Abstract
The benefit of adjuvant chemotherapy (CT) for hormone receptor-negative T1a and T1bN0M0 breast cancer remains uncertain. Our study was to explore prognostic value and identify candidates of adjuvant CT for these patients. The data of hormone receptor-negative T1a and T1bN0M0 breast cancer patients were extracted from the Surveillance, Epidemiology, and End Results (SEER) database from 2010 to 2015. All patients were divided into two groups according to the history of adjuvant CT namely the CT group and the no CT (No CT) group. Univariate and multivariate Cox regression analysis were utilized to identify factors linked with cancer specific survival (CSS) and overall survival (OS) for the patients. Kaplan-Meier method was employed to determine survival benefit of adjuvant CT. A total of 3889 patients were included. After propensity score-matching, 1217 patients were assigned to the CT group and 1217 patients were assigned to the No CT group respectively. Based on multivariate Cox regression analysis of OS, older age, single, T1b stage, triple-negative tumor and absence of adjuvant CT were identified as risk factors related to OS. Besides, multivariable Cox regression analysis of CSS showed significant association between grade III+IV, T1b stage, triple-negative tumor and absence of adjuvant CT and CSS. The results from Kaplan-Meier curves revealed that adjuvant CT could bring OS benefit for these patients with more than two risk factors and could improve CSS for the patients with more than one risk factor. Our study supports the implementation of individualized strategies for hormone receptor-negative T1a and T1bN0M0 breast cancer patients. Adjuvant CT was recommended for potential beneficial patients after undertaking a risk-benefit discussion.
Similar content being viewed by others
Introduction
Breast cancer is one of the most common diagnosed malignancy, which leads to an estimated 2.3 million new cases and an estimated 666,000 new deaths in 2022 around the world1. With increased health awareness and widespread use of diagnostic imaging, we have witnessed an increasing frequency of T1a and T1bN0M0 breast cancer2,3,4. In the absence of adjuvant therapy, these patients show a relatively low incidence of death and recurrence5,6. Hence, the application of adjuvant chemotherapy (CT) for hormone receptor-negative T1a and T1bN0M0 breast cancer remains controversial.
Hormone receptor-negative T1a and T1bN0M0 breast cancer was a subtype characterized by no expression of estrogen receptor (ER) and progesterone receptor (PR). It was well established that adjuvant CT is effective in reducing disease recurrence and improving survival for breast cancer7. According to the National Comprehensive Cancer Network guidelines, adjuvant CT was recommended consideration for hormone receptor-negative T1a and T1bN0M0 breast cancer8. However, there were no specific guidelines that guide patient selection for adjuvant CT to data. Some experts hold that adjuvant CT should be empirically applied to these patients because it behaved more aggressively in the absence of targets for endocrine therapy9. Whereas, toxic side-effects and medical costs of adjuvant CT may be the primary obstacles that stop these patients from receiving adjuvant CT10,11. Some scholars believed that all these patients could be exempted from adjuvant CT because they exhibited excellent prognosis12,13. Besides, limited studies concentrated on the administration and survival benefit of adjuvant CT for hormone receptor-negative T1a and T1bN0M0 breast cancer. As a result, decision-making of adjuvant CT for these patients is puzzling and challenging in clinical practice. A heat debate about benefit or harm of adjuvant CT for hormone receptor-negative T1a and T1bN0M0 breast cancer patients has been aroused. Therefore, a precise selection of the potential patient population who can benefit from adjuvant CT was necessary and helpful.
Hence, we examined the survival benefit of adjuvant CT on the hormone receptor-negative T1a and T1bN0M0 breast cancer patients from Surveillance, Epidemiology, and End Results (SEER) database to explore prognostic value of adjuvant CT on the population. In addition, we implemented a series of survival analyses to choose candidates who may gain survival benefit from adjuvant CT.
