Abstract
Accumulative lactate acid is a critical feature of pancreatic ductal adenocarcinoma (PDAC). Increasing evidence has demonstrated a close correlation between long non-coding RNAs (lncRNAs) and the survival of patients with PDAC. Nevertheless, research on the prognostic value of lactate-related lncRNAs in PDAC remains limited. In this study, the lactate-related lncRNAs were characterized based on their association with hypoxia-related genes in TCGA and StarBase database. Specifically, the dysregulated lactate-related lncRNAs in PDAC were identified as LA-DElncRNAs. Four LA-DElncRNAs were selected to develop clinical model, which demonstrated strong performance in survival prediction. The risk score derived from the model was identified as an independent prognostic factor for PDAC. Importantly, patients in the low-risk groups displayed more favorable prognoses compared to those in the high-risk groups. Moreover, patients with different risk scores showed distinct immune subtypes and variations in the levels of immune checkpoints. FAM225B was the most significant LA-DElncRNA associated with prognosis in Cox analysis, and the biological role of FAM225B was investigated both in vitro and in vivo. Knockdown of FAM225B, a significant LA-DElncRNAs, attenuated the proliferation and invasion of PDAC cells. In conclusion, the assessment model based on LA-DElncRNAs holds promise as a potential prognostic biomarker of PDAC patients. The identified four LA-DElncRNAs could help unravel the mechanisms underlying pancreatic tumorigenesis and identify novel molecular targets for treatment.
Similar content being viewed by others
Introduction
Pancreatic ductal adenocarcinoma (PDAC) ranks among the most lethal human malignancies worldwide1. Although considerable progress in diagnostic and therapeutic approaches, the prognosis for PDAC remains extremely grim2. The aggressive invasion, metastasis, and treatment resistance exhibited by PDAC cells contribute to rapid disease progression and unfavorable patient outcomes3. Therefore, there is an urgent necessity to investigate the biological characteristics and molecular mechanisms of PDAC to achieve breakthroughs in early diagnosis and precise treatment strategies.
Long non-coding RNAs (lncRNAs) play vital roles in regulating gene expression at the epigenetic, transcriptional, and post-transcriptional levels by interacting with DNA, RNA, and proteins4,5. As research advances, it becomes increasingly evident that lncRNAs participate widely in various biological processes and disease development6. The expression of lncRNA exhibited tissue and spatiotemporal specificity7, and they are frequently dysregulated in various types of cancer8,9. Due to their expression and functional roles in cancer, lncRNAs are emerging as potential and valuable biomarkers for early diagnosis and prognostic prediction10. Numerous studies have shown aberrant expression of many lncRNAs in PDAC and their significant association with patient survival11,12,13. However, the potential role and clinical application of dysregulated lncRNAs in PDAC remains uncertain. Investigations into the role of lncRNAs as biomarkers for diagnosing or predicting the prognosis of PDAC are in their nascent stages, especially regarding the development of prognostic prediction models based on lncRNAs.
Lactic acid serves as a potential energy source under various conditions, particularly in tumor cells, which can absorb and oxidize lactic acid to fuel their metabolic needs after consuming large amounts of glucose14. The acidic tumor microenvironment, with a pH of 6.0–6.6 due to the abnormal accumulation of lactic acid, plays significant roles in tumor cell migration, invasion, angiogenesis, and treatment resistance15. Additionally, lactic acid acts as a key regulatory molecule that induces and recruits immunosuppressive-related cells and molecules, thereby promoting tumor development16. Lactate-modified lactylation of histone lysine sites serves as epigenetic modification that directly influences transcription process, providing deeper insights into the functions of lactate and its involvement in diverse pathophysiological conditions17. Importantly, accumulating evidence suggests a close association between lactic acid and lncRNAs. Bioinformatics analysis has identified prognostic signatures based on lactate acid-related lncRNA, offering valuable insights into prognostic prediction and the identification of novel molecular targets for treatment across various malignancies, including esophageal squamous cell carcinoma18, colon adenocarcinoma19, and lung adenocarcinoma20. However, the identification and impact of lactic acid-related lncRNAs in PDAC remain largely unknown.
In this research, we systematically screened for lactate-related lncRNAs in the TCGA and StarBase databases. The differentially expressed lactate-related lncRNAs identified in PDAC were designated as LA-DElncRNAs. For the first time, we established a novel predictive model for PDAC using a panel of four LA-DElncRNAs. This model effectively predicted PDAC prognosis and showed significant correlations with immune subtypes and infiltration of immune cells. Furthermore, we selected FAM225B, one of the LA-DElncRNAs, for further research. Knockdown of FAM225B significantly reduced the proliferation and invasion of PDAC cells both in vitro and in vivo.
Materials and methods
Data collection
The RNA-seq profiles and clinical information of 350 samples, comprising 179 PDAC patients and 171 healthy controls, were sourced from two databases: The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx). Lactate metabolism-related genes were identified using the MSigDB and GeneCard databases.
