Abstract
This study aimed to analyze risk factors for postoperative VTE in pituitary tumor resection patients, focusing on coagulation indicators and their predictive value. This study collected clinical data from 300 patients who underwent pituitary adenoma resection from January 2021 to August 2023 in the Department of Neurosurgery, the Second Clinical College of the Army Medical University, China. Logistic regression modeling was used to identify risk factors for VTE. Restricted cubic spline curves were used to characterize the dose-response relationship between coagulation-related indicators and the risk of venous thromboembolism. The area under the curve (AUC) was calculated using the receiver operating characteristic (ROC) curve to evaluate the predictive power of coagulation-related indicators. Multivariate analysis showed that D-dimer, platelet count and hemoglobin (Hb) were significant predictors of VTE with OR (95% CI) of 1.967 (1.441–2.808), 1.020 (1.013–1.029), and 0.952 (0.914–0.994), respectively. The AUCs for D-dimer, Platelet Count, and Hb were 0.708, 0.731, and 0.712, respectively. The AUC for combining the three coagulation indices was the largest, 0.838. The combined use of D-dimer, Hb, and platelet count can identify high-risk patients early, enabling timely implementation of antithrombotic strategies.
Similar content being viewed by others
Introduction
Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), is a potentially fatal complication that occurs commonly after surgery in general1. Patients with tumors are at high risk of developing venous thromboembolism2. Previous studies have shown that the risk of VTE is four to seven times higher in patients with tumors than in those without tumors3. Additionally, patients with malignant tumors bear a 3.6-fold higher risk of developing VTE compared to those with benign tumors4.
Pituitary tumors are the third commonest intracranial tumors in adults5. They cause symptoms due to hormone overproduction or occupying effects and are classified as functional or non-functional pituitary tumors. Although pituitary tumors are histologically benign, they have strong endocrine effects that can lead to significant morbidity and shortened life expectancy6. Surgical removal is the standard treatment for patients with pituitary tumors. And venous thromboembolism is an important complication that may occur after surgery in pituitary tumor patients. Currently, numerous studies have focused on the pathogenesis of thrombosis, with most mechanisms ultimately influencing three key factors: slow blood circulation, damaged vascular walls, and hypercoagulability due to coagulation abnormalities7. When blood flow slows down, blood cells and coagulation factors tend to aggregate, increasing the risk of thrombosis; vascular wall damage activates platelets and the coagulation system, initiating thrombus formation; and coagulation dysfunction directly leads to hypercoagulability in the blood. These factors work together to promote thrombus formation. Coagulation function plays a crucial role in the formation and progression of blood clots. Platelet count, D-dimer, hemoglobin, prothrombin time, and thrombin time are commonly used coagulation function indicators in clinical practice, which can reflect coagulation factor activity and coagulation status, and may be closely related to the risk of postoperative thrombosis in patients8,9,10. Exploring the incidence of venous thrombosis and its risk factors in pituitary tumor patients after surgery is of great significance in reducing the incidence of postoperative venous thromboembolism complications in pituitary tumor patients and improving the postoperative survival of pituitary tumor patients.
VTE can be prevented effectively by pharmacologic or nonpharmacologic methods11. Anticoagulation should be used to prevent VTE in hospitalized patients at high risk for VTE12. Nevertheless, bleeding complications from anticoagulation are common in oncology patients, for whom thromboprophylaxis may potentially do more harm than good in patients at low risk for VTE13. Therefore, thromboprophylaxis should be stratified in accordance with the level of risk to benefit more high-risk patients.
Currently, many VTE scoring tools are used in clinical practice, including the COMPASS-CAT score for outpatient cancer patients14 and the Padua score for inpatient patients15. However, there is no simple, rapid, and validated VTE risk assessment tool that can be used for pituitary tumor surgery patients in China. Therefore, this study aimed to retrospectively analyze the potential risk factors for postoperative VTE in patients undergoing pituitary tumor resection, focusing on evaluating the association between coagulation-related indicators and thrombosis risk, as well as their predictive capability.