Materials and methods
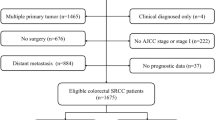
Study population
All included cases were from the SEER database, whose data were retrospectively reviewed. Cases met the following inclusion criteria were enrolled in this study: (1) female patients diagnosed breast cancer from 2010 to 2015; (2) pathological staged at T1a and T1bN0M0; (3) negative ER and PR status; and (4) breast cancer as the first primary malignancy. The cases fulfilled the following criteria were excluded: (1) male breast cancer patients; (2) unknown tumor grade, human epidermal growth factor receptor-2 (HER2) status and cause of death; (3) missing survival time or survival time was 0; and (4) received neoadjuvant chemotherapy. All cases were split into two groups according to the history of adjuvant CT namely the chemotherapy group (CT) and the no chemotherapy group (No CT). The informed consent of patients and ethical approval were waived by the Ethics Committee of the First Affiliated Hospital of Nanchang University because the data were publicly available from SEER database.
Variables
Several variables including age, gender, race, marital status, tumor grade, TNM stage, ER, PR, HER2 and survival status and survival months were gathered. The age at diagnosis was categorized into < 70 and ≥ 70. Tumor grade was split into two groups namely the grade I+II group and the grade III+IV group. The 7th AJCC staging system was utilized to stage all cases. Tumor diameter ranging from 2 to 5 mm was divided into T1a and from 6 to 10 mm was divided into T1b.
Statistical analysis
Statistical analysis was performed by SPSS software (version 26.0, IBM, Chicago, IL, USA) and R software (version 3.6.3). A 1:1 propensity score-matching (PSM) analysis was performed according to age, tumor grade, pathological T stage, molecular subtype and marital status with a caliper width of 0.01. Categorical variables which were described as numbers and percentages were evaluated by means of chi-square test. Risk factors linked with overall survival (OS) and cancer specific survival (CSS) were identified by univariate and multivariate Cox regression analysis. The Kaplan-Meier curve was utilized to explore the effect of adjuvant CT on OS and CSS determined by log-rank test. Statistical threshold was set at P < 0.05.
Results
Baseline characteristics of study population
A total of 3889 eligible cases were enrolled in this study, which includes 2001 cases in the CT group and 1888 cases in the No CT group. As was shown in Table 1, we noted there was significant difference in terms of T stage, tumor grade, molecular subtype, marital status and age between the two groups. There was no difference in race between the two groups. After PSM analysis, a total of 1217 cases were enrolled in the CT group and 1217 cases were enrolled in the No CT group respectively. No difference was noted in the above baseline characteristics between the two groups after PSM analysis.
Identification of prognostic factors
We conducted Cox regression analysis on all eligible cases to explore risk factors related to hormone receptor-negative T1a and T1bN0M0 breast cancer. As was displayed in Fig. 1, age, marital status, T stage, molecular subtype and the history of adjuvant CT were linked with OS for this disease based on the univariate Cox regression analysis (all P < 0.05). After multivariate Cox regression analysis, we found that these factors were also linked with OS (all P < 0.05). As Fig. 2 showed, tumor grade, T stage, molecular subtype and the history of adjuvant CT were relevant to CSS for this disease according to the univariate Cox regression analysis (all P < 0.05). Of note, the results of multivariate Cox regression analysis indicated that these factors were also relevant to CSS (all P < 0.05).
Survival benefit of adjuvant CT
Based on the number of risk factors identified (except the history of adjuvant CT), all patients were categorized into different subgroups (Tables 2 and 3). Survival analyses were implemented on the different subgroups before and after PSM analysis to investigate survival benefit of adjuvant CT. The results from Fig. 3 implied that the patients with more than two risk factors could gain OS benefit from adjuvant CT. The findings from Fig. 4 revealed that adjuvant CT could bring CSS benefit for the patients with more than one risk factor.
Overall survival analysis on total cohort stratified by the number of risk factor related to overall survival. (A) No risk factor; (B) One risk factor; (C) Two risk factors; (D) More than two risk factors. Overall survival analysis on the cohort after propensity score matching stratified by the number of risk factor related to overall survival. (E) No risk factor; (F) One risk factor; (G) Two risk factors; (H) More than two risk factors.
