Abstract
Brain and central nervous system (CNS) cancers pose a substantial global health challenge, with considerable variation in incidence, prevalence, mortality, and disability-adjusted life years (DALYs) across regions and demographics. This study comprehensively examines the global, regional, and national burden of brain and CNS cancers from 1990 to 2021 and projects trends through 2041, aiming to inform targeted prevention strategies and resource allocation in healthcare systems worldwide. Data were derived from the Global Burden of Disease 2021 study, covering 204 countries. The study analyzed age-standardized rates for incidence (ASIR), prevalence (ASPR), mortality (ASMR) and DALYs (ASDR), stratified by sex, age and socio-demographic index (SDI) quintiles. The estimated annual percentage change (EAPC) and joinpoint regression analysis were employed to assess temporal trends in cancer burden metrics from 1990 to 2021. Das Gupta’s decomposition method was used to quantify the relative contributions of population growth, aging and epidemiological changes on the cancer burden. Bayesian age-period-cohort models projected future trends through 2041. From 1990 to 2021, the global ASIR for brain and CNS cancers increased from 3.75 (95% UI: 3.21 to 4.21) to 4.28 (95% UI: 3.71 to 4.88) per 100,000, while the ASPR increased from 8.66 (95% UI: 7.55 to 9.53) to 12.01 (95% UI: 10.54 to 13.52). The ASMR remained stable at approximately 3.05, and the ASDR declined from 119.88 (95% UI: 99.23 to 137.57) to 107.91 (95% UI: 91.74 to 125.59). Higher incidence and prevalence were observed in high SDI regions (ASIR: 6.38, 95% UI: 6.08 to 6.64; ASPR: 26.10, 95% UI: 24.84 to 27.19) compared to low SDI regions (ASIR: 1.43, 95% UI: 1.00 to 1.82; ASPR: 2.53, 95% UI: 1.76 to 3.24), with males (ASIR: 4.72, 95% UI: 3.68 to 5.76) experiencing higher rates than females (ASIR: 3.88, 95% UI: 3.43 to 4.35). Population growth and aging were primary drivers of the increased cancer burden, particularly in high SDI regions. Despite historical increases, recent years have shown a deceleration in growth rates, which informs future projections suggesting a gradual decline in age-standardized metrics by 2041, although older populations will continue to bear higher rates compared to younger age groups. This study highlights the continuing global burden of brain and CNS cancers, with notable disparities by sex, age, and SDI. While age-standardized metrics are projected to decrease over the next two decades, the absolute burden may continue to increase due to demographic changes. These findings highlight the need for improved early detection and targeted interventions, particularly in aging populations and regions undergoing epidemiological transitions.
Similar content being viewed by others
Introduction
Brain and central nervous system (CNS) cancers represent a formidable global health challenge despite their relatively low incidence compared to other malignancies. Though less common, these neoplasms have a disproportionate impact due to their aggressive nature, poor prognosis, and significant effects on neurological function1. Despite tremendous advances in medicine, early detection and effective treatment remain limited2,3, leading to high case fatality rates and considerable contribution to disability-adjusted life years (DALYs)4. The global burden varies by region and demographic factors, such as age, sex, and socioeconomic status5. High-income countries report higher incidence rates due to advanced diagnostic capabilities, environmental exposures, genetic predispositions, lifestyle differences, and comprehensive cancer registration systems. Conversely, low- and middle-income countries likely underestimate their burden due to limited healthcare infrastructure, inadequate neuroimaging access, insufficient pathology services, and fragmented cancer registration systems6,7. This underreporting creates challenges in accurately comparing disease burdens across socioeconomic contexts and may mask a more extensive global problem than currently documented.
The Global Burden of Disease (GBD) study provides a vital framework for analyzing trends in brain and CNS cancers across 204 countries over 32 years, identifying patterns in incidence, prevalence, and mortality, and examining the effects of population aging and growth8. These analyses are crucial for developing targeted strategies to mitigate the rising cancer burden, particularly in resource-limited regions4. However, some knowledge gaps persist in understanding the global distribution and trends of these cancers. The relationship between socioeconomic development and cancer burden requires further exploration, particularly regarding how diagnostic capabilities and reporting systems influence observed patterns. Additionally, comprehensive projections of future burden that incorporate changing demographics across different socioeconomic contexts remain limited, hindering effective long-term health planning. This study aims to comprehensively assess the global, regional, and national burden of brain and CNS cancers from 1990 to 2021 using GBD 2021 study data, focusing on temporal trends stratified by sex, age, and socio-demographic index (SDI). The analysis examines patterns across different demographic and socioeconomic contexts and projects future trends through 2041. By quantifying the relative contributions of population aging, growth, and epidemiological changes to the observed cancer burden, this study provides valuable insights to guide the development of effective public health policies. Throughout our analysis, findings are interpreted with careful consideration of potential disparities in diagnostic and reporting capabilities across regions, acknowledging this as an important factor when comparing cancer burden in different socioeconomic contexts.
Methods
Data sources
This study employed deidentified, publicly accessible data from the GBD 2021 database (https://ghdx.healthdata.org/gbd-2021), which is maintained by the Institute for Health Metrics and Evaluation. The GBD 2021 study utilized spatiotemporal Gaussian process regression to model the input data, thereby facilitating the smoothing of incomplete datasets across various domains, including age, time, and ___location9. Brain and CNS cancers cases were identified using the International Classification of Diseases, Tenth Revision (ICD-10) codes C70-C70.1 and C70.9-C72.9. As the study did not involve any individually identifiable patient information, the requirement for obtaining informed consent was not applicated to this analysis.
