Abstract
Chronic obstructive pulmonary disease (COPD) is a heterogeneous condition, with varying clinical phenotypes and prognoses. Regulatory T cells (Tregs), particularly CD4+FOXP3+ T cell subpopulations, are crucial in modulating immune responses. This study investigates the distribution of two CD4+FOXP3+ T cell subpopulations in bronchoalveolar lavage fluid (BALF) from COPD patients and their association with disease phenotypes and prognosis. Patients were classified into Type A (lower frequencies of inflammatory FOXP3lo T cells) and Type B (higher frequencies of inflammatory FOXP3lo T cells). Type B COPD patients, who demonstrated more severe emphysema, heightened inflammatory responses, faster lung function decline, and more pronounced osteoporosis, showed a significant increase in FOXP3lo non-suppressive T cells. In contrast, Type A patients exhibited a higher proportion of FOXP3hi Treg cells, which correlated with milder disease phenotypes. The distinct distribution of CD4+FOXP3+ T cell subpopulations provides insights into the progression of COPD and suggests that these cells could serve as potential biomarkers for disease severity and prognosis. Further research may offer new therapeutic avenues by targeting these Treg subpopulations in COPD management.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a major global health concern and one of the leading causes of morbidity and mortality worldwide1,2. It is characterized by persistent respiratory symptoms and airflow limitation, primarily caused by significant exposure to noxious particles or gases, most notably tobacco smoke. Despite advances in treatment, the progressive nature of COPD often leads to frequent hospitalizations, decreased quality of life, and premature death, making it a significant public health burden3. The heterogeneity of the disease, ranging from chronic bronchitis to emphysema, complicates both diagnosis and management, as clinical outcomes can vary significantly between patients. Importantly, these varying clinical phenotypes of COPD may be driven by distinct underlying immunological mechanisms, contributing to the variability in disease progression and prognosis4,5,6.
Growing evidence suggests that the immune system’s response to lung self-antigens continues to drive inflammation, even long after the initial trigger of cigarette smoke has been removed7. This adaptive immune activity plays a crucial role in sustaining the disease process, with dysregulation of immune responses contributing to both the susceptibility to and severity of the disease8,9. Among the immune cells involved, regulatory T cells (Tregs), characterized by the expression of FOXP3, are essential in maintaining immune homeostasis by suppressing excessive inflammation10,11.
Most existing studies define Tregs as a single cell population, and the results are inconsistent12,13,14. This inconsistency is primarily due to variations in the criteria used for cell definition and the heterogeneity of the diseases being studied. More recently, Tregs can be categorized into three phenotypic subsets: naive Tregs (CD45RA+FOXP3lo), effector Tregs (CD45RA-FOXP3hi), and non-suppressive Tregs (CD45RA-FOXP3lo). These subsets differ in their functional capacities, with effector Tregs being highly suppressive and stable, while non-suppressive Tregs secrete pro-inflammatory cytokines15. This functional distinction among Treg subpopulations has been observed in other diseases, such as colorectal cancer, where higher frequencies of inflammatory FOXP3lo T cells (Type B) are associated with better prognosis compared to cancers dominated by FOXP3hi suppressive T cells (Type A), which correlate with poorer outcomes16. This underscores the significance of Treg subpopulation balance in determining disease prognosis.
In this study, we aim to investigate the distribution of CD4+FOXP3+ T cell subpopulations in BALF from COPD patients, with a focus on understanding their relationship to different clinical phenotypes and disease prognosis. By categorizing patients into Type A (lower frequencies of inflammatory FOXP3lo T cells) and Type B (higher frequencies of inflammatory FOXP3lo T cells), we found that the differential distribution of these CD4+FOXP3+ subsets is significantly associated with disease severity, particularly in patients with more severe emphysema and faster declines in lung function. These findings suggest that CD4+FOXP3+ T cell subpopulations could serve as potential biomarkers for assessing COPD progression and prognosis, offering new avenues for targeted therapeutic interventions in COPD management.
Materials and methods
Patient enrollment and study design
This study recruited 15 healthy volunteers and 41 COPD patients from the General Hospital of Ningxia Medical University, China. COPD diagnosis and severity were determined in accordance with the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines17. Patients with a history of asthma, allergic rhinitis, infections, malignancies, autoimmune or other immune-related diseases were excluded. Those receiving antibiotics, systemic steroids, chemotherapeutics, or immunosuppressants within four weeks prior to enrollment were also excluded. No COPD patient had experienced respiratory infections or acute exacerbations in the four weeks leading up to the study. The study protocol was approved by the Ethics Committee and Medical Faculty of Ningxia Medical University (approval no. 2020 − 678) and adhered to the principles outlined in the Declaration of Helsinki. Written informed consent was obtained from all participants.