Definition of LA-DElncRNAs
Pearson correlation analysis was conducted to assess the expression correlation between lactate metabolism-related genes and lncRNAs in PDAC. Data from the starBase database were utilized to identify lncRNAs potentially involved in regulating lactate metabolism-related genes. The lncRNAs correlated with expression or regulatory of lactate metabolism-related genes in both TCGA and starBase databases were termed lactate-related lncRNAs. Subsequently, differential expression analysis using the DESeq2 package was employed to compare the expression levels of lactate-related lncRNAs between PDAC and normal pancreatic tissue. Lactate-related lncRNAs exhibiting |Log2 FC| > 1 and p < 0.05 in this analysis were defined as LA-DElncRNAs.
Identification of LA-DElncRNAs related with survival of PDAC
To identify prognosis-associated LA-DElncRNAs, univariate Cox regression analysis was performed. Patients from the TCGA-PAAD and ICGC-PACA-CA datasets were divided into groups based on the median expression levels of the identified LA-DElncRNAs. Kaplan-Meier curves for these prognosis-related LA-DElncRNAs were generated.
Construction of the prognostic model based on LA-DElncRNAs
The least absolute shrinkage and selection operator (LASSO) was implemented to screen for lncRNA with significant regression coefficients. Patients were categorized into high- or low-risk groups based on their respective risk scores calculated derived from the coefficients of specific lncRNA. The Kaplan-Meier method was applied to assess the survival difference between these groups. Additionally, receiver operating characteristic curve (ROC) was performed to evaluate the performance of the model.
Validation of the model based on LA-DElncRNAs
The relationship between the risk score and various clinical factors, including immune subtype21, stage, age, alcohol use, tumor ___location, history of diabetes, history of chronic pancreatitis, gender, and radiotherapy, was evaluated using the chi-squared test or fisher’s exact test. Multivariate analyses were performed to identify independent prognostic predictors.
A nomogram analysis was performed to predict the overall survival (OS) of PDAC patients. The nomogram provided a visual tool for estimating individual survival probabilities based on the identified prognostic factors. Calibration curves were utilized to assess the consistency between the actual OS proportions and the predicted OS probabilities, ensuring the accuracy and reliability of the nomogram-based predictions.
Tumor immune microenvironment analysis
Three computational methods CIBERSORT, ssGSEA, and ESTIMATE were employed to investigate the relationship between the risk score and immune cell infiltration in PDAC. A comprehensive list of immune checkpoint genes (ICGs) was obtained from previous studies21. The expression levels of these ICGs were compared between the high-risk and low-risk groups.
Cell culture and transfection
The human PDAC cell lines (BxPC-3 and PANC-1) were sourced from the American Type Culture Collection. These cell lines were cultured in RPMI 1640 medium supplemented with 10% fetal bovine serum (FBS) and 1% penicillin–streptomycin, and maintained in a 37℃ incubator with 5% CO2.
FAM225B siRNA and siRNA negative control were transfected at a final concentration of 50 nM using Lipofectamine 2000 (Invitrogen, Carlsbad, CA) according to the manufacturer’s instructions. Total RNA was extracted 48 h post-transfection.
RNA isolation and quantitative real-time RT-PCR (qRT-PCR)
Tumor and adjacent nontumor pancreatic tissues of PDAC were collected from Xiangya Hospital (Changsha, China). Fresh samples were snap-frozen at −80℃.
Total RNA was extracted from cell lines and tissues using Trizol reagent (Invitrogen). Reverse transcription was performed using PrimeScript™ RT Master Mix (TaKaRa, Japan). qRT-PCR was conducted using SYBR® Premix Ex Taq™ II (TaKaRa). RNA expression levels were calculated using the 2−ΔΔCt method, normalized to GAPDH expression.
Cell proliferation assay
Cells were seeded into 96-well plates at a density of 2000 cells per well and allowed to proliferate for 1 to 5 days. MTT assay was ed used to assess the cell viability. Microplate reader was used to measure absorbance at 570 nm to determine cell proliferation.
Invasion assay
Transwell migration chambers coated with Matrigel were utilized to assess cell invasion ability. A total of 1 × 10^5 cells, resuspended in serum-free medium, were added to the upper chamber, while the lower chamber was filled with medium containing 30% FBS as a chemoattractant. After 24 h of incubation, cells on the upper side of the membranes were removed. The invasive cells on the bottom side of the membranes were then fixed, stained, and counted.
Xenograft assay
The sequence of FAM225B siRNA was constructed into a lentiviral vector, with an empty lentiviral vector serving as the negative control. A total of 1 × 10^7 transfected cells were subcutaneously injected into one side of 4-week-old male BALB/c nude mice. Tumor volume was measured every 3 days using the formula 0.5 * L (length) * W^2 (width). Three weeks post-injection, the mice were sacrificed by cervical dislocation, and tumor weight was recorded. Additionally, the livers were harvested to analyze for liver metastasis.
