Abstract
Unilateral pedicle screw (UPS) fixation has been applied in oblique lumbar interbody fusion (OLIF). However, the internal fixation strength required by OLIF is still controversial. Although satisfactory short-term outcome has been achieved with OLIF combined with UPS, the maintenance of stability in the fused segment remains a concern due to the lack of mid-term to long-term clinical follow-up reports. In this study, we compared the mid-term to long-term radiographic and clinical outcomes of unilateral (n = 100) versus bilateral (n = 86) instrumented one-level OLIF for lumbar degenerative disease (LDD).The mean follow-up duration was 75.09 ± 5.08 months. A significant decrease occurred in operative time, blood loss in UPS group. No statistical difference was detected regarding complication rate and fusion rate between the two groups. The VAS of low back pain at 6 months postoperatively was better than that of the BPS group. However, there were no significant differences in VAS and ODI at any other follow-up time point. The incidence of ASD was 12% lower in the UPS group than the 18.6% observed in the BPS group at the final follow-up. The standardized cross sectional area (SCSA) and degree of fat infiltration (DFF) of the multifidus muscle (MM) were better than those of the BPS group in the same period. The current data show that OLIF-UPS for the treatment of single-level LDD could achieve satisfactory mid-term to long-term outcomes comparable to BPS fixation, with less surgical time, less blood loss, and less DFF of the MM.
Similar content being viewed by others
Introduction
Bilateral pedicle screw fixation (BPS) combined with oblique lateral interbody fusion (OLIF) is a widely utilized and successful surgical procedure for treating lumbar degenerative diseases (LDD), including lumbar instability, lumbar spinal stenosis, and spinal deformity1,2. Bilateral screws and interbody fixation devices can effectively share spinal loads2, provide initial stability of the fixed segment, and have been developed to correct deformities, increase interbody fusion rates, and improve clinical outcomes in early rehabilitation3,4. However, BPS rigid fixation has corresponding disadvantages. For example, an increase in the number of implants leads to more extensive muscle stripping, greater blood loss, longer operative times and higher costs involved5. In addition, biomechanical studies have found that in animal models, a decrease in bone mineral content is detected in the region of fixation6,7,8, and the increased stiffness of the fused segments may have accelerated the degeneration of the adjacent segments9,10. Therefore, some studies have reduced the stiffness of the fixation system by reducing the number of screws in order to optimize the biomechanical conditions3,4,11. Unilateral pedicle screw fixation (UPS) is likely to be a better solution11. In addition, the cost-effectiveness of this approach is worthy of attention12. In 1991, Goel et al.13 demonstrated that UPS fixation did reduce the effect of stress shielding on the fixed segments and reduced peak stresses at adjacent levels above and below the fusion. Previous meta-analysis articles have also compared UPS and BPS fixation for the treatment of LDD, and found no differences between the two fixation modalities in terms of functional outcomes, fusion rates, and clinical satisfaction3,4,6,7,11,14. However, these studies mixed different lumbar interbody fusions (TLIF/PLIF) and did not address OLIF cases. Although studies1,2 have reported good results of UPS fixation after OLIF, they only evaluated the clinical efficacy in short-term follow-up (≤ 2 years), and the medium-term to long-term efficacy of both fixation modalities has not been well validated. To our knowledge, no mid- to long-term follow-up studies comparing UPS and BPS combined with OLIF for the treatment of LDD have been reported. Therefore, we performed consecutive clinical follow-ups averaging more than 6 years with the aim of comparing the mid- to long-term clinical efficacy of OLIF combined with two fixation modalities for the treatment of LDD.
Materials and methods
Study design and patients
The study was approved by the Ethics Committee of General Hospital of Ningxia Medical University (No.KYLL-2022-1137), and written informed consent was obtained from all participants. As agreed with the ethical committee, all methods were performed in accordance with the relevant guidelines and regulations.
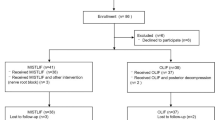
A consecutive cohort of patients receiving OLIF combined with UPS or BPS fixation from July 2017 to March 2019 was studied (Patients admitted before May 2018 received BPS fixation and received UPS fixation thereafter). Inclusion criteria were as follows: (1) All patients presented with varying degrees of low back or leg pain, and there was no significant improvement in symptoms after more than 3 months of conservative treatment; (2) diagnosed with lumbar disc herniation, degenerative lumbar spinal stenosis, and lumbar spondylolisthesis below degree 2; (3) treated with single-level OLIF, and completed a minimum of 60 months of follow-up; (4) patients whose preoperative adjacent segment degeneration did not exceed grade II15.