CT scan quantification of emphysema
All COPD patients had at least one high-resolution chest CT scan performed with multidetector-row scanners (Siemens Healthcare GmbH, Germany). The detailed CT scanning protocols have been published elsewhere. Emphysema quantification was based on the percentage of CT voxels with attenuation values lower than − 950 Hounsfield units, analyzed using 3DSlicer software (version 4.11.20210226, available at: https://www.slicer.org/)18.
Cell collection and processing
Peripheral blood samples were drawn from each subject into EDTA-treated tubes, followed by peripheral blood mononuclear cell (PBMC) isolation using Ficoll-Paque Plus (Amersham Biosciences). Samples were centrifuged at 400×g for 20 min at 22 °C, after which PBMCs were collected, washed twice in PBS at 300×g for 5 min at 4 °C, and resuspended for further analysis.
BALF was performed as previously outlined19. To eliminate acute smoking effects, smokers refrained from smoking for at least 12 h before the procedure. Using a flexible bronchoscope (Olympus BF-290, Tokyo, Japan) under topical lidocaine, four 50 mL aliquots of sterile saline were infused into one segment of the right middle lobe and aspirated. The first aliquot, containing central airway cells and material, was discarded. The remaining lavage fluid was filtered, washed, and resuspended at 10⁶ cells/mL in RPMI-1640 at 4 °C. All samples were processed immediately after collection.
CD4+ T cells were isolated using magnetic cell sorting with Dynabeads (Invitrogen). The purified cells were then stained with anti-CD25 and anti-CD45RA antibodies (BD Biosciences), and different T-cell subsets, including CD25+++CD45RA− (Fr. II) and CD25++CD45RA− (Fr. III), were subsequently sorted using a FACS Aria flow cytometer (BD Biosciences).
Flow cytometry analysis
Freshly isolated PBMCs were labeled with antibodies and kept at 4 °C for 30 min in darkness. Following a wash step, samples were analyzed using a BD LSRII flow cytometer (BD Biosciences, San Jose, CA, USA). Prior to surface staining, cells were incubated with human Fc receptor blocking solution (e.g., Human TruStain FcX™, BioLegend, Cat# 422302) for 10–15 min at 4 °C to minimize non-specific Fc receptor-mediated binding. For the intracellular cytokine analysis, cells were stimulated for 5 h with 20 ng/ml phorbol myristate acetate (PMA) and 1 µM ionomycin (Sigma) in the presence of Golgi-Stop (BD Biosciences). Afterward, they were fixed and permeabilized using a commercial kit (e-Bioscience, San Diego, CA, USA) as per the manufacturer’s protocol. Antibodies targeting intracellular markers such as interferon-γ (IFN-γ), IL-17, and Foxp3 were used, while extracellular markers included CD4, CD25, CD45RA. The following fluorochrome-conjugated antibodies were used for flow cytometry staining and cell sorting: anti-human CD4 (clone RPA-T4, PerCP-Cy5.5; BD Biosciences, Cat# 552838), anti-human CD25 (clone M-A251, PE; BD Biosciences, Cat# 555432), anti-human CD45RA (clone HI100, PE-Cy7; BD Biosciences, Cat# 560675), anti-human FOXP3 (clone PCH101, APC; eBioscience, Cat# 17-4776-42), anti-human IL-17 A (clone eBio64DEC17, FITC; eBioscience, Cat# 11-7179-42), and anti-human IFN-γ (clone 4 S.B3, PE-Cy7; eBioscience, Cat# 25-7319-82). Single-stained controls were used for cytometer setup and compensation, and appropriate isotype controls were included to assess non-specific antibody binding. Flow cytometry data were analyzed using FlowJo software (version 10.8.1, BD Biosciences; available at: https://www.flowjo.com/).
