Abstract
This study investigated the effectiveness and safety of ultrasound-guided non-incisional thread trigger finger release on cadavers using a newly developed domestic thread (Smartwire-01). Ultrasound-guided non-incisional thread trigger finger release was performed on 12 fresh cadaveric hands, including 12 thumbs and 48 long fingers. Two experts, experienced in an ultrasound-guided thread transecting technique, performed the procedures independently. The distal-to-proximal and proximal-to-distal approaches were performed in 6 hands each to determine which is safer and more effective. After the procedure, anatomical analyses were conducted by a blinded anatomist. The presence of a dissected A1 pulley and any damage to adjacent structures were assessed. Among the 60 cadaveric digits, 52 (86.7%) showed complete transection of the A1 pulley. The success rate for the thumb (66.7%) was relatively lower than that of the other fingers (91.7%). The distal-to-proximal approach showed a higher success rate (96.7%) compared to the proximal-to-distal approach (76.7%), with a near-significant difference (p = 0.052). Anatomical analysis revealed clear and sharp incisional margins of the transected A1 pulley, with only 1 minor flexor tendon injury observed, which occurred with the proximal-to-distal approach. Ultrasound-guided non-incisional thread trigger finger release using Smartwire-01 is a safe and effective procedure when performed with the distal-to-proximal approach, particularly in long fingers.
Similar content being viewed by others
Introduction
The first annular (A1) pulley physiologically maintains the flexor tendon’s alignment close to the phalanges and ensures smooth tendon excursion. In trigger finger, pathological thickening of the flexor tendon or the A1 pulley leads to a size mismatch between the two structures, resulting in painful triggering, crepitus, or the presence of a palpable tender nodule along the tendon1,2,3. The first-line treatment of trigger finger is conservative care, including activity modification (e.g., minimizing repetitive gripping or pinching), finger splinting, and nonsteroidal anti-inflammatory medications4,5. Additionally, corticosteroid injection in the palm at the first annular pulley level of the affected digit is safe and effective for relieving signs and symptoms but is also associated with a high recurrence rate6,7. If these measures are ineffective, surgical release of the annular pulley is recommended8.
Open release of the A1 pulley is considered the standard surgical technique to treat trigger finger4. The success rates of open A1 pulley release are between 90% and 100%, with a complication rate between 5% and 12%9,10. Several minimally invasive percutaneous approaches have emerged as an alternative to open surgery with studies suggesting these approaches may result in improved outcomes and have an efficacy similar to that of open release11,12,13,14,15,16. These techniques may save time and are associated with a smaller incision, potentially lowering the risk of infection. Some studies have reported percutaneous release to produce less postoperative pain and faster return to activity compared to the classical surgical treatment14,15. Although the non-image-guided percutaneous approach is reported to be safe11,12,13,15,16it solely relies on anatomic landmarks to avoid injuring adjacent anatomical structures. Using high-resolution ultrasound guidance for percutaneous release allows accurate identification of the thickened annular pulley while simultaneously identifying the digital neurovascular structures and the flexor tendons. A variety of cutting devices has been used for ultrasound-guided percutaneous release of trigger finger, including different size needles17,18blades19specially designed hooked knives20,21and thread22.
The thread transecting technique, first proposed by Guo et al.23divides only structures inside the loop of thread and does not require a skin incision, leaving only two needle punctures. It also has the advantages of not using a sharp dividing instrument, not requiring repetitive cutting motions, and reducing the risk of iatrogenic injury under continuous sonographic visualization24. Guo et al. first applied this technique to carpal tunnel release and demonstrated in a cadaver study23 that it is a feasible method capable of completely transecting the transverse carpal ligament without injuring vital neural or vascular structures. The clinical effectiveness and safety of non-incisional carpal tunnel release were reported by our previous studies with newly developed domestic thread (Smartwire-01) and by other groups25,26,27,28,29,30. In contrast, few cadaveric studies31,32 have evaluated the efficacy and safety of non-incisional trigger finger release, and to date, only 1 clinical trial has been performed22.
The present study is to determine the efficacy and safety of ultrasound-guided non-incisional thread trigger finger release on cadavers using a newly developed domestic thread (Smartwire-01). The procedure can be performed using either the distal-to-proximal approach or the proximal-to-distal approach. The secondary aim of the study is to determine the safety and efficacy of each approach.
