Abstract
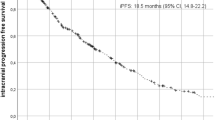
Brain metastases (BM) are the most prevalent intracranial malignancies. Approximately 30–40% of cancer patients develop BM at some stage of their illness, presenting with a high incidence and poor prognosis. Our clinical findings indicate a significant disparity in the efficacy between non-enhanced and enhanced lung cancer BM. Therefore, the aim of this study is to conduct a longitudinal MRI evaluation of the therapeutic effect of non-enhanced lung cancer BM, thereby enabling improved efficacy prediction and more personalized treatment plans. We conducted a retrospective analysis of clinical and imaging data from 72 patients with lung cancer BM. Exclusion criteria included participants with a history of primary brain tumors, other malignancies, or neurological symptoms. We performed a longitudinal MRI evaluation of 8 patients with non-enhanced BM who met the eligibility criteria. The response to systemic therapy was locally assessed using the Neuro-Oncology response assessment criteria (RANO 2.0). A total of 8 patients were included in this study, comprising 4 cases of non-enhanced BM and 4 cases featuring both enhanced and non-enhanced BM. The median follow-up time for non-enhanced BM was 19 months, with a disease control rate of 50%. In contrast, the median progression-free follow-up time for enhanced BM was 35.5 months, yielding a disease control rate of 100%. After standardized treatment in accordance with clinical guidelines, patients with enhanced BM exhibited significantly better therapeutic outcomes than those with non-enhanced BM. Cases 1–4 demonstrated non-enhanced or mildly circular-enhanced lung cancer BM, with the sizes of all 4 lesions increasing by over 60% within approximately one year, indicating disease progression. In cases 5–8, each patient presented with two lesions: enhanced (Foci 1) and non-enhanced (Foci 2) BM. Comparative analysis of Foci 1 and Foci 2 revealed significantly weaker treatment responses in non-enhanced lesions (Patients 7–8), with Patient 5 exhibiting disease progression without any response. This study demonstrates that, following standardized treatment protocols aligned with clinical guidelines, the therapeutic effect of non-enhanced lung cancer BM is inferior to that of enhanced BM. Evaluating the enhancement type of lung cancer BM is essential for efficacy prediction and holds important implications for treatment guidance.
Similar content being viewed by others
Introduction
Brain metastases (BM) are the most prevalent malignant tumors in the central nervous system (CNS), with an estimated 30–40% of cancer patients developing BM at some stage throughout their illness1, which is associated with a high incidence and poor prognosis. A recent study indicated that as many as 50% of patients with advanced non-small cell lung cancer (NSCLC) experience brain metastases, contributing significantly to mortality in this population2. Despite numerous advancements in the treatment of NSCLC—including surgery, whole-brain radiation therapy, stereotactic radiation therapy, chemotherapy, targeted therapy, and immunotherapy—the prognosis remains unfavorable, with brain metastases playing a crucial role in this outcome.
Davis et al. reported that the lung is the most common source of primary tumors that lead to BM, accounting for 20–40% of cases3. The distribution of BM correlates with tissue flow and volume, with approximately 80% located in the cerebral hemispheres, 15% in the cerebellum, and 5% in the brainstem4. Contrast-enhanced MRI is the standard method for screening BM, providing comprehensive details on the ___location and characteristics of brain parenchymal metastases5. BM disrupt the integrity of the blood-brain barrier (BBB), and the disruption can exhibit heterogeneity. Chemotherapy agents can penetrate the BBB associated with lung cancer BM, though they struggle to cross the normal BBB6. Enhanced MRI serves as the gold standard for evaluating BBB dysfunction and can indirectly assess drug exudation, analogous to gadolinium or magnetic nanoparticle permeability7,8.