Exclusion criteria were as follows: (1) congenital lumbar spinal stenosis, degree 2 or above lumbar spondylolisthesis; (2) bony stenosis of lateral recess, osteophyte formation at posterior margin of intervertebral space or obvious calcification of ligamentum flavum; (3) prolapse or free type disc herniation with rupture of annulus fibrosus, huge central lumbar disc herniation and calcification; (4) Bony spinal stenosis or combined non-inclusive disc herniation requiring direct spinal decompression; (5) Combined lumbar spondylolisthesis of II°or greater.
Sample size determination, sampling technique and procedure
This is a single-center retrospective study. The sample size was determined by comparing the sample size of two independent sample rates. Based on a previous study, the incidence of adjacent segmental disc degeneration was UPS VS BPS (55.9% vs. 72.7%). At 95% confidence interval and 80% test efficiency, PASS software 2020 (NCSS LLC., Kaysville, U.T., USA) software was used with an accuracy of 5% (0.05). The minimum sample size of this study was calculated to be 202 cases, 101 cases in each group. Considering the 20% loss of follow-up and the appropriate increase in sample size, the credibility of the research results can be improved. A total of 257 cases were included in this study.
Surgical methods
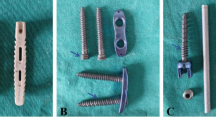
After general anesthesia, all patients were positioned in the lateral decubitus for oblique lateral approach, and intraoperative neurophysiological monitoring was given. The segment was fluoroscopically positioned and marked, and a transverse incision of approximately 3 cm to 5 cm in length is made to progressively establish the working channel, expose and resect the disc, cleaning residual nucleus pulposus tissue and cartilage endplate, and place the trial module, after the intervertebral height was satisfactorily propped up, the Cage (the allograft bone was jump tied with absorbable wires, Avoid allogeneic bone defluvium) filled with allograft bone (Beijing Xinkangchen Medical Technology Development Co., Ltd., China) was tightly implanted into the intervertebral space, fluoroscopy was performed again to confirm that the fusion device was well-positioned, the operative field was rinsed, and the incision was closed with layer-by-layer sutures. Afterwards, the patient was turned to the prone position, the skin was sterilized and a sheet was spread. In the UPS group, pedicle screw fixation was implanted unilaterally through the Wiltse approach, and in the BPS group, pedicle screw fixation was implanted through bilateral Wiltse approaches. Intraoperative fluoroscopy again confirmed that the pedicle screw rod was fixed in a good position, and the incision was closed layer by layer.
Definition of relevant change
The study recorded operative time, intraoperative bleeding, and complications in both groups. The clinical efficacy was evaluated by using the VAS and ODI. The radiological analysis was performed by a well-trained, experienced spine fellow who was familiar with all the techniques used in the study. Functional and radiologic data were collected at 3, 6, and 12 months postoperative follow-up, followed by annual follow-up visits.
Adjacent segmental disc degeneration
the lumbar disc degeneration grading criteria of Pfirrmann et al.16 were used to evaluate adjacent segmental disc degeneration (ASD) on T2-weighted Sagittal MRI: grade 0, no degeneration; grade I, mild degeneration; grade II, moderate degeneration; and grade III, severe degeneration. Specific evaluation is as follows: disc signals of grades I and II are normal discs, and grades III, IV and V are degenerated discs; disc signals that change from preoperative grades I and II to postoperative grades III and above are defined as degeneration, or preoperative signals are the grades of degenerated discs, and the increase in degeneration of grades 1 or 2 is also defined as the presence of degeneration after the operation. Patients were also observed for the presence of corresponding clinical symptoms.
SCSA and DEF
We used Image J software (version 1.51, National Institutes of Health) to measure the cross-sectional area (CSA) of the multifidus muscle (MM) and the CSA of fatty infiltration in the MM, as well as the CSA of vertebral bodies at the same level. To ensure comparability of data and mitigate the impact of body size and other variables, we converted CSA into standardized cross-sectional area (SCSA). This was achieved by calculating the SCSA as the ratio of the CSA of the MM to the CSA of the vertebrae at the same level× 100%. Additionally, we also measured the degree of fat infiltration (DFF) in the MM by calculating the DFF as the ratio of the fat CSA to the CSA of the MM × 100%.
