Abstract
The impact of bisphosphonates on cardiac arrhythmia has always been controversial. We aimed to evaluate the risk of bisphosphonates (BPs) on arrhythmia and to characterize the main features of BP-induced arrhythmia by data mining the FDA adverse event Reporting System (FAERS). From the first quarter of 2016 to the second quarter of 2022, reports for BP-related cardiac arrhythmia adverse event (AE) from FAERS database were analyzed in this study. The reporting odds ratio (ROR) and information components (IC) were used to identify disproportionate reporting of BP-related cardiac arrhythmias. We identified a total of 2377 BP-related cardiac arrhythmias cases which appeared to influence more women (61.88%) than men (28.02%), with a median age of 70 (interquartile range [IQR] 59–78) years. Compared with the full database, BPs were detected with pharmacovigilance of cardiac arrhythmias (ROR025 = 1.43, [1.39–1.47]). All studied bisphosphonates except ibandronate sodium and clodronate disodium were correlated with the reporting frequency of cardiac arrhythmia (HLGT), with ROR ranging from 1.28 with pamidronate disodium to 11.08 with etidronate disodium. The spectrum of arrhythmias induced by BPs differed among therapeutic regimens. There were significant differences in the onset time among BP regimens. Bisphosphonates use is associated with adverse cardiac arrhythmias, with the exception of ibandronate sodium and clodronate disodium. Our data support differential effects of BPs on cardiac arrhythmias.
Similar content being viewed by others
Introduction
Bisphosphonates (BPs) are a class of synthetic compounds that reduce bone resorption by inhibiting osteoclast activity, which are widely used for the treatment of various bone and joint diseases, such as osteoporosis, Paget’s disease of bone and malignancy-associated bone disease1,2,3,4,5. Development of BPs has reached their third generation, including clodronate disodium, etidronate disodium, zoledronic acid, risedronate sodium, ibandronate sodium, alendronate sodium and pamidronate disodium.
The proarrhythmic effect of BPs is a significant concern in using them, which showing conflicting results in previous studies6,7,8,9,10,11,12,13,14,15. The definitive confirmation of association between bisphosphonates and cardiac arrhythmia has since been strongly debated because some6,7,8,9,13,14 but not all studies have identified a similar risk10,11,12,15. A large population cohort study showed that zoledronic acid users had a higher risk of arrhythmias (adjusted hazard ratio 1.18 [1.06–1.31]) and atrial fibrillation (adjusted hazard ratio 1.18 [1.05–1.32]) compared with untreated subjects8, while another Danish cohort study revealed a reduced risk of cardiac arrhythmia [0.61; 0.41 to 0.89] and atrial fibrillation [0.67; 0.55 to 0.81] associated with oral BP use10. A meta-analysis including 9 randomized controlled trials (RCTs) with zoledronic acid observed elevated risk of arrhythmia and atrial fibrillation in women with primary osteoporosis6, which contradicted the results of another meta-analysis15. Furthermore, it is unclear if proarrhythmic effects of bisphosphonates are class-specific or related to individual drugs. The two recent pharmacovigilance studies did not comprehensively and systematically describe the effects of different BPs on different arrhythmias: both studies included only two kinds of BP, and one study was limited by grouping six arrhythmias as a single outcome, making it impossible to determine the differences of these BPs on different arrhythmias, while the other study included only three arrhythmias7,16. Moreover, the outlined relationship between BPs and arrhythmias, potential signal spectrum, factors associated with death, and clinical information of BP–related arrhythmias are still unclear.
Given the increasing use of BPs in real world, and the conflicting risk of arrhythmia induced by BPs, we conducted a systematic review to investigate arrhythmias in different BP therapies, leveraging real-world pharmacovigilance data from the FDA Adverse Event Reporting System (FAERS) database.