T-Cell proliferation assays
CD4+CD25− responder cells (5 × 10⁴) derived from healthy donors were labeled with carboxyfluorescein succinimidyl ester (CFSE, Molecular Probes) and cocultured with 5 × 10⁴ CD45RA−CD25hi and CD45RA−CD25lo regulatory T cells (Tregs) isolated from the BALF of COPD patients or from healthy controls. Cells were sorted using an Aria cell sorter and seeded onto plates coated with anti-CD3 (5 µg/mL OKT3 monoclonal antibody; e-Bioscience), along with the addition of soluble anti-CD28 (5 µg/mL; e-Bioscience). Proliferation was evaluated on day four or five by measuring CFSE dilution through flow cytometry. Markers used to sort Treg populations included anti-hCD4 (-PerCP-Cy5.5, BD Biosciences), anti-hCD25 (-PE, BD Biosciences), and anti-hCD45RA (-PE-Cy7, BD Biosciences).
Statistical analysis
Data are presented as mean ± SD or median and interquartile range, depending on distribution. For non-normally distributed data, comparisons between three groups were made using Kruskal-Wallis tests, with a significant threshold of p < 0.05. If significant, post-hoc analysis between two groups was performed using the Mann-Whitney test, with p-value corrections via Bonferroni. Spearman’s rank correlation coefficient was used for correlation analysis, with significance set at p < 0.05. All tests were two-tailed. Statistical analyses were performed using GraphPad Prism 7.0.
Results
Demographic characteristics of study subjects
A total of 41 COPD patients and 15 healthy controls were included in the study. The demographic characteristics of all subjects are summarized in Table S1. The COPD group had an average age of 66 ± 10 years, with 76% being male. The BMI of COPD patients was significantly lower (25 ± 8 kg/m²) compared to healthy controls (28 ± 6 kg/m²). Most COPD patients were heavy smokers, with an average smoking history of 41 ± 13 pack-years, and 23% were current smokers at the time of the study. In terms of lung function, COPD patients exhibited a lower FEV1 (50% ± 22% predicted) and FEV1/FVC ratio (45% ± 15%) compared to healthy controls (94% ± 5% and 85% ± 4%, respectively).
Differential distribution and functional characteristics of CD4+FoxP3+ T cell subsets in COPD BALF: classification into type A and type B
Human CD4+FoxP3+ T cells are categorized into three functional subsets based on the expression levels of FoxP3 and CD45RA: rTreg (FoxP3loCD45RA+, Fr. I), aTreg (FoxP3hiCD45RA−, Fr. II), and a pro-inflammatory cytokine-secreting subset (FoxP3loCD45RA−, Fr. III), as previously described15. These subsets can be isolated as live cells through cell sorting, identified as CD25++CD45RA+, CD25+++CD45RA−, and CD25++CD45RA− cells, respectively (Fig. 1A). We observed a significant increase in the number of Fr-II cells in some patients, accompanied by a substantial decrease in Fr-I cells in the BALF of all COPD patients. Notably, some COPD patients had markedly higher numbers of Fr-III cells, while others did not. This observation led us to classify COPD into two distinct types: Type A and Type B, based on Fr-III frequencies in BALF (Fig. 1A). Type A was defined as having less than 11.6%, while Type B had more than 11.6%, which corresponds to the upper limit of the mean plus (2×s.d.) of Fr-III cell frequencies observed in normal BALF (n = 7). Type A patients exhibited higher percentages of Fr-II cells compared to Type B (Fig. 1B). Functionally, Fr-II cells from both COPD types displayed a strong ability to suppress the proliferation of CD4+CD25− T cells in in vitro co-cultures, whereas Fr-III cells from Type B COPD showed no such ability (Fig. 1C). Additionally, a significantly higher frequency of IL-17-secreting Fr-III cells was found in Type B compared to Type A COPD (Fig. 1D-E).