Fusion rate
After 1 year of surgery, the intervertebral implant fusion was evaluated using CT plain scan and 3D reconstruction, and the fusion rate was assessed using the Bridwell grading system17. The Bridwell system consists of the following categories and grades: fused with remodeling and trabeculae present (Grade I); graft intact, not fully remodeled and incorporated, but no lucency present (Grade II); graft intact, potential lucency present at top and bottom of graft (Grade III); and fusion absent with collapse/resorption of the graft (Grade IV). Patients evaluated were considered unfused and were reassessed by CT scan after 2 years of follow-up.
Cage subsidence
Cage subsidence was assessed according to the staging proposed by Marchi et al.18 and it was classified into 4 degrees according to the degree of DH reduction (grade 0, 0–24%; grade I, 25-49%; grade II, 50-74%; and grade III, 75-100%). The risk factors associated with the occurrence of ASD were statistically analyzed, and the relationship between the trend of VAS score and ODI with the degree of ASD and cage subsidence was evaluated.
Statistical analysis
The SPSS (version 24.0, Inc, Chicago, IL, USA) was used for statistical analysis in this study. The measurement data were presented as mean ± SD, one-way ANOVA was used to compare groups, group difference was examined by Student’s t-test. The enumeration data were presented as n (%), and compared by χ2 test. The correlation between the VAS score and ODI with the cage subsidence was performed by Pearson correlation analysis. The P < 0.05 was considered to indicate a statistically significant difference.
Results
Patient-related and demographic variables
Of 257 patients who met the inclusion and exclusion criteria, 132 patients (51.36%) underwent UPS (Fig. 1) and 125 patients (48.64%) underwent BPS (Fig. 2). Ultimately, 186 of 257 (72.37%) patients were available for average 6-year radiologic and clinical follow-up data: 75.76% (100 of 132) patients in the UPS group and 68.80% (86 of 125) patients in the BPS group. No difference in sex, age, preoperative diagnosis, fusion level, and BMI were found in these patients between the two groups (all P > 0.05). The demographic characteristics of the patients are summarized in Table 1.
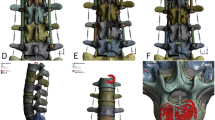
(A and B) Preoperative radiographs and (C and D) Follow-up (66 months postoperative) anteroposterior and lateral radiographs of a 62-year-old female with L4-L5 lumbar stenosis treated with decompression, interbody fusion, and BPS fixation. (E and F) Postoperative computed tomography (CT) scan showing complete fusion at L4/5 level.
(A and B) Preoperative radiographs and (C and D) Follow-up (68 months postoperative) anteroposterior and lateral radiographs of a 65-year-old female with L4-L5 lumbar stenosis treated with decompression, interbody fusion, and UPS fixation. (E and F) Postoperative computed tomography (CT) scan showing complete fusion at L4/5 level.
Comparison of clinical outcome
The UPS group had a shorter operative time and less blood loss than the BPS group (P < 0.001) (Table 2). No significant difference in length of hospital stay and general complications was found between the two groups (P > 0.05). There were 4 cases with left thigh numbness and 6 cases with psoas weakness in the UPS group and 4 cases with left thigh numbness and 8 cases with psoas weakness in the BPS group. Two cases suffered from superficial wound infection in the bilateral group. The symptoms relieved in all patients at 3-month post-operation. In terms of clinical outcomes, the VAS and ODI significantly reduced in both groups at different time points postoperative as compared to preoperative (Table 3). The VAS of low back pain at 6 months postoperatively was lower than that of the BPS group (P = 0.008), but no significant differences in VAS or ODI were found at other follow-up points. (P > 0.05). (Fig. 3).
Comparison of VAS score of low back and leg pain and ODI score between the OLIF-UPS and OLIF-BPS groups preoperatively (pre), 6 months (6 M), 12 months (12 M), Final follow-up(F fu) postoperatively. Data represents mean SD. Note: ns: the difference was not significant (P > 0.05). **:the difference was significant (P < 0.05).