Statistical analysis
Quantitative data were analyzed using t-test or Mann–Whitney U test, while categorical data were analyzed using the chi-square test or fisher’s exact test. Pearson correlation analysis was conducted to assess the correlation between lactate metabolism-related genes and lncRNAs. Cox proportional hazards models was used to investigate the prognostic factors. LASSO was implemented to screen for lncRNA with significant regression coefficients. Nomogram was used to visualize the model. Survival rates were estimated using Kaplan-Meier curve and log-rank test. ROC was performed to evaluate the performance of the model. Statistical analyses were performed using SPSS 26.0 and R 4.3.1. Statistical significance was set at p < 0.05.
Results
Screening of LncRNAs associated with lactate metabolism-related genes
Pearson correlation analysis was conducted to investigate the association between lncRNAs and lactate metabolism-related genes in the TCGA database. A total of 4,307 lncRNAs were found to be correlated with lactate metabolism (|R| > 0.5, p < 0.05). A heatmap was generated to visualize the lncRNAs that exhibited strong correlation with lactate metabolism-related genes at a threshold of |R| ≥ 0.8 (Fig. 1A). Additionally, the StarBase database was utilized to identify lncRNAs with potential regulatory relationships with lactate metabolism-related genes. Among the 95 screened lncRNAs, 72 were expressed in PDAC. Consequently, lncRNAs that displayed both expression and regulatory relationships with lactate metabolism-related genes, identified from the TCGA and StarBase databases, were combined and defined as lactate-related lncRNAs in PDAC (Fig. 1B).
Identifying lactate-related lncRNAs in pancreatic cancer. (A) The co-expression analysis between lactate metabolism-related genes and lncRNAs in TCGA database, |R| = 0.8. (B) Venn diagram showing the union set of lncRNAs with expression correlation or potential regulatory relationship with lactate metabolism-related genes. (C) Heatmap displaying the differential expression of lactate-related lncRNAs in pancreatic cancer tissues compared to normal tissues in the TCGA database. (D) Volcano plot illustrating the 1,455 differentially expressed lactate-related lncRNAs (LA-DElncRNAs), with 690 upregulated and 765 downregulated. (E) PCA distinguishing pancreatic cancer tissues from normal pancreatic tissues based on the expression of 1,455 LA-DElncRNAs.
Subsequently, DESeq2 analysis was performed to identify differentially expressed lncRNAs between PDAC tissue and normal tissue in the TCGA database. A total of 1,455 lactate-related lncRNAs met the criteria of |Log2FC| > 1 and adjusted p-value < 0.05 (Fig. 1C; Supplementary Table 1). Among them, 690 lactate-related lncRNAs were downregulated in PDAC tissues, while 765 lactate-related lncRNAs showed significant upregulation (Fig. 1D). These 1,455 differentially expressed lactate-related lncRNAs were designated as LA-DElncRNAs. Principal Component Analysis (PCA) based on the average log2-ratio of the 1,455 LA-DElncRNAs demonstrated a clear distinction between PDAC tissues and normal pancreatic tissues, indicating that LA-DElncRNAs could effectively differentiate between the two groups (Fig. 1E).
Identification of LA-DElncRNAs associated with prognosis of PDAC
The association between the 1,455 LA-DElncRNAs and OS of PDAC in TCGA-PAAD and ICGC-PACA-CA was assessed using univariate Cox regression analysis. The results revealed that 47 LA-DElncRNAs showed a significant correlation with OS of PDAC (p < 0.05). Among these, the 11 LA-DElncRNAs with the most significant differences were selected to create a forest plot (p < 0.015, Fig. 2A). Of these 11 LA-DElncRNAs, five, including RP11-10 K2.6, were found to be upregulated and negatively correlated with OS (Fig. 2B and C), while six, including PART1, were downregulated and positively correlated with OS (Fig. 2D and E). Furthermore, FAM225B exhibited the lowest p-value and the highest hazard ratio. In PDAC, the expression level of FAM225B was significantly increased and negatively correlated with OS (Fig. 2F and G).
LA-DElncRNAs correlated with the prognosis of pancreatic cancer patients. (A) Forest plot of univariate Cox regression analyses showing the 11 optimal prognostic LA-DElncRNAs. Kaplan–Meier survival analysis curves of OS for the high and low expression of RP11-10 K2.6 (B), PART1 (D), and FAM225B (F). The expression of RP11-10 K2.6 (C), PART1 (E), and FAM225B (G) in pancreatic cancer tissues and normal pancreatic tissue in the TCGA database.
Construction of a LA-DElncRNAs -related risk scoring model
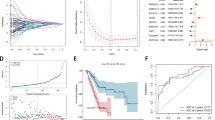
Based on the results of univariate Cox regression analysis in TCGA-PAAD (Supplementary Table 2), 23 LA-DElncRNAs with a p-value < 0.03 were selected to construct a LASSO regression model using the parameters: glmnet (cox_dat, clinic$event, alpha = 1). In the LASSO regression, the optimal λ value was determined to be 4 (Fig. 3A). Among the 23 LA-DElncRNAs, four had non-zero LASSO coefficients and were selected as prognostic parameters to establish a risk score model (Fig. 3B). The corresponding LASSO coefficients for RP11-16 K12.1, RP11-775D22.2, RP11-734 K21.3, and CTD-2619 J13.14 are shown in Fig. 3C.
