Abstract
The impact of diabetes on incident cardiovascular disease in relation to the extent of atherosclerotic disease remains unclear. We aimed to investigate major adverse cardiovascular events (MACE) in patients with or without type 2 diabetes (T2DM) presenting with two extremes of atherosclerotic disease, those with angiographically documented minor coronary atherosclerotic lesions and those with symptomatic peripheral artery disease. We included 1238 patients from two prospective, long-term cohort studies. Patients underwent coronary angiography and/or sonography in order to assess the grade of atherosclerosis and were defined as having no signs of Atherosclerosis (n = 332; Group I), minor atherosclerosis (n = 425; Group II) and major atherosclerosis (n = 481; Group III). Cardiovascular events were recorded over a median follow-up period of 7.1 years (Q1 = 3.6 years, Q2 = 7.1 years, Q3 = 11.3 years), covering a total of 9533 patient years. We tested the hypothesis that T2DM infers the same relative risk increase irrespective of the atherosclerosis stage, considering 3-point MACE as the primary endpoint. Incident MACE was reported in 681 patients (51%). MACE occurred more frequently in patients with T2DM than in patients without T2DM (p < 0.001). Further, MACE occurred more frequently in group III (58.1%), than group II (34.1%) or group I (19.1%) (group I vs. group II vs. group III, p < 0.001). In a cox-regression-model, T2DM was a significant predictor of MACE in univariate analyses (HR = 2.43 [1.88–3.14], p < 0.001) and after multivariate adjustment for cardiovascular risk factors, as well as the different grades of atherosclerosis (HR = 1.37 [1.02–1.84], p = 0.034). Also, atherosclerosis grades predicted MACE (HR = 3.19 [2.75–3.70], p < 0.001) in univariate analyses, and also after multivariate adjustment for known cardiovascular risk factors, including T2DM (HR = 1.61 [1.31–1.98], p < 0.001). Finally, when testing for interactions between T2DM and stages of atherosclerosis on MACE we could not find any significant interaction (HR = 1.14 [0.86–1.52], p = 0.364). We conclude that T2DM infers an increased risk for MACE across anatomically and morphologically distinct stages of atherosclerosis.
Similar content being viewed by others
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of morbidity and mortality in patients with type 2 diabetes (T2DM), although therapeutic advances have been achieved over the recent years. Ever since the Finnish EAST-WEST-study1 which reported risk equivalence between T2DM and myocardial infarction (MI), there is a matter of debate to what extent T2DM affects outcome at different stages of atherosclerosis. The risk equivalence concept has been challenged later on, mainly because the atherothrombotic event of an MI turned out more relevant than the simple presence of T2DM without a characterization of the arterial state2,3,4,5,6.
Previously, we have shown that T2DM as well as the presence of peripheral artery disease (PAD) or coronary artery disease (CAD) are predictors of major adverse cardiovascular events (MACE), independent of each other. Patients with both PAD and T2DM are at an exceedingly high risk of cardiovascular events7. Based on these data, we aimed to investigate incident MACE in patients with or without T2DM presenting with two extremes of atherosclerotic disease, namely those with angiographically documented minor coronary atherosclerotic lesions (Group II) and those with a severe manifestation of atherosclerosis, i.e. symptomatic peripheral artery disease (PAD; Group III). Imaging studies were performed in a large, prospective observational study. We tested the hypothesis that T2DM infers the same relative risk increase irrespective of the atherosclerosis stage, considering 3-point MACE as the primary endpoint.
Methods
Study design
We investigated patients from two prospective, long-term cohort studies including (i) patients who underwent coronary angiography for the evaluation of established or suspected stable CAD and (ii) patients with clinically and sonographically proven peripheral artery disease (PAD). Patients with normal coronary angiograms and absence of clinical signs of PAD served as a control group. The study design has been described in detail previously8,9. The primary endpoint of the present study was a composite of cardiovascular death, myocardial infarction, or ischemic stroke (3-point MACE).