Brain and CNS cancers indicators and social demographic variables
The present analysis employed a variety of metrics in order to quantify the global impact of brain and CNS cancers. Incidence was measured as the occurrence of newly diagnosed cases during specific timeframes, representing how frequently these cancers emerge in populations. Prevalence data captured the total existing cases at particular time points, illustrating how widespread these conditions are throughout communities. The mortality metric documented fatalities attributed to these cancers. The comprehensive DALYs metric combines mortality and disability measures to provide an integrated assessment of the total health burden.
For the purpose of contextual analysis, the SDI, a development indicator combining economic prosperity (per capita income), educational attainment (average schooling years), and demographic transition (fertility rates among those under 25), was incorporated. This composite scale ranges from 0 to 1, with ascending values corresponding to higher levels of development. To facilitate comparative analysis, nations were stratified into five development categories: high, high-middle, middle, low-middle, and low SDI regions. The epidemiological examination further disaggregated data by demographic characteristics including gender, age brackets, geographical ___location, and development classification to uncover patterns in how brain and CNS cancer burden varies across different population segments.
Data processing
The GBD 2021 study provides extensive epidemiological measurements for hundreds of health conditions across the global landscape covering 204 countries and territories from 1990 to 2021. All statistical analyses were performed using R version 4.3.3. The Global Health Data Exchange platform was utilized to access time-series information, with annual figures and age-standardized rates (per 100,000) for brain and CNS cancer incidence (ASIR), prevalence (ASPR), mortality (ASMR), and DALYs (ASDR) being gathered. These were then stratified by demographic categories, including sex, age groups, geographical regions, SDI classifications, individual countries and territories. The investigation concentrated on age-standardized metrics in order to ensure valid comparisons across populations with differing age structures. Uncertainty intervals (UIs) were calculated from 1000 draws for each quantity. The 95% UIs were determined by selecting the 25 th and 975 th draws from this ordered distribution, representing the lower and upper bounds of the interval, respectively.
To quantify temporal trends over the entire study period from 1990 to 2021, estimated annual percentage change (EAPC) was calculated using a linear regression model of the natural logarithm of the age-standardized rates (ASIR, ASPR, ASMR, and ASDR). The year was used as the independent variable, represented by the equation: ln(rate) = α + β × year, where α denotes the intercept and β represents the regression coefficient. The EAPC was then calculated using the formula EAPC = (e^β − 1) × 100%, which converts the regression coefficient to a percentage change per year. This transformation provides an intuitive measure of the average rate of change throughout the study period (1990–2021). For each EAPC value, 95% confidence intervals (CIs) were computed to assess statistical significance and precision of the estimates. A positive EAPC indicates an increasing trend over time, while a negative value suggests a decreasing trend.
For identifying and characterizing changes in trends over specific time segments within the study period, joinpoint regression analysis was performed using the Joinpoint Regression Program (Version 5.2.0.0) as previously reported10. This method identifies statistically significant turning points (joinpoints) and calculates segmented annual percent changes (APCs).
Decomposition analysis
To identify the factors driving changes in brain and CNS cancers burden between 1990 and 2021, Das Gupta’s decomposition method was applied to quantify contributions from population ageing, population growth, and epidemiological changes. A comprehensive set of age-standardized metrics (incidence, prevalence, mortality, and DALYs) along with population data stratified by age cohorts for both time points were collected as shown in previous study10. By creating counterfactual scenarios that systematically isolated each component while holding others constant, the individual contributions of these components to overall burden changes could be determined. The analysis was conducted separately across sex categories and SDI quintiles, revealing how these driving factors varied across different demographic contexts. This methodological approach enabled the determination of whether the observed changes were primarily attributable to demographic transitions or evolving disease patterns. Positive values were assigned to factors that increased disease burden, while negative values represented elements that reduced it.
Bayesian age-period-cohort (BAPC) projections
In order to forecast the future trajectory of brain and CNS cancer burden from 2022 to 2041, BAPC modelling techniques were implemented11. This approach enabled the incorporation of age effects (biological susceptibility), period effects (temporal trends affecting all age groups), and cohort effects (generation-specific risk patterns) simultaneously. The historical cancer metrics from 1990 to 2021 were integrated with demographic projections from GBD population forecasts. Standardization weights were calculated using the GBD world population standard to ensure comparability across time periods. Separate models were constructed for males and females in order to account for gender-specific epidemiological patterns. The BAPC framework employed 5-year age aggregations to balance granularity with statistical stability. The modelling process generated 20-year projections of incidence, prevalence, mortality and DALYs, providing both age-specific estimates and age-standardized summaries. The final outputs included central estimates with corresponding measures of uncertainty (standard deviations) for each demographic segment, all expressed as rates per 100,000 population. The BAPC prediction was implemented using the BAPC (version 0.0.36) and INLA (version 23.06.29) packages in R.