Cancer specific survival analysis on total cohort stratified by the number of risk factor related to cancer specific survival. (A) No risk factor; (B) One risk factor; (C) More than one risk factor. Cancer specific survival on the cohort after propensity score matching stratified by the number of risk factor related to cancer specific survival. (D) No risk factor; (E) One risk factor; (F) More than one risk factor.
Discussion
In this study, we found that adjuvant CT was linked with OS and CSS for T1a and T1bN0M0 breast cancer. Besides, we noted that adjuvant CT could achieve survival benefit for subgroups with higher risk of disease recurrence. In addition, we identified the candidates who could benefit from adjuvant CT. As a consequence, the results indicated that individual decision of adjuvant CT should be made after comprehensive evaluation of clinicopathologic characteristics.
To data, it is inconclusive to apply adjuvant CT to T1a and T1bN0M0 breast cancer patients. Excellent prognosis of T1a and T1bN0M0 breast cancer making administering adjuvant CT to these patients seem unnecessary. However, survival benefit brought by adjuvant CT may lead to under-treatment by omitting adjuvant CT. Hence, it is crucial to clarify the survival beneficial effect of adjuvant CT on those patients. After conducting Cox regression analysis on the cohort from SEER database, we noticed that adjuvant CT could bring CSS and OS survival benefit for these patients which was consistent with previous studies14,15. While existing evidence showed that adjuvant CT did not achieve survival benefit for these patients16,17. Controversial conclusions may be attributed to the different study cohort or limited sample size. Different study cohort exhibit diverse baseline characterizes, which may affect the outcomes of adjuvant CT. In addition, the regimens and dosages of adjuvant CT are another confounding factors for assessing the survival benefit. As a consequence, further studies which minimized the confounders are warranted to clarify the survival benefit of adjuvant CT for T1a and T1bN0M0 breast cancer patients. Besides, in agreement with prior studies, we noticed that tumor grade, T stage and molecular subtype were linked with prognosis18,19,20. The conclusions suggested that treatment effect of adjuvant CT may be influenced by other factors. The extent of survival benefit varies from person to person due to different baseline characterizes, which imply that precise personalized administration of adjuvant CT should take all prognostic indexes into consideration.
To better assistant the decision of adjuvant CT for T1a and T1bN0M0 breast cancer patients in clinical practice, we performed survival analysis on subgroups according to risk stratification to explore the prognostic value of adjuvant CT. As a result, a comprehensive survival analysis was carried out on the cohort stratified by the number of risk factors to assessed the necessity of adjuvant CT. We found that the patients with more than two risk factors could benefit from adjuvant CT as regarding OS. There were many studies focused on the survival benefit of adjuvant CT for T1a and T1bN0M0 breast cancer patients. Several researches concluded that adjuvant CT could achieve survival benefit for these patients21,22,23. While An et al. and Nonneville et al. demonstrated adjuvant CT could not bring survival benefit for these patients24,25. The contradictory results indicated that there may be an optimal cut-off to select the patients who could benefit from adjuvant CT. Hence, it is imperative to find the threshold that determines survival benefit of adjuvant CT to avoid over-treatment or under-treatment of these patients. In this study, separated survival analyses were performed on stratified subgroups, which may be a feasible way to find the optimal threshold. Besides, the results revealed that adjuvant CT could bring CSS benefit for the patients with more than one risk factor who are identified as high-risk patients. According to our findings, we recommend administration of adjuvant CT for these high-risk patients. Surprisingly, the findings go exactly counter to conclusion of Daniela,s study that adjuvant CT was useless for in lymph node-negative, T1a triple-negative breast cancer26. This may be attributed to different study cohort. We include hormone receptor-negative T1a and T1bN0M0 breast cancer patients, while that study focuses on lymph node-negative, T1a triple-negative breast cancer patients. One another explanation is that we implemented survival analyses on subgroups stratified by the number of risk factors, while Daniela,s study drew conclusion based on whole study cohort. Hence, more studies are warranted to verify our conclusions. Altogether, these results may help develop management strategies and gain understanding of adjuvant CT for this disease.
