Abstract
Ventral hernias pose a prevalent challenge in abdominal wall surgery, with ongoing advancements in repair techniques designed to enhance patient outcomes. This study evaluates the efficacy, safety, and socio-economic impact of Totally Extraperitoneal Sublay Repair (TES) versus Laparoscopic Intraperitoneal Onlay Mesh Repair (IPOM) for small to medium-sized ventral hernias, with a particular focus on postoperative quality of life and patient satisfaction. A retrospective cohort study was conducted, encompassing 125 patients who underwent ventral hernia repair between May 2018 and November 2023. The cohort included 55 patients treated with TES and 70 with Laparoscopic IPOM. Baseline characteristics, including age, gender, BMI, operative time, postoperative pain, hospitalization costs, and patient satisfaction score, were compared. Postoperative quality of life was evaluated through outpatient visits or telephone follow-ups. The propensity score matching (PSM) technique was applied in a 1:1 ratio to balance the significant differences in general characteristics between the two groups. Out of 125 patients, 70 cases were successfully matched using the PSM method, resulting in 35 cases in each group. The baseline characteristics of patients in groups were well-matched (P > 0.05). The TES group exhibited a significantly longer operative duration (P < 0.001); however, this group also experienced markedly reduced postoperative pain, decreased hospitalization costs, and diminished postoperative drainage (all P < 0.001). The length of hospital stay and the incidence of long-term complications were similar between the two groups. Follow-up evaluations at 3 and 6 months showed a significantly improved quality of life and higher patient satisfaction in the TES group. Both TES and IPOM demonstrate comparable safety and efficacy in the repair of ventral hernias. Although TES is associated with a longer operative duration, it provides significant advantages in postoperative quality of life, patient satisfaction, and cost-effectiveness, thereby supporting its broader clinical adoption.
Similar content being viewed by others
Introduction
Ventral hernias are a prevalent surgical challenge1, characterized by the protrusion of intra-abdominal contents through a defect in the abdominal wall. They can lead to significant morbidity if left untreated, with patients often experiencing pain, discomfort, and impaired quality of life. The increasing incidence of ventral hernias has prompted the development and refinement of various surgical techniques aimed at improving patient outcomes and minimizing complications.
Traditionally, open repair methods were widely used; however, the advent of minimally invasive techniques, such as Laparoscopic Intraperitoneal Onlay Mesh (IPOM) repair, has shifted the paradigm in hernia surgery2. Minimally invasive approach is considered a safe and effective method for Ventral hernias3,4. IPOM has gained popularity due to its reduced postoperative pain and shorter recovery time. Nonetheless, concerns remain regarding the potential for intraperitoneal adhesions and complications related to mesh placement within the peritoneal cavity. Recent research shows patients who have undergone incisional hernia repair using IPOM face a heightened risk of bowel obstruction compared to those with a similar surgical history yet without incisional hernia repair (IHR)5. Study evaluating the use of meshes in animal models reveal that they can cause adhesions in the intraperitoneal ___location, even when composite meshes are employed6. The Totally Extraperitoneal Sublay Repair (TES) technique has emerged as an alternative approach, offering the theoretical advantage of placing the mesh in the extraperitoneal space, thereby reducing the risk of intraperitoneal complications. TES, however, is associated with a longer operative duration, raising questions about its overall efficiency compared to IPOM.
This study aims to objectively compare the efficacy, safety, and socio-economic impact of TES and IPOM in the repair of small to medium-sized ventral hernias. Specifically, it focuses on assessing postoperative quality of life and patient satisfaction, two critical metrics that directly influence the long-term success of hernia repair procedures7. By analyzing these outcomes, this study seeks to provide evidence-based insights that may guide surgeons in selecting the most appropriate technique for their patients.The importance of this research lies in its potential to inform clinical decision-making, optimize patient outcomes, and contribute to the ongoing evolution of ventral hernia repair methodologies. As the field continues to advance, understanding the comparative benefits and limitations of TES and IPOM is essential for enhancing patient care and improving surgical practice.