Construction of the prognostic Model based on LA-DElncRNAs. (A) LASSO regression was applied to screen the most robust lncRNAs used 10-fold cross-validation via minimum criteria. (B) LASSO coefficient profiles of the 23 features. A coefficient profile plot was generated against the log (λ) sequence. The vertical line indicated the value selected using 10-fold cross-validation, resulting in four features with non-zero coefficients. (C) The four optimal prognostic hypoxia-related lncRNAs selected by LASSO regression.
These four LA-DElncRNAs were used to construct a prognostic model. The risk score was calculated using the formula: (0.615 * RP11-16 K12.1 expression − 0.498 * RP11-775D22.2 expression − 0.517 * RP11-734 K21.3 expression − 0.551 * CTD-2619 J13.14 expression). To validate the prognostic value of the model, the risk score was calculated for each patient. The expression profiles of the four LA-DElncRNAs in patients with different risk scores were displayed in a heatmap (Fig. 4A). Subsequently, the patients were divided into high- or low-risk groups based on the median risk score. The survival status comparison between the two groups revealed a higher proportion of deceased patients in the high-risk group (Fig. 4B). Kaplan-Meier survival analysis demonstrated a highly significant difference in survival rates between the two groups (p < 0.001, Fig. 4C). Additionally, the area under the curve (AUC) of the ROC curve was calculated, with AUCs of 0.685, 0.607, and 0.595 for predicting one-, three-, and five-year OS, respectively, demonstrating the efficient performance of the risk score (Fig. 4D).
Assessing the performance of the prognostic Model based on LA-DElncRNAs. (A) Distribution of risk scores and the expression signature of lncRNAs in the high- and low-risk groups. (B) Distribution of risk scores and survival status of patients in the high- and low-risk groups. (C) Kaplan-Meier survival analysis of pancreatic cancer patients stratified by the risk score. (D) Prognostic performance of the model confirmed by ROC curves for one-year, three-year, and five-year survival predictions.
Relation between risk score and clinicopathologic characteristics
To validate the clinical practicality of the risk score, we analyzed the correlation between the risk score and various clinicopathological characteristics, including immune subtype, stage, age, alcohol use, tumor ___location, diabetes, chronic pancreatitis, sex, and radiotherapy. The analysis revealed significant differences in risk scores between immune subtypes C1-2 and C3-6 (Fig. 5A). However, no significant differences in risk scores were observed among other clinicopathological parameters (Fig. 5B–I).
Relationships between the risk score and clinical factors. The risk score in patients with different clinicopathologic parameters: (A) immune subtype (B) stage (C) age (D) alcohol using (E) ___location of the tumor (F) history of diabetes (G) history of chronic pancreatitis (H) gender (I) radiotherapy.
The risk score is an independent prognostic factor for PDAC
Multivariate Cox regression analysis was performed to determine whether the risk score served as an independent prognostic factor. After adjusting for other confounding factors, the analysis revealed a significant correlation between the risk score and prognosis (Fig. 6A).
The risk score was an independent prognostic factor for pancreatic cancer. (A) Multivariate analysis of the risk score and clinical features for correlation with OS. (B) Nomogram integrating clinical features and risk score to predict the probability of OS. (C) ROC curves and AUC of the risk score compared with clinical features including age, tumor grade, immune subtype, and tumor ___location. Calibration plots evaluating the consistency between actual and nomogram-predicted OS at: (D) one year (E) two years (F) three years.
Moreover, a nomogram was constructed based on the risk score, immune subtype, tumor ___location, history of chronic pancreatitis, age, and stage (Fig. 6B). The AUC of the risk score was 0.6738, indicating that the risk score based on LA-DElncRNAs exhibited a strong predictive capacity for survival time (Fig. 6C). Additionally, the calibration curves demonstrated excellent predictive capability, showing stable and accurate performance in predicting survival (Fig. 6D–F).
Comparison of tumor immune microenvironment between high- and low-risk group
The proportion of immune cells in the microenvironment of each sample was determined using three different algorithms: CIBERSORT, ssGSEA, and ESTIMATE. However, no significant differences were observed in the proportion of immune cell infiltration between the low- and high-risk groups (Fig. 7A-C). Given the promising potential therapies, the expression of immune checkpoints in the two groups was also examined. Interestingly, there were significant differences in the expression of immune checkpoints CD40 and HLA-DQB1 (Fig. 7D).
Knockdown of FAM225B inhibits the proliferation and invasion of PDAC cells
In univariate Cox regression analysis, the HR value of the non-coding RNA FAM225B was the highest, suggesting its significant regulatory role in PDAC. Therefore, we further investigated the biological functions of FAM225B in vitro and in vivo.