Methods
Data source
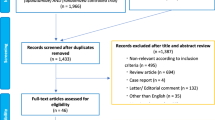
To explore the relationship between BPs and cardiac arrhythmias, we used the FAERS database containing spontaneous adverse event reports from the first quarter of 2016 to the second quarter of 2022 to perform the pharmacovigilance study. The bisphosphonates in the study included zoledronic acid, risedronate sodium, ibandronate sodium, alendronate sodium, pamidronate disodium, clodronate disodium and etidronate disodium. Open Vigil FDA, an application programming interface (API), was a pharmacovigilance tool adapted to extract FAERS data by removing duplicate reports or reports with missing data1714. We used OpenVigil 2.1 to query the FAERS database and retrieve reports on the generic name of BPs (“zoledronic acid"+“risedronate sodium”+“ibandronate sodium”+“alendronate sodium”+“pamidronate disodium”+“clodronate disodium”+"etidronate disodium”) from January 1, 2016 to June 30, 2022.
Definition of AEs
Based on Medical Dictionary for Regulatory Activities (MedDRA), the high-level group term (HLGT) we investigated was “Cardiac arrhythmias (10007521).” The complete list of preferred terms (PTs) within cardiac arrhythmias can be accessed in supplemental table S1. The above PT level adverse events (AEs) were grouped into the following four High Level Terms (HLTs): “Ventricular arrhythmias and cardiac arrest [10047283],” “Cardiac conduction disorders [10000032],” “Rate and rhythm disorders NEC [10037908],” and “Supraventricular arrhythmias [10042600].” Moreover, we collected the following demographic features of AE cases: patient’s characteristics (age, gender, country of origin), drug information (drug indication, receipt date, concurrent medications, treatment start and end date), and arrhythmia characteristics (seriousness, final outcome).
Statistical analysis
Descriptive analysis was performed for the clinical characteristics of BPs-associated cardiac arrhythmias. We used Chi-square (Chi2) tests to compare categorical variables between the fatal and non-fatal groups. To compare the onset time of BP-associated arrhythmias, we used t-test and nonparametric test (Kruskal Wallis test). Disproportionality analysis was performed to identify potential safety signals for BP-associated arrhythmias by using reporting odds ratio (ROR) and information component (IC)18. The calculation formulas for IC and ROR were as follows:
Nobserved represented the count of observed records for the target drug AEs, Nexpected was the anticipated count of such records. Ndrug was the total count of records for the target drug irrespective of AEs. Nevent was the total count of records for the specific AEs, regardless of the drug involved. Lastly, Ntotal signified the overall count of records in the entire database. If there were not less than three reports and one algorithm was positive, the arrhythmia AE was considered to be associated with BP treatment. In this study, all statistical analyses were conducted using SPSS 24.0, and p values < 0.05 was considered statistically significant.
Results
Descriptive analysis
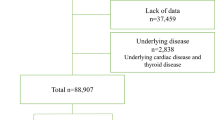
From the first quarter of 2016 to the second quarter of 2022, the FAERS database recorded 91,588 bisphosphonate-related AEs and 164,227 cases associated with cardiac arrhythmias. We identified 2377 reports of bisphosphonate-related cardiac arrhythmias and presented the clinical characteristics of cases in Table 1. Among individual areas, the North America reported the highest number of arrhythmia AEs with 52.25% (1242/2377). The median age of patients was 70 years (interquartile range [IQR] 59–78), and 61.88% of BP recipients were female. Zoledronic acid (1020 reports, 42.91%), alendronate sodium (823 reports, 34.62%), and risedronate sodium (352 reports, 14.81%) accounted for a higher proportion of events. As shown in Table 1, there was no significant difference in patient age, sex, reporter, region, BP regimen between fatal and nonfatal reports.