Methods
Study design and participants
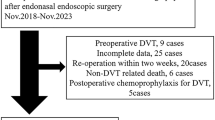
This retrospective, single-center, cross-sectional study collected the demographic and clinical data from patients who underwent pituitary adenoma surgery in the Department of Neurosurgery at the Second Clinical College of the Army Medical University between January 2021 and August 2023. The follow-up time was 7 days after the operation. The inclusion criteria were as follows: (1) patients aged 18 years and older diagnosed with Pituitary adenomas in the Department of Neurosurgery, the Second Clinical College of the Army Medical University who underwent endoscopic surgical treatment, (2) complete clinical data, and (3) VTE patients must have evidence of imaging diagnosis. The exclusion criteria were as follows: (1) patients diagnosed with VTE at admission or with a history of VTE, (2) patients who did not undergo endoscopic surgery, and (3) patients with a history of malignancy. In total, 300 patients were selected for this retrospective study.
This study adhered to the ethical standards of the institutional and national research committees and complied with the 1964 Helsinki Declaration and its subsequent amendments or equivalent ethical guidelines. Approval was obtained from the Ethics Committee of Medical Ethics Committee of the Second Affiliated Hospital of Army Medical University, PLA 2023- New Technology 144-01. Additionally, written informed consent was secured from all participants involved in the study.
Data collection
We obtained patient characteristics and clinical data from the electronic medical records system of our hospital. These data were as follows: (1) patient factors: sex; age; body mass index (BMI), hypertension, hyperlipemia, diabetes mellitus (DM), cardiovascular disease (CVD), smoking history, and past alcohol use; (2) surgical factors: previous VTE (defined as VTE occurred before hospital admission), operation time and intraoperative blood loss; (3) preoperative laboratory parameters: total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-c), low-density lipoprotein cholesterol (LDL-c), D-dimer, red blood cell count (RBC), hemoglobin(Hb), platelet count, prothrombin time (PT) and thrombin time(TT).
BMI was measured as the following two groups according to the BMI classification standard for Chinese individuals: underweight/normal (< 24 kg/m2), and overweight/obese (≥ 24 kg/m2). Age was categorized as < 60 years old and ≥ 60 years old. Hypertension, hyperlipemia, DM, CVD, smoking history, and past alcohol use were analyzed as binary variables categorized as yes or no. Operation time was categorized as < 2 hours and ≥ 2 hours. Intraoperative blood loss was categorized as < 200 mL and ≥ 200 mL. TC, TG, HDL-c, LDL-c, D-dimer, RBC, Hb, platelet count, PT, and TT were analyzed as continuous variables.
Primary outcome measures
The primary outcome measure was the imaging-based diagnosis of VTE, which included both DVT and PE. Venous dual ultrasound is the gold standard for the diagnosis of DVT due to its non-invasive nature and high sensitivity. In addition, CT venography and CT pulmonary arteriography (CTPA) are commonly used imaging modalities for the clinical diagnosis of PE and DVT, but may produce false-positive results due to anatomical variants. Therefore, in this study, bedside dual venous ultrasound, CT venography, and CTPA were used for the combined diagnosis of VTE to reduce false positives of VTE. Before surgery, all patients underwent preoperative lower extremity venous color Doppler ultrasound to exclude preexisting VTE. Immediate Doppler ultrasound was performed for patients showing lower extremity pain, swelling, or skin color changes to detect potential venous issues. Postoperatively, patients displaying unexplained chest symptoms or signs of PE (such as chest tightness, chest pain, hemoptysis, dyspnea, syncope, or decreased oxygen saturation) underwent urgent CTPA to confirm the diagnosis of PE. The imaging diagnosis of the above mentioned VTEs was determined and reviewed independently by two senior imaging physicians.
Statistical analysis
The Shapiro–Wilk test was used to assess the normal distribution of continuous variables. Normally distributed data were presented as means ± standard deviations, while non-normally distributed data were reported as medians (interquartile range) and compared using the Kruskal-Wallis test. Categorical variables were described by percentages and compared using the chi-square test or Fisher’s exact test. Variables found significant in univariate analysis were included as independent variables in a multivariate logistic regression model with VTE occurrence as the dependent variable. In the adjusted logistic regression model, restricted cubic splines with three knots were employed to analyze the dose-response relationship between significant coagulation-related indicators identified in the multivariate analysis and the risk of venous thromboembolism, including testing for nonlinear associations. Receiver operating characteristic (ROC) curves and the area under the ROC curve (AUC) were used to assess and compare the predictive capability of coagulation-related indicators. All data analyses were conducted using R 4.3.2 software. A significance level of P < 0.05 (two-sided) was considered statistically significant.