Patients and methods
Study population
This retrospective cohort study was conducted at Shaoxing Central Hospital, involving patients who underwent ventral hernia repair. Ventral hernias encompass all hernias occurring in the anterior abdominal wall, including epigastric, umbilical, and linea alba hernias. The sample size of 125 patients was determined based on the availability of eligible cases from May 2018 to November 2023. The study included all patients meeting the inclusion criteria to minimize selection bias and ensure representative analysis. Patients were divided into two groups based on the surgical technique employed: Totally Extraperitoneal Sublay Repair (TES) and Laparoscopic Intraperitoneal Onlay Mesh (IPOM) repair. The TES group consisted of 55 patients, while the IPOM group comprised 70 patients. Patients included in the study were those diagnosed with small to medium-sized ventral hernias primarily included cases of epigastric and umbilical hernias, defined as defects with ventral hernias ≤ 7 cm8.The diameter of the hernia defect was primarily measured using preoperative imaging, with a preference for CT scans, which provided the most accurate and consistent measurements. In some cases, ultrasound was also used to measure smaller defects. Exclusion criteria included patients with large hernias (greater than 7 cm), recurrent hernias, severe obesity or previous extensive abdominal surgeries, or those with significant comorbidities that could impact surgical outcomes. The HERQules tool was used for evaluating the patients’ postoperative QoL. It was applied during outpatient visits at 1 month, 3 months, and 6 months following surgery to track improvements in QoL.
Key technical points
Several key technical considerations were observed during both TES and IPOM procedures to optimize surgical outcomes. For TES, the careful dissection of the preperitoneal space was crucial to minimize the risk of injury to surrounding structures, such as the bladder and epigastric vessels. Ensuring adequate overlap of the mesh was essential to reduce the likelihood of hernia recurrence. The choice between tacks and sutures for mesh fixation in TES was based on surgeon preference and patient-specific factors, with the primary goal being secure mesh placement without excessive tension.
In the IPOM procedure, special attention was paid to the positioning of the mesh within the peritoneal cavity to prevent migration or folding, which could lead to recurrence or other complications. The use of composite mesh, with one side designed to minimize adhesions, was critical in reducing the risk of intraperitoneal complications. Transfascial sutures provided additional security for mesh fixation, particularly in larger defects or in patients with higher intra-abdominal pressure.
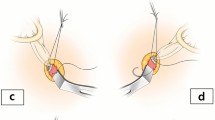
The IOPM procedure has been thoroughly detailed in previous literature9,10, while the surgical process of TES is demonstrated in the supplementary video materials. An example of an umbilical hernia can be seen in video and Fig. 1 .
Postoperative care, follow-up, and data collection
All patients received standardized postoperative care, which included pain management, early mobilization, and discharge planning based on recovery progress. Postoperative pain was assessed using the Visual Analog Scale (VAS), and patients were monitored for complications such as seroma, infection, or mesh-related issues. Follow-up assessments were conducted at 3 and 6 months post-surgery through either outpatient visits or telephone interviews. These assessments focused on evaluating the patients’ quality of life, satisfaction with the surgical outcome, and any long-term complications, such as recurrence or chronic pain.
Baseline characteristics were assessed for all patients included in the study. These characteristics included age, gender, body mass index (BMI), preoperative pain levels, and other relevant factors that could impact postoperative outcomes. The two groups, TES and IPOM, were compared for these characteristics to ensure their comparability at the time of inclusion.
Data collection encompassed operation time, postoperative complications, recovery status, quality of life (assessed using the Hernia-Related Quality of Life Survey), and patient satisfaction questionnaires. Long-term outcomes were primarily concerned with recurrence rates and chronic complications. The HerQLes questionnaire, designed to evaluate the impact of hernia surgery on quality of life, assessed pain, daily activity, psychological state, socioeconomic burden, and overall quality of life. Scores for each item ranged from 1 to 5, with higher scores indicating greater issues and a reduced quality of life. The patient satisfaction questionnaire evaluated pain management, the recovery process, medical services, and overall satisfaction, also using a 1 to 5 point scale, with higher scores reflecting greater satisfaction.
Statistical analysis
To compare the outcomes between the TES and IPOM groups with similar general characteristics, propensity score matching (PSM) was employed to to minimize confounding between the two groups. PSM estimates the likelihood of group assignment based on baseline variables (e.g., age, BMI, gender) and matches participants with similar scores, ensuring comparability between groups. After matching, statistical tests were selected based on data characteristics. Student’s t-test is used to compare the means of continuous variables (such as age and BMI) between two groups when the data are normally distributed. Mann-Whitney U test is used to compare continuous variables between two groups when the data are not normally distributed. Chi-square test or Fisher’s exact test are used to compare categorical variables (such as gender) between two groups. Fisher’s exact test is typically used when the sample size is small or the expected frequencies are low. A P-value of less than 0.05 was considered statistically significant. All analyses were performed using SPSS software (version 26.0; IBM Corp., Armonk, NY, USA), ensuring robust and reliable results. This comprehensive methodology accounted for baseline differences and ensured valid comparisons of outcomes between the TES and IPOM groups.