Signal values associated with different bisphosphonate regimens
The signal values and the correlation between bisphosphonates and arrhythmias were shown in Table S1 and Fig. 1. All studied bisphosphonates except ibandronate sodium and clodronate disodium were significantly associated with the reporting frequency of cardiac arrhythmia (HLGT), with ROR ranging from 1.28 with pamidronate disodium to 11.08 with etidronate disodium (Fig. 1). Regarding four specific arrhythmias in HLT level, the bisphosphonates with the highest ROR were etidronate disodium in cardiac conduction disorders (ROR025 = 66.5) and supraventricular arrhythmias (ROR025 = 26.17), risedronate sodium in rate and rhythm disorders (ROR025 = 1.54), and pamidronate disodium in ventricular arrhythmias (ROR025 = 1.42). Ibandronate sodium presented no signal in the above four specific arrhythmias respectively.
The signal spectrum of cardiac arrhythmias differs in bisphosphonate strategies
The arrhythmia signal spectra of different bisphosphonate therapies were shown in Fig. 2. Zoledronic acid presented a broadest spectrum of cardiac arrhythmias AEs, with 9 PTs detected as positive signals, ranging from supraventricular tachycardia (IC 025 = 0.14) to atrial fibrillation (IC 025 = 1.17). There were 6 PTs as signals associated with risedronate sodium, with signal values ranging from IC 025 = 0.02 (tachycardia) to IC 025 = 1.68 (supraventricular extrasystoles). However, the drug with the least PTs was ibandronate sodium, with no signal detected, followed by pamidronate disodium, with one signal detected. Atrial fibrillation was the most overlapping PTs, which was found significantly associated with zoledronic acid, risedronate sodium, alendronate sodium and etidronate disodium. Bundle branch block left and atrial fibrillation were detected as the strongest two signals in etidronate disodium (IC 025 = 5.56; IC 025 = 4.36). No BPs showed positive signals in cardiac flutter, bradycardia, extrasystoles, sinus bradycardia, cardiac arrest, ventricular tachycardia and ventricular fibrillation.
Time to onset of BP-associated cardiac arrhythmia adverse effects
The onset time of BP-associated arrhythmia was shown in Table S2 and Fig. 3. According to all BPs, the median time to onset (TTO) is 71 days (IQR 2–444 days). There were significant differences in the reported TTO of arrhythmias among BP regimens (p < 0.001). The median TTO was 42 days for zoledronic acid (IQR 1–355), 38 days for risedronate sodium (IQR 10.25–873.75), 251 days for ibandronate sodium (IQR 23.5–649.0), 145 days for alendronate sodium (IQR 13–741), 92 days for pamidronate disodium (IQR 38–356), and 59 days for clodronate disodium (IQR 16–122), respectively.
Discussion
This study is the first pharmacovigilance study to comprehensively evaluate the cardiac arrhythmia AEs associated with BPs based on the FAERS database, and to explore the clinical characteristics of BP-induced arrhythmia AEs.
Our research detected significant signals between cardiac arrhythmia and all BPs except ibandronate sodium and clodronate disodium, with ROR ranging from 1.28 with pamidronate disodium to 11.08 with etidronate disodium. Notably, the risk signals of BP are different, with high-risk signal of arrhythmia detected in etidronate disodium, no risk of signal of arrhythmia detected in ibandronate sodium and clodronate disodium, and modest risk signal of arrhythmia detected in other BPs. The risk of cardiac arrhythmia of BPs varied in different literatures, some of which showed a positive arrhythmia risk of BPs6,8,13,14,16,19,20,21, while others showed the opposite10,11,12,15,22,23. In HORIZON clinical trial, zoledronate versus placebo presented an increased risk of arrhythmia and AF (6.9% vs. 5.3%, p = 0.003; 1.3% vs. 0.5%, p < 0.001)20. Moreover, a case-control study from the United States showed that the ever-users of bisphosphonates had a higher risk of incident atrial fibrillation compared to never-users (OR 1.86, 95% CI 1.09–3.15)21. Interestingly, the risk for AF was inversely correlated with adherence to BPs22, which was supported by another research23. Two large population cohort studies respectively revealed the opposite risk of arrhythmia and atrial fibrillation for BPs8,10. A meta-analysis re-assessing all