Results
Characteristics of the study participants
The sociodemographic characteristics, smoking, drinking, surgical factors, and laboratory examination data of participants are summarized in Table 1. The observational study involved 300 participants. The median (interquartile) age of the study population was 52(48–58), and 163 (54.33%) were women. According to the results of CT, 48 (16%) participants were diagnosed with VTE. Compared with patients without VTE, VTE patients were older, and had higher D-dimer, RBC and platelet counts, and lower Hb (P < 0.05). In addition, VTE patients have a higher prevalence of hyperlipidemia, diabetes and cardiovascular disease. In addition, there were significant differences in the amount of intraoperative blood loss between VTE patients and non-VTE patients.
Risk factors for patients with VTE
Table 2 presents the multivariate associations between various indicators and VTE occurrence. After the multivariate logistic regression analysis, the D-dimer, Platelet Count and Hb were proved to be effective predictors of VTE with odd ratio (OR) and 95% confidential interval (CI) of 1.967 (1.441–2.808), 1.020 (1.013–1.029), and 0.952 (0.914–0.994), respectively. We also got some other predictive factors: age ≥ 60 years (OR: 4.256; 95% CI: 1.470-12.522, P = 0.007), hyperlipemia (OR: 6.895; 95% CI: 1.437–31.221, P = 0.012), intraoperative blood loss (OR:3.094; 95% CI: 1.262–8.026, P = 0.016). No significant relationship was detected between RBC, DM, and VTE after adjustment.
Restricted cubic spline curves for coagulation-related indicators and VTE risk
Figure 1 shows the dose-response relationships between the above coagulation-related factors and VTE risk by multivariable-adjusted restricted cubic spline analysis after adjusting hyperlipemia, age and intraoperative blood loss. A non-linear positive correlation was identified between VTE risk and D-dimer and Platelet Count and negatively correlated with hemoglobin (all P non-linear < 0.001).
Accuracy of coagulation-related indicators in predicting VTE
Figure 2 and Table 3 show the results of the individual and combined ROC analyses and AUCs for three coagulation-related indicators used to predict thromboembolism. The AUCs for the three coagulation-related indicators and their combination are all greater than 0.5, indicating a moderate predictive value for VTE. Among the study participants, the model combining the three coagulation indicators had the largest AUC, exceeding 0.8 (AUC: 0.838; 95% CI: 0.756–0.919). Additionally, Hb also had a high predictive performance for VTE, and the AUC was greater than 0.7 (AUC: 0.731;95% CI: 0.618–0.7982). The AUC of D-dimer was 0.708 (95% CI: 0.618–0.7982). The AUC of Platelet Count was 0.712 (95% CI: 0.625-0.800). The above results suggested that these indexes may be effective in the early prediction of VTE risk.
Discussion
There are many risk factors leading to VTE in clinical practice. Studies have found that the common risk factors for patients with vein thrombosis include trauma, age, gender, operation time, and body mass index, which total more than 30 items16,17,18. We found that high D-dimer levels, high platelet count levels, and low hemoglobin levels are important risk factors for postoperative thrombosis in pituitary tumors, further demonstrating the importance of these indicators in assessing the risk of postoperative thrombosis.
D-dimer is a kind of specific degradation product formed by fibrin hydrolysis, which is often used to evaluate whether the body has thrombosis8. Multiple studies have shown that D-dimer is an important biomarker for VTE19,20,21, which is consistent with our findings. A prospective nested case-control study that recruited trauma patients and healthy volunteers found that D-dimer levels (median (interquartile range) of 7.30 (5.85) mg/L) were significantly higher in patients with traumatic DVT than in patients with traumatic non-DVT (3.31 (10.68) mg/L)22. In a prospective, observational, cohort study of 821 patients with newly diagnosed cancer or disease progression, a 2-fold increase in D-dimer was associated with a 30% increased risk of VTE in a univariate Cox regression analysis [hazard ratios (HR) 1.3, 95% CI 1.1–1.5; P < 0.001], the results remained unchanged in multivariate analysis after adjusting for age, sex, surgery, chemotherapy and radiotherapy (HR 1.3, 95% CI 1.2–1.6; P < 0.001)23. A cohort study of the general population in the United States found that the likelihood of future VTE gradually increased as the baseline concentration of D-dimer increased. The 20% with the highest D-dimer value had a 3.9-fold increased risk of VTE compared with the 20% with