Radiographic measurement
Postoperatively, both groups showed significant improvement in DH (P < 0.05). DH decreased at the last follow-up compared to six months postoperatively, but remained significantly higher than preoperatively (P < 0.05). The degree of DH loss was not a significant difference between the two groups (Table 3). At 1 year postoperatively, the fusion rate in the UPS group was 91% (76% in grade I and 15% in grade II), and was 93.03% (81.40% in grade I and 11.63% in grade II) in the BPS group. There was no statistically significant difference between the fusion rates of the two groups (P = 0.613).
The majority (93/100, 93%) of the fused segment cage subsidence in the final follow-up UPS group was grade 0, 7 cases had grade I subsidence (7/100, 7%), and there were no patients with grade II or III subsidence. No statistical difference in the degree of cage subsidence at 1 year postoperative (10.77 ± 7.12) % compared with the last follow-up (10.98 ± 7.26) % (P = 0.148). The majority (45/81, 85.2%) of the BPS group had grade 0 fusion segment Cage settlement, 3 cases had grade I settlement (6/51, 11.8%), and there were no patients with grade II or III settlement. No statistical difference in the degree of cage subsidence at 1year postoperative (10.23 ± 5.50) % compared with the last follow-up (10.39 ± 5.71) % (P = 0.258). No secondary scoliosis, cage displacement and screw loosening or breakage were found in all patients.
ASD in first cephalad or caudal adjacent segment was noted in 12% of the UPS group and 18.60% of the BPS group (P = 0.145). In the UPS group, there were 9 cases of grade I, 2 cases of grade II, and 1 case of grade III. 7 patients had mild low back pain. In the UPS group, there were 12 cases of grade I, 4 cases of grade II, and 1 case of grade III. 10 patients had mild low back and leg pain. All patients were radiologic ASD and none needed revisions. The differences in SCSA (49.38 ± 1.72 vs. 41.17 ± 2.62) and DEF (17.80 ± 1.48 vs. 18.48 ± 2.23) in the UPS group at the final follow-up were statistically significant compared with the BPS group (P < 0.05). (Fig. 4).
Related clinical outcome analysis
Subgroup analysis was performed by dividing the cage subsidence into mild group (grade 0, 0–24%) and moderate group (grade 1, 25–50%), and the results showed no difference in efficacy between groups with different degrees of cage subsidence (P > 0.05). Pearson correlation analysis showed no significant correlation between VAS of low back and leg pain, ODI score and cage subsidence at the last follow-up (r1 = 0.05, P1 = 0.485), (r2 = 0.023, P2 = 0.752) and (r3 = 0.083, P3 = 0.259). (Table 4).
Discussion
OLIF combined with pedicle screw fixation has been widely used in clinical practice1,2. However, the required internal fixation strength of OLIF is still controversial. Biomechanical studies have shown that compared with the three-point fusion structure fixed by BPS, the fixation asymmetry of the UPS two-point fusion structure leads to a decrease in fixation strength and stability, especially in terms of resistance to lateral bending and axial rotation19. For example, in the report of Harris BM et al.20 the ROM of the fixed segment of the UPS group increased by 26% and 44% respectively compared with the BPS group in the left and right lateral flexion modes. However, studies have shown that there is no significant difference in clinical results between UPS and BPS fixation after OLIF1,2. However, to be noted, these studies only focus on short-term efficacy (< 2 years), and mid-term to long-term efficacy has not been reported. To our knowledge, this is the first study on the mid-term to long-term efficacy of OLIF combined with UPS fixation for LDD.
