Abstract
This study evaluated the association between admission to operation (ATO) time and preoperative deep vein thrombosis (DVT) in geriatric hip fractures under anticoagulation and mechanical thromboprophylaxis. Geriatric patients with hip fractures were screened between January 2015 and September 2019. We collected demographic information and DVT screening results from the medical system. Multivariate binary logistic regression and generalized additive models were used to identify the linear and non-linear associations between ATO and preoperative DVT. Also, we performed Propensity Score Matching (PSM) to test the robustness of our results in a real-world study. This study included one thousand seven hundred and thirty-five patients. There were 443, 726, and 566 patients in ATO ≤ 2d, 2d < ATO ≤ 4d, and ATO > 4d groups, respectively. Preoperative DVT occurred in 543 (31.3%) patients. There was a “J” type in curve fitting, and the result showed a curvilinear relationship between ATO and preoperative DVT. ATO of 3d was the inflection point. ATO increasing was not associated with an increase of preoperative DVT when ATO < 3d (OR = 0.83; 95%CI: 0.66–1.03; P = 0.09), whereas ATO increasing was associated with DVT (OR = 1.08; 95%CI: 1.04–1.14; P < 0.01) at ATO > 3d. In a real-world population of 1:1 under PSM, we found that the results were stable and the inflection point was the same as the total population. ATO is nonlinearly associated with preoperative DVT in geriatric patients with hip fractures under anticoagulation and mechanical thromboprophylaxis. The 3d was the important point in DVT formation. Each one-day increase in ATO was associated with an 8% increase in the incidence of preoperative DVT when ATO > 3d. Study Registration: This study was registered on the website of the Chinese Clinical Trial Registry (ChiCTR: ChiCTR2200057323).
Similar content being viewed by others
Introduction
Deep vein thrombosis (DVT) of the lower extremities is a common preoperative complication in hip fracture patients1. The DVT may lead to pulmonary embolism, long-term limb dysfunction, or even death, which will bring great pain to the patients and prolong the recovery time2,3. Therefore, preoperative prevention of DVT has become an important clinical intervention in the management of elderly hip fracture patients.
Studies have shown that the occurrence of DVT is associated with a variety of factors, including age, past DVT history, and the patient’s activity level4,5. However, among these factors, the interval between admission and surgery, called the time of admission to operation (ATO), appears to be an overlooked but potentially clinically important variable6,7. In elderly patients, fractures are often accompanied by pain, limited mobility, and the effects of underlying disease, and prolonged bed rest further exacerbates venous stasis and contributes to thrombus formation8. The delay in ATO usually means that patients may be bedridden for long periods while waiting for surgery, which slows blood flow and venous reflux, increases inflammatory response9,10, and increases the state of hypercoagulability of the blood11, which in turn provides favourable conditions for thrombosis12. The delayed ATO affects a patient’s overall prognosis13 and may also increase the risk of lower extremity thrombosis in some cases. A previous study found that patients who waited more than 48 h for surgery had a significantly higher rate of DVT compared to those who underwent earlier surgical intervention7. To better understand this association, some surgeons have begun to focus on the relationship between ATO and lower extremity DVT7,14,15. Clinically, early diagnosis and prevention of DVT are critical to a patient’s postoperative recovery, and surgeons have developed various thromboprophylaxis measures, such as anticoagulation therapy, mechanical thromboprophylaxis, and the use of antithrombotic stockings16.
Among the factors related to DVT, the ATO appears to be an overlooked but potentially clinically important variable. The effectiveness of existing thromboprophylaxis measures is closely related to the timing of the patient’s surgery, the type of surgery, and the presence of a preoperative thrombus. However, how to rationalize the ATO and minimize the time interval between the time to operation of hip fracture to reduce the occurrence of preoperative DVT effectively remains to be further explored.
With the increasing understanding of the relationship between ATO and DVT, the purpose of this study is to explore how to reduce the incidence of DVT through early intervention and optimization of surgical timing, aiming to help develop more precise treatment strategies in clinical practice, improve the prognosis of elderly hip fracture patients, and reduce the incidence of DVT.
Materials and methods
Institutional review boards approval
In this retrospective cohort study, we included older adults with hip fractures in the medical records from January 1, 2015, to September 30, 2019. All human procedures followed the 1964 Declaration of Helsinki and its later amendments.