Results
For all 60 digits (12 thumbs and 48 long fingers), the complete transection rate was 86.7% (52 of 60), while 6 were partially transected, and 2 experienced failure, defined as an intact A1 pulley (Table 1). Among the thumbs, 8 of 12 underwent complete transection, whereas 3 cases involved incomplete transection, and 1 demonstrated failure. For the long fingers, 44 of 48 achieved complete release, with 3 cases of incomplete transection and 1 case of failure. The success rate for the thumb (66.7%) was lower than that of the other fingers (91.7%). There was no difference in the incomplete/failure rate or procedure time between the two experts. Excluding instrument preparation, the procedure time ranged from 5 to 10 min under cadaveric conditions and decreased further with operator experience.
In the distal-to-proximal approach, only 1 thumb showed partial release. The overall complete A1 pulley transection rate was 96.7%, with 83.3% for the thumb and 100% for the long fingers. With the proximal-to-distal approach, the overall success rate was 76.7% (23 of 30), with 50.0% for the thumb and 83.3% for the long fingers. Partial transection was found in 5 cases (2 thumbs and 3 long fingers), and failure occurred in 2 cases (1 thumb and 1 long finger). The distal-to-proximal group showed a higher complete transection rate (96.7%) than the proximal-to-distal group (76.7%), with a near-significant difference (p = 0.052, Fisher’s exact test), as determined using SPSS software (version 29.0; IBM Corp., Armonk, NY, USA).
A gross anatomical evaluation of the transection transected A1 pulley was performed by a blinded anatomist. Figure 3 presents the gross findings of the successfully dissected A1 pulley on the cadaveric hands. The incisional margins of all transected A1 pulleys were sharp and clear. No injuries to the digital nerves were observed in any of the 12 thumbs or 48 long fingers with either approach. However, 1 minor partial injury to the flexor tendon was noted in the left fourth finger with the proximal-to-distal approach (Table 1).
Discussion
Percutaneous methods of A1 pulley release under sonographic guidance have been introduced for the management of trigger finger17,18,19,20,21,22. The procedural technique, including the direction of approach, selection of cutting instruments, and other related factors, varies considerably depending on the operator and facility. Although it is generally regarded as a safe and effective procedure, no randomized studies have yet established the most optimal approach or device. Among various cutting instruments, the use of a thread offers notable advantages. The transection occurs precisely along the targeted anatomical structure and is mechanically confined within the thread loop, with negligible influence on adjacent nontargeted tissue22. Smartwire-01, used as a cutting device in our study, was developed for the percutaneous dissection thread technique with higher cutting force, better visibility on ultrasound, and easier handling due to an additional coating of thin titanium nitride28,33. Particularly in the thumb, A1 pulley release has been reported to be technically more challenging than in the long fingers, with one case of incomplete release in the cadaveric study34 and one case of failed release in the clinical study18. This has been explained by the unique anatomical characteristics of the thumb, which tends to move more easily during the procedure and cannot be positioned fully flat on its dorsal side. Caution has also been advised regarding the risk of radial digital nerve injury, due to the reduced safety margin in the thumb compared to the long fingers35. The clinical investigation reported transient radial digital nerve numbness in three thumbs immediately following the procedure, all of which resolved spontaneously within two weeks20.
To our knowledge, there are only 3 studies on ultrasound-guided non-incisional thread trigger finger release, comprising 2 cadaver studies31,32 and 1 preliminary clinical report22. Guo et al. tested the efficacy and safety of this procedure on 14 fingers and 4 thumbs of 4 cadaveric hands32. They reported nearly perfect results, with all digits demonstrating complete A1 pulley release without injury to nearby structures. In the study of Jengojan et al.31thread trigger finger release was performed on 20 cadaveric fingers, excluding the thumb. Complete release was achieved in 85% of cases, with slight flexor tendon injuries observed in 5 cases, and no neurovascular damage reported. Both cadaveric studies demonstrated that ultrasound-guided thread release for trigger finger is effective and safe. Our study achieved comparable results. Guo et al.22 evaluated the clinical feasibility and effectiveness of 34 digits (11 thumbs and 23 long fingers) in 24 patients. They reported resolution of triggering and locking, and complete flexion and extension immediately following the release with no complications.