the lowest, and after further adjustment for hemostatic factors, the risk increased 3.0-fold. The association between D-dimer and VTE was consistently observed in subgroup analyses by age, race, and thrombus type24. Takuji et al. showed that compared with D-dimer of ≤ 1.2 µg/mL, > 1.2 µg/mL significantly increased the risk of VTE (OR: 24.80, 95%CI: 9.57–64.30; P < 0.001)1. Luo et al. studied 1532 patients undergoing ankle fracture surgery and found that D dimer > 0.3 mg/L significantly increased the risk of DVT (OR (95% CI) = 1.65(1.02–2.68), P = 0.042)25. In a prospective multicenter study that included 1380 stroke patients followed for 12 months, elevation of D-dimer measured at hospitalization was independently associated with the first occurrence of subsequent VTE (OR 3.45; 95% CI: 2.01–8.52)26. In this study, a “J-shaped” correlation was found between D-dimer level and postoperative thrombosis (OR (95% CI) = 1.967 (1.441–2.808), P nonlinear <0.001), and the ROC curve showed an AUC of 0.708 (95% CI: 0.618–0.798), the optimal critical value was 2.04 µg/ml (sensitivity 63%, specificity 75%), which provided a reference for the prediction of postoperative VTE in patients with pituitary tumors to a certain extent. Elevated levels of D-dimer polymers usually indicate activation of the clotting system and fibrinolysis in the body, resulting in excessive fibrin degradation products in the blood27,28,29. In addition, the longer duration of surgery may lead to blocked blood circulation and increased blood viscosity, thus increasing the risk of thrombosis30,31,32.
Platelets are cytoplasmic fragments of megakaryocytes produced by bone marrow and are involved in primary hemostasis as well as secondary hemostasis in cases of trauma or injury. Therefore, platelet count is an important indicator to evaluate blood coagulation capacity, with abnormal elevations often signaling an increased risk of thrombosis. In line with previous studies32,33,34, a high platelet count was identified as a risk factor for postoperative thrombosis (OR = 1.020, 95% CI = 1.013–1.029). In addition, further analysis in this study found a “J-shaped” correlation between platelet count and postoperative thrombosis, with an AUC value of 0.712 (95%CI = 0.625-0.800), the optimal critical value was 290.5 × 109/L, sensitivity and specificity of 44% and 92%, respectively. In a retrospective case-control study (65 VTE cases, 123 controls), Zakai et al. investigated risk factors for VTE in hospitalized patients. They found that those with high platelet counts (> 350 × 109/L) had a 3.1-fold increased risk of developing VTE during hospitalization [OR (95% CI) = 3.1(1.4–7.0)]9. In a prospective observational study of patients with newly diagnosed cancer or disease progression, venous thromboembolism occurred in 44 (6.6%) patients during follow-up. At univariate analysis, patients with high platelet counts (≥ 443 × 109/L, representing the 95% percentile of our patients’ cohort) had a more than 5-fold increased risk of VTE compared with patients with platelet counts below the 95th percentile of the data (HR: 5.07, 95% CI: 2.35–10.95, P < 0.0001), increased more than 3-fold in multivariate analysis [HR: 3.50, 95%CI): 1.52–8.06, P = 0.0032]35. In addition, Zhang et al. found that there was a statistically significant difference in platelet counts between the thrombus group (176 × 109/L) and the non-thrombus group (142 × 109/L) in elderly hip fracture patients (P < 0.001). Further multiple logistic regression analysis showed that platelet count was one of the independent risk factors for DVT (P < 0.05), AUC = 0.642 (95%CI: 0.569 ~ 0.714), the critical value was 200.5 × 109/L, sensitivity and specificity were 38.9% and 85.9%36. Similarly, a prospective observational study found a significant association between VTE and thrombocytosis throughout cancer in patients [HR 1.65; 95%CI: 1.04–2.637, P < 0.0341]37. The role of platelets in VTE may be due to the following reasons: secondary soluble mediators of platelet activation, such as TXA2, ADP, and HMGB1, promote platelet aggregation and activation of clotting factors38,39. When the platelet count is abnormally high, the ability of platelets to aggregate and activate is correspondingly enhanced, thus accelerating the formation of blood clots. In addition, platelets can interact with vascular endothelial cells through the release of bioactive substances, destroying the integrity of vascular endothelial cells, and the interaction between platelets and immune cells leads to the release of cytokines, platelet particles, and the increase of tissue factors and thrombin production40,41,42, further promoting thrombosis.
