose tissue insulin resistance and lipidome alterations as the characterizing factors of non-alcoholic steatohepatitis. Eur. J. Clin. Invest. 52, e13695 (2022).
Samuel, V. T. & Shulman, G. I. Nonalcoholic fatty liver disease as a nexus of metabolic and hepatic diseases. Cell. Metab. 27, 22–41 (2018).
Wang, J. et al. The diagnostic and prognostic value of the triglyceride glucose index in metabolic dysfunction-associated fatty liver disease (MAFLD): a systematic review and meta-analysis. Nutrients 14, 4969 (2022).
Sheng, G. et al. The usefulness of obesity and lipid-related indices to predict the presence of non-alcoholic fatty liver disease. Lipids Health Dis. 20(1), 134 (2021).
Chang, P. S., Chang, P. F. & Lin, Y. C. Usefulness of the triglyceride glucose index to predict nonalcoholic fatty liver disease in children with obesity. J. Pediatr. 255, 260–261 (2023).
Wang, R., Dai, L., Zhong, Y. & Xie, G. Usefulness of the triglyceride glucose-body mass index in evaluating nonalcoholic fatty liver disease: insights from a general population. Lipids Health Dis. 20, 77 (2021).
Malek, M., Khamseh, M. E., Chehrehgosha, H., Nobarani, S. & Alaei-Shahmiri, F. Triglyceride glucose-waist to height ratio: a novel and effective marker for identifying hepatic steatosis in individuals with type 2 diabetes mellitus. Endocrine 74, 538–545 (2021).
Ling, Q. et al. The triglyceride and glucose index and risk of nonalcoholic fatty liver disease: a dose-response meta-analysis. Front. Endocrinol. (Lausanne). 13, 1043169 (2023).
Guo, W. et al. The triglyceride glucose index is associated with the severity of hepatic steatosis and the presence of liver fibrosis in non-alcoholic fatty liver disease: a cross-sectional study in Chinese adults. Lipids Health Dis. 19, 218 (2020).
Castera, L., Friedrich-Rust, M. & Loomba, R. Noninvasive assessment of liver disease in patients with nonalcoholic fatty liver disease. Gastroenterology 156, 1264–1281 (2019).
Newsome, P. N. et al. FibroScan-AST (FAST) score for the non-invasive identification of patients with non-alcoholic steatohepatitis with significant activity and fibrosis: a prospective derivation and global validation study. Lancet Gastroenterol. Hepatol. 5, 362–373 (2020).
Black, N. Why we need observational studies to evaluate the effectiveness of health care. BMJ 312, 1215–1218 (1996).
Acknowledgements
Thanks to all the staff of the Department of Interventional Ultrasound for their support of this study.
Funding
This work was supported by the National Natural Science Foundation of China (82272026); the Research Project Supported by the Shanxi Scholarship Council of China (2022 -193).
Author information
Authors and Affiliations
Contributions
Qian Zhang wrote the manuscript; Liping Liu designed the manuscript; Zhilong Liu, Jiaqi Zhang and Shangjie Yang revised the manuscript; all authors approved the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study protocol for NHANES was approved by the NCHS Research Ethics Review Board. Participants provided completed an informed consent form at enrollment (https://www.cdc.gov/nchs/nhanes/irba98.htm). This study used publicly available de-identified data, therefore informed consent was not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, Q., Liu, Z., Zhang, J. et al. Association between TyG related parameters and metabolic dysfunction associated fatty liver disease among nondiabetic individuals. Sci Rep 15, 4566 (2025). https://doi.org/10.1038/s41598-024-84917-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-84917-9
Keywords
This article is cited by
-
TyG-BMI as a superior predictor of MAFLD and pre-MAFLD in Chinese adults: a cross-sectional study
BMC Gastroenterology (2025)