To our best of knowledge, this is the first study that clarifies the survival benefit of adjuvant CT based on risk stratification. Additionally, this study aids the decision of adjuvant CT by identifying candidate who may benefit from adjuvant CT for T1a and T1bN0M0 breast cancer patients. However, with increased understanding of breast cancer, the precise decision of adjuvant CT may be made instead of solely relying on clinicopathological indicators. Accumulating evidence showed genetic counseling may enable precise determination of adjuvant CT27,28. Moreover, a series of encouraging results implied that immunotherapy could result in improved survival, which indicated omission of adjuvant CT may be feasible29,30. Immunotherapy may be the way out of the dilemma of the administration of adjuvant CT for the patients. Besides, great breakthroughs in target therapy making omission of adjuvant CT reasonable for HER2-enriched breast cancer31,32,33. Improvement in immunotherapy and target therapy has optimized management strategies of breast cancer, which may resolve the issue of adjuvant CT for hormone receptor-negative T1a and T1bN0M0 breast cancer. In addition, fewer cycles of adjuvant CT or low-toxicity adjuvant CT regimen may be another feasible way to address this issue34.
There exist many limitations in our study. First, information regarding prognostic factors such as Ki-67 and lymphovascular invasion are not available in the SEER database that are crucial for assessing the risk of recurrence. Besides, we did not perform external validation to verify the conclusions that weakens the strength of the conclusions. Hence, we should interpret the conclusions cautiously. In addition, the regimen and dose of adjuvant CT are not provided in the SEER database, which are essential factors to determine the effect of adjuvant CT on OS and CSS. Different regimen and dose of adjuvant CT of patients may act as a confounder influence statistical power. Besides, the clinical managements of HER2-positive and triple-negative breast cancer are different, so it is better to investigate survival impact of adjuvant CT on them separately. While we failed to conduct a separated analysis to explore survival benefit of CT for HER2-positive and triple-negative T1a and T1bN0M0 breast cancer owing to small sample size. Furthermore, a limited study cohort size may also damage statistical power. Further randomized, controlled clinical trials are warranted to confirm our conclusions.
Conclusion
Our results confer OS and CSS advantages of adjuvant CT for T1a and T1bN0M0 breast cancer patients with high risk of recurrence. Additionally, our study indicated that T1a and T1bN0M0 breast cancer patients can be stratified into subgroups that could benefit from adjuvant CT and is unsuitable for adjuvant CT. Hence, when considering adjuvant CT for T1a and T1bN0M0 breast cancer patients, it is wise to tailor personal therapeutic approaches for these patients based on clinicopathological parameters.
Data availability
All data and materials used in present study are available from the corresponding author on reasonable request.
References
Bray, F. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J. Clin. 74, 229–263. https://doi.org/10.3322/caac.21834 (2024).
Benitez Fuentes, J. D. et al. Global stage distribution of breast Cancer at diagnosis: A systematic review and meta-analysis. JAMA Oncol. 10, 71–78. https://doi.org/10.1001/jamaoncol.2023.4837 (2024).
Rahman, W. T. & Helvie, M. A. Breast cancer screening in average and high-risk women. Best Pract. Res. Clin. Obstet. Gynaecol. 83 https://doi.org/10.1016/j.bpobgyn.2021.11.007 (2022).
Welch, H. G., Prorok, P. C., O’Malley, A. J. & Kramer, B. S. Breast-Cancer tumor size, overdiagnosis, and mammography screening effectiveness. N. Engl. J. Med. 375, 1438–1447 (2016).
Caswell-Jin, J. L. et al. Analysis of breast Cancer mortality in the US-1975 to 2019. JAMA 331, 233–241. https://doi.org/10.1001/jama.2023.25881 (2024).
Larsen, I. K., Myklebust, T. Å., Johannesen, T. B., Møller, B. & Hofvind, S. Stage-specific incidence and survival of breast cancer in Norway: The implications of changes in coding and classification practice. Breast 38, 107–113. https://doi.org/10.1016/j.breast.2017.12.001 (2018).
Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: An overview of the randomised trials. Lancet (London England) 365, 1687–1717 (2005).
National Comprehensive Cancer Network. BREAST CANCER. Version 3. (2024). https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1419. Accessed 17 June 2024.
Parise, C. A. & Caggiano, V. Risk of mortality of node-negative, ER/PR/HER2 breast cancer subtypes in T1, T2, and T3 tumors. Breast Cancer Res. Treat. 165, 743–750. https://doi.org/10.1007/s10549-017-4383-5 (2017).
Andrews, C. et al. Facilitators and barriers to reducing chemotherapy for early-stage breast cancer: A qualitative analysis of interviews with patients and patient advocates. BMC Cancer 22, 141. https://doi.org/10.1186/s12885-022-09189-w (2022).
Tao, J. J., Visvanathan, K. & Wolff, A. C. Long term side effects of adjuvant chemotherapy in patients with early breast cancer. Breast 24 (Suppl 2), S149–S153. https://doi.org/10.1016/j.breast.2015.07.035 (2015).
Hanrahan, E. O. et al. Overall survival and cause-specific mortality of patients with stage T1a,bN0M0 breast carcinoma. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 25, 4952–4960 (2007).
Iqbal, J., Ginsburg, O., Rochon, P. A., Sun, P. & Narod, S. A. Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the United States. JAMA 313, 165–173. https://doi.org/10.1001/jama.2014.17322 (2015).
Ignatov, T., Eggemann, H., Burger, E., Costa, S. D. & Ignatov, A. Management of small T1a/b breast cancer by tumor subtype. Breast Cancer Res. Treat. 163, 111–118. https://doi.org/10.1007/s10549-017-4168-x (2017).
Liu, L. et al. Retrospective study of treatment patterns and natural history of patients with T1a/b N0 triple-negative breast cancers: A single-Institution experience. Oncology 101, 765–772. https://doi.org/10.1159/000533149 (2023).
Olszewski, A. J. et al. Effects of adjuvant chemotherapy in HER2-positive or triple-negative pT1ab breast cancers: A multi-institutional retrospective study. Breast Cancer Res. Treat. 138, 215–223. https://doi.org/10.1007/s10549-013-2423-3 (2013).
Wu, C. et al. Tumor size is associated with adjuvant chemotherapy benefit in T1N0M0 triple-negative breast cancer: A multicenter and propensity score matched analysis. Gland Surg. 12, 1375–1386. https://doi.org/10.21037/gs-23-189 (2023).
Howlader, N., Cronin, K. A., Kurian, A. W. & Andridge, R. Differences in breast cancer survival by molecular subtypes in the United States. Cancer Epidemiol. Biomarkers Prev. 27, 619–626. https://doi.org/10.1158/1055-9965.EPI-17-0627 (2018).
Johansson, A. L. V. et al. In modern times, how important are breast cancer stage, grade and receptor subtype for survival: A population-based cohort study. Breast Cancer Res. 23, 17. https://doi.org/10.1186/s13058-021-01393-z (2021).
Rakha, E. A. et al. Histologic grading is an independent prognostic factor in invasive lobular carcinoma of the breast. Breast Cancer Res. Treat. 111, 121–127 (2008).
An, X. et al. Adjuvant chemotherapy for small, lymph node-negative, triple-negative breast cancer: A single-center study and a meta-analysis of the published literature. Cancer 126 (16), 3837–3846. https://doi.org/10.1002/cncr.32878 (2020).
Hassing, C. M. S. et al. Adjuvant treatment with trastuzumab of patients with HER2-positive, T1a-bN0M0 breast tumors: A systematic review and meta-analysis. Crit. Rev. Oncol./Hematol. 184, 103952 (2023). https://doi.org/10.1016/j.critrevonc.2023.103952
Stüber, T. et al. Are there breast cancer patients with node-negative small tumours, who do not benefit from Adjuvant systemic therapy? Oncology 92, 317–324. https://doi.org/10.1159/000455050 (2017).