Regarding the direction of the procedure, the cadaveric study of Guo et al.32 utilized both approaches for the fingers and found no differences. For the thumbs, only the proximal-to-distal approach was used, as the other approach suffered from difficulty in removing the needle. These findings differ from ours, which showed that the distal-to-proximal approach had a higher success rate for the long fingers (100% vs. 80.3%) and for the thumbs (83.3% vs. 50.0%). Also, our study was performed by 2 experts, with similar outcomes. The difference in these results may be associated with various factors, such as the condition of cadaveric hands, variations in procedural settings, and operator preferences. Guo et al. used the proximal-to-distal approach in a preliminary clinical study22. In contrast, Jengojan et al.31 employed the distal-to-proximal approach in their cadaveric study. Many studies on percutaneous release of trigger finger using various devices have also utilized the distal-to-proximal approach12,17,19,20,21,36. Our results comparing the 2 approaches showed that the distal-to-proximal approach had a higher complete transection rate (96.7% vs. 76.7%, p = 0.052), potentially due to easier needle manipulation and improved procedural accuracy. Although the difference did not reach conventional statistical significance, these findings support the preferential consideration of the distal-to-proximal approach. This approach may be particularly advantageous for long fingers, in which a 100% success rate was achieved.
Incomplete transection occurred in some cases of each approach. Although real-time ultrasound guidance played an important role in ensuring a successful and safe procedure, it cannot confirm complete release of the A1 pulley. It is challenging to accurately delineate the proximal and distal boundaries of the pulley based solely on echogenicity in the ultrasound image20,21,35. Nevertheless, the determination of the limits of division on the A1 pulley is critical for successful release. Many researchers have used the topographic bone landmarks of the metacarpal head-neck junction and the phalangeal base-shaft junction as references for the proximal and distal boundaries of the pulley, respectively37,38. However, the specific extent of release based on these landmarks has varied among studies. Rojo-Manaute et al.21 defined the proximal cutting margin as 5 mm proximal to the metacarpal head-neck junction and the distal margin as 3 mm distal to the base-shaft junction of the proximal phalanx, whereas Jou and Chern et al.20 defined both margins at 5 mm from the respective landmarks. In a cadaveric study, Smith et al.35 set the release extent from 1 to 2 mm proximal to the metacarpal head-neck junction to 1–2 mm distal to the base-shaft junction of the proximal phalanx. Also, anatomical studies demonstrated that the length of the A1 pulley varies among digits, correlates with finger length, and differs across ethnic groups38,39,40,41. This indicates that the security margin should not be a constant but adjusted for each patient.
Even partial transection could lead to sufficient mechanical decompression of the flexor tendon and immediate symptom relief in patients. This was demonstrated by Lapegue et al.18whose full transection of the A1 pulley was not successful in a cadaver study, while the same technique led to complete symptom relief in 96.8% of patients within 6 months. Similarly, Rojo-Manaute et al.21 noted limited visualization in the cadaveric setting, particularly in the thumb, and recommended conversion to open surgery when sonographic guidance was inadequate. However, in their clinical study, ultrasound visualization was excellent, and no conversions were required. These observations suggest that technical limitations encountered in cadaveric models may not pose significant challenges in clinical practice. These findings also highlight a limitation of the present study, which was conducted using cadaveric specimens. Therefore, a follow-up clinical study is warranted to confirm the efficacy and safety of ultrasound-guided non-incisional thread trigger finger release using Smartwire-01. As the thread transection technique is highly dependent on the operator’s proficiency in both ultrasound guidance and procedural skill, the level of expertise plays a critical role in ensuring safety and accuracy. In the present study, both operators had been performing ultrasound-guided thread procedures since 2020 and had clinical experience with over 100 cases of carpal tunnel release using this technique29.
Conclusion
We demonstrated in this cadaveric study that ultrasound-guided non-incisional thread trigger finger release with Smartwire-01 was safe and effective for fingers other than the thumb, especially with the distal-to-proximal approach. Based on these promising findings, future clinical studies are recommended to assess the feasibility and safety of the thread transecting technique for trigger finger treatment.
Materials and methods
Materials
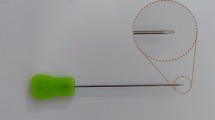
Cadaveric hands with no evidence of previous surgery or trauma history were included in the study. Twelve fresh cadaveric hands with 12 thumbs and 48 long fingers were used for this study. The mean age of the cadavers was 80.9 ± 7.2 years (one male and five females). The newly developed thread Smartwire-01 (Smart Wire Co., Ltd., Goyang-si, South Korea) was used as the cutting thread.