Firstly, we assessed the expression of FAM225B in 50 PDAC tissues and paired adjacent non-cancerous tissues. qPCR showed that FAM225B was significantly upregulated in PDAC (Fig. 8A).
Knockdown of FAM225B inhibits proliferation and invasion of PANC-1 and BxPC-3. (A) Expression levels of FAM225B in pancreatic cancer tissues (PC) compared to matched adjacent noncancerous pancreatic tissues (NP), n = 50, assessed by qRT-PCR. (B) Expression levels of FAM225B in PANC-1 and BxPC-3 cells after transfection with three different FAM225B siRNA (siFAM225B-1,2,3) or siRNA negative control (siNC), assessed by qRT-PCR. (C) Proliferation of PANC-1 and BxPC-3 cells transfected with siFAM225B-1, siFAM225B-2 or siNC measured by MTT assay. (D) Representative images of invasion assays showing the invasion ability of PANC-1 and BxPC-3 cells transfected with siFAM225B-1, siFAM225B-2 or siNC using Transwell assays.
To explore the role of FAM225B in PDAC cells, its expression was inhibited using three distinct siRNAs. qPCR analysis confirmed that siFAM225B-1 and siFAM225B-2 significantly reduced FAM225B expression, and these two siRNAs were selected for further experiments (Fig. 8B). After knockdown of FAM225B, growth retardation was observed in PANC-1 and BxPC-3 cells starting from three days post-transfection (Fig. 8C). Additionally, Transwell assays demonstrated that downregulation of FAM225B reduced the invasion ability of PANC-1 and BxPC-3 cells (Fig. 8D).
Knockdown of FAM225B inhibits growth and invasion of xenograft tumor
To investigate whether FAM225B regulates growth and invasion in vivo, a PDAC xenograft model was established using cells stably expressing Lv-siNC or Lv-siFAM225B (Fig. 9A). PANC-1 cells transfected with Lv-siFAM225B showed delayed tumor growth and reduced tumor volume (Fig. 9B and C). Furthermore, the FAM225B knockdown group exhibited fewer liver metastases compared to the control group (Fig. 9D).
Knockdown of FAM225B inhibits xenograft tumor growth and metastasis. (A) Representative photographs of nude mice bearing subcutaneous xenograft tumors derived from PANC-1 cells transfected with Lentivirus containing FAM225B siRNA (Lv-siFAM225B) or negative control (Lv-NC). (B) Tumor weight recorded after sacrifice of the mice. (C) Tumor volume measured every 3 days during the experiment using the formula 0.5 * L (length) * W^2 (width). (D) Representative photographs of liver metastases in nude mice with subcutaneous xenografts. The histogram shows the number of mice with liver metastases in each group.
Discussion
With the continual advancements in therapeutic strategies for PDAC, there is an urgent need to establish effective prognostic evaluation methods to guide personalized treatment for PDAC patients1. However, due to the complex molecular mechanism and high malignancy of PDAC, the predictive power of current prognostic models for PDAC prognosis remains limited22. In this study, we identified 1,455 LA-DElncRNAs in PDAC from the TCGA and StarBase databases. Further univariate Cox regression analysis revealed that 23 of these LA-DElncRNAs are associated with the prognosis of PDAC. Subsequently, we constructed a prognostic model using four key LA-DElncRNAs. Multivariate Cox regression analysis confirmed that the risk score of the model is an independent prognostic factor for PDAC. The nomogram model based on the risk score demonstrated excellent performance in predicting the prognosis of PDAC patients. In summary, our prediction models effectively evaluate the prognosis and survival of patients with PDAC, providing a robust theoretical foundation for clinical decision-making and individualized treatment approaches.
Metabolic reprogramming is a well-established hallmark of cancer, reshaping gene expression profiles, metabolic mechanisms, and energy requirements, thereby endowing cancer cells with new functionalities and heightened adaptability to diverse conditions23,24. Aerobic glycolysis, commonly known as the Warburg effect, stands central to this metabolic reprogramming and serves as a crucial driver of cancer progression25. This metabolic adaptation results in excessive lactate production, pivotal for sustaining cancer cell proliferation and growth26. The flux of lactate mediated by tumors is intricately linked with extensive epigenomic reprogramming27.PDAC, characterized by intricate vascular structures and dense desmoplastic stroma, exhibits pronounced enhancements in glycolysis and accumulation of lactate28. Consequently, lactate metabolism offers a novel perspective for comprehending the pathogenesis of PDAC29. Notably, lactate-regulated activation of myeloid-derived suppressor cells (MDSCs) fosters an immunosuppressive microenvironment, thereby promoting PDAC progression and recurrence30. Despite these insights, the prognostic significance of lactate in PDAC remains ambiguous. In this study, we identified lactate-related long non-coding RNAs (LA-DElncRNAs) that exhibit dysregulation in PDAC samples and are significantly correlated with prognosis. These LA-DElncRNAs hold substantial promise as biomarkers or therapeutic targets for PDAC.