Results
Global incidence and prevalence rates of brain and CNS cancers
In 2021, the ASIR of brain and CNS cancers was 4.28 (95% UI: 3.71 to 4.88) per 100,000 population, representing an increase from 3.75 (95% UI: 3.21 to 4.21) in 1990 (Table 1). Similarly, the global ASPR rose from 8.66 (95% UI: 7.55 to 9.53) to 12.01 (95% UI: 10.54 to 13.52) per 100,000 over the same period. The EAPC values of 0.44 (95% CI: 0.4 to 0.49) for incidence and 1.18 (95% CI: 1.12 to 1.24) for prevalence indicate a steady upward trajectory throughout the 32-year study period. However, joinpoint regression analysis revealed important recent trend changes that challenge this apparent steady increase. Most notably, both incidence and prevalence showed significant recent declines, with incidence decreasing by −0.72 from 2018 to 2021 and prevalence declining by −0.85 during the same period (Table S1-S2). This recent downturn represents a notable shift from the significant increases observed in the preceding period (2003–2018 for incidence: 0.44; 2004–2018 for prevalence: 1.17).
When analyzed by sex, males consistently exhibited higher disease burden than females. In 2021, males had 190,130 new cases with an ASIR of 4.72 (95% UI: 3.68 to 5.76) compared to 167,353 new cases with an ASIR of 3.88 (95% UI: 3.43 to 4.35) for females (Table 1, Fig S1A). The EAPC values for incidence were 0.42 (95% CI: 0.38 to 0.47) for males and 0.47 (95% CI: 0.43 to 0.51) for females. The temporal analysis demonstrated that both sexes experienced significant recent declines in incidence during 2018–2021, though the magnitude differed substantially between males (−0.77) and females (−0.53) (Table S1). This contemporary downturn contrasts notably with the preceding growth phase, where females exhibited a more consistent upward trajectory (0.43 from 1997 to 2018) while males displayed greater temporal variability. Prevalence patterns showed similar sex differences, with males having 490,044 cases (ASPR: 12.28, 95% UI: 9.72 to 15.05) and females having 485,235 cases (ASPR: 11.76, 95% UI: 10.48 to 13.28) in 2021. The EAPC values for prevalence were 1.09 (95% CI: 1.03 to 1.15) for males and 1.28 (95% CI: 1.21 to 1.34) for females (Table 1, Fig S1B).
Examination across SDI quintiles revealed substantial disparities. High SDI regions reported the highest rates with an ASIR of 6.38 (95% UI: 6.08 to 6.64) and ASPR of 26.10 (95% UI: 24.84 to 27.19) in 2021, both having increased notably since 1990 (Table 1, Fig S1C-F). Remarkably, joinpoint analysis revealed that High SDI regions experienced the most pronounced recent decline, with incidence decreasing by −1.77 during 2018–2021 (Table S1). This sharp recent decrease contrasts markedly with the increases observed in the preceding period (2004–2018: 0.62), suggesting a significant epidemiological transition in the most developed regions. In contrast, low SDI regions had the lowest rates with an ASIR of 1.43 (95% UI: 1.00 to 1.82) and ASPR of 2.53 (95% UI: 1.76 to 3.24). When comparing age groups, the highest incidence and prevalence were observed in older populations, with rates increasing progressively with age (Fig S2, Table S3).
Global mortality and DALYs rates of brain and CNS cancers
The global ASMR remained relatively stable over the study period, with a slight increase from 3.04 (95% UI: 2.58 to 3.45) per 100,000 in 1990 to 3.06 (95% UI: 2.62 to 3.50) in 2021 (Table 2). Concurrently, the ASDR decreased from 119.88 (95% UI: 99.23 to 137.57) to 107.91 (95% UI: 91.74 to 125.59) per 100,000, with an EAPC of −0.37 (95% CI: −0.63 to −0.12). The segmented trend analysis illuminated notable recent improvements across both mortality and disability metrics. The 2018–2021 period witnessed substantial mortality reductions (−0.86) alongside even more dramatic decreases in DALYs (−1.21) (Table S4-S5). This accelerated improvement trajectory represents a marked departure from the more gradual progress characterizing earlier periods.
The mortality burden showed notable sex differences, with males experiencing higher rates. In 2021, the ASMR for males was 3.54 (95% UI: 2.75 to 4.32) compared to 2.62 (95% UI: 2.31 to 2.92) for females (Table 2, Fig S3 A). The EAPC values for mortality were 0.03 (95% CI: −0.02 to 0.09) for males and − 0.03 (95% CI: −0.08 to 0.02) for females. The DALYs burden followed a similar pattern to mortality, with males having an ASDR of 122.96 (95% UI: 93.65 to 157.33) and females having 93.46 (95% UI: 82.86 to 104.06) per 100,000 (Table 2, Fig S3B). EAPC values were − 0.37 (95% CI: −0.41 to −0.33) for males and − 0.37 (95% CI: −0.47 to −0.34) for females.
Analysis by SDI quintile revealed notable disparities in mortality and DALYs. High-middle SDI regions had the highest ASMR at 3.94 (95% UI: 3.36 to 4.51) per 100,000 in 2021, followed by high SDI at 3.54 (95% UI: 3.36 to 3.68), middle SDI at 3.02 (95% UI: 2.45 to 3.65), low-middle SDI at 2.08 (95% UI: 1.68 to 2.62), and low SDI regions at 1.33 (95% UI: 0.93 to 1.69) in 2021 (Table 2, Fig S3 C). From 1990 to 2021, high SDI regions showed a declining trend in mortality with an EAPC of −0.17 (95% CI: −0.51 to 0.17), while low-middle SDI regions experienced the largest increase with an EAPC of 0.88 (95% CI: 0.68 to 1.09). Joinpoint regression analysis revealed that high SDI regions experienced fluctuating mortality trends with periods of both increase and decrease, ultimately showing a pronounced decline in the most recent period (Table S4 and S5). For DALYs, high-middle, high, and middle SDI regions showed the substantial decreases with EAPCs of −0.68 (95% CI: −0.95 to −0.40), −0.43 (95% CI: −0.75 to −0.10), and − 0.40 (95% CI: −0.63 to −0.18), respectively, while low-middle SDI regions experienced an increase with an EAPC of 0.68 (95% CI: 0.47 to 0.90) (Table 2, Fig S3D-F). When examining age distributions, mortality and DALYs rates were mainly among individuals aged 60 years and above, highlighting the substantial burden of brain and CNS cancers in older populations (Fig S4, Table S6).