In this study, we found a negative correlation between reduced hemoglobin levels and postoperative thrombosis. RCS showed an “L-shaped” correlation between the two (P nonlinear < 0.001), with an AUC of 0.731 (0.618–0.7982), the optimal critical value was 123.5 g/L (sensitivity 63%, specificity 79%), which was consistent with the results reported in the previous literature. Chi et al. found that low hemoglobin levels at baseline were associated with symptomatic venous thromboembolism in patients hospitalized for acute medical conditions [relative risk (RR) = 1.94; 95% CI: 1.27–2.98; P = 0.002], symptomatic DVT (RR = 2.29; 95% CI: 1.12–4.68; P = 0.019) and non-fatal pulmonary embolism (RR 2.63; 95% CI: 1.22–5.65; P = 0.010) was associated with a higher risk. In addition, low hemoglobin (as a categorical or continuous variable) was still associated with an increased likelihood of VTE (adjusted RR 1.71, 95% CI 1.09–2.69; P = 0.020)10. A study of 2059 total joint replacement (TJA) patients found an AUC of 0.646 for Hb based on the ROC curve. Multivariate binary regression analysis showed that TJA patients with Hb ≤ 118 g/L had a 2.15-fold increased risk of DVT (P < 0.001, 95%CI [1.42–3.24])43. In a prospective observational study, low baseline (pre-chemotherapy) hemoglobin levels (< 100 g/L) have been shown to be a risk factor for chemotherapy-associated VTE44. The degree of hemoglobin decline often reflects the severity of anemia in patients, and a large retrospective study has confirmed that anemia is associated with the occurrence of thrombosis. When hemoglobin is decreased, the lower iron content promotes the activation of the clotting system and inhibits fibrinolytic activity, thus increasing the chance of thrombosis. Early control of hemoglobin levels, and rapid correction of anemia, can avoid coagulation balance in the body, and maintain a relatively stable blood environment45. Moreover, low hemoglobin levels can lead to endothelial dysfunction, blood stasis, and/or hypercoagulability, and are often indicative of many conditions that can lead to VTE, such as inflammation and malnutrition46,47,48. In addition, hemoglobin is an iron-containing protein inside red blood cells whose primary function is to transport oxygen and carbon dioxide. When hemoglobin levels are reduced, the oxygen-carrying capacity of red blood cells is correspondingly reduced, resulting in tissue hypoxia. Studies have shown that hypoxia stimulates endothelial cells to release endothelial microvesicles (EMVs), which can bind to vascular cell adhesion molecules, cell adhesion molecules, and platelet endothelial cell adhesion molecules, promote inflammatory cell infiltration, destroy endothelial cell function, and then lead to thrombosiss49,50,51.
The results of this study show that significant changes in coagulation related factors (D-dimer levels, platelets, hemoglobin, etc.) in patients with pituitary tumors after surgery are closely related to the risk of thrombosis. This discovery provides important monitoring indicators for clinical practice, suggesting that dynamic monitoring of coagulation function should be strengthened after surgery, especially for high-risk patients (such as those with long surgery time, long postoperative bed rest time, or other thrombotic risk factors). In addition, the research results suggest the necessity of preventive anticoagulant therapy in the early postoperative period, especially in cases of abnormal elevation of coagulation related factors. Based on the data from this study, it is recommended to include personalized VTE risk assessment and prevention strategies for postoperative patients with pituitary tumors in clinical guidelines, such as adjusting anticoagulant therapy based on changes in coagulation related factors to reduce the incidence of postoperative VTE. Future research can further explore the effectiveness and safety of different anticoagulation regimens in postoperative patients with pituitary tumors, providing more specific guidance for clinical practice.