Patient populations and group allocation
Patients, all Caucasian ethnicity, were recruited at the Academic Teaching Hospital Feldkirch, Austria, a central European tertiary care center and at the Inselspital, University of Bern, Switzerland.
According to the aim of the study we generated three groups of atherosclerotic disease-stages. Two of our three groups (Group I and II) were referred for evaluation of CAD based on clinical criteria. Coronary angiography was performed with the Judkins technique, as described previously10. Atherosclerotic lesion severity was defined according to the 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization11. Subjects without any signs of coronary atherosclerosis in coronary angiography were allocated to group I and served as control group. Patients with signs of atherosclerosis but without relevant lumen obliteration over > 50% of any coronary vessel were allocated to Group II. Groupe III was conducted of patients with symptomatic PAD Fontain-Stage IIa, IIb and III, according to “2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS)”12. In all patients PAD was sonographically verified.
Excluded from analyses were patients with a relevant CAD (angiographically revealed > 50% lumen narrowing) of any vessel and PAD patients Fontain-Stage I and patients with media-sclerosis, diagnosed with ABI (ancel-brachial index)13.
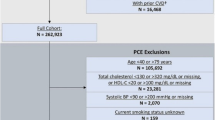
In total, data from 1,238 patients were analyzed. Group I consisted of 332 subjects, Group II of 425 patients, and Group III of 481 patients. The inclusion criteria and group allocation is shown in Fig. 1. The follow-up period is reported as the median with interquartile range (IQR), where Q1 represents the 25th percentile, Q2 the median (50th percentile), and Q3 the 75th percentile.
Study procedures
Baseline analyses included height and weight as well as waist and hip circumferences. Common cardiovascular risk factors were recorded (history of smoking and current smoking, hypertension, established T2DM) from a standardized interview. Systolic and diastolic blood pressures were measured by Riva-Rocci method under resting conditions in sitting position at the day of hospital admission. Hypertension was defined according to the 2023 European Society of Cardiology (ESC)/ESH guidelines14. T2DM was diagnosed according to ADA clinical practice recommendations15. The study was designed as a two-center (Feldkirch, A; Bern, CH), prospective cohort study. During the follow-up period, we recorded cardiovascular events and all-cause death. Date and cause of death were collected annually using a national register (Statistik Austria, Vienna, Austria) and the Insel Data Science Center (Bern, Switzerland), hospital registries and telephone contacts. Standardized interviews were performed at 2-year intervals to assess non-fatal events. Cardiovascular death (fatal myocardial infarction, sudden cardiac death, mortality from congestive heart failure due to CAD, and fatal ischemic stroke), non-fatal myocardial infarction, non-fatal ischemic stroke and limb amputation were recorded.
Laboratory analyses
Laboratory measurements were performed from fresh serum samples, as described previously8,16. Serum levels of C reactive protein, plasma glucose triglycerides, total cholesterol, low density lipoprotein (LDL) cholesterol and high-density lipoprotein (HDL) cholesterol were measured with a Cobas Integra 800 (Roche, Basel, Switzerland). Hemoglobin A1c (HbA1c) was determined on a Menarini-Arkray KDK HA 8160 (Arkray KDK, Kyoto, Japan) by high-performance liquid chromatography. Creatinine was measured by a kinetic Jaffe method (Roche, Switzerland) using a Hitachi 717 or 911 or a Cobas Integra 800 (Roche). The Chronic Kidney Disease Epidemiology Collaboration creatinine equation was applied to estimate the glomerular filtration rate (eGFR)17.