This retrospective study was approved by the Ethics Committee of Xi’an Honghui Hospital (No. 202201009), and the Institutional Review Boards of Xi’an Honghui Hospital waived participants’ informed consent. All methods were performed following the relevant guidelines and regulations17.
Participants
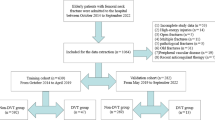
The demographic and clinical data of the patients were obtained from their original medical records. The inclusion criteria were as follows: (1) age of ≥ 65 years; (2) X-ray or computed tomography diagnosis of the femoral neck or intertrochanteric; (3) patients who were receiving surgical or conservative treatment in the hospital; and (4) availability of clinical data in the hospital. The exclusion criteria were as follows: (1) patients with previous pulmonary embolism or DVT history; (2) patients who already had the DVT before the admission, which were examined in other hospitals; (3) patients without the Doppler ultrasonography results of lower extremities in our hospital; (4) Patients who received antiplatelet aggregation therapy and anticoagulant therapy for other diseases before admission to the hospital.
Hospital treatment
Patients were examined before the operation. Prophylaxis for DVT was initiated on admission. Mechanical thromboprophylaxis was used. In patients without contraindications, low-molecular-weight heparin was injected subcutaneously to prevent DVT. Doppler ultrasonography was performed to diagnose DVT before the operation. The diagnostic criterion was the presence of a constant intraluminal filling defect. All patients received an ultrasonography examination of the bilateral lower extremities the day before the scheduled surgery.
Variables
The variables collected in this study were as follows: age, sex, injury mechanism, fracture classification, hypertension, diabetes, coronary heart disease, arrhythmia, hemorrhagic stroke, ischemic stroke, cancer, associated injuries, dementia, chronic obstructive pulmonary disease, hepatitis, gastritis, age-adjusted Charlson comorbidity index (aCCI), time from injury to admission, and time from injury to operation.
The dependent variable in this study was preoperative DVT in bilateral lower extremities, and the independent variable was the ATO. The other variables were potentially confounding factors.
Statistics analysis
Continuous variables were reported as mean ± standard deviation (Gaussian distribution) or median (minimum and maximum) (skewed distribution), and categorical variables were presented as frequencies and percentages. We used χ2 (categorical variables), one-way ANOVA (normal distribution), or the Kruskal–Wallis H test (skewed distribution) to test for differences among different delayed ATO values (tertiles). We used univariate and multivariate binary logistic regression models to test the association between ATO and preoperative DVT using three distinct models. Model 1 was a non-adjusted model without adjusted covariates. Model 2 was a minimally adjusted model with adjusted sociodemographic variables. Model 3 was a fully adjusted model with the covariates. To account for the non-linear relationship between ATO and preoperative DVT, we also used a generalized additive model to address the nonlinearity. In addition, a two-piecewise binary logistic regression model was used to explain nonlinearity further. Also, we performed Propensity Score Matching (PSM) to test the robustness of our results in a real-world study.
All analyses were performed using statistical software packages R (http://www.R-project.org, R Foundation) and EmpowerStats (http://www.empowerstats.com, X&Y Solutions Inc., Boston, MA, USA). Odds ratios (ORs) and 95% CIs were calculated. Statistical significance was set at a two-sided P value of < 0.05 (two-sided).
Results
Patient characteristics
In this retrospective cohort study, we screened and included 1735 patients who met the inclusion criteria. Table 1 lists the demographic and clinical characteristics of the study population after dividing the ATO tertiles into the ATO ≤ 2 d, 2 d < ATO ≤ 4 d, and ATO > 4 d groups. There were 443, 726, and 566 patients in every group, and females accounted for 71.3%, 72.0%, and 69.1% of the total number of patients in each group, respectively. As for the delay in ATO, the index of aCCI increased in every group, from 4.06 to 4.32. In the comorbidities, there were more patients with hypertension, diabetes, CHD, arrhythmia, and COPD in the ATO > 4 d group. Also, patients in the ATO > 4 d group had longer operation time, and more operative infusion. As for time to admission, the ATO > 4 d group had a mean of 68.1 h, less than 103.7 and 76.2 h in the ATO ≤ 2 d and 2 d < ATO ≤ 4 d group.