Results
As presented in Table 1, significant differences were observed between the two groups in terms of the longest diameter of defect and BMI (all P < 0.05). However, after 1:1 PSM, the general characteristics became comparable between the TES and IPOM groups. The TES group had a longer operative time but lower costs, less postoperative pain, reduced drainage volume, a lower complication rate, and significantly better quality of life improvements compared to the IPOM group.
The operative and perioperative parameters of the TES and IPOM groups are summarized in Table 2. The mean operative time was significantly longer in the TES group (204.45 ± 37.35 min) compared to the IPOM group (167.68 ± 35.96 min, P < 0.001), as shown in Fig. 2a. The TES group demonstrated significantly lower medical expenses (1.51 ± 0.25 × 10,000 RMB) than the IPOM group (2.85 ± 0.45 × 10,000 RMB, P < 0.001, Fig. 2b). The TES group experienced significantly less postoperative pain than the IPOM group on Day 1 (3.22 ± 0.98 vs. 4.35 ± 1.12, P < 0.001) and Day 2 (2.65 ± 0.82 vs. 3.55 ± 0.94, P < 0.001), as shown in Fig. 2c and d. The TES group had lower drainage volumes (136.54 ± 55.68 ml) compared to the IPOM group (208.58 ± 78.86 ml, P < 0.001, Fig. 2e). The TES group had a lower complication rate (14.3%, 5/35) than the IPOM group (34.3%, 12/35), but the difference was not statistically significant (P = 0.051, Fig. 2f). Among complications, the IPOM group exhibited higher rates of symptomatic seroma (2 vs. 1 case), postoperative ileus (5 vs. 1 case), and chronic pain (5 vs. 2 cases). Chronic pain was defined as pain for more days than not over the last three months post-surgery11. Postoperative ileus was characterized by symptoms such as abdominal pain, vomiting, and abdominal distension occurring within two weeks after surgery. Diagnosis was confirmed through abdominal imaging, with mechanical causes like intestinal torsion and other factors such as hypokalemia and tumor metastasis being excluded.
The quality of life (QOL) outcomes, assessed using the HerQLes questionnaire, are presented in Table 3. Key differences between the TES and IPOM groups over time are highlighted. The TES group reported significantly lower pain scores at 30 days (3.35 ± 0.49 vs. 3.75 ± 0.63, P = 0.004) and 60 days (3.04 ± 0.65 vs. 3.33 ± 0.51, P = 0.042), with no significant difference at 180 days (P = 0.755, Fig. 3a). The TES group showed less movement limitation at 30 days (2.75 ± 0.41 vs. 3.05 ± 0.59, P = 0.016), with differences diminishing at 60 days (P = 0.665) and 180 days (P = 0.168, Fig. 3b). Differences in psychological state were significant at 30 days (2.54 ± 0.41 vs. 2.75 ± 0.46, P = 0.048) but not at 60 (P = 0.108) or 180 days (P = 0.077, Fig. 3c). The TES group demonstrated better daily activity scores at 30 days (3.10 ± 0.55 vs. 3.40 ± 0.65, P = 0.041) and 60 days (2.86 ± 0.46 vs. 3.09 ± 0.48, P = 0.045), with no significant difference at 180 days (P = 0.233, Fig. 3d). Overall Quality of Life: The TES group performed better at 180 days (2.48 ± 0.44 vs. 2.71 ± 0.45, P = 0.034), despite no significant differences at earlier timepoints (30 days P = 0.211, 60 days P = 0.512, Fig. 3e).
Follow-ups were conducted monthly via outpatient visits or telephone for the first six months, and then every three to six months thereafter. No recurrences were observed in any patients by the final follow-up. Satisfaction scores also indicated that patients in the TES group experienced better pain management and reported higher overall satisfaction postoperatively compared to the IPOM group, as shown in Table 4.