Statistical analyses
Analyses were performed considering prevalent atherosclerosis status within the three groups (Group I, Group II, Group III) overall, and stratified by diabetes status (T2DM; NoT2DM). Between group differences of baseline data were tested for statistical significance with χ2 and Mann-Whitney U tests for categorical and continuous variables as appropriate. Event-free survival was estimated by an actuarial approach. Pairwise comparisons of event-free survival between patient groups were done with the Wilcoxon-Gehan statistic. HRs for the incidence of first cardiovascular events were derived from Cox regression analysis. Results from Cox regression analysis were obtained both univariately and after multivariate adjustment for covariates that may potentially affect cardiovascular outcomes. As such, we included age, sex, smoking, (including history of smoking and current smoking), arterial hypertension, LDL cholesterol, HDL cholesterol and body-mass-index (BMI). Potential interactions between T2DM and stages of atherosclerosis were tested for statistical significance by including interaction terms T2DM x atherosclerosis stage into the regression models. Results are given as mean (SD) if not denoted otherwise. All statistical analyses were performed with the software package IBM SPSS Statistics Version 28.0.0.0 for Windows (SPSS).
Results
Baseline data (Tables 1 and 2)
At baseline 332 patients were included into Group I, 425 patients to Group II and 481 patients to Group III. Mean age of Group I was 60.5 years, 65.3 years in the Group II and 67.2 years in Group III (p < 0,001). The prevalence of T2DM significantly increased (p < 0.001) from those in Group I (20.5%) over those in Group II (24.2%) to those in Group III (44.5%). Patients in Group III were more likely to have a history of smoking (n = 371, p < 0.001) and a large majority of the patients had a history of hypertension (n = 432 (89.8%), p < 0.001). Body mass index (BMI) was highest in group I (28 kg/m², p = 0.002).
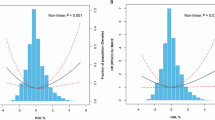
Primary endpoint (Fig. 2a,b)
The endpoint of MACE was reported in 681 (51%) patients over a median follow-up period of 7.1 years (Q1 = 3.6 years, Q2 = 7.1 years, Q3 = 11.3 years). The study thus covered a total of 9533 patient years. Figure 2 shows the incidence of MACE in a Kaplan-Meier survival analysis. MACE occurred more frequently in patients with diabetes than in patients without diabetes (Fig. 2a; p < 0.001). Also, MACE occurred more frequently in Group III (58.1%), than in those in Group II (34.1%) or group I (19.1%), with statistically significant differences between the 3 groups (Group I vs. Group II vs. Group III, p < 0.001; Fig. 2b).
Analyses considering both diabetes status as well as grades of atherosclerosis (Figs. 3, 4 and 5)
Hazard ratios (HRs) for diabetes impacting major adverse cardiac events (MACE) within the entire study cohort are presented as follows: in a univariate analysis, HR = 2.43 [95% CI 1.88–3.14], p < 0.001; and after adjustment for multiple variables including age, sex, LDL, HDL, BMI, smoking status, hypertension, and the degree of atherosclerosis (Group I, Group II and Group III) in a multivariate analysis, HR = 1.37 [95% CI 1.02–1.84], p = 0.034.
T2DM significantly increased the risk of MACE both among patients in Group I (78.0% vs. 67.6%; p = 0.023) and Group III (49.4% vs. 32.9%; p < 0.001); in Group I the risk of MACE did not differ between those with T2DM and those who did not have T2DM (88.0% vs. 87.9%; p = 0.663). In patients in Group III who did not have T2DM, the risk of MACE was higher than that of T2DM patients in Group II (p < 0.001) (Fig. 3).
In a cox-regression-model, T2DM was a significant predictor of MACE in univariate analyses (HR = 2.43 [1.88–3.14], p < 0.001) and also after multivariate adjustment for cardiovascular-risk-factors (age, sex, hypertension, smoking, low density lipoprotein (LDL), high density lipoprotein, body-mass-index) and as well after adjustment for the three stages of atherosclerotic disease (Group I, Group II and Group III) (HR = 1.37 [1.02–1.84], p = 0.034) (Fig. 4). Further, we found that our defined atherosclerotic stages predicted MACE (HR = 3.19 [2.75–3.70], p < 0.001) in a univariate analysis, and also after multivariate adjustment for known cardiovascular-risk-factors including T2DM (age, sex, hypertension, smoking, low density lipoprotein (LDL), high density lipoprotein, body-mass-index and the diabetes-state) (HR = 1.61 [1.31–1.98], p < 0.001).