Substantial researches have underscored the critical role of lncRNAs in the mechanism of occurrence and development of PDAC31,32. Dysregulated lncRNAs plays a key role in proliferation, metastasis, invasion, and angiogenesis during the development of PDAC33. The lncRNA FAM225B has been implicated in various cancers: its expression correlates positively with glioma grade and serves as a critical prognostic factor in recurrent glioblastoma34. Also, elevated FAM225B levels are associated with advanced TNM stage and poor OS in nasopharyngeal carcinoma35. Similarly, in renal clear cell carcinoma, higher FAM225B expression predicts a worse prognosis, and its knockdown inhibits renal cancer cell proliferation, migration, and invasion36. In our study, we observed upregulation of FAM225B in PDAC, which correlates with poor prognosis. Furthermore, the HR of FAM225B is the highest, highlighting the vital role of FAM225B in PDAC. Despite these associations, the biological function of FAM225B in PDAC has remained unclear. Therefore, we conducted further investigations to elucidate its role both in vitro and in vivo. Our findings demonstrate that knockdown of FAM225B suppresses proliferation and invasion of PDAC cells, confirming its regulatory role in this malignancy.
The dysregulation of multiple lncRNAs is closely associated with the survival and clinicopathological features of PDAC patients, suggesting their potential as biomarkers for diagnosis and prognosis37. Increasing evidence demonstrates that prognostic models constructed using lncRNAs exhibit impressive accuracy in predicting the overall survival of PDAC patients. For example, signatures based on ferroptosis-associated lncRNAs have been shown to evaluate prognosis, molecular characteristics, and drug sensitivity38. Similarly, prognostic risk model based on m5C-related lncRNAs39, m6A-related lncRNA40, immune-related lncRNA41, and pyroptosis-related lncRNA42, have demonstrated effectiveness in estimating prognostic outcomes in PDAC. Importantly, an increasing number of studies have highlighted the potential role of lactate-related lncRNAs in the occurrence and development of tumors43,44. However, there have been no published investigations on the function of lactate-related lncRNAs in predicting the prognosis of PDAC patients. In this study, we constructed a prognostic model based on four lactate-related lncRNAs. Multivariate Cox regression and Nomogram analysis confirmed that this risk model exhibits a powerful predictive capacity for the survival outcomes of PDAC patients. Furthermore, patients with different risk scores showed distinct expression patterns of immune checkpoints. To the best of our knowledge, this is the first study to construct a prognostic model based on lactate-related lncRNAs.
With the continuous advancement of treatment strategies for PDAC, including neoadjuvant therapy, targeted therapy, and immunotherapy45, there is an urgent need to introduce new indicators and novel models to evaluate the prognosis of PDAC. To improve precision and accuracy, new prognostic model should utilize quantitative indicators to predict the survival outcome of PDAC patients, moving away from previous empirical judgments. Various factors such as tumor differentiation degree, tumor size and stage, lymph node metastasis, serum albumin level, carbohydrate antigen CA19-9, and negative incisal margin have been used to construct preoperative prediction evaluation models to guide treatment and postoperative evaluation models to predict survival time46. Additionally, new factors including serum inflammatory markers, gene expression data, patient nutritional status, and imaging data have been incorporated into these models47,48. However, apart from TNM staging, the existing prognostic models have not been widely utilized and validated. It is anticipated that the development of new technologies will facilitate the progress of prognostic models in the future, with the inclusion of more indicators. In this study, we creatively developed a prognostic model using lactate-related lncRNAs and confirmed its effectiveness and accuracy. PDAC has an extremely poor prognosis, and reliable prognostic model remain limited. Even with a not excellent AUC, our model may still have prognostic potential. Furthermore, our study is the first to establish a predictive model based on lactate metabolism-related lncRNA, providing new perspectives to future research of prognostic model in PDAC. It is believed that in the near future, survival prediction models incorporating lncRNAs will become more accurate and individualized, providing more comprehensive information for clinical decision-making.
In conclusion, this study identified a set of lactate-related lncRNAs associated with the prognosis of PDAC. These lncRNAs exhibit significant potential as biomarkers or therapeutic targets. Using these lactate-related lncRNAs, we developed a prognostic prediction model for PDAC. Our findings suggest that lactate-related lncRNAs represent promising biomarkers for cancer prognosis and provide an attractive perspective for future therapeutic strategies.
Data availability
The datasets used and analysed during the current study were available from the corresponding author on reasonable request.
References
Klein, A. P. Pancreatic cancer epidemiology: Understanding the role of lifestyle and inherited risk factors. Nat. Rev. Gastroenterol. Hepatol. 18 (7), 493–502 (2021).
Park, W., Chawla, A. & O’Reilly, E. M. Pancreat. Cancer: Rev. JAMA 326(9), 851–862. (2021).
Mizrahi, J. D. et al. Pancreatic cancer. Lancet (London England). 395 (10242), 2008–2020 (2020).