Preoperative DVT occurred in 543 (31.3%) patients with hip fractures. There were 142 (32.1%), 200 (27.6%), and 201 (35.5%) patients with lower extremity DVT in ATO ≤ 2 d, 2 d < ATO ≤ 4 d, and ATO > 4 d groups, respectively.
Univariate analysis of the association between variables and DVT
We investigated the association between these variables and DVT to identify the potential confounding factors in this study, as the criteria of P < 0.1, shown in Table 2. Sex, fracture classification, associated injuries, dementia, transfusion, and treatment strategy were identified as confounding factors.
Multivariate analysis between ATO and DVT
We used multivariate logistic regression to perform multifactorial logistic regression to demonstrate the association between ATO and DVT, as shown in Table 3. In addition, ATO was used as a categorical variable, followed by a continuous variable for P for trend test.
There were an identified association in non-adjusted model (OR = 1.05, 95%CI: 1.01–1.09, P = 0.02) and adjusted model I (OR = 1.05, 95%CI: 1.01–1.09, P = 0.02). Also, we found that ATO was associated with preoperative DVT when adjusting for the confounding factors in adjusted model II (OR = 1.05, 95%CI: 1.01–1.09, P = 0.02). However, there was no statistical association when dividing ATO into three groups: ATO ≤ 2 d, 2 d < ATO ≤ 4 d, and ATO > 4 d, or in the trend test calculated as a dummy variable. Therefore, the results were unstable in different statistical methods, and a non-linear association should be considered.
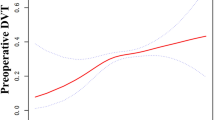
Curve fitting and analysis of threshold effect
The curve fitting between ATO and preoperative DVT is shown in Fig. 1. Therefore, the threshold effect was analyzed to identify the curvilinear relationship and the inflection point, shown in Table 4. Interestingly, the result showed a curvilinear relationship, and the ATO value of 3 d was the inflection point in the curve. More specifically, ATO was not correlated with preoperative DVT when ATO < 3 d (OR = 0.83; 95%CI: 0.66–1.03; P = 0.09), whereas ATO was associated with DVT (OR = 1.08; 95%CI: 1.03–1.14; P < 0.01) at ATO > 3d. The P for log-likelihood ratio test was 0.03, which means the difference between fitting the model by stand linear regression and two-piecewise linear regression is significant, and two-piecewise linear regression is more appropriate.
Propensity score matching (PSM)
To test the robustness of our results in the real world, we performed a sensitivity analysis using PSM. In total, 998 patients (57.5%) were successfully matched according to the ratio of 1:1 in each group. Sex, fracture classification, associated injuries, dementia, treatment strategy, and transfusion did not match between the two groups (Table 5). In the regression analysis under the PSM and PSM-adjusted models, we found that the results were stable and the inflection point was 3 d (Table 6).
Discussion
In this study, we aim to emphasize the detailed curve association between ATO and the development of preoperative DVT in geriatric patients with hip fractures. There was an obvious “J” type curve. In the early stage of ATO, the incidence of preoperative DVT was relatively low. When beyond some point of ATO, the incidence of preoperative DVT began to rise quickly. This study presents several new facts contributing to our understanding of this relationship. Firstly, through two-piecewise multivariate logistical regression, we have discovered a curve association between ATO and preoperative DVT in geriatric hip fracture patients. Specifically, an ATO of 3 d was identified as the inflection point in the curve fitting. When the ATO exceeded 3 d, we observed that each one-day increase in ATO was associated with an 8% increase in the incidence of preoperative DVT. Secondly, we obtained consistent results regarding the inflection point at 3 d of ATO using the PSM sample in a real-world study. However, the magnitude of the association between ATO and DVT was even more pronounced in the PSM analysis. In the PSM model, each one-day increase in ATO was associated with a 13% increase in the incidence of preoperative DVT(OR = 1.13). In the PSM-adjusted model, it was associated with an 11% increase (OR = 1.11). These findings further support the notion that ATO delay is a crucial risk factor for preoperative DVT in geriatric hip fracture patients.