Geographical distribution of incidence, prevalence, mortality, and DALYs
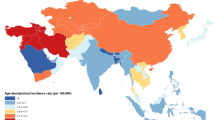
Considerable geographical variation was observed in the burden of brain and CNS cancers in 2021. Norway recorded the highest ASIR at 14.96 per 100,000 (95% UI: 13.93 to 16.07), while Gambia had the lowest at 0.14 per 100,000 (95% UI: 0.09 to 0.19) (Fig. 1A, Table S3). The EAPCs for incidence rates showed diverse patterns globally, with the largest increase observed in Turkmenistan (7.44, 95% CI: 6.35 to 8.54) and the largest decrease in Greenland (−1.29, 95% CI: −1.48 to −1.11) (Fig. 1B, Table S3). The geographical distribution of prevalence rates followed a similar pattern to that of incidence rates (Fig. 1C, Table S3), with widespread increases in the EAPCs, particularly in Ecuador (7.69, 95% CI: 5.66 to 9.77), and Turkmenistan (7.51, 95% CI: 6.53 to 8.50) (Fig. 1D, Table S3).
The Age-standardized Incidence and Prevalence Rate of Brain and CNS Cancers in 204 Countries and Territories. (A) The ASIR of brain and CNS cancers in 2021. (B) The EAPC of ASIR of brain and CNS cancers from 1990 to 2021. (C) The ASPR of brain and CNS cancers in 2021. (D) The EAPC of ASPR of brain and CNS cancers from 1990 to 2021. ASIR age-standardized incidence rate, ASPR age-standardized prevalence rate, EAPC estimated annual percentage change.
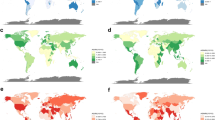
For mortality, Montenegro reported the highest rate at 7.77 per 100,000 (95% UI: 6.11 to 10.25), while Gambia again had the lowest at 0.12 per 100,000 (95% UI: 0.08 to 0.16) (Fig. 2A, Table S6). The EAPCs for mortality rates showed heterogeneous trends globally, with notable increases in Turkmenistan (7.30, 95% CI: 6.18 to 8.43), Ecuador (7.17, 95% CI: 5.12 to 9.25), and Georgia (5.42, 95% CI: 4.89 to 5.95), contrasted by decreases in Greenland (−1.63, 95% CI: −1.78 to −1.48), Republic of Korea (−1.41, 95% CI: −1.70 to −1.11), and Bahrain (−1.03, 95% CI: −1.17 to −0.90) (Fig. 2B, Table S6). The geographical distribution of DALYs rates was basically similar to that of mortality rates, with increased EAPCs in Turkmenistan (6.95, 95% CI: 5.91 to 8.00), Ecuador (6.59, 95% CI: 4.58 to 8.64), and Georgia (4.90, 95% CI: 4.36 to 5.43), contrasted by decreases in Greenland (−1.83, 95% CI: −2.01 to −1.65), Republic of Korea (−1.47, 95% CI: −1.80 to −1.14), and Luxembourg (−1.41, 95% CI: −1.54 to −1.28) (Fig. 2C-D, Table S6).
The Age-standardized Mortality and DALYs Rate of Brain and CNS Cancers in 204 Countries and Territories. (A) The ASMR of brain and CNS cancers in 2021. (B) The EAPC of ASMR of brain and CNS cancers from 1990 to 2021. (C) The ASDR of brain and CNS cancers in 2021. (D) The EAPC of ASDR of brain and CNS cancers from 1990 to 2021. ASMR age-standardized mortality rate, ASDR age-standardized DALYs rate, EAPC estimated annual percentage change, DALYs disability-adjusted life years.
Decomposition analysis of brain and CNS cancer burden
Between 1990 and 2021, the number of brain and CNS cancer incident cases increased from 173,086 to 357,482 across all SDI regions (Fig. 3A, Table S7). Population growth contributed the most to this increase with 98,494 additional cases, followed by aging with 55,337 cases, while epidemiological changes added 30,565 cases. The middle SDI regions experienced the largest absolute increase, adding 59,861 new cases during this period.
Changes in Burden of Brain and CNS Cancers from 1990 to 2021 at the Global Level and by SDI Quintile. (A-B) Changes in brain and CNS cancers incidence (A) and prevalence (B) according to population-level determinants of population growth, aging, and epidemiological change. (C-D) Changes in brain and CNS cancers deaths (C) and DALYs (D) according to population-level determinants of population growth, aging, and epidemiological change. The black dot represents the overall value of change contributed by all 3 components. For each component, the magnitude of a positive value indicates a corresponding increase in brain and CNS cancers DALYs attributed to the component; the magnitude of a negative value indicates a corresponding decrease in brain and CNS cancers attributed to the related component. SDI socio-demographic index, DALYs disability-adjusted life years.