BM predominantly occur in patients with lung adenocarcinoma, particularly those harboring epidermal growth factor receptor (EGFR) mutations or anaplastic lymphoma kinase (ALK) rearrangements. These metastases are often susceptible to cystic transformation and tend to show diminished responsiveness to treatment9. Traditionally, cystic metastases have been associated with poor therapeutic outcomes and unfavorable prognoses10, and BM are widely recognized as a significant prognostic marker for malignant tumors, especially in cases involving cystic BM, for which treatment approaches remain contentious11. Reports indicate that the rate of tumor reduction in cystic BM is slower compared to solid BM following standard treatment protocols12. Potential factors contributing to the development of cystic masses in cystic BM may include BBB destruction or cystic transformation in tumors with low histological grades10. Cystic BM may appear as cystic or necrotic tumors with thin- or thick-wall enhancement and may exhibit mild to moderate perifocal edema. In some instances, thin-walled cystic metastases may show no enhancement or only minimal enhancement13. MRI findings for non-enhanced BM typically reveal homogeneous low signal intensity on T1-weighted images (WI) and high signal intensity on T2-WI sequences, with diffusion showing no restrictions on diffusion-weighted imaging (DWI), resembling high-tension cysts. Cystic BM are a unique subset of non-enhanced brain metastases, and the specifics of their internal cystic components remain undetermined9,10. However, the therapeutic efficacy and prognostic implications of non-enhanced lung cancer BM have not been reported in the literature.
In clinical observations, we identified a particular form of lung adenocarcinoma BM that exhibited significantly high signal intensity on T2-WI, markedly low signal intensity on T1-WI, and absent perifocal edema, along with low signal intensity on DWI, resembling cystic metastases, and showed no enhancement or only mild circular enhancement on enhanced sequences. We defined these lesions as non-enhanced BM (Fig. 1). Conversely, BM exhibiting varying degrees of enhancement were categorized as enhanced BM. Furthermore, we noted a significant difference in the treatment efficacy between non-enhanced BM and enhanced BM following standardized treatment according to established guidelines. To investigate this clinical observation further, we collected medical records of 72 patients with lung cancer BM from our hospital, spanning from July 2016 to October 2022. We compared the MR imaging characteristics of non-enhanced BM across different patients and time points to evaluate clinical treatment outcomes, aiming to provide valuable insights for clinicians in selecting optimal treatment strategies.
Follow-up MR imaging characteristics of non-enhanced BM during treatment. Patient 1, Female, 57-year-old, invasive adenocarcinoma of left inferior lobe of lung. The patient underwent chemotherapy, targeted therapy, immunotherapy, radiotherapy and other comprehensive treatment. The figure shows axial enhanced T1-weighted MR image of left frontal lobe brain metastases. Patient 2, Male, 69-year-old, adenocarcinoma of left inferior lobe of lung. He was treated with chemotherapy, targeted therapy, radiotherapy and other comprehensive treatment. The figure shows the axial T2-weighted and enhanced T1-weighted MR image of the left cerebellar metastatic tumor. Patient 3, Female, 59-year-old, adenocarcinoma of right lung. She was treated with chemotherapy, immunotherapy, radiotherapy and other comprehensive treatment. The figure shows axial T2-weighted and enhanced T1-weighted MR images of the right parietal lobe metastasis. Patient 4, Male, 47-year-old, adenocarcinoma of upper lobe of left lung. He was treated with chemotherapy, radiotherapy and targeted therapy and other comprehensive treatment. The figure shows the axial T2-weighted and T1-weighted MRI images of right frontal lobe metastases. Note The follow-up time was marked in the upper right corner (Month), the MR scan sequence was marked in the lower left corner, and the red arrow showed the metastatic focus.
Materials and methods
Patient selection
The study was conducted in accordance with the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of Xiangyang NO.1 People’s Hospital, Hubei University of Medicine, Xiangyang, Hubei, China (Approval #XYYYE20230133). This article is based on the Observational Study Report following the STROBE guidelines14. Informed consent was obtained from each patient prior to examination. Between July 2016 and October 2022, a retrospective analysis was performed on 72 patients with lung cancer BM in our hospital. Based on their comprehensive clinical and radiological information, and the availability of treatment and follow-up data, head enhanced-MRI images were used as research subjects. The inclusion criteria were as follows: (1) a definitive pathological diagnosis of lung cancer; (2) the presence of brain parenchymal metastases without meningeal involvement; (3) enhanced MRI images showing non-enhanced metastases; and (4) patients receiving standardized treatment in accordance with the ASCO - SNO - ASTRO guidelines for brain metastases15. The exclusion criteria were: (1) patients with a history of brain tumors or neurological symptoms; (2) patients lacking enhanced MRI scans and follow-up examinations after treatment; (3) patients with severe cranial diseases, such as brain herniation or edema, or other serious systemic illnesses; and (4) MRI images exhibiting significant artifacts. Ultimately, the study included brain metastases from 8 patients (5 males and 3 females; age range: 33–73 years; mean age: 58 years).