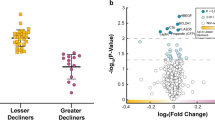
Classification of type A and type B associates with disease phenotype and status
We further investigated whether the distinct immunological profiles of Type A and Type B COPD patients correlate with differences in their clinical presentations and disease outcomes. We further investigated whether the distinct immunological profiles of Type A and Type B COPD patients were associated with differences in clinical characteristics and disease outcomes. As shown in Table 1, individuals with Type B COPD had significantly more severe emphysema, as indicated by a higher percentage of low attenuation area (LAA%) (18 ± 10% vs. 11 ± 5%, p < 0.01), and a lower body mass index (BMI) (23 ± 6 vs. 27 ± 7 kg/m², p < 0.01). They also exhibited significantly reduced oxygen saturation (92.8 ± 3.4% vs. 95.8 ± 2.9%, p < 0.05), poorer lung function including lower FEV1% predicted (43 ± 13% vs. 57 ± 15%, p < 0.01) and FEV1/FVC ratios (42 ± 10% vs. 48 ± 12%, p < 0.01), and shorter 6-minute walk distance (6MWD) (350 ± 116 m vs. 390 ± 110 m, p < 0.01). Symptom burden was greater, as reflected by higher mMRC dyspnea scores (1.8 ± 1.3 vs. 1.3 ± 1.0, p < 0.05) and total SGRQ scores (56 ± 14 vs. 46 ± 17, p < 0.01), indicating a decline in quality of life. Type B patients were also more likely to be heavy ex-smokers (Table 1) and had a higher prevalence of osteoporosis (20% vs. 13%, p < 0.01). Most participants in both groups were receiving inhaled corticosteroid (ICS) therapy, while only a small proportion (< 2%) were on oral corticosteroids (Table 1). As shown in Fig. 2; Table 2, retrospective analysis revealed that Type B patients experienced significantly more frequent COPD-related hospitalizations (1.6 vs. 0.4 per patient per year, p < 0.001), a higher number of acute exacerbations (3.2 vs. 1.0 per patient per year, p < 0.001), and a faster annual decline in FEV1 (36 ± 24 mL/year vs. 27 ± 19 mL/year, p < 0.01) over the past two years compared to Type A patients.
Discussion
Chronic obstructive pulmonary disease (COPD) involves persistent T cell-mediated inflammation, with growing evidence suggesting it shares features of an autoimmune response. Smoking-induced epithelial damage exposes lung self-antigens, driving chronic adaptive immune activity. Regulatory T (Treg) cells play a crucial role in maintaining immune tolerance, and disruptions in their function, often linked to smoking, may contribute to COPD progression20. Targeting Treg cells could offer new therapeutic strategies for managing the disease.
Clinical phenotypes and Immunologic mechanisms
This study highlights the critical role of two distinct CD4+FOXP3+ regulatory T cell (Treg) subpopulations in the progression of chronic obstructive pulmonary disease (COPD). Our findings show that the differential distribution of FOXP3hi and FOXP3lo T cells within the bronchoalveolar lavage fluid (BALF) correlates with distinct COPD phenotypes. Specifically, type A COPD, characterized by a higher proportion of suppressive FOXP3hi Tregs, represents a more controlled immune environment, which may help explain the milder disease phenotype observed in these patients. In contrast, Type B COPD, with an abundance of FOXP3lo non-Tregs, is associated with unchecked inflammation, more severe emphysema, and rapid lung function decline. This suggests that the immune dysregulation in COPD is heterogeneous, with different Treg subpopulations playing distinct roles in modulating the disease course. Different clinical phenotypes of COPD may arise from distinct immunologic mechanisms, involving imbalances in regulatory T cells (Tregs), dysregulated adaptive and innate immune responses, persistent neutrophilic inflammation, altered macrophage polarization and function, and microbial interactions within the respiratory tract21. These mechanisms contribute to the heterogeneity in disease presentation and progression. Understanding these differences is crucial for developing targeted therapeutic strategies aimed at modulating immune responses in COPD.
Potential mechanisms behind the increase in FOXP3lo non-Tregs
As shown in Fig. 1E, IL-17 production was primarily observed in fraction III (FOXP3loCD45RA−), indicating a pro-inflammatory phenotype consistent with Th17-like effector function. Previous studies have shown that FOXP3lo cells can co-express ROR-γt, the key transcription factor for Th17 differentiation15, suggesting that fraction III may represent a transitional or plastic population with Th17 potential. While their terminal fate remains unclear, these cells may either differentiate fully into Th17 cells or exhibit dual Treg/Th17 features. Given the established role of Th17 cells in COPD pathogenesis22, we speculate that this subset reflects an intermediate stage in the shift from regulatory to effector phenotype and may contribute to the Treg/Th17 imbalance observed in COPD. Further studies are warranted to clarify their role in disease mechanisms.