Globally, there was substantial growth in the prevalence of brain and CNS cancers, with a rise of 540,856 cases (Fig. 3B, Table S8). The population growth accounted for 259,589 additional prevalent cases, while epidemiological changes and aging contributed 210,964 and 70,303 cases, respectively. High SDI regions experienced a notable pattern where epidemiological changes contributed 93,152 cases to prevalence.
Deaths from brain and CNS cancers exhibited an increase across in all SDI quintiles, with global deaths rising from 136,219 to 258,627 (Fig. 3C, Table S9). The primary drivers of this increase were population growth and aging, contributing 74,040 and 49,857 additional deaths, respectively, while epidemiological changes resulted in a slight reduction of 1,489 deaths. It is noteworthy that in low-middle SDI regions, the epidemiological component contributed 4,830 deaths, deviating from the global trend.
Concerning to DALYs, the global burden of brain and CNS cancers increased by approximately 3 million DALYs between 1990 and 2021 (Fig. 3D, Table S10). Population growth had the largest impact, adding 2,855,653 DALYs, while aging contributed 926,678 DALYs. Importantly, epidemiological changes reduced the DALYs burden by 828,217, partially offsetting the increases from demographic factors. However, similar to mortality patterns, in low-middle SDI regions, epidemiological changes actually increased the DALYs burden by 160,206, contrasting with the reductions seen in high, high-middle, and middle SDI regions.
Projections of future burden in the next 20 years
BAPC models were employed to forecast the burden of brain and CNS cancers through 2041, revealing notable patterns in projected trends by sex (Fig. 4). The findings of this study indicate a gradual decline in all metrics over the next two decades, with varying trajectories between females and males. For incidence rates, a decrease is projected for females from 3.874 ± 0.009 per 100,000 in 2021 to 3.387 ± 0.812 per 100,000 by 2041 (Fig. 4A, Table S11), representing a 12.6% reduction. A similar decline is predicted for male incidence rates, which are forecasted to decrease from 4.721 ± 0.011 to 4.060 ± 0.936 per 100,000 over the same period (Fig. 4A, Table S12), representing a 14.0% decrease. Prevalence rates demonstrate a comparable pattern of decline, with projections for females decreasing from 11.753 ± 0.017 to 10.200 ± 3.137 per 100,000. For males, the decline is projected to be from 12.269 ± 0.018 to 10.569 ± 3.253 per 100,000 by 2041 (Fig. 4B).
Trends and Projection for Brain and CNS Cancers by Sex from 1990 to 2041. (A-B) BAPC trends and projection for incidence rate (A) and prevalence rate (B) in females and males. (C-D) BAPC trends and projection for mortality rate (C) and DALYs rate (D) in females and males. BAPC Bayesian age-period-cohort projections, DALYs disability-adjusted life years.
Projections indicate a parallel decline in mortality rates, with female mortality rates anticipated to decrease from 2.620 ± 0.007 per 100,000 in 2021 to 2.133 ± 0.476 per 100,000 by 2041, representing an 18.6% reduction (Fig. 4C, Table S11). For males, the mortality rate is projected to decrease from 3.537 ± 0.009 to 2.885 ± 0.617 per 100,000, representing an 18.4% decline (Fig. 4C, Table S12). The most substantial reductions are projected for DALYs rates, with females expected to experience a 22.8% decrease from 93.390 ± 0.048 to 72.137 ± 17.723 per 100, 000, and males a 24.9% reduction from 122.878 ± 0.055 to 92.248 ± 20.945 per 100,000 (Fig. 4D, Table S12). Additionally, age-segmented forecasts reveal an important pattern in brain and CNS cancer burden through 2041 (Tables S13-20). Younger age groups are projected to experience substantial decreases in disease rates over time. Meanwhile, older populations aged 60 years and above will continue to have higher overall rates compared to younger groups, although their rates are also expected to decrease gradually from current levels.
Discussion
Whilst earlier studies have utilized GBD study data to examine the global burden of brain and CNS cancers12,13the present study advances this field through employing decomposition analysis to precisely quantify demographic versus epidemiological drivers of changing cancer burden, and providing comprehensive projections through 2041 across diverse populations and socioeconomic contexts. This methodological approach offers insights into not just how the burden is changing, but why it differs across regions and what factors will shape its future trajectory. The study’s key findings indicate a complex epidemiological landscape, characterized by increasing ASIR and ASPR on a global scale. This suggests a rise in the number of people living with these cancers. However, the stability of ASMR and the decline in ASDR indicate the potential for improvements in patient outcomes.
The apparent paradox of an increase in incidence alongside stable mortality requires careful interpretation, and while this pattern might suggest improved survival, alternative explanations must be considered in the absence of direct survival analysis. Firstly, earlier detection through advanced neuroimaging may identify cases that would previously have gone undiagnosed, creating a lead-time bias without necessarily changing disease outcomes14. Secondly, increased palliative care services might reduce disability burden while not affecting mortality rates15. Thirdly, changes in death certification practices or misclassification of causes could influence reported mortality patterns. Additionally, improved supportive care might reduce disability without extending survival16. These trends align with previous studies showing increased cancer detection driven by advancements in diagnostics, better reporting, and aging populations1,17,18.