Non-incisional trigger finger release
Non-incisional trigger finger release is a percutaneous technique for A1 pulley transection using a transecting thread without skin incision. All procedures were performed using a Samsung RS85 Prestige US system (Samsung Medison, Seoul, South Korea) equipped with a linear US probe (L3–12 A). Prior to the procedure, ultrasound was used to assess the A1 pulley and common flexor tendon. The real-time ultrasound system was used to monitor the thread loop during the procedure. Non-incisional trigger finger release with Smartwire and a 20G Tuohy needle was performed on 12 fresh cadaveric hands (12 thumbs and 48 long fingers) by two experts in ultrasound-guided thread transecting technique. The distal-to-proximal approach and the proximal-to-distal approach were each performed in 6 hands to determine which is safer and more effective in non-incisional trigger finger release (Fig. 1).
Two methods of non-incisional trigger finger release. A: Needle puncture sites and direction of the procedure (blue points indicate distal puncture sites, red points indicate proximal puncture sites, dotted lines indicate needle pathway under the skin, black arrow indicates the direction of the distal-to-proximal approach, and green arrow indicates the direction of the proximal-to-distal approach). B: The distal-to-proximal approach of non-incisional trigger finger release with ultrasound guidance. C: Looped Smartwire-01 with the distal-to-proximal approach before transecting the first annular pulley.
A schematic drawing illustrating the procedure is shown in Fig. 2. The cadaveric hands were placed in supination (palms facing upward). The entire A1 pulley and the flexor tendon were identified using ultrasound. A 20G Tuohy needle was bent at the distal shaft and connected to a syringe containing 5 mL of normal saline. Under longitudinal ultrasound guidance, the needle was inserted into the palm at a ___location beyond the A1 pulley, allowing for easier needle manipulation. The needle was advanced toward the A1 pulley, and upon reaching its end, a small amount of normal saline was injected to separate the surrounding tissues. The needle passed under the A1 pulley while simultaneously hydrodissecting its margins and then exited the skin beyond the full length of the A1 pulley. The Smartwire-01 was passed through the needle, which was then removed, leaving the Smartwire-01 in place beneath the A1 pulley. Another needle was inserted at the same entry point, passed above the A1 pulley, and exited at the same exit point. Then, the tip of the pre-inserted Smartwire-01 was passed through the needle tip to create a looped configuration that was positioned at the A1 pulley after withdrawing the needle. Prior to cutting, ultrasound was used to verify that the thread adequately encircled the entire A1 pulley. The A1 pulley was manually transected using a reciprocal motion of the thread under continuous ultrasound visualization, and the thread was subsequently removed.
Schematic drawing illustrating the non-incisional trigger finger release procedure, and corresponding ultrasound images obtained during the distal-to-proximal approach. A: (1) A bent 20G Tuohy needle was inserted into the palm at a point beyond the A1 pulley and advanced toward A1 pulley. Upon reaching the end of the A1 pulley, a small amount of normal saline was injected to separate the surrounding tissues. The needle was advanced beneath the A1 pulley with hydrodissection and exited the skin beyond the full length of the pulley. (2) Smartwire-01 was passed through the needle and positioned beneath the A1 pulley, after which the needle was removed. (3) A second needle was inserted at the same entry point, passed above the A1 pulley, and exited at the same exit point. (4) The tip of the pre-inserted Smartwire-01 was passed through the second needle to form a looped configuration around the A1 pulley. The needle was then withdrawn, leaving the thread looped in place. (5) The pulley was transected using a reciprocal motion of the Smartwire-01 under continuous ultrasound monitoring. (6) The thread was subsequently removed. B: Red arrowheads indicate the needle positioned beneath the A1 pulley. C: Blue arrowheads indicate the needle positioned above the A1 pulley, and white arrowheads indicate the Smartwire-01 beneath the A1 pulley. D: White arrowheads indicate the looped Smartwire-01 prior to transection of the A1 pulley.
After trigger finger release, anatomical dissection was performed by a single blinded anatomist to visually assess the cut sites and to evaluate procedural efficacy and safety. Efficacy was defined as complete transection of the A1 pulley, and safety was assessed by identifying any injury to adjacent structures, including the digital neurovascular bundle or flexor tendon (Fig. 3).
Data availability
The dataset generated and analyzed during this study is available from the corresponding author upon reasonable request.
References
Currie, K. B., Tadisina, K. K. & Mackinnon, S. E. Common hand conditions: A review. JAMA 327, 2434–2445 (2022).
Sbernardori, M. C. & Bandiera, P. Histopathology of the A1 pulley in adult trigger fingers. J. Hand Surg. Eur. Vol. 32, 556–559 (2007).