the RCTs employing alendronate found no increased risk of AF for this drug in any single trial nor in the pooled analysis15. Following the study, the meta-analysis including 9 RCTs with zoledronic acid observed elevated risk of arrhythmias and atrial fibrillation in women with primary osteoporosis6. Given the conflicting results presented by RCTs and observational studies, previous research recommended avoiding the prescription of BPs in patients with a history of atrial fibrillation24,25; however, the varying signal strengths of BPs observed in our study may not only provide more options for such patients, such as choosing ibandronate sodium or clodronate disodium with negative arrhythmia signals, and avoiding etidronate disodium with a strong positive arrhythmia signal, but also favor clinicians to spontaneously report arrhythmia incidents through heightened awareness and enhanced development of pharmacovigilance frameworks. The mechanisms that might explicate such a relation remained unclear but it had been suggested that hypocalcemia and related secondary hyperparathyroidism might be potential factors for triggering arrhythmias26. Supporting the possibility that the risk of arrhythmia may not be uniform across different BPs may be due to difference in predominant use27, affinity for bone and powerful inhibition of resorption28, but may not be attributed to the nitrogen containing moiety23. Both our study and previous research had shown that BPs used primarily for neoplastic indications or rare bone disorders presented a lower risk of arrhythmia compared to those used for non-neoplastic indications27. Although the benefits of BP use may outweigh the modest increased risk of incident arrhythmia for most patients, the findings of this study require further exploration and discovery of these causal relationships in clinical studies to further validate their value.
Atrial fibrillation (AF) induced by zoledronic acid, risedronate sodium, alendronate sodium and etidronate disodium was over-reported, but only the signal intensity of etidronate disodium was strong; ibandronate sodium and pamidronate disodium did not present a significant signal value. This was the first comprehensive study to compare the effects of different BPs on atrial fibrillation, and to find that the risk of atrial fibrillation varied among different BPs. The previous studies showed that either all BPs in the report were associated with atrial fibrillation13,14,19, or none of the BPs are associated10,11,12. Our study shows that zoledronic acid, risedronate, and alendronate indicated a similar risk of atrial fibrillation, which is consistent with previous clinical data for the three BPs indicating no significant differences from placebo in overall incidence of AF AEs29. The no signal value of ibandronate sodium and pamidronate disodium in AF found in our study, which was supported by a meta-analysis of the pivotal RCTs for ibandronate30 and a pharmaco-epidemiological study detecting a lower risk of severe AF following pamidronate acid compared to zoledronic acid use27. Atrial fibrillation and serious atrial fibrillation events with ibandronate were 0.8% and 0.4% in previous study30, which is lower than that reported in the study on zoledronic acid (2.4% and 1.3%, respectively)20. Ibandronate and pamidronate were deemed to be safe overall in AF, which required further research and certification. Several mechanisms were postulated for the increased risk of AF with BPs, including calcium shifts after the infusion, cytokine release, and deposition of bisphosphonates in myocardial tissue31,32 which needed further validation in future studies.
Our study demonstrated that BP-related arrhythmias occurred early after BP initiation, with significant differences among different BP therapies (p < 0.001). The median TTO of BP-related arrhythmias was 71 (IQR 2- 444) days, and most known cases (406/969, 41.49%) occurred within the first thirty days after the initiation of BP therapy, which indicated the significance of early cardiac monitoring within the higher-risk time window of 30 days. It is important to recognize the difference in onset time of arrhythmias among different BP regimens, providing evidence for effective interventions in affected population.