MRI imaging techniques
The integrated head and neck coil of the Toshiba 1.5T MRI scanning system was utilized in this study. The imaging sequences employed were as follows: T1-weighted inversion recovery (T1WI-IR; repetition time (TR) 1950 ms, echo time (TE) 15 ms), T2-weighted imaging (T2WI; TR 4100 ms, TE 105 ms), fluid-attenuated inversion recovery (FLAIR; TR 9000 ms, TE 100 ms), diffusion-weighted imaging (DWI; b-value = 1000, TR 4000 ms, TE 100 ms), and enhancement imaging using an intravenous injection of gadolinium meglumine (Beijing Beilu Pharmaceutical Co., Ltd.; specification: 10 mL containing 4.69 g). The total dosage administered was 0.2 mmol/kg, with a flow rate of 2 mL/s, followed by a T1WI sequence (TR 1950 ms, TE 15 ms).
Image evaluation
Non-enhanced BM were defined as lesions that either lack enhancement or exhibit marginal mild enhancement. The non-enhanced components displayed low signal intensity on T1-WI images, high signal intensity on T2-WI images and no enhancement. In contrast, BM that exhibited varying degrees of enhancement were classified as enhanced BM. Imaging evaluations of metastatic tumors were carried out independently by two experienced physicians, each possessing 8 to 15 years of experience, categorizing the tumors as either non-enhanced or enhanced BM. In cases of disagreement, consultation with a senior physician was sought to reach a consensus. Enhanced MRI scans were conducted 1 month or after 2 cycles of initial treatment, and subsequently every two months or after 2–4 cycles for lesions that remained stable.
Endpoints and Response Assessment
The Response Assessment in Neuro-Oncology for Brain Metastases (RANO-BM) criteria represent the gold standard for evaluating treatment responses in brain metastases (RANO 2.0)16,17. These criteria encompass complete remission (CR), partial remission (PR), stable disease (SD), and progressive disease (PD). The overall response rate (ORR) is defined as the total of CR and PR, while the disease control rate (DCR) is calculated as the sum of the objective response rate and stable disease rate (CR + PR + SD). Our objective is to dynamically monitor the treatment response of non-enhanced lung cancer BM through MRI findings, thereby assessing their clinical efficacy.
Statistical analysis
Data analysis was conducted using SPSS version 22.0. Continuous variables were expressed as means and standard deviations (SD), whereas medians were presented as ranges. Categorical variables were summarized using frequencies. We processed the images using Adobe Illustrator CC 2019 and GraphPad Prism 8.0.
Results
Patient clinical characteristics
We conducted a study involving 72 patients with lung cancer BM, of whom 47 (65.2%) were male, with a mean age of 58 years. Among the patients, 43 (59.7%) had a history of smoking. Of the 72 cases, 11 exhibited non-enhanced BM, while the remaining 61 cases presented enhanced lesions. Among the 11 patients with non-enhanced BM, 6 had a solitary lesion prior to standard treatment. One patient died after a follow-up of 2 months, and another opted to discontinue treatment after 3 months. Of the 5 patients with multiple lesions, 4 had both enhanced and non-enhanced BM, while 1 showed no enhancement in any of the metastases and was subsequently excluded from the study. Ultimately, 8 patients with non-enhanced BM were included in our cohort, yielding a male-to-female ratio of 5:3 and an average age of 57.9 years (± 13.5, range 33–73 years) (see Tables 1 and Supplement Fig. 1). Among these patients, there were 4 cases of non-enhanced or mildly circularly-enhanced metastases (Fig. 1) and 4 cases exhibiting both enhanced and non-enhanced metastases (Fig. 2). The median follow-up duration for non-enhanced metastasis progression was 19 months, with a lesion control rate of 50%. In contrast, the median duration of progression-free follow-up was 35.5 months, and the control rate for enhanced metastases was 100%.