Our results provide new insights into the timing of DVT risk in this patient population. While earlier studies showed surgery 48 h later was a risk factor for developing proximal DVT, our study pinpoints 3 d as a more precise and clinically relevant threshold. This distinction has important implications for clinical practice. Given that ATO delay is a significant risk factor for DVT, early surgical intervention may play a pivotal role in reducing the incidence of DVT in these patients. Our findings thus provide additional evidence for the potential advantages of early operation in geriatric hip fracture patients, which could guide the development of more optimal treatment strategies to minimize the risk of DVT and its associated complications.
As for the association between delay in operation and preoperative DVT, some studies reported that the delay in time from injury to admission and the delay in time from injury to surgery were the risk factors for preoperative DVT. Taoka et al. reported that a delay in surgery beyond 48 h after a hip fracture injury is a risk factor for developing venous thromboembolism and proximal DVT7. In a systematic review and meta-analysis, it was reported that a longer time from injury to admission and a longer time from injury to surgery were correlated with a high risk of DVT4,18. The time from injury to surgery often contains the time from injury to admission and the time of ATO. The management for individual patients varied in time from injury to admission, such as finding a fall, calling an emergency, and transferring to a trauma center so that the confounding factors would be diverse in the population in epidemiological analysis. Therefore, it was necessary to choose a stable independent to find the real association in the field of DVT after hip fractures. ATO was a stable and united indicator, under which an individual patient with hip fracture began to receive the same management in a standard trauma center. As for the association between ATO and preoperative DVT, two retrospective studies reported a linear correlation14,15. Zhang et al. reported that ATO was an independent risk factor for preoperative DVT in elderly patients with hip fractures, with OR = 1.88114. In the study by Xue et al., preoperative time was reported as an independent risk factor for preoperative DVT and the OR = 1.28 in multivariate logistic linear regression analysis15. These two studies reported the linear association between ATO and preoperative DVT. However, we found the curve association and 3 d was the inflection point in the curve fitting. Meanwhile, the PSM models showed the same results in a real-world study. Thus, curve association is the real relationship between ATO and DVT.
The popular pathogenesis of DVT formation is based on slow blood flow, damaged vascular endothelial cells, and a high coagulation state, proposed by Virchow19. DVT formation is a dynamic physiological process. Before admission, patients with hip fractures would enter a gap time without the strategy of prevention of DVT, such as pharmacologic anticoagulation and physical prophylaxis.
The hypercoagulation state was reported to start soon after fractures20. More than 50% of patients remained hypercoagulable 6 weeks after hip fracture despite thromboprophylaxis11. The hypercoagulable state promotes slower blood flow, while post-fracture bed rest further slows blood flow. In addition, other mechanisms of DVT formation have been reported, such as the inflammatory response after fracture9,21,22, which is also a key factor in the early formation of DVT, and C-reactive protein, IL-6, IL-8, TNF-alpha23, Gab2-MALT1 axis24 and NF-κB signalling pathway25 have been reported to be involved in the response. An immune response was also involved in DVT formation after hip fracture26. With the multiplicity of these underlying factors, DVT has begun to form, and it has been reported that the fastest time to form DVT was the first day after fracture27, and 68.2% of DVTs were diagnosed within 24 h of injury28. After admission, patients routinely receive anticoagulation and physical DVT prophylaxis after contraindications to anticoagulation have been ruled out. Because of the suppression of these strategies for preventing DVT, the speed of DVT formation after admission does not rise rapidly29,30. This also explains why the formation of DVT does not correlate with the ATO in the first 3 d of ATO.
However, it was reported that the median time of DVT 9 [IQR 4–17] in geriatric hip fractures31, and the DVT trend was stabilized within 1 week27. Actually, the hypercoagulable state, inflammatory response, and immune response will peak after fracture, so drug and physical prevention did not wholly prevent DVT formation. At the same time, the longer the ATO, the more often it is associated with poor patients’ comorbidities8, higher American Society of Anesthesiologists classes, and the Charlson Comorbidity Index, increased waiting time32. Because of these reasons, the formation of DVT will be increased in the late stage of the ATO, which explains the “J” shape of the curve fitting.