This study involves several limitations that should be acknowledged. Firstly, the FAERS database has some inherent limitations, including data duplication, missing data, and reporting bias (e.g., selective reporting, inevitable underreporting, and false or inaccurate reporting), which can lead to disproportionate analysis inaccuracies, confuse signal detection work, and result in incomplete description of drug safety. Additionally, as a spontaneous reporting system, the FAERS database does not provide detailed clinical information. Secondly, it is difficult to control for confounding factors, such as medication history for patients, concomitant diseases status, potential drug interactions, the use of multiple drug combinations and other health conditions, all of which may influence the risk of arrhythmias. Thirdly, data mining using Bayesian analysis and non-proportional analysis can only indicate a statistical association between adverse reactions and drugs rather than a causal relationship. The slight increase in ROR does not indicate a risk of AEs in clinical practice, which may be relevant. Therefore, these values only provide safety signals, not real risks, and require further confirmation. Moreover, future pharmacovigilance efforts need to explore the use of advanced artificial intelligence methods, such as employing machine learning33,34,35 and deep learning models35,36 to identify patterns in adverse event data, while also utilizing natural language processing to extract insights from unstructured text fields in the FAERS database.
Conclusion
We reviewed BP-associated arrhythmia AEs from the FAERS database to explore the safety profile of BPs for arrhythmia and optimize their use among individual patients. Our study showed that BPs presented different spectrum and risk of positive arrhythmia signals, with high-risk signal of arrhythmia detected in etidronate disodium, no risk of signal of arrhythmia detected in ibandronate sodium and clodronate disodium, and modest risk signal of arrhythmia detected in other BPs. Our study is practical for clinicians to enhance the management of BP-related arrhythmia AE signals and improve BPs treatment safety. Due to the spontaneous nature of the FAERS reporting system, which includes omissions, misreporting, and incomplete reports, this study could not definitively infer a causal relationship between BPs and arrhythmias. Therefore, further clinical research is needed in the future to validate this association.
Data availability
The study used data from the FDA Adverse Event Reporting System (FAERS) database. The raw data supporting the conclusions of this article will be made available by the corresponding author, without undue reservation.
References
Ralston, S. H. et al. Diagnosis and management of Paget’s disease of bone in adults: A clinical guideline. J. Bone Min. Res. 34, 579–604. https://doi.org/10.1002/jbmr.3657 (2019).
Gopinath, V. & Osteoporosis Med. Clin. North. Am. 107, 213–225, doi:https://doi.org/10.1016/j.mcna.2022.10.013 (2023).
Tang, C. H. & Osteoporosis From molecular mechanisms to therapies 3.0. Int. J. Mol. Sci. 22 https://doi.org/10.3390/ijms222312725 (2021).
Reid, I. R. & McClung, M. R. Osteopenia: a key target for fracture prevention. Lancet Diabetes Endocrinol. 12, 856–864. https://doi.org/10.1016/S2213-8587(24)00225-0 (2024).
Almuradova, E. & Cicin, I. Cancer-related hypercalcemia and potential treatments. Front. Endocrinol. (Lausanne). 14, 1039490. https://doi.org/10.3389/fendo.2023.1039490 (2023).
Liu, S. et al. Cardiovascular safety of Zoledronic acid in the treatment of primary osteoporosis: A meta-analysis and systematic review. Semin Arthritis Rheum. 64, 152304. https://doi.org/10.1016/j.semarthrit.2023.152304 (2024).
Rodriguez, A. J., Nerlekar, N. & Ebeling, P. R. Cardiac adverse events in bisphosphonate and teriparatide users: an international pharmacovigilance study. Bone 168, 116647. https://doi.org/10.1016/j.bone.2022.116647 (2023).
Rubin, K. H. et al. Cardiovascular and skeletal safety of Zoledronic acid in osteoporosis observational, matched cohort study using Danish and Swedish health registries. Bone 134 https://doi.org/10.1016/j.bone.2020.115296 (2020).
Kirchmayer, U. et al. Bisphosphonates and cardiovascular risk in elderly patients with previous cardiovascular disease: a population-based nested case-control study in Italy. Ther. Adv. Drug Saf. 10, 2042098619838138. https://doi.org/10.1177/2042098619838138 (2019).