Comparison of follow-up MR characteristics between non-enhanced and enhanced BM during treatment. Patient 5, Male, 73-year-old, adenocarcinoma of the upper lobe of right lung. The patient was treated with chemotherapy, radiotherapy and targeted therapy according to clinical guidelines. The figure shows axial T2-weighted and T1-weighted enhanced MRI images of left frontal lobe (Foci 1) enhanced and left parietal lobe (Foci 2) non-enhanced metastatic tumors. Patient 6, Female, 54-year-old, adenocarcinoma of the inferior lobe of left lung. The patient was treated with chemotherapy, radiotherapy, targeted therapy and other comprehensive treatment. The figure shows axial enhanced T1-weighted MR images of left frontal lobe (Foci 1) enhanced and left thalamus (Foci 2) non-enhanced metastatic tumors. Patient 7, Male, 33-year-old, adenocarcinoma of the right inferior lung lobe. The patient was treated with chemotherapy, radiotherapy, targeted therapy, immunotherapy and other comprehensive treatment. The figure shows axial enhanced T1-weighted MR images of left temporal lobe (Foci 1) enhanced and brain stem (Foci 2) non-enhanced metastatic tumors. Patient 8, Male, 71-year-old, adenocarcinoma of the inferior lobe of the left lung. He was treated with chemotherapy, radiotherapy, targeted therapy, immunotherapy and other comprehensive treatment. The figure shows axial enhanced T1-weighted MR images of left temporal lobe (Foci 1) enhanced and right occipital lobe (Foci 2) non-enhanced metastatic tumors. Note The follow-up time was marked in the upper right corner (Month), the MR scan sequence was marked in the lower left corner, and the yellow arrow shows the Foci 1 metastasis and the red arrow shows the Foci 2 metastasis.
Longitudinal assessment of Non-enhanced Lung Cancer Brain metastases
In Cases 1–4, T1-weighted enhanced MRI images revealed lung cancer BM exhibiting either no enhancement or mild circular enhancement (Fig. 1). All four patients demonstrated a progressive increase in metastatic foci of over 60% within approximately one year, indicative of disease progression, with a disease control rate of 25%. In Case 1, a solitary metastasis in the left frontal lobe progressively expanded over 11 months. Following a modification of the treatment plan in accordance with clinical guidelines, this metastasis exhibited enhancement and was significantly reduced (partially relieved) 4 months later, suggesting effective treatment. In Cases 2–4, the brain metastases were localized in the left cerebellum, right parietal lobe, and right frontal lobe, respectively. Cases 2 and 3 showed no enhancement, while Case 4 presented with circular enhancement and no central enhancement, indicating a poor therapeutic effect associated with non-enhancement or circular enhancement (see Supplement Fig. 2A and B).
Comparative assessment of Non-enhanced and enhanced Lung Cancer Brain metastases
Figure 2 showed 4 cases of lung cancer BM and each case showed two lesions (Foci 1/2), with a total of 8 lesions. MR T1-WI enhanced scan showed enhanced type (upper panel, Foci 1) and non-enhanced type (bottom panel, Foci 2). The lesions were distributed in temporal lobe, frontal lobe, parietal lobe, thalamus and brain stem in 4 patients. In case 5–8, the foci 1 referred to enhanced BM. The lesions significantly reduced after 1–3 months treatment. During 1–3 years of follow-up, the lesions showed complete remission (Patient 7–8, Foci 1), partial remission (Patient 5, Foci 1), and maintained stable (Patient 6, Foci 1). The disease control rate was 100% (4 /4). The foci 2 of case 5 was a non-enhanced BM and it began to increase by more than 50% (disease progression) in about one year, which was almost consistent with the cases showed in Fig. 1. The foci 2 in case 6 initially originated in the left thalamus and showed obvious enhancement. After treatment, at the 5th month, it was found that the lesion significantly reduced, but the enhancement mode changed to non-enhancement type. At the 13th month, the non-enhancement lesion became enlarged, which was almost similar to the progression time of the non-enhancement lesion in cases 1–5. Then the lesion showed circular enhancement at the 18th month, and were followed up for 27 months, and the lesion was partially relieved (Patient 6, Foci 2). The foci 2 in case 7–8 was non-enhanced lesion, and the lesion disappeared at about 1 year during the follow-up, at 9 and 13 months respectively, which was evaluated as complete remission, and which seemed to be inconsistent with the outcome of patients with non-enhanced metastasis in cases 1–6. In fact, a careful analysis revealed that the duration of lesion shrinkage to disappearance of the non-enhanced lesions were significantly longer (11 M vs. 2 M) than that of their own enhanced lesions (Patient 7–8, Foci 1).
In case 5–8, a comparative study of non-enhanced lesions (Foci 2) and self-enhanced lesions (Foci 1) showed that the treatment response of non-enhanced lesions was significantly weaker than that of enhanced lesions (Patient 7–8), and even showed lesion progression (Patient 5) without treatment response, and the disease control rate was 87.5%.