Previous studies have established a linear relationship between ATO and DVT14,15, whereas our study not only found a more meaningful curvilinear relationship, but also the key time point of 3d. In this study, we performed multifactorial logistic regression by adjusting confounding factors for DVT formation to explore a more reliable relationship between ATO and preoperative DVT. Later, the PSM method in the real-world setting was used to enhance the stability and reliability of our results. This is the first study to deeply explore the curve relationship between ATO and preoperative DVT formation in a large sample size. Also, this study has some limitations. First, this study was designed as a retrospective, providing limited evidence compared to a prospective study. Second, this study could not prove the causal relationship between ATO and preoperative DVT formation.
In conclusion, the ATO is nonlinearly associated with preoperative DVT in geriatric patients with hip fractures under anticoagulation and mechanical thromboprophylaxis. The 3 d was the important point in DVT formation. Each one-day increase in ATO was associated with an 8% increase in the incidence of preoperative DVT.
Data availability
The data was implemented by Xi’an Honghui Hospital. According to relevant regulations, the data could not be shared, but could request from correspondence author.
References
Zhang, B. F. et al. Deep vein thrombosis in bilateral lower extremities after hip fracture: a retrospective study of 463 patients. Clin. Interv Aging. 13, 681–689 (2018).
Larisa, C., Yaroslav, K. & Halyna, K. Danger of floating venous thrombosis: myth or reality?. Phlebology 38 (5), 322–333 (2023).
Marcello, D. N. & Nick vE, Harry, R. B. Deep vein thrombosis and pulmonary embolism. Lancet Diabetes Endocrinol. 388 (10063), 3060–3073 (2016).
Wang, T. et al. Risk factors for preoperative deep venous thrombosis in hip fracture patients: a meta-analysis. J. Orthop. Traumatol. 23 (1), 19 (2022).
He, S. Y. et al. Incidence and risk factors of preoperative deep venous thrombosis following hip fracture: a retrospective analysis of 293 consecutive patients. Eur. J. Trauma. Emerg. Surg. 48 (4), 3141–3147 (2022).
Liu, F. et al. Risk factors for prolonged preoperative waiting time of intertrochanteric fracture patients undergoing operative treatment. BMC Musculoskelet. Disord. 23 (1), 912 (2022).
Takuya, T. et al. Delayed surgery after hip fracture affects the incidence of venous thromboembolism. J. Orthop. Surg. Res. 18 (1), 630 (2023).
Bengoa, F. et al. High prevalence of deep vein thrombosis in elderly hip fracture patients with delayed hospital admission. Eur. J. Trauma. Emerg. Surg. 46 (4), 913–917 (2020).
Saribal, D. et al. Inflammatory cytokines IL-6 and TNF-α in patients with hip fracture. Osteoporos. Int. 30 (5), 1025–1031 (2019).
Lv, X. et al. Immune-mediated inflammatory diseases and risk of venous thromboembolism: A Mendelian randomization study. Front. Immunol. 13, 1042751 (2022).
You, D. et al. Identification of hypercoagulability with thrombelastography in patients with hip fracture receiving thromboprophylaxis. Can. J. Surg. 64 (3), E324–E329 (2021).
Stone, J. et al. Deep vein thrombosis: pathogenesis, diagnosis, and medical management. Cardiovasc. Diagn. Ther. 7 (Suppl 3), S276–S284 (2017).
Horton, I. et al. Delayed mobilization following admission for hip fracture is associated with increased morbidity and length of hospital stay. Can. J. Surg. 66 (4), E432–E438 (2023).
Zhang, L. et al. Analysis of high-risk factors for preoperative DVT in elderly patients with simple hip fractures and construction of a nomogram prediction model. BMC Musculoskelet. Disord. 23 (1), 441 (2022).
Xue, Z. et al. Optimal preoperative timing for prevention of deep vein thrombosis (DVT) in patients over 60 years of age with intertrochanteric fractures. Eur. J. Trauma. Emerg. Surg. 48 (5), 4197–4203 (2022).
Barrera, L. et al. Thromboprophylaxis for trauma patients. Cochrane Database Syst. Rev. 28 (3), CD008303 (2013).
Mathew, G. et al. STROCSS: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int. J. Surg. 96: 106165 (2021).