The underlying mechanism for the expansion of FOXP3lo non-Tregs in Type B COPD is multifactorial. One of the primary drivers is the cytokine-rich microenvironment found in COPD lungs. Pro-inflammatory cytokines—including IL-6, IL-12, IL-23, TGF-β, and TNF-α—are often elevated in chronic inflammatory conditions and can skew the Treg compartment by promoting the expansion of FOXP3lo T cells at the expense of suppressive FOXP3hi Tregs. Among these, IL-6 and TGF-β are key in initiating Th17 cell differentiation23, while IL-23 plays a critical role in stabilizing and expanding Th17 cells and enhancing their pathogenic potential24. This cytokine-induced shift enhances inflammation through the secretion of additional inflammatory cytokines like IL-17, which is associated with tissue damage, severe emphysema, and rapid lung function decline16,25. Future studies should explore the local cytokine milieu in BALF to better understand its influence on the plasticity and effector function of FOXP3lo T cells in COPD.
In addition to the cytokine milieu, tissue-specific factors play a key role in driving the imbalance of Treg subpopulations. Chronic exposure to irritants like cigarette smoke causes structural damage to the lung, which in turn triggers the release of growth factors such as TGF-β. This environment favors the expansion of FOXP3lo non-Tregs and perpetuates a feedback loop of tissue destruction, promoting the development of emphysema and more pronounced inflammatory responses in Type B patients25.
Epigenetic instability is another critical factor that may contribute to the expansion of FOXP3lo Tregs. FOXP3lo non-Tregs cells exhibit incomplete demethylation of the FOXP3 gene, resulting in a less stable phenotype and reduced suppressive capacity. This instability, influenced by the chronic inflammatory and oxidative stress conditions in COPD, drives the expansion of non-suppressive Tregs, which in turn accelerates lung function decline and exacerbates inflammation26.
Although direct evidence linking microbial influences on Type B COPD is still lacking, it is speculated that chronic bacterial infections or lung colonization could contribute to immune dysregulation in this phenotype27,28. Persistent immune activation triggered by microbial presence may potentially drive the expansion of IL-17-secreting cells29, such as Th17 cells and FOXP3lo non-Tregs. This mechanism is similar to that observed in colorectal cancer, where bacterial pathogens promote the expansion of inflammatory Tregs, thus worsening the disease’s inflammatory landscape30.
Previous studies and novelty of observations
Research on Tregs in COPD has produced mixed results due to methodological challenges and the heterogeneity of disease phenotypes. Prior studies often treated Tregs as a single group, overlooking functional subpopulations. Our study addresses this gap by examining FOXP3hi Tregs and FOXP3lo non-Tregs in BALF, revealing that elevated FOXP3lo non-Tregs in Type B COPD are linked to severe emphysema and faster lung decline, while Type A COPD shows higher FOXP3hi Tregs, indicating better immune control. These findings highlight the immunological diversity of COPD and offer new insights for personalized therapies targeting Treg subsets. Specifically, the balance between FOXP3hi and FOXP3lo T cells could serve as a valuable biomarker for predicting disease progression. A higher proportion of FOXP3lo non-Tregs correlates with more severe outcomes, such as faster lung function decline and greater emphysema, suggesting that this subset may identify high-risk patients. This could inform treatment strategies, such as targeting immune dysregulation with IL-17 inhibitors. While the role of FOXP3hi Tregs in corticosteroid response remains uncertain, further research is needed to better understand how Treg subsets influence treatment outcomes. Ultimately, using Treg distribution as a biomarker could lead to more precise patient stratification and personalized treatments, though further studies are required to confirm its clinical utility.
Potential limitations
One of the key strengths of this study is its novel exploration of Treg subpopulations in COPD, yet certain limitations must be acknowledged. First, the study’s cross-sectional design limits the ability to draw definitive conclusions about causality between Treg subset distribution and COPD progression. While we identified significant correlations, further longitudinal studies are needed to confirm whether changes in Treg subpopulations directly influence disease outcomes over time. Additionally, the relatively small sample size, particularly when analyzing subgroups of COPD phenotypes, may restrict the generalizability of our findings. Moreover, patients did not discontinue their inhaled corticosteroid (ICS) treatment prior to sample collection, and since ICS can modulate immune responses, including Treg function and phenotype, we cannot fully exclude its potential influence on the observed results. Future studies involving corticosteroid-naïve patients or standardized treatment washout protocols will be important to clarify this effect. Finally, although we provide insights into the potential role of FOXP3lo non-Treg cells as a biomarker for disease severity, functional assays exploring the mechanistic pathways by which these cells contribute to inflammation would strengthen the interpretation of our data. Despite these limitations, our study offers important preliminary evidence that CD4+FOXP3+ T cell subpopulations could serve as biomarkers for COPD prognosis, paving the way for future research in this area.