We performed K-M curve analysis on 12 lesions of 8 patients according to the types of enhancement and non-enhancement, and the results were statistically significant, and the progression-free survival of the enhanced lesions was longer than that of the non-enhanced lesions. However, the results were not statistically significant when analyzed by overall patient survival. In addition, lymph node metastasis and stratified analysis of different treatment regimens were not statistically significant (Supplement Fig. 2).
Discussion
Brain is a common site of metastasis in advanced lung cancer. Contrast-enhanced MRI is a preferred method for diagnosing BM. Traditionally, clinicians have emphasized the significance of the presence and number of metastases in informing treatment plans, often overlooking the impact of enhancement patterns on therapeutic regimens. Metastatic tumors exhibit heterogeneity, and even brain metastatic lesions of the same histological type may harbor genetic mutations, leading to diverse MRI appearances. Brain metastases can show low, equal or high signal intensity on T1- and T2 -WI images. Sometimes, very thin-walled cystic metastases do not enhance or only slightly enhance13. In this study, we observed that non-enhanced BM can occur as either singular or multiple lesions, and may coexist with enhanced brain metastases, presenting with irregular intracranial distribution.
Non-enhanced BM typically shows long T1 and T2 signal characteristics, with unrestricted diffusion resembling that of high-tension capsules. Cystic brain metastases may represent a specific subtype of non-enhanced BM, although the nature of their internal cystic components remains undetermined9,10. Low signal intensity on T1-WI and high signal intensity on T2-WI images suggest a high water content in the tumor tissue, while unrestricted diffusion implies looser tissue composition. Therefore, we hypothesize that non-enhanced BM may consist of loose tissues with significant mucous components. The observed lack of enhancement could be attributed to insufficient blood supply, thereby hindering the infiltration of contrast agents. Cumsing et al. proposed that cystic fluid in BM arises from adjacent blood vessel leakage following tumor deterioration18. Conversely, Gardner et al. suggested that cystic components in metastatic tumors result from a lack of lymphatic drainage in the brain, culminating in tissue fluid accumulation19. Leaky fluid generally exhibits low signal intensity on FLAIR sequences, which is not exactly consistent with the non-enhanced BM in this study. Cystic BM are more common in mucinous adenocarcinoma, indicating that the cyst may be mucous components secreted by the tumor20, and the inside components of the brain metastases may be mucous containing cancer cells. Some tumor tissues have poor histological grade and rapid growth, resulting in poor blood supply in the center. Due to insufficient blood supply, tumor tissues undergo necrosis and cystic transformation. When the tumor has only a thin wall, cystic metastases are formed21. Non-enhanced BM may share the same formation process.
Our study indicates that the short-term treatment efficacy of enhanced BM is superior to that of non-enhanced BM. Specifically, in patients presenting with both enhanced and non-enhanced BM, enhanced lesions exhibited markedly better short-term therapeutic responses, while non-enhanced BM demonstrated suboptimal or significantly weaker therapeutic effects. For instance, in cases 7 and 8, the rate of volume reduction for non-enhanced metastases was notably slower compared to the enhanced metastases. This discrepancy may be attributed to the slower absorption of cystic components relative to solid tumors, partially explaining the observed differences in volume reduction rates12.
There is a certain correlation between the poor chemotherapy efficacy and the non-enhancement MRI manifestations7,8. The principle of MRI enhancement relies on gadolinium diffusion from capillaries into tissue space, resulting in shortened T1 time of the tissue and enhanced contrast between of the tissue tissues. The absence of enhancement in metastatic tumors implies that the contrast medium injected into the systemic circulation cannot infiltrate tumor tissue effectively. Similarly, during chemotherapy, the inability of intravenous or orally administered chemotherapeutic agents to penetrate tumor tissue results in low intratumoral drug concentrations, leading to inferior treatment outcomes compared to enhanced BM7,8.
Systemic therapy represents a crucial pillar of multimodal treatment approaches for BM. Numerous preclinical and clinical studies indicate that the blood-tumor barrier can limit drug penetration, leading to heterogeneous drug distribution within tumors due to deviations in the characteristics of tumor-associated blood vessels from physiological state. A more comprehensive understanding of the blood-tumor barrier’s role is essential in formulating effective systemic treatment regimens for BM patients22. Failure to adequately address tumor metastases may result in serious complications, including acute hydrocephalus, brainstem compression, cerebellar tonsillar herniation, and coma23.