The findings also revealed substantial geographical variation in disease burden, reflecting both true epidemiological differences and methodological challenges in data collection. The dramatic 107-fold difference between countries with the highest incidence rates (Norway at 14.96 per 100,000) and those with the lowest (Gambia at 0.14 per 100,000) illustrates a complex interplay of factors including true epidemiological differences, healthcare access disparities, cancer registration quality, and varying population risk profiles19,20,21. It is crucial to acknowledge that comparisons between countries with vastly different healthcare infrastructures must be interpreted with extreme caution. In low-resource settings, the absence of advanced neuroimaging technology, limited pathology services, and fragmented cancer surveillance systems may result in substantial underdiagnosis and underreporting22. This creates a situation where observed geographical patterns may partially represent disparities rather than true disease distribution. While detection capability is a major factor, these variations likely reflect a combination of both reporting differences and genuine epidemiological variation. Therefore, interpreting geographical patterns requires careful consideration of both actual disease occurrence and the varying capabilities of detection systems across different regions23,24,25. The global decline in ASDR signifies enhancements in clinical care, particularly in developed countries, although mortality persists as a challenge in low SDI regions. Recent advances in treatments such as neurosurgery, radiation, and chemotherapy may have contributed to improved outcomes17,26,27though rising prevalence emphasizes the growing need for supportive care for cancer survivors.
As has been previously observed in other report28males are subject to a disproportionately higher burden of these diseases in comparison to females, thus necessitating a more profound investigation into the potential mechanisms responsible. The underlying causes of this gender disparity are multifaceted and include, but are not limited to, hormonal factors. Evidence suggests that estrogen and progesterone may exert neuroprotective effects and influence cancer growth29,30,31. Another significant factor is occupational exposures, particularly in male-dominated industries where there is greater contact with potential carcinogens such as pesticides, solvents, ionizing radiation, and electromagnetic fields32. Additionally, genetic factors, including differences in DNA repair mechanisms and immune responses between the sexes, may also contribute to differential susceptibility30,33. It is therefore essential to understand these sex-specific risk factors in order to develop targeted prevention strategies.
In order to enhance comprehension of the factors that are contributing to the shifting patterns of cancer burden, decomposition analysis was employed. This analysis indicated that population growth and aging represent the predominant factors driving the increase in cancer burden on a global scale. However, the impact of epidemiological factors varied across different regions, underscoring important socioeconomic disparities. In high SDI regions, epidemiological shifts led to an increase in prevalence but a decrease in mortality and DALYs, indicating improvements in patient outcomes despite an increase in number of cases being detected. Conversely, in low-middle SDI regions, epidemiological factors contributed to increased mortality and DALYs, potentially reflecting growing environmental exposures or challenges in healthcare delivery5,28. These findings demonstrate how the relative contributions of demographic and epidemiological factors vary substantially across different socioeconomic contexts, underscoring the need for context-specific approaches to cancer control.
In consideration of future projections, the analysis of age-standardized rates reveals an intriguing pattern. Projections indicate a decline in age-standardized rates through 2041, which aligns with the recent downturns identified in joinpoint analysis. This apparent contradiction to the overall historical increases observed from 1990 to 2021 can be resolved through a detailed examination of recent trends. While there has been an overall increase in rates since 1990, the rate of increase has been gradually slowing in recent years, particularly in high SDI regions where rates are beginning to plateau. Meanwhile, external factors may have influenced recent data points that inform our projection models. Notably, the COVID-19 pandemic likely impacted brain cancer diagnosis patterns in 2020–2021. Evidence revealed significant decreases in brain cancer incidence during early pandemic months (March-May 2020), particularly for non-malignant cancers (50% reduction) and with disproportionate effects across demographic groups34. While aggressive cancers like glioblastoma maintained stable diagnosis rates, overall pandemic-related healthcare disruptions may have created short-term data anomalies that influence projection models. The BAPC models have detected this recent deceleration pattern and extended it forward in their projections, rather than simply continuing the long-term upward trend11. Furthermore, ongoing improvements in prevention, early detection, and treatment technologies will likely continue to develop, potentially accelerating the downward trend in coming decades32. It’s imperative to draw distinctions between absolute case numbers and age-standardized rates. While population aging and growth will likely result in an increase in the total number of cancer cases, age-standardized rates account for these demographic changes, thereby enabling the observation of the underlying disease risk patterns28. Despite the projected decreases in age-standardized rates, the age-specific analysis demonstrates that older populations will continue to experience substantially higher rates compared to younger groups, emphasizing the necessity for age-targeted approaches to cancer management.
Drawing up the findings of these exhaustive analyses, a number of pivotal research and policy priorities have been identified for future research and policy. The establishment of standardized brain cancer registries and the enhancement of diagnostics in low-resource settings is crucial for the accurate estimation of the disease burden. Moreover, the investigation of modifiable risk factors, particularly those contributing to gender disparities, in conjunction with the expansion of access to neurosurgical and radiation services in low and middle SDI regions, has the potential to address critical gaps in care. Additionally, the enhancement of supportive care programs and the development of age-appropriate interventions for older populations will be essential as the global prevalence of the condition continues to rise.