Conclusion
The increased presence of FOXP3lo non-Treg cells in Type B COPD is driven by a combination of factors, including the local cytokine microenvironment, tissue-specific signals, epigenetic instability, and microbial influences. These mechanisms are strongly linked to the more severe clinical phenotype seen in Type B patients, characterized by extensive tissue damage, systemic inflammation, and rapid disease progression. Targeting the pathways that regulate FOXP3lo non-Treg cells expansion may offer new therapeutic strategies for mitigating inflammation and improving clinical outcomes in COPD.
COPD classification based on the phenotypic and functional variability of CD4+FOXP3+ cells in BALF. (A) Representative flow cytometry plots showing CD45RA and FOXP3 staining in CD4+ T cells. (B) Quantification of total FOXP3+ cells and the frequency of each fraction among CD4+ T cells in PBMCs (n = 15), BALF (n = 8), type A COPD (n = 19), and type B COPD (n = 22). (C) Flow cytometry plots from three independent experiments illustrating the suppressive function of CD4+CD25+FOXP3+ T cells in type A (top) and type B (bottom) COPD. (D) Flow cytometry plots depicting IL-17 production by PMA- and ionomycin-stimulated Fr-II and Fr-III CD4+ T cells. (E) Mean fluorescence intensity (MFI) of IL-17 expression in Fr-II and Fr-III T cell subsets from BALF of Type A and Type B COPD patients. Data are presented as mean ± SD.
Retrospective analysis of clinical outcomes over the past 2 years for patients with Type A and Type B COPD. Panel A shows the decline in forced expiratory volume in 1 s (FEV1) expressed as a percentage change from the baseline measured two years ago. Panels B and C illustrate the frequency of exacerbations and hospitalizations per patient per year (PPPY) over the same two-year period. Data are presented as mean ± SD.
Data availability
Data and materials are available upon request by contacting the correspondence author Jia Hou ([email protected]).
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- BALF:
-
Bronchoalveolar lavage fluid
- Tregs:
-
Regulatory T cells
- PBMC:
-
Peripheral blood mononuclear cell
References
Ahmad, F. B. & Anderson, R. N. The leading causes of death in the US for 2020. JAMA 325 (18), 1829–1830 (2021).
Prevalence and attributable health burden of chronic respiratory diseases. 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet Respir Med. 8 (6), 585–596 (2020).
Webber, E. M., Lin, J. S. & Thomas, R. G. Screening for chronic obstructive pulmonary disease: updated evidence report and systematic review for the US preventive services task force. JAMA 327 (18), 1812–1816 (2022).
Eriksson Strom, J. et al. Airway regulatory T cells are decreased in COPD with a rapid decline in lung function. Respir Res. 21 (1), 330 (2020).
Tan, D. B. et al. Impaired function of regulatory T-cells in patients with chronic obstructive pulmonary disease (COPD). Immunobiology 219 (12), 975–979 (2014).
Lee, S. H. et al. Antielastin autoimmunity in tobacco smoking-induced emphysema. Nat. Med. 13 (5), 567–569 (2007).
Bonarius, H. et al. Antinuclear autoantibodies are more prevalent in COPD in association with low body mass index but not with smoking history. THORAX 66 (2), 101–107 (2011).
Cosio, M. G., Saetta, M. & Agusti, A. Immunologic aspects of chronic obstructive pulmonary disease. N. Engl. J. Med. 360 (23), 2445–2454 (2009).
Núñez, B. et al. Anti-tissue antibodies are related to lung function in chronic obstructive pulmonary disease. Am. J. Respir. Crit Care Med. 183 (8), 1025–1031 (2011).
Sakaguchi, S. Naturally arising Foxp3-expressing CD25 + CD4 + regulatory T cells in immunological tolerance to self and non-self. Nat. Immunol. 6 (4), 345–352 (2005).
Wing, J. B., Tanaka, A. & Sakaguchi, S. Human FOXP3(+) regulatory T cell heterogeneity and function in autoimmunity and Cancer. Immunity 50 (2), 302–316 (2019).
Barcelo, B. et al. Phenotypic characterisation of T-lymphocytes in COPD: abnormal CD4 + CD25 + regulatory T-lymphocyte response to tobacco smoking. Eur. Respir J. 31 (3), 555–562 (2008).
Bhat, T. A., Panzica, L., Kalathil, S. G. & Thanavala, Y. Immune dysfunction in patients with chronic obstructive pulmonary disease. Ann. Am. Thorac. Soc. 12 (Suppl 2), S169–175 (2015).