Takaomi, K., Takayuki, A. & Masaaki, M. Predictors of preoperative deep vein thrombosis in hip fractures: A systematic review and meta-analysis. J. Orthop. Sci. 28 (1), 222–232 (2021).
Chung, I. & Lip, G. Y. Virchow’s triad revisited: blood constituents. Pathophysiol Haemost Thromb. 33 (5–6), 449–454 (2003).
Tsantes, A. et al. Higher coagulation activity in hip fracture patients: A case-control study using rotational thromboelastometry. Int. J. Lab. Hematol. 43 (3), 477–484 (2021).
Ling, H. et al. Construction of a nomogram model for deep vein thrombosis in patients with tibial plateau fracture based on the systemic inflammatory response Index. BMC Musculoskelet. Disord. 25 (1), 240 (2024).
Zeng, G. et al. A nomogram model based on the combination of the systemic immune-inflammation index, body mass index, and neutrophil/lymphocyte ratio to predict the risk of preoperative deep venous thrombosis in elderly patients with intertrochanteric femoral fracture: a retrospective cohort study. J. Orthop. Surg. Res. 18 (1), 561 (2023).
Branchford, B. & Carpenter, S. The role of inflammation in venous Thromboembolism. Front. Pead. 6, 142 (2018).
Kondreddy, V. et al. The Gab2-MALT1 axis regulates thromboinflammation and deep vein thrombosis. Blood Cells. 140 (13), 1549–1564 (2022).
Wang, Z. et al. Research progress of NF-κB signaling pathway and thrombosis. Front. Immunol. 14, 1257988 (2023).
Chen, X. et al. A nomogram model based on the systemic immune-inflammation index to predict the risk of venous thromboembolism in elderly patients after hip fracture: A retrospective cohort study. Heliyon 10 (6), e28389 (2024).
Cong, Y. X. et al. Dynamic observation and risk factors analysis of deep vein thrombosis after hip fracture. PLoS One. 19 (6), e0304629 (2024).
Kim, Y. V. et al. Prevalence of venous thromboembolism after immediate screening in hip fracture Patients. Hip Pelvis, 36 (1), 47-54 (2024).
Ahmed, M. N. et al. Effectiveness of thromboprophylaxis agents following hip fracture: a systematic review and network meta-analysis. JB JS Open Access 8(4), e23.00064 (2023).
Sobieraj, D. M. et al. Comparative effectiveness of combined Pharmacologic and mechanical thromboprophylaxis versus either method alone in major orthopedic surgery: a systematic review and meta-analysis. Pharmacotherapy 33 (3), 275–283 (2013).
Malik, A. et al. Timing of complications following surgery for geriatric hip fractures. J. Clin. Orthop. Trauma. 10 (5), 904–911 (2019).
Cato, K. et al. Waiting time for hip fracture surgery: hospital variation, causes, and effects on postoperative mortality: data on 37,708 operations reported to the Norwegian hip fracture register from 2014 to 2018. Bone Jt. Open. 2 (9), 710–720 (2021).
Acknowledgements
Not applicable.
Funding
This work was supported by the Foundation of Xi’an Municipal Health Commission (Grant Number: 2024ms15).
Author information
Authors and Affiliations
Contributions
According to the definition given by the International Committee of Medical Journal Editors (ICMJE), the authors listed above qualify for authorship based on making one or more of the substantial contributions to the intellectual content of the following: Conceived and designed the study: Bin-Fei Zhang. Performed the study: Wen-Si Qiang, Lu Dang, Yi-Lun Wu and Bin-Fei Zhang. Analyzed the data: Bin-Fei Zhang. Wrote the manuscript: Wen-Si Qiang.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Honghui Hospital, Xi’an Jiaotong University (No. 202201009), and the Institutional Review Boards of Xi’an Honghui Hospital waived participants’ informed consent.
Consent for publication
The work described has not been published before (except in the form of an abstract or as part of a published lecture, review, or thesis); it is not under consideration for publication elsewhere; and all co-authors have approved its publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qiang, WS., Dang, L., Wu, YL. et al. The waiting time of admission to operation was associated with preoperative deep vein thrombosis in geriatric hip fracture. Sci Rep 15, 23843 (2025). https://doi.org/10.1038/s41598-025-09255-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-09255-w