Limitation
Despite its strengths, the study has several limitations. Firstly, while GBD data are extensive, underreporting or misclassification - especially in low- and middle-income countries - may lead to an underestimation of the true burden of brain and CNS cancers. The apparent low rates in many low SDI regions likely reflect a combination of true lower incidence and substantial underdiagnosis. Secondly, the study focuses on trends without examining specific environmental, genetic or lifestyle risk factors contributing to the observed patterns. Finally, projections are based on current demographic and epidemiological trends and do not account for potential disruptive factors such as major technological breakthroughs, environmental changes, or health policy shifts that could alter future trajectories. Further research is essential to address these limitations.
Conclusion
In conclusion, this study provides valuable insights into the evolving global burden of brain and CNS cancers, highlighting regional and demographic variations. The findings underscore the complex interplay between healthcare access, diagnostic capabilities, and population demographics in shaping cancer burden. While age-standardized rates are projected to decline globally, the absolute burden may continue to rise due to demographic shifts, particularly population aging. These findings can inform the development of targeted prevention strategies, resource allocation, and healthcare planning to address the persistent challenge of brain and CNS cancers worldwide.
Data availability
The datasets analyzed during the current study are available at the https://ghdx.healthdata. org/gbd-2021.
Abbreviations
- ASDR:
-
Age-standardized DALYs rates
- ASIR:
-
Age-standardized incidence rates
- ASMR:
-
Age-standardized mortality rates
- ASPR:
-
Age-standardized prevalence rates
- BAPC:
-
Bayesian age-period-cohort
- CI:
-
Confidence interval
- CNS:
-
Central nervous system
- DALYs:
-
Disability-adjusted life years
- EAPC:
-
Estimated annual percentage change
- GBD:
-
The Global Burden of Disease
- SDI:
-
Socio-demographic index
- UI:
-
Uncertainty interval
References
Ostrom, Q. T., Francis, S. S. & Barnholtz-Sloan, J. S. Epidemiology of brain and other CNS tumors. Curr. Neurol. Neurosci. Rep. 21, 68. https://doi.org/10.1007/s11910-021-01152-9 (2021).
Delaidelli, A. & Moiraghi, A. Recent advances in the diagnosis and treatment of brain tumors. Brain Sci. 14 https://doi.org/10.3390/brainsci14030224 (2024).
Lertsumitkul, L. et al. EphA3-targeted chimeric antigen receptor T cells are effective in glioma and generate curative memory T cell responses. J. Immunother. Cancer. 12 https://doi.org/10.1136/jitc-2024-009486 (2024).
Saeidi Borojeni, H. R. et al. Disability-Adjusted life years and mortality rate attributed to brain and central nervous system Cancer in the middle East and North Africa countries. Neuroepidemiology 55, 447–459. https://doi.org/10.1159/000519281 (2021).
Ilic, I. & Ilic, M. International patterns and trends in the brain cancer incidence and mortality: an observational study based on the global burden of disease. Heliyon 9, e18222. https://doi.org/10.1016/j.heliyon.2023.e18222 (2023).
Aderinto, N., AbdulBasit Opeyemi, M., Opanike, J., Afolayan, O. & Sakaiwa, N. Navigating the challenges of neuro-oncology in africa: addressing diagnostic and treatment barriers in the region: a correspondence. Int. J. Surgery: Global Health. 6, e136–e136. https://doi.org/10.1097/gh9.0000000000000136 (2023).
Chatterjee, S. & Roy, R. Brain tumor epidemiology: updates from the USA, UK and Australia. Preprints 2021100071 https://doi.org/10.20944/preprints202110.0071.v1 (2021).
Liu, X., Cheng, L. C., Gao, T. Y., Luo, J. & Zhang, C. The burden of brain and central nervous system cancers in Asia from 1990 to 2019 and its predicted level in the next twenty-five years: burden and prediction model of CNS cancers in Asia. BMC Public. Health. 23, 2522. https://doi.org/10.1186/s12889-023-17467-w (2023).
Collaborators, G. B. D. R. F. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet 403, 2162–2203. https://doi.org/10.1016/S0140-6736(24)00933-4 (2024).
Gu, L. et al. Global, regional, and National burden of subarachnoid hemorrhage: trends from 1990 to 2021 and 20-Year forecasts. Stroke; J. Cereb. Circulation. https://doi.org/10.1161/STROKEAHA.124.048950 (2025).
Jurgens, V., Ess, S., Cerny, T. & Vounatsou, P. A bayesian generalized age-period-cohort power model for cancer projections. Stat. Med. 33, 4627–4636. https://doi.org/10.1002/sim.6248 (2014).
Fan, Y. et al. Burden and trends of brain and central nervous system cancer from 1990 to 2019 at the global, regional, and country levels. Archives Public. health = Archives Belges De Sante Publique. 80, 209. https://doi.org/10.1186/s13690-022-00965-5 (2022).
Maimaiti, A. et al. Global, regional, and National burden of brain and central nervous system cancers for males from 1990 to 2021 and its predicted level in the next 25 years. Neuroepidemiology 1–20. https://doi.org/10.1159/000541917 (2024).
Chang, E. T., Clarke, C. A., Colditz, G. A., Kurian, A. W. & Hubbell, E. Avoiding lead-time bias by estimating stage-specific proportions of cancer and non-cancer deaths. Cancer Causes Control: CCC. 35, 849–864. https://doi.org/10.1007/s10552-023-01842-4 (2024).
Pando, A. et al. Palliative care effects on survival in glioblastoma: who receives palliative care? World Neurosurg. 170, e847–e857. https://doi.org/10.1016/j.wneu.2022.11.143 (2023).