Drossos, K. et al. Correlations between clinical presentations of adult trigger digits and histologic aspects of the A1 pulley. J. Hand Surg. Am. 34, 1429–1435 (2009).
Gil, J. A., Hresko, A. M. & Weiss, A. C. Current concepts in the management of trigger finger in adults. J. Am. Acad. Orthop. Surg. 28, e642–e650 (2020).
Lunsford, D., Valdes, K. & Hengy, S. Conservative management of trigger finger: A systematic review. J. Hand Ther. 32, 212–221 (2019).
Peters-Veluthamaningal, C., van der Windt, D. A. & Winters, J. C. & Meyboom-de jong, B. Corticosteroid injection for trigger finger in adults. Cochrane Database Syst. Rev, CD005617 (2009).
Ma, S. et al. Efficacy of corticosteroid injection for treatment of trigger finger: A Meta-Analysis of randomized controlled trials. J. Invest. Surg. 32, 433–441 (2019).
Amirfeyz, R. et al. Evidence-based management of adult trigger digits. J. Hand Surg. Eur. Vol. 42, 473–480 (2017).
Bruijnzeel, H. et al. Adverse events of open A1 pulley release for idiopathic trigger finger. J. Hand Surg. Am. 37, 1650–1656 (2012).
Everding, N. G., Bishop, G. B., Belyea, C. M. & Soong, M. C. Risk factors for complications of open trigger finger release. Hand (N Y). 10, 297–300 (2015).
Wang, J., Zhao, J. G. & Liang, C. C. Percutaneous release, open surgery, or corticosteroid injection, which is the best treatment method for trigger digits? Clin. Orthop. Relat. Res. 471, 1879–1886 (2013).
Xie, P. et al. Stenosing tenosynovitis: evaluation of percutaneous release with a specially designed needle vs. open surgery. Orthopade 48, 202–206 (2019).
Sato, E. S., Dos Santos, G., Belloti, J. B., Albertoni, J. C., Faloppa, F. & W. M. & Treatment of trigger finger: randomized clinical trial comparing the methods of corticosteroid injection, percutaneous release and open surgery. Rheumatol. (Oxford). 51, 93–99 (2012).
Yavari, M., Modaresi, S. M., Hassanpour, S. E., Moosavizadeh, S. M. & Tabrizi, A. Clinical study between percutaneous Ultrasound-Guided release and open classic surgery in treating multiple trigger fingers. Adv. Biomed. Res. 12, 88 (2023).
Gilberts, E. C., Beekman, W. H., Stevens, H. J. & Wereldsma, J. C. Prospective randomized trial of open versus percutaneous surgery for trigger digits. J. Hand Surg. Am. 26, 497–500 (2001).
Bamroongshawgasame, T. A comparison of open and percutaneous pulley release in trigger digits. J. Med. Assoc. Thai. 93, 199–204 (2010).
Rajeswaran, G., Lee, J. C., Eckersley, R., Katsarma, E. & Healy, J. C. Ultrasound-guided percutaneous release of the annular pulley in trigger digit. Eur. Radiol. 19, 2232–2237 (2009).
Lapegue, F. et al. US-guided percutaneous release of the trigger finger by using a 21-gauge needle: A prospective study of 60 cases. Radiology 280, 493–499 (2016).
Colberg, R. E., Velez, J., Garrett, J. A., Hart, W. H., Fleisig, G. S. & K. & Ultrasound-guided microinvasive trigger finger release technique using an 18-gauge needle with a blade at the tip: A prospective study. PM R. 14, 963–970 (2022).
Jou, I. M. & Chern, T. C. Sonographically assisted percutaneous release of the a1 pulley: a new surgical technique for treating trigger digit. J. Hand Surg. Br. 31, 191–199 (2006).
Rojo-Manaute, J. M. et al. Sonographically guided intrasheath percutaneous release of the first annular pulley for trigger digits, part 1: clinical efficacy and safety. J. Ultrasound Med. 31, 417–424 (2012).
Guo, D. et al. Minimally invasive thread trigger digit release: a preliminary report on 34 digits of the adult hands. J. Hand Surg. Eur. Vol. 43, 942–947 (2018).
Guo, D. et al. A cadaveric study for the improvement of thread carpal tunnel release. J. Hand Surg. Am. 41, e351–e357 (2016).
Guo, D. et al. A non-scalpel technique for minimally invasive surgery: percutaneously looped thread transection of the transverse carpal ligament. Hand (N Y). 10, 40–48 (2015).