Carbajal-Ochoa, W., Bravo-Solarte, D. C., Bernal, A. M. & Anampa, J. D. Benefit of adjuvant chemotherapy in lymph node-negative, T1b and T1c triple-negative breast cancer. Breast Cancer Res. Treat. 203, 257–269. https://doi.org/10.1007/s10549-023-07132-6 (2024).
de Nonneville, A. et al. Adjuvant chemotherapy in pT1ab node-negative triple-negative breast carcinomas: Results of a national multi-institutional retrospective study. Eur. J. Cancer 84, 34–43. https://doi.org/10.1016/j.ejca.2017.06.043 (2017).
Bravo-Solarte, D. C., Zhang, F. & Anampa, J. D. Assessment of use and impact of chemotherapy in lymph node-negative, T1a triple-negative breast cancer. Clin. Breast Cancer 23, 763–773. https://doi.org/10.1016/j.clbc.2023.08.002 (2023).
Bharucha, P. P. et al. Genetic testing and screening recommendations for patients with Hereditary breast Cancer. Radiographics 40, 913–936. https://doi.org/10.1148/rg.2020190181 (2020).
Tischler, J., Crew, K. D. & Chung, W. K. Cases in precision medicine: The role of tumor and germline genetic testing in breast cancer management. Ann. Intern. Med. 171, 925–930. https://doi.org/10.7326/M18-2417 (2019).
Blackley, E. F. & Loi, S. Targeting immune pathways in breast cancer: Review of the prognostic utility of TILs in early stage triple negative breast cancer (TNBC). Breast 48 (Suppl 1), S44–S48. https://doi.org/10.1016/S0960-9776(19)31122-1 (2019).
Dixon-Douglas, J. & Loi, S. Immunotherapy in early-stage triple-negative breast cancer: Where are we now and where are we headed? Curr. Treat. Options Oncol. 24, 1004–1020. https://doi.org/10.1007/s11864-023-01087-y (2023).
de Haas, S. L. et al. Tumor biomarkers and efficacy in patients treated with trastuzumab emtansine + pertuzumab versus standard of care in HER2-positive early breast cancer: An open-label, phase III study (KRISTINE). Breast Cancer Res. 25, 2. https://doi.org/10.1186/s13058-022-01587-z (2023).
Dowling, G. P. et al. Neoadjuvant trastuzumab deruxtecan (T-DXd) with response-directed definitive therapy in early stage HER2-positive breast cancer: A phase II study protocol (SHAMROCK study). BMC Cancer 24, 91. https://doi.org/10.1186/s12885-024-11851-4 (2024).
Prat, A. et al. HER2-enriched subtype and ERBB2 expression in HER2-positive breast cancer treated with dual HER2 blockade. J. Natl. Cancer Inst. 112, 46–54. https://doi.org/10.1093/jnci/djz042 (2020).
Duan, F. et al. Screening optimal candidates with operable, early-stage triple-negative breast cancer benefitting from capecitabine maintenance: A post-hoc analysis of the SYSUCC-001 study. Breast 76, 103740. https://doi.org/10.1016/j.breast.2024.103740 (2024).
Acknowledgements
This study was supported by grant from National Natural Science Foundation of China (No 81960441) and Jiangxi Provincial Natural Science Foundation of China (No 20232BAB206100).
Author information
Authors and Affiliations
Contributions
YX-L: study design, manuscript writing and data analyses; HH-L, JS-Land CL-W: data collection and data analyses; JS-Z and QH-T: study design, revising manuscript and supervision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical statement
The data are publicly available, the informed consent of patients and ethical approval were waived by the Ethics Committee of the First Affiliated Hospital of Nanchang University.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, Y., Li, H., Li, J. et al. Prognostic value of adjuvant chemotherapy for hormone receptor-negative T1a and T1bN0M0 breast cancer patients. Sci Rep 15, 2260 (2025). https://doi.org/10.1038/s41598-025-85434-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-85434-z