In this study, consecutive follow-up (range 60~80 months) was performed in both groups, and the results showed that OLIF combined with UPS fixation in the treatment of LDD can achieve satisfactory mid-term to long-term results, with less blood loss and shorter operative time, whereas the clinical outcomes were similar between the two groups, which is in line with the results of the study by Wen et al.2. Although there was no significant difference in the length of hospital stay between the two groups, UPS fixation from the Wiltse approach reduces muscle and soft tissue stripping, unilateral nail placement, and minimally invasive surgical procedure, which may be more conducive to early postoperative recovery, which explains the were lower lumbar VAS scores in the UPS group than in the BPS group at the six-month postoperative follow-up. Theoretically, decreased structural stiffness and increased segmental motion with unilateral fixation may affect the rate of fusion, whereas our study demonstrated that the current fusion rates are satisfactory and consistent with those reported in the OLIF literature series1,2,21,22. The quality and speed of fusion were comparable between the two groups when compared over the same period of time, which is consistent with the findings of Gu et al.23 where a comparison of parameters such as (segmental lordosis, SL) and (lumbar lordosis, LL) by radiographic analysis revealed no significant changes in the two groups from the immediate postoperative period to any point in time of fusion. A possible explanation for this is that the fusion device used in OLIF is wider and spans the epiphyseal rings of the vertebrae bilaterally, providing additional stability to the anterior column, which may help to prevent displacement of the fusion device and provide a more efficient environment for the fusion process19. In addition, UPS fixation preserves the intact contralateral structures, which contributes to the stability of the posterior column of the spine. There is evidence24 that prolonged stripping and contraction of the muscle can lead to its ischemic necrosis and denervation, which predisposes the multifidus muscle (MM) to atrophy postoperatively, which in turn leads to sagittal instability, increased shear forces around the lesser joints, and decreased trunk stability25, whereas unilateral fixation using the Wiltse approach preserves the tendon origin of the MM and the posterior column tension band of the spinal column with the " bowstring effect”25, which can act as a soft tension band to stabilize the spine. Therefore, considering the published articles and our study, we believe that UPS fixation can provide adequate stability for one-level fusion.
From the consecutive imaging follow-up, we found that the incidence of cage subsidence was similar in the two groups, and the vast majority of them were grade I subsidence, and the settlement stabilized after 1 year of operation, and there was no statistically significant difference in the degree of DH loss between the two groups at different time intervals, and cage displacement and screw loosening and fracture were not detected during the follow-up. Although there is still uncertainty about whether fusion settlement affects long-term clinical outcomes26, from the results of this study, there was no difference in clinical outcomes between groups with different degrees of cage subsidence, and correlation analysis suggests that there is also no exact relationship between cage subsidence and outcomes, The findings were the same as those of Hiyama A et al.27. However, it should be noted that severe cage subsidence may lead to screw loosening, concomitant intervertebral space collapse, and recurrent neurologic compression symptoms, resulting in an increased rate of reoperation26. Several studies have reported that postoperative resulting lumbar scoliosis is more common due to the asymmetry of unilateral fixation6. Choi et al.28 reported postoperative scoliosis in 6 out of 26 patients in the unilateral group and in 1 out of 27 patients in the bilateral group, with all the changes manifesting as surgical scoliosis. In this study, no secondary scoliosis was observed in the UPS group, and the sagittal plane balance of the spinal pelvis remained stable during follow-up. This may be related to the fact that UPS fixation preserved the posterior column muscle-ligament complex and the contralateral articular synchondrosis joint intact, and the contralateral paravertebral muscles were rebalanced6. Theoretically, less rigid UPS fixation could prevent early degeneration of adjacent segments11,13,29. In an in vitro study, Goel et al.13 demonstrated that a less rigid fixation structure reduced the “stress rise” effect at the adjacent level. Kim et al.30 found that the incidence of ASD in 55.9% (33/59) of patients receiving UPS was lower than that in 72.7% (64/88) of the group receiving BPS by radiologic and clinical follow-up of 147 patients for at least 10 years. In our study, contrary to the hypothesis that BPS fixation is excessively stiff and would accelerate ASD, there was no significant difference between the two groups at an average of 5 years of follow-up, and most of the degeneration was of grade I, which may be related to the shorter duration of follow-up. Zhu et al.31 found that lumbar MM atrophy or fatty infiltration is one of the risk factors for the development of ASD. We also noted that the area of the MM decreased to varying degrees in both groups, and the decrease was more pronounced in the BPS group after the same time point, UPS fixation preserves the integrity of the midline muscle-ligament complex as much as possible, which may be an important reason for the slightly lower incidence of ASD. Therefore, the fixation of Wiltse approach32 or lateral approach33 can be considered to reduce the injury of MM during operation, and the stability training of core muscles such as MM should be actively carried out after operation in order to slow down the occurrence of ASD.
Several limitations of this study need to be acknowledged. First, this is a retrospective case-control study with inevitable selection and recall bias. Second, The sample size was relatively small, and prospective and larger case sizes are needed at a later stage to further validate the reliability of the findings. Third, The bone mineral density of the cases included in this study is mostly normal or osteopenia, and the number of osteoporosis cases is relatively small. In the case of osteoporosis, whether unilateral fixation can effectively maintain the long-term stability of the fusion segment needs further study. Finally, a mean follow-up of 6 years is still relatively short, and longer follow-up is needed to determine the clinical significance of these two fixation techniques in OLIF.