Goodall, G. J. & Wickramasinghe, V. O. RNA in cancer. Nat. Rev. Cancer. 21 (1), 22–36 (2021).
Herman, A. B., Tsitsipatis, D. & Gorospe, M. Integrated LncRNA function upon genomic and epigenomic regulation. Mol. Cell. 82 (12), 2252–2266 (2022).
Ali, T. & Grote, P. Beyond the RNA-dependent function of LncRNA genes. eLife. 9, e60583 (2020).
McCorkindale, A. L. et al. A gene expression atlas of embryonic neurogenesis in Drosophila reveals complex Spatiotemporal regulation of LncRNAs. Dev. (Cambridge England) 146(6), dev175265 (2019).
Zhang, H. et al. CircRNA: a novel type of biomarker for cancer. Breast Cancer (Tokyo Japan). 25 (1), 1–7 (2018).
Chan, J. J. & Tay, Y. Noncoding RNA:RNA regulatory networks in Cancer. Int. J. Mol. Sci. 19(5), 1310 (2018).
Chandra Gupta, S. & Nandan Tripathi, Y. Potential of long non-coding RNAs in cancer patients: from biomarkers to therapeutic targets. Int. J. Cancer. 140 (9), 1955–1967 (2017).
Zhou, C. et al. LncRNA PVT1 promotes gemcitabine resistance of pancreatic cancer via activating Wnt/β-catenin and autophagy pathway through modulating the miR-619-5p/Pygo2 and miR-619-5p/ATG14 axes. Mol. Cancer. 19 (1), 118 (2020).
Zhai, S. et al. Epigenetic Silencing of LncRNA LINC00261 promotes c-myc-mediated aerobic Glycolysis by regulating miR-222-3p/HIPK2/ERK axis and sequestering IGF2BP1. Oncogene 40 (2), 277–291 (2021).
Arnes, L. et al. Comprehensive characterisation of compartment-specific long non-coding RNAs associated with pancreatic ductal adenocarcinoma. Gut 68 (3), 499–511 (2019).
Li, X. et al. Lactate metabolism in human health and disease. Signal. Transduct. Target. Therapy. 7 (1), 305 (2022).
Ivashkiv, L. B. The hypoxia-lactate axis tempers inflammation. Nat. Rev. Immunol. 20 (2), 85–86 (2020).
Certo, M. et al. Lactate modulation of immune responses in inflammatory versus tumour microenvironments. Nat. Rev. Immunol. 21 (3), 151–161 (2021).
Zhang, D. et al. Metabolic regulation of gene expression by histone lactylation. Nature 574 (7779), 575–580 (2019).
Zhao, F. et al. Identification of A risk signature based on lactic acid Metabolism-Related LncRNAs in patients with esophageal squamous cell carcinoma. Front. Cell. Dev. Biology. 10, 845293 (2022).
Xiao, J. et al. Lactate Metabolism-Associated LncRNA pairs: A prognostic signature to reveal the immunological landscape and mediate therapeutic response in patients with Colon adenocarcinoma. Front. Immunol. 13, 881359 (2022).
Mai, S. et al. Development and validation of lactate Metabolism-Related LncRNA signature as a prognostic model for lung adenocarcinoma. Front. Endocrinol. 13, 829175 (2022).
Thorsson, V. et al. The immune landscape of Cancer. Immunity 48(4), 812–830 (2018).
Cai, J. et al. Advances in the epidemiology of pancreatic cancer: trends, risk factors, screening, and prognosis. Cancer Lett. 520, 1–11 (2021).
Sun, L., Zhang, H. & Gao, P. Metabolic reprogramming and epigenetic modifications on the path to cancer. Protein Cell. 13 (12), 877–919 (2022).
Sun, L. et al. Metabolic reprogramming for cancer cells and their microenvironment: beyond the Warburg effect. Biochimica et biophysica acta. Reviews Cancer. 1870 (1), 51–66 (2018).
Vaupel, P. & Schmidberger, H. The Warburg effect: essential part of metabolic reprogramming and central contributor to cancer progression. Int. J. Radiat. Biol. 95 (7), 912–919 (2019).
Brown, T. P. & Ganapathy, V. Lactate/GPR81 signaling and proton motive force in cancer: role in angiogenesis, immune escape, nutrition, and Warburg phenomenon. Pharmacol. Ther. 206, 107451 (2020).
Bhagat, T. D. et al. Lactate-mediated epigenetic reprogramming regulates formation of human pancreatic cancer-associated fibroblasts. eLife. 8, e50663 (2019).
Yang, J. et al. The enhancement of Glycolysis regulates pancreatic cancer metastasis. Cell. Mol. Life Sci. 77 (2), 305–321 (2020).
Adeva-Andany, M. et al. Comprehensive review on lactate metabolism in human health. Mitochondrion 17, 76–100 (2014).
Yang, X. et al. Lactate-Modulated immunosuppression of Myeloid-Derived suppressor cells contributes to the radioresistance of pancreatic Cancer. Cancer Immunol. Res. 8 (11), 1440–1451 (2020).