Discussion
The management of ventral hernias remains a critical focus in abdominal surgery due to the high incidence of associated postoperative complications and the imperative for repair strategies that ensure long-term recurrence prevention12. A study revealed that the prevalence of abdominal wall hernias in the general Russian population was 20.9%13. The rising prevalence of ventral hernias, alongside advancements in surgical techniques, necessitates a comprehensive understanding of the available surgical approaches14. Ventral hernia repair has evolved significantly over the past few decades. Traditional open repair methods, while effective, are associated with high complication morbidity, including increased pain, longer recovery periods, and higher recurrence rates. The advent of minimally invasive techniques such as IPOM has shifted the paradigm, offering reduced postoperative pain, shorter hospital stays, and quicker return to normal activities15,16. However, IPOM is not without its drawbacks, particularly concerning the risk of intraperitoneal adhesions, mesh-related complications, and chronic pain17. A 2022 systematic review concluded that the incidence of bowel obstruction in IPOM was higher than Sublay18. Spiral tacks used for intraperitoneal mesh fixation is the leading cause of adhesions and bowel lesions19. TES, an alternative to IPOM, places the mesh in the extraperitoneal space, theoretically reducing the risk of intraperitoneal complications while potentially enhancing patient outcomes. The primary objective of this study was to evaluate and compare the efficacy, safety, postoperative quality of life, patient satisfaction, and socio-economic impact of TES and IPOM in the repair of small-to-medium ventral hernias. By analyzing these outcomes, the study sought to provide evidence-based insights that could guide surgeons in selecting the most appropriate technique for their patients, ultimately improving clinical decision-making.
Ventral hernias, if left untreated or improperly managed, can lead to severe complications, including bowel obstruction, strangulation, and chronic pain, significantly impairing a patient’s quality of life. As surgical techniques continue to evolve, it is crucial to determine which methods offer the best balance between safety, efficacy, and patient-centered outcomes.This research is particularly important because it addresses the need for a clearer understanding of how these two techniques perform in real-world clinical settings. The results of this study provide valuable data on the postoperative experiences of patients, including pain management, recovery time, and overall satisfaction with the surgical outcome. These factors are critical not only for immediate postoperative recovery but also for long-term patient well-being and the prevention of hernia recurrence. Moreover, the socio-economic impact of these procedures is a significant consideration. With healthcare costs rising globally, the ability to reduce hospitalization costs, minimize postoperative complications, and enhance recovery times is increasingly important. By demonstrating that TES may offer advantages in terms of cost-effectiveness and patient satisfaction, this study contributes to the ongoing discussion about how to optimize resource allocation in healthcare settings while maintaining high standards of patient care.
The results of this study indicate that while both TES and IPOM are effective in repairing small-to-medium ventral hernias, they offer distinct advantages and drawbacks. TES, despite its longer operative duration, was associated with significantly reduced postoperative pain, lower hospitalization costs, and diminished postoperative drainage. Our result is generally consistent with the previous research results of Li et al.20 These findings suggest that TES may be a more cost-effective option, particularly for patients where postoperative pain management and cost are major concerns. In contrast, IPOM, showed a slightly higher complication rate in this study, particularly concerning postoperative ileus and chronic pain. These complications, while not statistically significant in this study, highlight the need for careful patient selection and technique refinement when opting for IPOM. The quality of life assessments further support the advantages of TES, with patients in the TES group reporting higher satisfaction scores and better overall quality of life at both 3 and 6 months postoperatively. The results of our study are similar to other reports in the literature21. This suggests that TES may provide more durable improvements in patient outcomes, potentially leading to fewer long-term complications and a lower likelihood of recurrence.
Furthermore, our analysis identified several factors that significantly influence postoperative QoL in patients undergoing ventral hernia repair. Patient-related factors such as age, body mass index (BMI), and preoperative pain levels were found to be significantly correlated with QoL outcomes. For instance, older patients or those with higher preoperative pain levels tended to report lower QoL scores after surgery. Surgical factors, including operative time and intraoperative complications, also had a substantial impact. Longer operative times and the occurrence of intraoperative complications were associated with poorer postoperative QoL. Additionally, complications during the postoperative period, including, seromas, and chronic pain, were found to negatively affect QoL. These findings underscore the importance of careful patient selection and surgical technique optimization in enhancing postoperative outcomes. Our future work will explore these factors in greater detail to better understand their contribution to QoL changes.