Conclusion
In summary, UPS and BPS had comparable mid- and long-term clinical and radiologic outcomes at an average of 6 years of OLIF surgery follow-up. Compared with BPS, UPS fixation is a shorter operating time, less invasive procedure with a lower rate of fatty infiltration of the MM. Therefore, OLIF combined with UPS fixation is an effective and reliable option for the treatment of single-segment lumbar spine disease.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Yang, S. L. et al. Treatment of degenerative lumbar scoliosis with oblique lumbar interbody fusion in conjunction with unilateral pedicle screw fixation via the Wiltse approach. Orthop. Surg. 13, 1181–1190 (2021).
Wen, J. et al. Unilateral versus bilateral percutaneous pedicle screw fixation in oblique lumbar interbody fusion. World Neurosurg. 134, e920–e927 (2020).
Xiao, S. W., Jiang, H., Yang, L. J. & Xiao, Z. M. Comparison of unilateral versus bilateral pedicle screw fixation with cage fusion in degenerative lumbar diseases: A Meta-Analysis. Eur. Spine J. 24, 764–774 (2015).
Xue, H., Tu, Y. & Cai, M. Comparison of unilateral versus bilateral instrumented transforaminal lumbar interbody fusion in degenerative lumbar diseases. Spine J. 12, 209–215 (2012).
Deyo, R. A., Nachemson, A. & Mirza, S. K. Spinal-Fusion Surgery - The case for restraint. New. Engl. J. Med. 350, 722–726 (2004).
Xie, Y. et al. Comparative study of unilateral and bilateral pedicle screw fixation in posterior lumbar interbody fusion. Orthopedics 35, e1517–e1523 (2012).
Mao, L., Chen, G. D., Xu, X. M., Guo, Z. & Yang, H. L. Comparison of lumbar interbody fusion performed with unilateral or bilateral pedicle screw. Orthopedics 36, e489–e493 (2013).
McAfee, P. C. et al. The effect of spinal implant rigidity on vertebral bone density. Canine Model. Spine. 16, S190–S197 (1991).
Okuda, S. et al. Adjacent segment disease after single segment posterior lumbar interbody fusion for degenerative spondylolisthesis: minimum 10 years Follow-Up. Spine 43, E1384–E1388 (2018).
Shono, Y., Kaneda, K., Abumi, K., McAfee, P. C. & Cunningham, B. W. Stability of posterior spinal instrumentation and its effects on adjacent motion segments in the lumbosacral spine. Spine 23, 1550–1558 (1998).
Suk, K. S., Lee, H. M., Kim, N. H. & Ha, J. W. Unilateral versus bilateral pedicle screw fixation in lumbar spinal fusion. Spine 25, 1843–1847 (2000).
Kuntz, K. M., Snider, R. K., Weinstein, J. N., Pope, M. H. & Katz, J. N. Cost-Effectiveness of fusion with and without instrumentation for patients with degenerative spondylolisthesis and spinal stenosis. Spine 25, 1132–1139 (2000).
Goel, V. K. et al. Effects of rigidity of an internal fixation device. A comprehensive Biomechanical investigation. Spine 16, S155–S161 (1991).
Hiyama, A., Katoh, H., Sakai, D., Sato, M. & Watanabe, M. Short-Term comparison between unilateral versus bilateral percutaneous pedicle screw fixation in Short-Level lateral lumbar interbody Fusion-a prospective randomized study. Glob Spine J. 14, 1485–1497 (2024).
Pfirrmann, C. W., Metzdorf, A., Zanetti, M., Hodler, J. & Boos, N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26, 1873–1878 (2001).
Ghiselli, G., Wang, J. C., Hsu, W. K. & Dawson, E. G. L5-S1 segment survivorship and clinical outcome analysis after L4-L5 isolated fusion. SPINE 28, 1275–1280 (2003).
Bridwell, K. H., Lenke, L. G., McEnery, K. W., Baldus, C. & Blanke, K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects?? Spine. 20, 1410–1418 (1995).