This study is based on a patient population with pituitary tumors, and given the relatively few previous studies in this area, it provides data support for thrombosis prevention strategies in this patient population. In addition, this study adopted highly unified and rigorous procedures in the data collection process to ensure the authenticity, accuracy, and reliability of the collected data, and laid a solid foundation for subsequent analysis and conclusions. Finally, we further explored the nonlinear relationship between D-dimer, platelet count, hemoglobin level, and venous thrombosis, and studied the best cutoff values of each index, which provided a reference for effective prevention and treatment strategies of VTE. However, there are some shortcomings in this study. First of all, this study is a single center retrospective study with a population of hospitalized patients in our hospital. There may be selection bias and information bias, and the extrapolation of the research results may be limited. In order to reduce selection bias and information bias, we have established strict inclusion and exclusion criteria, especially for the exclusion of malignant tumors with previous VTE. This is because patients with previous thrombosis may have long-term changes in coagulation function, or these patients may have received anticoagulant therapy or other treatments that may affect postoperative coagulation function changes. Malignant tumor patients often have different blood coagulation characteristics (such as tumor induced coagulation abnormalities, procoagulant status, etc.). The tumor itself or its treatment may have an impact on coagulation indicators, and excluding these patients can avoid the interference of tumor factors on the research results. Multi center research is needed in the future to further evaluate the reliability of this conclusion. Second, according to previous research7,52,53, there is no unified standard for the follow-up time of postoperative patients, but considering that most neurosurgical postoperative thrombosis usually occurs within 7 days after surgery, showing obvious symptoms or diagnostic results. The determination time for venous thrombosis in this study was on the seventh day after surgery. Some studies have also indicated that 1–3 months after discharge is still a high-risk stage for thrombosis, so there may be some bias in the results. Therefore, after the follow-up is completed, the long-term VTE risk of patients still needs to be considered, especially for patients with potential risk factors such as long-term bed rest, obesity, and a history of thrombosis. It is necessary to continue to pay attention to the risk of thrombosis and conduct further monitoring and evaluation if necessary. Third, the sample size of this study is relatively limited, which fails to fully control for all potential confounding factors, and the results need to be further verified. Finally, the laboratory indicators selected in this study were the detection indicators at the time of admission without dynamic monitoring, and these indicators may vary greatly with the development of the disease.
Conclusions
D-dimer, high platelet count, and low hemoglobin level are high risk factors for VTE after pituitary tumor surgery. The combined use of D-dimer, Hb, and platelet count can identify high-risk patients early, enabling timely implementation of antithrombotic strategies. This helps reduce the incidence of postoperative VTE, improving patient outcomes and enhancing the quality of postoperative care.
Data availability
Data supporting the results of this study are available from the authors, but the availability of these data is restricted, and these data used in this study were used with the permission of Chongqing General Hospital affiliated with Chongqing University, and therefore are not available to the public. However, these data are available through the corresponding author(s) if the author(s) make a reasonable request and obtain permission from Chongqing General Hospital affiliated with Chongqing University. Example from: https://doi.org/10.1186/s12943-024-01977-1.
References
Okusaka, T. et al. Incidence and risk factors for venous thromboembolism in the Cancer-VTE registry pancreatic cancer subcohort. J. Gastroenterol. 58, 1261–1271.
Khorana, A. A. Risk assessment and prophylaxis for VTE in cancer patients. J. Natl. Compr. Cancer Netw. JNCCN 789 –797 (2011).
Douketis, J. D., Frere, C. & Farge, D. International clinical practice guidelines for the treatment of venous thromboembolism – Authors’ reply. Lancet Oncol. 20, e656 (2019).
Thomas, D. C. et al. Timing and risk factors associated with venous thromboembolism after lung cancer resection. Ann. Thorac. Surg. 105, 1469–1475.
Nie, D. et al. Immune checkpoints: therapeutic targets for pituitary tumors. Dis. Markers 5300381. (2021).
Mehta, G. U. & Lonser, R. R. Management of hormone-secreting pituitary adenomas. Neuro-oncology, 762–773 (2017). https://doi.org/10.1093/neuonc/now130
Ganau, M. et al. Risk of deep vein thrombosis in neurosurgery: State of the Art on prophylaxis protocols and best clinical practices. J. Clin. Neurosci. 45, 60–66.
Liu, Q. et al. A new method of monitoring catheter-directed thrombolysis for deep venous thrombosis—application of D-dimer and fibrinogen testing. Phlebology 37, 216–222.
Zakai, N. A., Wright, J. & Cushman, M. Risk factors for venous thrombosis in medical inpatients: validation of a thrombosis risk score. J. Thromb. Haemostasis: JTH 2156–2161.
Chi, G. et al. Association of anemia with venous thromboembolism in acutely ill hospitalized patients: An APEX trial substudy. Am. J. Med. 131, 972.e1–972.e7.
Liu, K. et al. Handgrip exercise reduces peripherally-inserted central catheter-related venous thrombosis in patients with solid cancers: A randomized controlled trial. Int. J. Nurs. Stud. 86, 99–106.
Yang, Y. et al. Identification of prophylaxis and treatment for hospitalized patients associated with venous thromboembolism. Chin. Med. J. 136, 1111–1113 (2023).