In a cox-regression-model for MACE (Fig. 5) stratified by the three groups, T2DM was no significant predictor for MACE in Group I and Group II univariately (Group I: HR = 1.39 [0.59–3.25], p = 0.451; Group II: HR = 1.34 [0.84–2.13], p = 0.214), and there was a borderline significance in patients Group III (HR = 1.46 [1.01–2.11], p = 0.043, respectively). However, there was a similar trend for risk increase by T2DM along the three grades of atherosclerosis, indicated by respective comparable point estimates of between 1.34 and 1.46 (Fig. 5).
After multivariate adjustment for common cardiovascular risk-factors (age, sex, smoking state, hypertension, low density lipoprotein cholesterol (LDL-C) and high-density-lipoprotein cholesterol, HDL-C and body-mass-index (BMI)) there was no correlation in Group I (aHR = 1.17 [0.48–2.87], p = 0.733) and Group II (aHR = 1.13 [0.70–1.83], p = 0.609), but a trend in patients Group III (aHR = 1.47 [0.99–2.18], p = 0.55), respectively.
When testing for interactions between T2DM and stages of atherosclerosis on MACE we could not find any significant interaction (HR = 1.14 [0.86–1.52], p = 0.364).
Discussion
The present prospective, observational study over a median follow-up period of 7.1 years yielded several new clinically important findings.
First, our data indicate that both prevalent T2DM, as well as prevalent atherosclerosis are mutually independent prognostic factors for incident MACE. Also, we were able to demonstrate that the presence of diabetes remained a significant contributor to the risk of MACE, independent of underlying atherosclerosis-stage. Although the effect of diabetes on MACE was numerically more pronounced in Group I and Group II, as compared to Group III (Fig. 3). Corresponding multivariate analyses (Fig. 5), as well as interaction analyses suggest an independent effect of T2DM. This indicates that the risk of experiencing a MACE is inevitably higher once diabetes is diagnosed, regardless of underlying atherosclerosis-stage. This finding is new, and further prospective studies including morphological data should be encouraged.
Second, we found that patients with prevalent atherosclerosis represent a very high-risk population, which is particularly pronounced in patients with advanced PAD. This is in line with previous findings and has also been reflected in several clinical practice recommendations18,19,20,21. In our study as many as around 60% of patients with PAD Fountain stages 2 or 3 at baseline reached the primary endpoint of MACE during follow-up. Previously we have shown that PAD is a stronger risk factor for future cardiovascular events than T2DM, and that T2DM accelerates atherothrombotic disease and dramatically increases the incidence of cardiovascular events in PAD patients22,23. This confirms a clear need for intensive risk factor management in these patients.
Third, both T2DM as well as the grade of atherosclerosis at baseline predicted MACE. This has been shown previously in populations at various stages of atherosclerosis and different stages of diabetes, such as in a large post-hoc analyses of the EXSCEL trial24 demonstrating increased risk in patients with T2DM depending on the amount of vascular bed involvement25. Results from large clinical trials (e.g. SAVOR-TIMI 5326; LEADER27, IMPROVE-IT28) indicate that diabetes should not be seen as a precursor for atherosclerotic disease, rather that diabetes confers additive cardiovascular risk25. Remarkably, the higher incidence of MACE in patients with T2DM was observed despite of glycaemic control being close to an HbA1c target of 7% at baseline. The prognostic importance of glycaemic control for cardiovascular outcomes has been confirmed by a recent interesting study in diabetic patients following stent-supported angioplasty. The optimally controlled T2DM in this cohort was associated with a favourable cardiovascular outcome, even in patients with advanced atherosclerotic lesions in renal arteries causing renovascular hypertension29.