The blood-brain barrier (BBB) is a pivotal topic concerning enhancement effects and chemotherapy in brain tumors. This unique structure within normal brain tissue selectively permits certain molecules to cross from intracranial capillaries. The gadolinium meglumine utilized in MR-enhanced scans does not pass through the BBB and thus lacks enhancement effects on brain tissue exhibiting well-preserved BBB function. Brain metastases disrupt the integrity of the BBB during invasion6, resulting in a blood-tumor barrier that functions similarly to the BBB, inhibiting the infiltration of large intravascular molecules into the extravascular space. This barrier may contribute to the observed lack of enhancement in brain metastases and their poor therapeutic responses. It not only obstructs the exosmosis of gadolinium but also limits the extravasation of chemotherapeutic agents. The permeability of this barrier can be inversely inferred from the degree of MRI enhancement, and the obvious enhancement indicates the poor selectivity and strong permeability of this barrier. The non-enhancement shows that the screen has strong selectivity to the passing molecules and poor permeability6.
Sometimes, we found that the enhanced and non-enhanced lung cancer BM could be transformed into each other during the follow-up. For instance, the metastatic lesion of Patient 1 changed from non-enhanced type to enhanced type (Fig. 1) during the treatment, and the size decreased with the treatment. However, for the Patient 6, the metastatic lesion changed from enhanced type to non-enhanced type, and tended to increase during follow-up. After standardized treatment, the lesion changed to enhanced type again, and tended to be stable and then partially relieved after follow-up. The mechanisms underlying these transformations remain unclear but may be linked to the dynamics of the blood-tumor barrier6. Notably, MRI enhancement patterns during follow-up examinations may provide critical insights for clinicians to dynamically adjust the treatment plan.
There are some limitations in this study. First of all, due to the particularity of the brain, the puncture injury of brain metastases is often greater than the benefit. In this study, the diagnosis of metastatic tumors is a clinical diagnosis, and there is no definite pathological evidence. The pathological structure and mechanism of non-enhanced brain metastases can only be speculated by existing experience and related studies, and further research needs to be proved by pathological sections, immunohistochemistry and animal experiments. Secondly, there is no detailed analysis on the comprehensive treatment of lung cancer and brain metastases. Third, this study is a single-center study, with a small sample size and a small number of cases of non-enhanced metastatic tumors, so a more accurate study requires a multi-center and large sample study. The current findings have yet to be confirmed in a larger population.
Our comparative analysis of cases meeting the inclusion criteria revealed that most non-enhanced metastases gradually increased in about 1 year, which may be related to the slow proliferation of tumors due to the effect of blood tumor barrier or the lack of abundant blood supply for nutrition. Under the same treatment regimen, the non-enhanced metastases could not reach the effective drug concentration in the lesion area in a short time due to the blood tumor barrier, so that the non-enhanced metastases showed an inert response, and it took a longer time to shrink the lesion than the self-enhanced type (Fig. 2, Patient 6–7, Foci 2). In conclusion, the therapeutic efficacy of non-enhanced lung cancer BM is inferior to that of enhanced BM, likely due to insufficient blood supply and low local drug concentrations. Evaluating enhancement profiles of BM via contrast-enhanced MR scans holds significant implications for clinicians in optimizing treatment plans, particularly in dynamically adjusting therapies during follow-up.
Conclusion
This study demonstrates that the therapeutic effect of non-enhanced metastatic lesions is significantly inferior to that of enhanced metastatic lesions when standardized treatment is administered according to clinical guidelines. The degree of MRI enhancement in lung cancer BM serves as an effective imaging biomarker for predicting treatment outcomes. Furthermore, non-enhanced metastases may be identified as an independent prognostic factor. Assessing the enhancement degree of lung cancer BM is valuable for predicting treatment efficacy and guiding the management of lung cancer BM.
Data availability
The clinical data supporting the conclusions of this manuscript will be made available by the corresponding author on reasonable request.
References
Kotecha, R. et al. Recent advances in managing brain metastasis. F1000Res. 2018, 7 (2018).
Page, S. et al. Systemic treatment of brain metastases in non-small cell lung cancer. Eur. J. Cancer. 132, 187–198 (2020).
Essig, M. et al. Perfusion MRI: the five most frequently asked clinical questions. AJR Am. J. Roentgenol. 201 (3), W495–510 (2013).
Eichler, A. F. et al. The biology of brain metastases-translation to new therapies . Nat. Rev. Clin. Oncol. 8 (6), 344–356 (2011).