Marchi, L. et al. Radiographic and clinical evaluation of cage subsidence after Stand-Alone lateral interbody fusion. J. Neurosurg-Spine. 19, 110–118 (2013).
Zhang, Z., Fogel, G. R., Liao, Z., Sun, Y. & Liu, W. Biomechanical analysis of lateral lumbar interbody fusion constructs with various fixation options: based on a validated finite element model. World Neurosurg. 114, e1120–e1129 (2018).
Harris, B. M. et al. Transforaminal lumbar interbody fusion: the effect of various instrumentation techniques on the flexibility of the lumbar spine. Spine 29, E65–E70 (2004).
Blizzard, D. J. & Thomas, J. A. Mis Single-Position lateral and oblique lateral lumbar interbody fusion and bilateral pedicle screw fixation: feasibility and perioperative results. Spine 43, 440–446 (2018).
Zeng, Z. Y. et al. Complications and prevention strategies of oblique lateral interbody fusion technique. Orthop. Surg. 10, 98–106 (2018).
Gu, G. et al. Clinical and radiological outcomes of unilateral versus bilateral instrumentation in Two-Level degenerative lumbar diseases. Eur. Spine J. 24, 1640–1648 (2015).
Zhu, H. F. et al. Comparison of oblique lateral interbody fusion (Olif) and minimally invasive transforaminal lumbar interbody fusion (Mi-Tlif) for treatment of lumbar degeneration disease: A prospective cohort study. Spine 47, E233–E242 (2022).
Jermy, J. E., Copley, P. C., Poon, M. & Demetriades, A. K. Does Pre-Operative multifidus morphology on mri predict clinical outcomes in adults following surgical treatment for degenerative lumbar spine disease?? A systematic review. Eur. Spine J. 29, 1318–1327 (2020).
Choi, J. Y. & Sung, K. H. Subsidence after anterior lumbar interbody fusion using paired Stand-Alone rectangular cages. Eur. Spine J. 15, 16–22 (2006).
Hiyama, A. et al. Comparative study of cage subsidence in Single-Level lateral lumbar interbody fusion. J. Clin. Med. 11, (2022).
Choi, U. Y. et al. Unilateral versus bilateral percutaneous pedicle screw fixation in minimally invasive transforaminal lumbar interbody fusion. Neurosurg. Focus. 35, E11 (2013).
Nie, T. et al. In vivo dynamic motion characteristics of the lower lumbar spine: L4-5 lumbar degenerative disc diseases undergoing unilateral or bilateral pedicle screw fixation combined with Tlif. J. Orthop. Surg. Res. 14, 171 (2019).
Kim, T. H., Lee, B. H., Moon, S. H., Lee, S. H. & Lee, H. M. Comparison of adjacent segment degeneration after successful posterolateral fusion with unilateral or bilateral pedicle screw instrumentation: A minimum 10-Year Follow-Up. Spine J. 13, 1208–1216 (2013).
Zhu, H. F., Wang, G. L., Zhou, Z. J. & Fan, S. W. Prospective study of Long-Term effect between multifidus muscle bundle and conventional open approach in One-Level posterior lumbar interbody fusion. Orthop. Surg. 10, 296–305 (2018).
Junhui, L. et al. Comparison of pedicle fixation by the Wiltse approach and the conventional posterior open approach for thoracolumbar fractures, using mri, histological and electrophysiological analyses of the multifidus muscle. Eur. Spine J. 26, 1506–1514 (2017).
Xie, T. et al. Minimally invasive oblique lateral lumbar interbody fusion combined with anterolateral screw fixation for lumbar degenerative disc disease. World Neurosurg. 135, e671–e678 (2020).
Acknowledgements
This study was supported by Ningxia Provincial Key Research and Development Planed Projects (No.2023BEG02017); General Hospital of Ningxia Medical University Medical Engineering Special Project (No. NYZYYG-005).
Author information
Authors and Affiliations
Contributions
Z.W., and W.G. wrote the manuscript. W.Y., X.L., S.L., and J.Z. analysed data. Z.G. designed experiments. All authors revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, Z., Guo, W., Yang, W. et al. Mid-term efficacy of OLIF combined with unilateral pedicle screw fixation in the treatment of lumbar degenerative diseases. Sci Rep 15, 18252 (2025). https://doi.org/10.1038/s41598-025-02414-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-02414-z