Rodriguez, A. J. et al. Oral bisphosphonate use reduces cardiovascular events in a cohort of Danish patients referred for bone mineral density. J. Clin. Endocrinol. Metab. 105 https://doi.org/10.1210/clinem/dgaa481 (2020).
Kim, S. Y., Kim, M. J., Cadarette, S. M. & Solomon, D. H. Bisphosphonates and risk of atrial fibrillation: a meta-analysis. Arthritis Res. Ther. 12, R30. https://doi.org/10.1186/ar2938 (2010).
Mak, A., Cheung, M. W., Ho, R. C., Cheak, A. A. & Lau, C. S. Bisphosphonates and atrial fibrillation: bayesian meta-analyses of randomized controlled trials and observational studies. BMC Musculoskelet. Disord. 10, 113. https://doi.org/10.1186/1471-2474-10-113 (2009).
Sharma, A. et al. Risk of atrial fibrillation with use of oral and intravenous bisphosphonates. Am. J. Cardiol. 113, 1815–1821. https://doi.org/10.1016/j.amjcard.2014.03.008 (2014).
Kim, D. H. et al. Bisphosphonates and risk of cardiovascular events: a meta-analysis. PLoS One. 10, e0122646. https://doi.org/10.1371/journal.pone.0122646 (2015).
Barrett-Connor, E. et al. Alendronate and atrial fibrillation: a meta-analysis of randomized placebo-controlled clinical trials. Osteoporos. Int. 23, 233–245. https://doi.org/10.1007/s00198-011-1546-9 (2011).
Moreland-Head, L. N., Coons, J. C., Seybert, A. L., Gray, M. P. & Kane-Gill, S. L. Use of disproportionality analysis to identify previously unknown drug-Associated causes of cardiac arrhythmias using the food and drug administration adverse event reporting system (FAERS) database. J. Cardiovasc. Pharmacol. Ther. 26, 341–348. https://doi.org/10.1177/1074248420984082 (2021).
Bohm, R. et al. Pharmacovigilance-based drug repurposing: the search for inverse signals via openvigil identifies putative drugs against viral respiratory infections. Br. J. Clin. Pharmacol. 87, 4421–4431. https://doi.org/10.1111/bcp.14868 (2021).
Zhai, Y. et al. Endocrine toxicity of immune checkpoint inhibitors: a real-world study leveraging US food and drug administration adverse events reporting system. J. Immunother Cancer. 7, 286. https://doi.org/10.1186/s40425-019-0754-2 (2019).
D’Silva, K. M., Cromer, S. J., Yu, E. W., Fischer, M. & Kim, S. C. Risk of incident atrial fibrillation with Zoledronic acid versus denosumab: A propensity Score-Matched cohort study. J. Bone Min. Res. 36, 52–60. https://doi.org/10.1002/jbmr.4174 (2021).
Black, D. M. et al. Once-yearly Zoledronic acid for treatment of postmenopausal osteoporosis. N Engl. J. Med. 356, 1809–1822. https://doi.org/10.1056/NEJMoa067312 (2007).
Heckbert, S. R., Li, G., Cummings, S. R., Smith, N. L. & Psaty, B. M. Use of alendronate and risk of incident atrial fibrillation in women. Arch. Intern. Med. 168, 826–831. https://doi.org/10.1001/archinte.168.8.826 (2008).
Abrahamsen, B., Eiken, P. & Brixen, K. Atrial fibrillation in fracture patients treated with oral bisphosphonates. J. Intern. Med. 265, 581–592. https://doi.org/10.1111/j.1365-2796.2008.02065.x (2009).
Sorensen, H. T. et al. Use of bisphosphonates among women and risk of atrial fibrillation and flutter: population based case-control study. BMJ 336, 813–816. https://doi.org/10.1136/bmj.39507.551644.BE (2008).