Our study has several important strengths and limitations. Major strengths are the large sample size, the comprehensive clinical and demographic characterization of study subjects, and a long follow-up period. Also, we used imaging techniques in order to quantify atherosclerosis, rather than solely relying on clinical data. A limitation is that our study is restricted to only two study sites, and therefore our findings may be less applicable to other populations. The diabetes therapy of the study patients was in the hands of the physicians referring patients to our two centers. It represents a limitation of our protocol in that we cannot provide data of glycaemic control. Furthermore, populations of our study differ in terms of site (PAD, CAD) as well as stages of atherosclerosis. However, both atherosclerosis entities are morphologically well defined, minor CAD by angiography and PAD by ultrasonography30,31,32,33.
Conclusions
In summary, we would like to conclude that T2DM infers an increased risk for incident MACE across anatomically and morphologically distinct stages of atherosclerosis.
Data availability
The datasets generated during the current study are available in the VIVIT-Institute repository and from the corresponding author on reasonable request.
Abbreviations
- T2DM:
-
type 2 diabetes mellitus
- ASCVD:
-
atherosclerotic cardiovascular disease
- CAD:
-
coronary artery disease
- noAS:
-
no atherosclerosis
- minAS:
-
minor atherosclerosis
- majAS:
-
major atherosclerosis
- PAD:
-
peripheral artery disease
- HR:
-
hazard ratio
- aHR:
-
adjusted hazard ratio
- MACE:
-
major adverse cardiovascular event
References
Haffner, S. M., Lehto, S., Rönnemaa, T., Pyörälä, K. & Laakso, M. Mortality from Coronary Heart Disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl. J. Med. 339, 229–234 (1998).
Juutilainen, A., Lehto, S., Rönnemaa, T., Pyörälä, K. & Laakso, M. Type 2 diabetes as a coronary heart disease equivalent. Diabetes Care 28, 2901–2907 (2005).
Raggi, P., Cooil, B., Ratti, C., Callister, T. Q. & Budoff, M. Progression of coronary artery calcium and occurrence of myocardial infarction in patients with and without diabetes mellitus. Hypertens. (Dallas Tex. 1979) 46, 238–243 (2005).
Saely, C. H., Aczel, S., Marte, T., Langer, P. & Drexel, H. Cardiovascular complications in type 2 diabetes mellitus depend on the coronary angiographic state rather than on the diabetic state. Diabetologia 47, 145–146 (2004).
Bulugahapitiya, U., Siyambalapitiya, S., Sithole, J. & Idris, I. Is diabetes a coronary risk equivalent? Systematic review and meta-analysis. Diabet. Med. 26, 142–148 (2009).
Pajunen, P. et al. Myocardial infarction in diabetic and non-diabetic persons with and without prior myocardial infarction: the FINAMI Study. Diabetologia 48, 2519–2524 (2005).
Sprenger, L. et al. Type 2 diabetes and the risk of cardiovascular events in peripheral artery disease versus coronary artery disease. BMJ Open. Diabetes Res. Care 9, e002407 (2021).
Drexel, H. et al. Is atherosclerosis in diabetes and impaired fasting glucose driven by elevated LDL cholesterol or by decreased HDL cholesterol? Diabetes Care 28, 101–107 (2005).
Dopheide, J. F., Papac, L., Schindewolf, M., Baumgartner, I. & Drexel, H. Poor attainment of lipid targets in patients with symptomatic peripheral artery disease. J. Clin. Lipidol. 12, 711–717 (2018).
Drexel, H. et al. Relation of the level of high-density lipoprotein subfractions to the presence and extent of coronary artery disease. Am. J. Cardiol. 70, 436–440 (1992).
Lawton, J. S. et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice guidelines. Circulation (2022).
Aboyans, V. et al. 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur. Heart J. 39, 763–816 (2018).
Laurent, S. et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur. Heart J. 27, 2588–2605 (2006).
Mancia(Chairperson, G. et al. 2023 ESH guidelines for the management of arterial hypertension the Task Force for the management of arterial hypertension of the European Society of Hypertension Endorsed by the European Renal Association (ERA) and the International Society of Hypertensi. J. Hypertens. (2023).
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of Medical Care in Diabetes-2018. Diabetes Care. 41, S13–S27 (2018).