Guo, D., Guo, D., Guo, J., Schmidt, S. C. & Lytie, R. M. A clinical study of the modified thread carpal tunnel release. Hand (N Y). 12, 453–460 (2017).
Burnham, R. S. et al. A controlled trial evaluating the safety and effectiveness of Ultrasound-Guided looped thread carpal tunnel release. Hand (N Y). 16, 73–80 (2021).
Mende, K. et al. Early postoperative recovery after modified Ultra-Minimally invasive Sonography-Guided thread carpal tunnel release. J. Personalized Med. 13, 610 (2023).
Park, J., Kim, I. J., Park, H. Y., Heo, D. J. & Kim, J. M. A clinical study of thread carpal tunnel release with a newly developed thread: A retrospective pilot study. PLoS One. 17, e0276630 (2022).
Kim, I. J. & Kim, J. M. Long-Term outcomes of Ultrasound-Guided thread carpal tunnel release and its clinical effectiveness in severe carpal tunnel syndrome: A retrospective cohort study. J. Clin. Med. 13, 262 (2024).
Asserson, D. B. et al. Return to work following ultrasound guided thread carpal tunnel release versus open carpal tunnel release: a comparative study. J. Hand Surg. (European Volume). 47, 359–363 (2022).
Jengojan, S. et al. Ultrasound-guided thread versus ultrasound-guided needle release of the A1 pulley: a cadaveric study. Radiol Med. 129, 1513–1521 (2024).
Guo, D., Guo, D., Guo, J., McCool, L. C. & Tonkin, B. A cadaveric study of the thread trigger finger release: the first annular pulley transection through thread transecting technique. Hand (N Y). 13, 170–175 (2018).
Park, H. Y. et al. Cadaveric study of thread carpal tunnel release using newly developed thread, with a histologic perspective. Ann. Rehabil Med. 47, 19–25 (2023).
Chern, T. C., Jou, I. M., Yen, S. H., Lai, K. A. & Shao, C. J. Cadaveric study of sonographically assisted percutaneous release of the A1 pulley. Plast. Reconstr. Surg. 115, 811–822 (2005).
Smith, J., Rizzo, M. & Lai, J. K. Sonographically guided percutaneous first annular pulley release cadaveric safety study of needle and knife techniques. J. Ultras Med. 29, 1531–1542 (2010).
Rojo-Manaute, J. M. et al. Percutaneous intrasheath ultrasonographically guided first annular pulley release anatomic study of a new technique. J. Ultras Med. 29, 1517–1529 (2010).
Strickland, J. W. Flexor tendon injuries: I. Foundations of treatment. J. Am. Acad. Orthop. Surg. 3, 44–54 (1995).
Hauger, O. et al. Pulley system in the fingers: normal anatomy and simulated lesions in cadavers at MR imaging, CT, and US with and without contrast material distention of the tendon sheath. Radiology 217, 201–212 (2000).
Idler, R. S. Anatomy and biomechanics of the digital flexor tendons. Hand Clin. 1, 3–11 (1985).
Fiorini, H. J. et al. Anatomical study of the A1 pulley: length and ___location by means of cutaneous landmarks on the palmar surface. J. Hand Surg. Am. 36, 464–468 (2011).
Jongjirasiri, Y. Length and landmark of A1 pulley in hand: an anatomical study. J. Med. Assoc. Thai. 92, 41–46 (2009).
Funding
This work was supported by the National Research Foundation of Korea(NRF) grant funded by the Korea government(MSIT) (No.RS-2024-00337550).※ MSIT: Ministry of Science and ICT.
Author information
Authors and Affiliations
Contributions
J.M.K., I.J.K., and U.Y.L. contributed to the conceptualization and methodology. J.M.K. and I.J.K. conducted the formal analysis. J.M.K., I.J.K., H.Y.P., and S.H.K. carried out the investigation. K.E.N. and J.M.K. wrote the original draft of the manuscript. All authors reviewed and approval of the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The cadaveric specimens in this study were legally donated to the university-affiliated institute for applied anatomy. Informed consent was obtained from all the participants. The Institutional Review Board of the Catholic University of Korea approved this study. (Protocol number: MC22EISI0127) All experiments were performed in accordance with relevant guidelines and regulations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nam, K.E., Kim, I.J., Park, HY. et al. A cadaveric study of ultrasound guided nonincisional trigger finger release with newly developed threads. Sci Rep 15, 23532 (2025). https://doi.org/10.1038/s41598-025-08847-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-08847-w