Dancer, R. & Sansom, D. M. Regulatory T cells and COPD. THORAX 68 (12), 1176–1178 (2013).
Miyara, M. et al. Functional delineation and differentiation dynamics of human CD4 + T cells expressing the FoxP3 transcription factor. Immunity 30 (6), 899–911 (2009).
Saito, T. et al. Two FOXP3(+)CD4(+) T cell subpopulations distinctly control the prognosis of colorectal cancers. Nat. Med. 22 (6), 679–684 (2016).
Agusti, A. et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Am. J. Respir Crit. Care Med. 207 (7), 819–837 (2023).
Fedorov, A. et al. 3D slicer as an image computing platform for the quantitative imaging network. Magn. Reson. Imaging. 30 (9), 1323–1341 (2012).
Tanino, M. et al. Increased levels of interleukin-8 in BAL fluid from smokers susceptible to pulmonary emphysema. Thorax 57 (5), 405–411 (2002).
Hou, J. & Sun, Y. Role of regulatory T cells in disturbed immune homeostasis in patients with chronic obstructive pulmonary disease. Frontiers Immunology ; 11. (2020).
Barnes, P. J. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J. Allergy Clin. Immunol. 138 (1), 16–27 (2016).
Lamela, J. & Vega, F. Immunologic aspects of chronic obstructive pulmonary disease. N. Engl. J. Med. 361 (10), 1024–1024 (2009).
McGeachy, M. J. et al. TGF-beta and IL-6 drive the production of IL-17 and IL-10 by T cells and restrain T(H)-17 cell-mediated pathology. Nat. Immunol. 8 (12), 1390–1397 (2007).
Langrish, C. L. et al. IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J. Exp. Med. 201 (2), 233–240 (2005).
Rubinstein, M. R. et al. Fusobacterium nucleatum promotes colorectal carcinogenesis by modulating E-cadherin/β-catenin signaling via its FadA adhesin. Cell. Host Microbe. 14 (2), 195–206 (2013).
Ohkura, N. et al. T cell receptor stimulation-induced epigenetic changes and Foxp3 expression are independent and complementary events required for Treg cell development. Immunity 37 (5), 785–799 (2012).
Gomez, C. & Chanez, P. The lung microbiome: the perfect culprit for COPD exacerbations? Eur. Respir J. 47 (4), 1034–1036 (2016).
Wang, Z. et al. Lung Microbiome dynamics in COPD exacerbations. Eur. Respir J. 47 (4), 1082–1092 (2016).
Yadava, K. et al. Microbiota promotes chronic pulmonary inflammation by enhancing IL-17A and autoantibodies. Am. J. Respir Crit. Care Med. 193 (9), 975–987 (2016).
Kostic, A. D. et al. Fusobacterium nucleatum potentiates intestinal tumorigenesis and modulates the tumor-immune microenvironment. Cell. Host Microbe. 14 (2), 207–215 (2013).
Funding
This work was supported by the National Natural Science Foundation of China (81360008), Ningxia Key Research and Development Project (2021BEG03079), Ningxia Natural Science Foundation (Grants No. 2024AAC02075).
Author information
Authors and Affiliations
Contributions
J. H. contributed as the primary investigator and was responsible for designing the study and analyzing the data. J.Z. was responsible for the preparation and analysis of blood samples, as well as manuscript preparation. H. H. provided scientific expertise and assisted with manuscript preparation. W. M., D. W., and X. P. participated in subject recruitment. X. G. was responsible for the emphysema quantification assay, statistical analyses, and manuscript preparation. J. C. contributed to data analysis and manuscript preparation. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Research ethics approval was obtained from the Ethics Committee of General Hospital of Ningxia Medical University. All subjects provided written informed consent.
Consent for publication
Not applicable.
Generative AI use in scientific writing
In the preparation of this manuscript, chatGPT4 was employed exclusively for language editing to improve clarity and coherence. The scientific content, data analysis, interpretation, and conclusions were developed independently by the authors. All authors have reviewed and taken full responsibility for the content of the publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hou, J., Zhao, J., He, H. et al. Distribution of two CD4+FOXP3+ T cell subpopulations reflects disease phenotypes and prognosis in COPD. Sci Rep 15, 17721 (2025). https://doi.org/10.1038/s41598-025-02935-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-02935-7