Frere, C. et al. Incidence, risk factors, and management of bleeding in patients receiving anticoagulants for the treatment of cancer-associated thrombosis. Support. Care Cancer 30, 2919–2931.
Spyropoulos, A. C. et al. External validation of a venous thromboembolic risk score for Cancer outpatients with solid tumors: the COMPASS-CAT venous thromboembolism risk assessment model. Oncologist 25, e1083–e1090.
Peng, Q. et al. Applicability of the Padua scale for Chinese rheumatic in-patients with venous thromboembolism. PloS One 17, e0278157.
Gent, J. M. V. et al. Risk factors for deep vein thrombosis and pulmonary embolism after traumatic injury: A competing risks analysis. J. Trauma. Acute Care Surg. 83, 1154–1160.
Stark, K. & Massberg, S. Interplay between inflammation and thrombosis in cardiovascular pathology. Nat. Rev. Cardiol. 18, 666–682.
Cai, X. et al. Correlation between the fracture line plane and perioperative deep vein thrombosis in patients with tibial fracture. Clin. Appl. Thromb.Hemos. 27, 10760296211067258.
Zhang, W. et al. A retrospective cohort study on the risk factors of deep vein thrombosis (DVT) for patients with traumatic fracture at Honghui hospital. BMJ Open. 9, e024247 (2019).
Favresse, J. et al. D-dimer: Preanalytical, analytical, postanalytical variables, and clinical applications. Crit. Rev. Clin. Lab. Sci. 55, 548–577.
Evensen, L. H. et al. Hemostatic factors, inflammatory markers, and risk of incident venous thromboembolism: the Multi-Ethnic study of atherosclerosis. J. Thromb. Haemostasis: JTH 19, 1718–1728.
Cao, X. et al. The impact of anticoagulant activity of tissue factor pathway inhibitor measured by a novel functional assay for predicting deep venous thrombosis in trauma patients: A prospective nested Case-Control study. Clin. Appl. Thrombosis/hemostasis 27, 10760296211063877.
Ay, C. et al. D-Dimer and prothrombin fragment 1 + 2 predict venous thromboembolism in patients with cancer: results from the Vienna Cancer and thrombosis study. J. Clin. Oncology: Official J. Am. Soc. Clin. Oncol. 27, 4124–4129 (2009).
Cushman, M. et al. Fibrin fragment D-dimer and the risk of future venous thrombosis. Blood, 1243–1248 (2003).
Luo, Z. et al. Preoperative incidence and locations of deep venous thrombosis (DVT) of lower extremity following ankle fractures. Sci. Rep. 10, 10266 (2020).
Yi, X. et al. The incidence of venous thromboembolism following stroke and its risk factors in Eastern China. J. Thromb. Thrombolysis 34, 269–275.
Wada, H. et al. Elevated levels of soluble fibrin or D-dimer indicate high risk of thrombosis. 1253–1258.
Riondino, S., Ferroni, P., Zanzotto, F. M., Roselli, M. & Guadagni, F. Predicting VTE in cancer patients: candidate biomarkers and risk assessment models. Cancers 11, 95 (2019).
Bernardi, E. & Camporese, G. Diagnosis of deep-vein thrombosis. Thromb. Res. 163, 201–206.
Osaki, T. et al. Risk and incidence of perioperative deep vein thrombosis in patients undergoing gastric cancer surgery. Surg. Today 48, 525–533.
Groot, O. Q. et al. High risk of symptomatic venous thromboembolism after surgery for spine metastatic bone lesions: A retrospective study. Clin. Orthop. Relat. Res. 477, 1674–1686.
Schlick, C. J. R. et al. Pre-operative, intra-operative, and post-operative factors associated with post-discharge venous thromboembolism following colorectal cancer resection. J. Gastrointest. Surg. 24, 144–154.
Lagrange, J., Lacolley, P., Wahl, D., Peyrin-Biroulet, L. & Regnault, V. Shedding light on hemostasis in patients with inflammatory bowel diseases. Clin. Gastroenterol. Hepatol. 19, 1088–1097.
Henry, D. H., Dahl, N. V. & Auerbach, M. A. Thrombocytosis and venous thromboembolism in cancer patients with chemotherapy induced anemia May be related to ESA induced iron restricted erythropoiesis and reversed by administration of IV iron. Am. J. Hematol. 87, 308–310.
Simanek, R. et al. High platelet count associated with venous thromboembolism in cancer patients: results from the Vienna Cancer and thrombosis study (CATS). J. Thromb. Haemostasis: JTH 8, 114–120.