The findings of this study have several important clinical implications. First, it underscores the choice of surgical technique is tailored to the patient’s specific circumstances, including their health status, hernia characteristics, and personal preferences. Surgeons should consider the potential benefits of TES in terms of postoperative pain reduction and cost-effectiveness, particularly for patients who are at higher risk for chronic pain or who may benefit from a more cost-efficient approach. Second, the study underscores the importance of optimizing ventral hernia repair techniques. As minimally invasive methods continue to evolve, it is crucial to refine these techniques to minimize complications and further enhance patient outcomes. Future research should prioritize the long-term follow-up of patients who undergo TES and IPOM, with particular attention to recurrence rates, chronic pain management, and overall quality of life. Finally, this study suggests that there is still room for improvement in both TES and IPOM. For TES, reducing operative time without compromising the benefits observed in this study could enhance its appeal as a preferred technique. For IPOM, addressing the risks associated with intraperitoneal mesh placement, such as adhesions and chronic pain, will be critical for its continued use in ventral hernia repair22. Our findings align with previous studies that have demonstrated the efficacy of TES in reducing postoperative complications and improving recovery time, albeit with longer operative durations compared to IPOM23. Similarly, while IPOM has been widely adopted due to its safey24, its association with long-term mesh-related complications cannot be ignored.
This study acknowledges several limitations that warrant consideration. First of all, the limited sample size in this study constrains the generalizability and statistical power of our findings. Future research with larger cohorts is necessary to validate these results across diverse populations. Secondly, as a retrospective study, there is a potential for selection bias. However, the PSM analysis was conducted to mitigate discrepancies in general characteristics between the two groups. This adjustment allows for a more accurate comparison of the efficacy and quality of life outcomes between the two surgical approaches, minimizing the potential for confounding factors to influence the results. While this mitigates confounding factors to some extent, randomized controlled trials remain the gold standard for eliminating such biases. Furthermore, the follow-up period was inadequate for a comprehensive evaluation of long-term outcomes, including recurrence rates. This limitation underscores the need for extended follow-up in future studies to capture a more comprehensive picture of outcomes, particularly concerning different hernia types and sizes. Addressing these limitations in subsequent research will enhance the reliability of findings and provide more robust clinical guidance.
In conclusion, both TES and IPOM are effective options for small-to-medium ventral hernia repair, each with unique advantages. TES, characterized by lower postoperative pain, reduced hospitalization costs, and greater patient satisfaction, may present a more cost-effective and patient-centered option. The selection between TES and IPOM should be guided by a comprehensive assessment of the patient’s specific needs, the surgeon’s expertise, and the hernia’s particular characteristics. This study contributes valuable insights to clinical practice, emphasizing the need for individualized treatment plans. The findings support the growing preference for TES in suitable cases. Future research should focus on long-term outcomes, cost-effectiveness, and quality of life assessments in larger, more diverse patient populations. Additionally, studies exploring hybrid approaches combining both techniques could further optimize patient outcomes, offering more personalized care pathways for hernia repair.
Data availability
The authors will make the raw data supporting the conclusions of this article available without undue reservation.The data is available from the corresponding author on reasonable request. (Xiufeng Chu:[email protected] or Wei Chen: [email protected])
References
Campanile, F. C. et al. Italian laparoscopic ventral hernia Guideline Group. Laparoscopic treatment of ventral hernias: the Italian national guidelines. Updates Surg. 75(5), 1305–1336 (2023).
Lodha, M. et al. Assessment of Quality of Life after ventral hernia repair: a prospective observational study at a Tertiary Care Centre. Cureus 14(6), e26136 (2022).
Olmi, S. et al. Laparoscopic treatment of Incisional and ventral hernia. JSLS ;25(2), e202100007 (2021).
Eker, H. H. et al. Laparoscopic vs open incisional hernia repair: a randomized clinical trial. JAMA Surg. 148(3), 259–263 (2013).
Delorme, T. et al. Does intraperitoneal mesh increase the risk of bowel obstruction? A nationwide French analysis. Hernia 28(2), 419–426 (2024).
Fuziy, R. A. et al. Comparative study of four different types of intraperitoneal mesh prostheses in rats. Acta Cir. Bras. 34(7), e201900703 (2019).
Campanelli, G. Quality of life is the most important outcome measure of hernia repair. Hernia 26(3), 685 (2022).
Jensen, K. K., Helgstrand, F. & Henriksen, N. A. Short-term outcomes after laparoscopic IPOM versus robot-assisted retromuscular repair of small to medium ventral hernias: a Nationwide Database Study. Ann. Surg. 279(1), 154–159 (2024).