Azenha, L. F. et al. Role of pre-operative brain imaging in patients with NSCLC Stage I: A retrospective. Multicenter Anal. Cancers (Basel) 14 (10), 2419 (2022).
Ye, L. Y. et al. The structure of blood-tumor barrier and distribution of chemotherapeutic drugs in non-small cell lung cancer brain metastases. Cancer Cell. Int. 21 (1), 556 (2021).
Arvanitis, C. D., Ferraro, G. B. & Jain, R. K. The blood-brain barrier and blood-tumour barrier in brain tumours and metastases. Nat. Rev. Cancer. 20 (1), 26–41 (2020).
Sorensen, A. G. et al. A vascular normalization index as potential mechanistic biomarker to predict survival after a single dose of cediranib in recurrent glioblastoma patients. Cancer Res. 69 (13), 5296–5300 (2009).
Xu, Y. B. et al. Treatment and prognosis of solid and cystic brain metastases in patients with non-small-cell lung Cancer. Cancer Manag. Res. 13, 6309–6317 (2021).
Sun, B. et al. Cystic brain metastasis is associated with poor prognosis in patients with advanced breast cancer. Oncotarget 7 (45), 74006–74014 (2016).
Uchino, M. et al. Radiosurgery for cystic metastatic brain tumor. No Shinkei Geka. 28 (5), 417–421 (2000).
Wang, H. et al. Cystic brain metastases had slower speed of tumor shrinkage but similar prognosis compared with solid tumors that underwent radiosurgery treatment. Cancer Manag. Res. 11, 1753–1763 (2019).
Tadros, S. & Ray-Chaudhury, A. Pathological features of Brain metastases. Neurosurg. Clin. N Am. 31 (4), 549–564 (2020).
von Elm, E. et al. The strengthening the reporting of Observational studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 12 (12), 1495–1499 (2014).
Vogelbaum, M. A. et al. Treatment for Brain metastases: ASCO- SNO-ASTRO Guideline. J. Clin. Oncol. 40 (5), 492–516 (2022).
Ocana-Tienda, B. et al. Volumetric analysis: Rethinking brain metastases response assessment. Neurooncol Adv. 6 (1), d161 (2024).
Wen, P. Y. et al. RANO 2.0: Update to the response assessment in neuro-oncology criteria for high- and low-grade gliomas in adults . J. Clin. Oncol. 41 (33), 5187–5199 (2023).
Cumings, J. N. The chemistry of cerebral cysts . Brain 73 (2), 244–250 (1950).
GARDNER W J, COLLIS J J, LEWIS, L. A. Cystic brain tumors and the blood-brain barrier. Comparison of protein fractions in cyst fluids and sera . Arch. Neurol. 8, 291–298 (1963).
Hayashi, H. et al. Cystic brain metastasis in non-small-cell lung cancer with ALK rearrangement. J. Clin. Oncol. 32 (36), e122–4 (2014).
Wang, J. et al. Correlation analysis between retention of Gd-DTPA in the cystic area of brain metastasis and MRI signs. J. Oncol. 2022, 2738892. (2022).
Berghoff, A. S. & Preusser, M. Role of the blood-brain barrier in metastatic disease of the central nervous system . Handb. Clin. Neurol. 149, 57–66 (2018).
Ramazanoglu, A. F. et al. Peritumoural Oedema as a predictor of overall survival for patients with posterior Fossa metastases . J. Coll. Physicians Surg. Pak. 33 (2), 136–140 (2023).
Acknowledgements
We would like to thank the patients who participated in this study and the staff from the Departments of radiology, pathology and oncology for their contributions to this study.
Funding
This study was supported by Faculty Development Grants of Xiangyang No.1 People’s Hospital Affiliated to Hubei University of Medicine (Grants number: XYY2023D02) and Innovative Research Program of Xiangyang No.1 People’s Hospital (Grants number: XYY2023QT01).
Author information
Authors and Affiliations
Contributions
All authors attest that they meet the current International Committee of Medical Journal Editors (ICMJE) criteria for Authorship. All the authors had fully participated to the study and approved the final draft.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, X., Yang, J., Hu, H. et al. Longitudinal MRI evaluation of the efficacy of non-enhanced lung cancer brain metastases. Sci Rep 15, 3318 (2025). https://doi.org/10.1038/s41598-025-87422-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-87422-9