Saely, C. H. et al. The metabolic syndrome, insulin resistance, and cardiovascular risk in diabetic and nondiabetic patients. J. Clin. Endocrinol. Metab. 90, 5698–5703 (2005).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150, 604 (2009).
Aday, A. W. & Matsushita, K. Epidemiology of peripheral artery disease and polyvascular disease. Circ. Res. 128, 1818–1832 (2021).
Mach, F. et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur. Heart J. 41, 111–188 (2020).
Grundy, S. M. et al. Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 139 (2019).
Gerhard-Herman, M. D. et al. 2016 AHA/ACC Guideline on the management of patients with Lower Extremity Peripheral Artery Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. Circulation 135 (2017).
Saely, C. H. et al. Type 2 diabetes mellitus is a strong predictor of LDL cholesterol target achievement in patients with peripheral artery disease. J. Diabetes Compl. 34, 107692 (2020).
Saely, C. H. et al. Single and combined effects of peripheral artery disease and of type 2 diabetes mellitus on the risk of cardiovascular events: a prospective cohort study. Atherosclerosis 279, 32–37 (2018).
Holman, R. R. et al. Effects of once-weekly exenatide on cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 377, 1228–1239 (2017).
Gutierrez, J. A., Aday, A. W., Patel, M. R. & Jones, W. S. Polyvascular disease. Circ. Cardiovasc. Interv 12 (2019).
Scirica, B. M. et al. Saxagliptin and Cardiovascular outcomes in patients with type 2 diabetes Mellitus. N. Engl. J. Med. 369, 1317–1326 (2013).
Marso, S. P. et al. Liraglutide and Cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 375, 311–322 (2016).
Cannon, C. P. et al. Ezetimibe added to statin therapy after Acute Coronary syndromes. N. Engl. J. Med. 372, 2387–2397 (2015).
Badacz, R. et al. The maintained glycemic target goal and renal function are associated with cardiovascular and renal outcomes in diabetic patients following stent-supported Angioplasty for Renovascular atherosclerotic disease. J. Pers. Med. 12, 537 (2022).
Nishimura, R. A. et al. 2014 AHA/ACC Guideline for the management of patients with Valvular Heart Disease: executive Summary. Circulation 129, 2440–2492 (2014).
Sibley, R. C. et al. Noninvasive physiologic vascular studies: a guide to diagnosing peripheral arterial disease. RadioGraphics 37, 346–357 (2017).
Gupta, P., Lyons, S. & Hedgire, S. Ultrasound imaging of the arterial system. Cardiovasc. Diagn. Ther. 9, S2–S13 (2019).
Neumann, F-J. et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur. Heart J. 40, 87–165 (2019).
Acknowledgements
The authors are indebted to Iris Baumgartner, MD, Professor of Medicine, former Head, of the Department of Angiology at the Insel Spital Bern, Switzerland for long-term organizational support.
Funding
This work has been supported by the Jubiläumsfonds of the Austrian National Bank (project number 14159). The authors would like to thank Dr. Peter Prast and the Emotion Foundation (Vaduz, Liechtenstein) for providing a generous research grant to the VIVIT-Institute.
Author information
Authors and Affiliations
Contributions
A.M.: data evaluation and statistical analysis, drafting of the manuscriptD.H.: data evaluation and statistical analysisB.L.: data evaluation, drafting of the manuscriptJ.D.: data evaluation, revision of the manuscript for intellectually important contentC. S.: data evaluation, revision of the manuscript for intellectually important C.H.: statistical analysisP.A.: revision of the manuscript for intellectually important contentM.S.: data evaluation and statistical analysisA.F.: data evaluation, revision of the manuscript for intellectually important H.D. conception and design of the study, drafting of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mader, A., Haeberli, D., Larcher, B. et al. Contribution of type 2 diabetes to major adverse cardiovascular events (MACE) in a long-term observational study with different stages of atherosclerosis. Sci Rep 15, 2792 (2025). https://doi.org/10.1038/s41598-024-84985-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-84985-x