Nunna, R. S. et al. Outcomes and Patterns of Care in Elderly Patients with Glioblastoma Multiforme. World neurosurgery 149, e1026-e1037 (2021). https://doi.org/10.1016/j.wneu.2021.01.028
Huang, J. et al. The comparative burden of brain and central nervous system cancers from 1990 to 2019 between China and the united States and predicting the future burden. Front. Public. Health. 10, 1018836. https://doi.org/10.3389/fpubh.2022.1018836 (2022).
Price, M. et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the united States in 2017–2021. Neuro Oncol. 26, vi1–vi85. https://doi.org/10.1093/neuonc/noae145 (2024).
Larsen, I. et al. (ed, K.) Data quality at the Cancer registry of norway: an overview of comparability, completeness, validity and timeliness. Eur. J. cancer (Oxford England: 1990) 45 1218–1231 https://doi.org/10.1016/j.ejca.2008.10.037 (2009).
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J. Clin. 68, 394–424. https://doi.org/10.3322/caac.21492 (2018).
Jedy-Agba, E. et al. Cancer incidence in nigeria: a report from population-based cancer registries. Cancer Epidemiol. 36, e271–278. https://doi.org/10.1016/j.canep.2012.04.007 (2012).
Shakir, M. et al. Challenges to early detection of brain tumors in Low- and Middle-Income countries: A systematic review. World Neurosurg. 191, 68–80. https://doi.org/10.1016/j.wneu.2024.07.130 (2024).
Brain, G. B. D. & Other, C. N. S. C. C. Global, regional, and National burden of brain and other CNS cancer, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 18, 376–393. https://doi.org/10.1016/S1474-4422(18)30468-X (2019).
Leece, R. et al. Global incidence of malignant brain and other central nervous system tumors by histology, 2003–2007. Neuro Oncol. 19, 1553–1564. https://doi.org/10.1093/neuonc/nox091 (2017).
Knaul, F. M. et al. Alleviating the access Abyss in palliative care and pain relief-an imperative of universal health coverage: the lancet commission report. Lancet 391, 1391–1454. https://doi.org/10.1016/S0140-6736(17)32513-8 (2018).
Ladbury, C. et al. Stereotactic radiosurgery in the management of brain metastases: A Case-Based radiosurgery society practice guideline. Adv. Radiat. Oncol. 9, 101402. https://doi.org/10.1016/j.adro.2023.101402 (2024).
Gawel, A. M., Betkowska, A., Gajda, E., Godlewska, M. & Gawel, D. Current Non-Metal Nanoparticle-Based therapeutic approaches for glioblastoma treatment. Biomedicines 12 https://doi.org/10.3390/biomedicines12081822 (2024).
Thierheimer, M. et al. Mortality trends in primary malignant brain and central nervous system tumors vary by histopathology, age, race, and sex. Journal of neuro-oncology 162, 167–177 (2023). https://doi.org/10.1007/s11060-023-04279-6
Tavares, C. B. et al. Expression of Estrogen and progesterone receptors in astrocytomas: a literature review. Clin. (Sao Paulo). 71, 481–486. https://doi.org/10.6061/clinics/2016(08)12 (2016).
Carrano, A., Juarez, J. J., Incontri, D., Ibarra, A. & Guerrero Cazares, H. Sex-Specific differences in glioblastoma. Cells-Basel 10 https://doi.org/10.3390/cells10071783 (2021).
Hirtz, A., Rech, F., Dubois-Pot-Schneider, H. & Dumond, H. Estrogen signaling in healthy and tumor brain. Steroids 199, 109285. https://doi.org/10.1016/j.steroids.2023.109285 (2023).
Schaff, L. R. & Mellinghoff, I. K. Glioblastoma and other primary brain malignancies in adults: A review. JAMA 329, 574–587. https://doi.org/10.1001/jama.2023.0023 (2023).
Huang, Y. F. et al. Genetic mutation patterns among glioblastoma patients in the Taiwanese population - insights from a single institution retrospective study. Cancer Gene Ther. 31, 894–903. https://doi.org/10.1038/s41417-024-00746-y (2024).
Cioffi, G. et al. The impact of COVID-19 on 2020 monthly incidence trends of primary brain and other CNS tumors. Neuro Oncol. 26, 764–774. https://doi.org/10.1093/neuonc/noad235 (2024).
Acknowledgements
Thanks to ChatGPT and Claude for support in refining this manuscript.
Funding
This work was supported by grants from the Sichuan Province Science and Technology Support Program (2024ZYD0113, 2023 NSFSC0028 and 2022YFS0615). Luzhou Government-Southwest Medical University Strategic Cooperation Project (2021LZXNYD-D07). Clinical Research Special Project of Southwest Medical University (2024LCYXZX32).
Author information
Authors and Affiliations
Contributions
Conceptualization: J.Z., L.G., F.D., and J. Peng. Data curation and formal analysis: J.Z., L.G., F.D., F.Z., and X.Z. Methodology: J.Z., C.L., J. Pang, and B.X. Visualization and Writing - original draft: J.Z., and F.D. Writing - review & editing: X.W., J. Peng, and Y.J. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors have reviewed the final version of this manuscript and give their consent for the manuscript to be submitted and published.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhou, J., Gu, L., Du, F. et al. The global, regional, and national brain and CNS cancers burden and trends from 1990 to 2021. Sci Rep 15, 19228 (2025). https://doi.org/10.1038/s41598-025-04636-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-04636-7