Tisdale, J. E. et al. Drug-Induced arrhythmias: A scientific statement from the American heart association. Circulation 142 https://doi.org/10.1161/cir.0000000000000905 (2020).
Delli Poggi, C., Fusaro, M., Mereu, M. C., Brandi, M. L. & Cianferotti, L. Cardiovascular safety and effectiveness of bisphosphonates: from intervention trials to Real-Life data. Nutrients 14 https://doi.org/10.3390/nu14122369 (2022).
Lyles, K. W. et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl. J. Med. 357, 1799–1809. https://doi.org/10.1056/NEJMoa074941 (2007).
Pijnenburg, L. et al. Atrial fibrillation in patients treated with intravenous Zoledronic or Pamidronic acid: a pharmacoepidemiological study. Eur. J. Endocrinol. 184, 437–444. https://doi.org/10.1530/EJE-20-0650 (2021).
Russell, R. G. Bisphosphonates: the first 40 years. Bone 49, 2–19. https://doi.org/10.1016/j.bone.2011.04.022 (2011).
John Camm, A. Review of the cardiovascular safety of Zoledronic acid and other bisphosphonates for the treatment of osteoporosis. Clin. Ther. 32, 426–436. https://doi.org/10.1016/j.clinthera.2010.03.014 (2010).
Lewiecki, E. M. et al. Ibandronate does not increase risk of atrial fibrillation in analysis of pivotal clinical trials. Int. J. Clin. Pract. 64, 821–826. https://doi.org/10.1111/j.1742-1241.2010.02335.x (2010).
Pazianas, M., Compston, J. & Huang, C. L. Atrial fibrillation and bisphosphonate therapy. J. Bone Min. Res. 25, 2–10. https://doi.org/10.1359/jbmr.091201 (2010).
Cipriani, C. et al. Acute effect of Zoledronic acid on the risk of cardiac dysrhythmias. Intern. Emerg. Med. 10, 151–156. https://doi.org/10.1007/s11739-014-1125-0 (2015).
Arku, D., Yousef, C. & Abraham, I. Changing paradigms in detecting rare adverse drug reactions: from disproportionality analysis, old and new, to machine learning. Exp. Opin. Drug Saf. 21, 1235–1238. https://doi.org/10.1080/14740338.2022.2131770 (2022).
Battini, V. et al. Timing matters: A machine learning method for the prioritization of Drug–Drug interactions through signal detection in the FDA adverse event reporting system and their relationship with time of Co-exposure. Drug Saf. 47, 895–907. https://doi.org/10.1007/s40264-024-01430-8 (2024).
Farnoush, A., Sedighi-Maman, Z., Rasoolian, B., Heath, J. J. & Fallah, B. Prediction of adverse drug reactions using demographic and non-clinical drug characteristics in FAERS data. Sci. Rep. 14 https://doi.org/10.1038/s41598-024-74505-2 (2024).
Knisely, B. M., Hatim, Q. & Vaughn-Cooke, M. Utilizing deep learning for detecting adverse drug events in structured and unstructured regulatory drug data sets. Pharm. Med. 36, 307–317. https://doi.org/10.1007/s40290-022-00434-y (2022).
Acknowledgements
This study was performed using the FDA Adverse Event Reporting System (FAERS) database that was provided by the FDA. The information, results, or interpretation of the current study do not represent any opinion of the FDA.
Funding
This paper was not funded.
Author information
Authors and Affiliations
Contributions
FF Wang and Guishui Xu designed and wrote the manuscript. FF Wang, Q Wang and XA Wu performed the data acquisition, statistical analysis and revising. All other authors participated in the interpretation of the results. The final manuscript was read, checked and approved by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Institutional review board approval was waived for this study because FAERS is a public anonymized database.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, F., Xu, G., Wang, Q. et al. A disproportionality analysis of cardiac arrhythmia associated with bisphosphonates based on the FAERS database. Sci Rep 15, 20753 (2025). https://doi.org/10.1038/s41598-025-00900-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-00900-y