Slavu, I. M. et al. Laparoscopic intraperitoneal onlay mesh (IPOM) in the treatment of ventral hernias: technique discussion points. Cureus 16(5), e61199 (2024).
Wang, T. et al. Lapa comparative review of outcomes: single-incision laparoscopic total extra-peritoneal sub-lay (SIL-TES) mesh repair versus laparoscopic intraperitoneal onlay mesh (IPOM) repair for ventral hernia. Updates Surg. 74(3), 1117–1127 (2022).
Wijayabahu, A. T. et al. Associations between vitamin D, Omega 6:Omega 3 ratio, and biomarkers of aging in individuals living with and without Chronic Pain. Nutrients 14(2), 266 (2022).
Liang, M. K. et al. Ventral Hernia Management: Expert Consensus guided by systematic review. Ann. Surg. 265(1), 80–89 (2017).
Sazhin, A. et al. Prevalence and risk factors for abdominal wall hernia in the general Russian population. Hernia 23(6), 1237–1242 (2019).
Poulose, B. K. et al. Epidemiology and cost of ventral hernia repair: making the case for hernia research. Hernia 16, 179–183 (2012).
Alizai, P. H. et al. Incisional Hernia repair of medium- and large-sized defects: laparoscopic IPOM Versus Open SUBLAY technique. Acta Chir. Belg. 119(4), 231–235 (2019).
Alizai, P. H. et al. Incisional hernia repair of medium- and large- sized defects: laparoscopic IPOM versus open sublay technique. Acta Chir. Belg. 119(4), 231–235 (2019).
Bittner, R. et al. Update of guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))-Part A. Surg. Endosc. 33(10), 3069–3139 (2019).
Li, J., Wang, Y. & Wu, L. The comparison of eTEP and IPOM in ventral and Incisional Hernia Repair: a systematic review and Meta-analysis. Surg. Laparosc. Endosc. Percutan Tech. 32(2), 252–258 (2022).
Haltmeier, T. & Groebli, Y. Small bowel lesion due to spiral tacks after laparoscopic intraperitoneal onlay mesh repair for incisional hernia. Int. J. Surg. Case Rep. 4(3), 283–285 (2013).
Li, B. et al. Totally endoscopic sublay (TES) repair for lateral abdominal wall hernias: technique and first results. Hernia 25(2), 523–533 (2021).
Zhuang, B. et al. An improved approach of totally visceral sac separation (TVS) for incisional hernia compared with laparoscopic intraperitoneal onlay mesh plus repair (IPOM plus). Sci. Rep. 13(1), 18037 (2023).
Helmedag, M. J. et al. Ultra-fine polyethylene hernia meshes improve biocompatibility and reduce intraperitoneal adhesions in IPOM position in animal models. Biomedicines 10(6), 1294 (2022).
Li, B., Qin, C. & Bittner, R. Totally endoscopic sublay (TES) repair for midline ventral hernia: surgical technique and preliminary results. Surg. Endosc. 34(4), 1543–1550 (2020).
Maskal, S. M. et al. Long-term mesh-related complications from minimally invasive intraperitoneal onlay mesh for small to medium-sized ventral hernias. Surg. Endosc. 38(4), 2019–2026 (2024).
Author information
Authors and Affiliations
Contributions
This work was conceived by Miaofeng Wang and Wei Chen. Data was collected and analyzed by Xiufeng Chu. The manuscript was written by Miaofeng Wang. Wei Chen and Xiufeng Chu helped to revise manuscript and proposed constructive opinions. All authors contributed to the article and approved the submitted version. We thank the following author for their role as co-corresponding authors: Wei Chen and Xiufeng Chu , who contributed equally to the supervision and communication of this study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics Declaration
The Shaoxing Central Hospital’s Institutional Review Committee approved this study. All methods were carried out in accordance with relevant guidelines and regulations. All experimental protocols were approved by The Shaoxing Central Hospital’s Institutional Review Committee. Informed consent was obtained from all patients.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, M., Chen, W. & Chu, X. Comparative analysis of efficacy and quality of life between totally extraperitoneal sublay and intraperitoneal onlay mesh repair for ventral hernia. Sci Rep 15, 3179 (2025). https://doi.org/10.1038/s41598-025-87555-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-87555-x