Liu, Y. et al. LncRNA-PACERR induces pro-tumour macrophages via interacting with miR-671-3p and m6A-reader IGF2BP2 in pancreatic ductal adenocarcinoma. J. Hematol. Oncol. 15 (1), 52 (2022).
Ghafouri-Fard, S. et al. LncRNAs: novel biomarkers for pancreatic Cancer. Biomolecules 11(11), 1665 (2021).
Bin, W. et al. Long non-coding RNAs and pancreatic cancer: A multifaceted view. Biomed. Pharmacother. 167, 115601 (2023).
Li, J. et al. FAM225B Is a Prognostic lncRNA for Patients with Recurrent Glioblastoma. Dis Markers. 2020: 8888085. (2020).
Dai, W. et al. Long noncoding RNA FAM225B facilitates proliferation and metastasis of nasopharyngeal carcinoma cells by regulating miR-613/CCND2 axis. Bosn J. Basic. Med. Sci. 22 (1), 77–86 (2022).
Li, X. et al. Disulfideptosis-associated LncRNAs reveal features of prognostic, immune escape, tumor mutation, and tumor malignant progression in renal clear cell carcinoma. Aging (Albany NY). 16 (4), 3280–3301 (2024).
Seyed Hosseini, E. et al. The impact of LncRNA dysregulation on clinicopathology and survival of pancreatic cancer: a systematic review and meta-analysis (PRISMA compliant). Cancer Cell Int. 21 (1), 447 (2021).
Tang, R. et al. Ferroptosis-related LncRNA pairs to predict the clinical outcome and molecular characteristics of pancreatic ductal adenocarcinoma. Brief. Bioinform. 23(1), bbab388 (2022).
Yuan, H. et al. Prognostic risk model and tumor immune environment modulation of m5C-Related LncRNAs in pancreatic ductal adenocarcinoma. Front. Immunol. 12, 800268 (2021).
Cao, P-W. et al. Prognostic value of drug targets predicted using deep bioinformatic analysis of m6A-Associated lncRNA-Based pancreatic Cancer model characteristics and its tumour microenvironment. Front. Genet. 13, 853471 (2022).
Zhang, Q. et al. Immune subtypes based on Immune-Related lncrna: differential prognostic mechanism of pancreatic Cancer. Front. Cell. Dev. Biology. 9, 698296 (2021).
Lu, S-Y. et al. Pyroptosis-related LncRNA pairs to estimate the molecular features and prognostic outcomes of pancreatic ductal adenocarcinoma. Translational Oncol. 25, 101524 (2022).
Chen, F. et al. Extracellular vesicle-packaged HIF-1α-stabilizing LncRNA from tumour-associated macrophages regulates aerobic Glycolysis of breast cancer cells. Nat. Cell Biol. 21 (4), 498–510 (2019).
Li, J. et al. A lactate-related LncRNA model for predicting prognosis, immune landscape and therapeutic response in breast cancer. Front. Genet. 13, 956246 (2022).
Neoptolemos, J. P. et al. Therapeutic developments in pancreatic cancer: current and future perspectives. Nat. Rev. Gastroenterol. Hepatol. 15 (6), 333–348 (2018).
Ioannou, L. J. et al. Prognostic models to predict survival in patients with pancreatic cancer: a systematic review. HPB: Official J. Int. Hepato Pancreato Biliary Association. 24 (8), 1201–1216 (2022).
Lanki, M. et al. Pancreatic cancer survival prediction via inflammatory serum markers. Cancer Immunol. Immunotherapy: CII. 71 (9), 2287–2292 (2022).
Xu, D. et al. Development and clinical validation of a novel 9-gene prognostic model based on multi-omics in pancreatic adenocarcinoma. Pharmacol. Res. 164, 105370 (2021).
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (81802450 to SZ), the Natural Science Foundation of Hunan Province (2021 JJ31135 to SZ), and Changsha Municipal Natural Science Foundation (kq2208394 to SJ).
Author information
Authors and Affiliations
Contributions
Shuai Zhu conceived, designed and refined the study protocol; Jing Sun and Tao Zhang finished the experiments, collected and analyzed the data and drafted the manuscript; Shuai Zhu reviewed and revised the manuscript. Jing Sun and Tao Zhang contributed equally to this work as co-first authors. All authors had access to the study data and reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Ethics approval
All experimental protocols were approved by the Institutional Review Board at Xiangya Hospital of Central South University and all experiments were performed in accordance with relevant guidelines and regulations.
ARRIVE guidelines statement
The authors have read the ARRIVE guidelines, and the manuscript was prepared and revised according to the ARRIVE guidelines.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sun, J., Zhang, T. & Zhu, S. Lactate-related lncRNAs assessment model predicts the prognosis of pancreatic ductal adenocarcinoma. Sci Rep 15, 21226 (2025). https://doi.org/10.1038/s41598-025-05486-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-05486-z