Zhang, L. et al. Analysis of high-risk factors for preoperative DVT in elderly patients with simple hip fractures and construction of a nomogram prediction model. BMC Musculoskelet. Disord. 23, 441 (2022).
Mandalà, M. et al. Acquired and inherited risk factors for developing venous thromboembolism in cancer patients receiving adjuvant chemotherapy: A prospective trial. Ann. Oncol. 21, 871–876.
Mitrugno, A. et al. The role of coagulation and platelets in colon cancer-associated thrombosis. Am. J. Physiol. Cell Physiol. 316, C264–C273 (2019).
Vogel, S. et al. Platelet-derived HMGB1 is a critical mediator of thrombosis. J. Clin. Investig. 125, 4638–4654.
von Brühl, M. L. et al. Monocytes, neutrophils, and platelets cooperate to initiate and propagate venous thrombosis in mice in vivo. J. Exp. Med. 209, 819–835 (2012).
Matthay, Z. A. et al. Postinjury platelet aggregation and venous thromboembolism. J. Trauma. Acute Care Surg. 93, 604–612 (2022).
Barrett, T. J. et al. Platelets amplify endotheliopathy in COVID-19. Sci. Adv. 7, eabh2434 (2021).
Xiong, X., Li, T., Yu, S. & Cheng, B. Association between red blood cell indices and preoperative deep vein thrombosis in patients undergoing total joint arthroplasty: A retrospective study. Clin. Appl. Thrombosis/hemostasis 28, 10760296221149029.
Khorana, A. A., Kuderer, N. M., Culakova, E., Lyman, G. H. & Francis, C. W. Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 111, 4902–4907 (2008).
Lin, C. L., Lin, C. L., Tzeng, S. L. & Chung, W. S. Aplastic anemia and risk of deep vein thrombosis and pulmonary embolism: A nationwide cohort study. Thromb. Res. 149, 70–75.
Solovey, A. et al. Circulating activated endothelial cells in sickle cell anemia. N. Engl. J. Med. 1584–1590 (1997).
Timp, J. F., Braekkan, S. K., Versteeg, H. H. & Cannegieter, S. C. Epidemiology of cancer-associated venous thrombosis. Blood 122, 1712–1723 (2013).
Martino, R. R. D. et al. Variation in thromboembolic complications among patients undergoing commonly performed cancer operations. J. Vasc. Surg. 55, 1035–1040.
Deng, F. et al. Endothelial microvesicles in hypoxic hypoxia diseases. J. Cell. Mol. Med. 22, 3708–3718.
Yong, P. J. A., Koh, C. H. & Shim, W. S. N. Endothelial microparticles: missing link in endothelial dysfunction? Eur. J. Prev. Cardiol. 20, 496–512.
Markiewicz, M., Richard, E., Marks, N. & Ludwicka-Bradley, A. Impact of endothelial microparticles on coagulation, inflammation, and angiogenesis in age-related vascular diseases. J. Aging Res. 734509. (2013).
Khaldi, A., Helo, N., Schneck, M. J. & Origitano, T. C. Venous thromboembolism: deep venous thrombosis and pulmonary embolism in a neurosurgical population. J. Neurosurg. 114, 40–46.
Singh, T. et al. Timing of symptomatic venous thromboembolism after surgery: meta-analysis. Br. J. Surg. 110, 553–561 (2023).
Acknowledgements
The investigators are grateful to the dedicated participants and all research staff of the study.
Author information
Authors and Affiliations
Contributions
Yi Xiang and Ya Wu statistically analyzed the data. Yi Xiang and Huan Liu accessed and verified the data. Zheng Chen made substantial contributions to the acquisition of data. Yi Xiang wrote the first draft of the manuscript with input from JinYu Pan. All authors contributed to the conception and design of the study, data interpretation, and manuscript revision. All authors read and approved the submitted manuscript and had final responsibility for the decision to submit for publication. JinYu Pan was the overall guarantor of the content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the Medical Ethies Committee of Second Affiliated Hospital Of Army Medical University, PLA, and written informed consent was obtained from all participants (Reference Number: 2023-New Technique-144-01).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xiang, Y., Wu, Y., Liu, H. et al. Association of coagulation-related indicators with postoperative venous thromboembolism occurrence in patients with pituitary tumors. Sci Rep 15, 16694 (2025). https://doi.org/10.1038/s41598-025-01029-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-01029-8